Abstract
Background
Classification of infants into low birth weight (LBW, <2500 g) or very low birth weight (VLBW, <2000 g) categories is a crucial step in targeting interventions to high-risk infants.
Objective
To compare the validity of chest circumference and foot length as surrogate anthropometric measures for the identification of LBW and VLBW infants.
Subjects and setting
Newborn infants (n = 1640) born between March and June 2004 in 30 Village Development Committees of Sarlahi district, Nepal.
Design
Chest circumference, foot length and weight (SECA 727, precise to 2 g) of newborns were measured within 72 h after birth. The sensitivity, specificity and predictive values for a range of cutoff points of the anthropometric measures were estimated using the digital scale measurements as the gold standard.
Results
Among LBW infants (469/1640, 28.6%), chest circumference measures <30.3 cm were 91% sensitive and 83% specific. Similar levels of sensitivity for foot length were achieved only with considerable loss of specificity (<45%). Foot length measurements <6.9 cm were 88% sensitive and 86% specific for the identification of VLBW infants.
Conclusion
Chest circumference was superior to foot length in classification of infants into birth weight categories. For the identification of VLBW infants, foot length performed well, and may be preferable to chest circumference, as the former measure does not require removal of infant swaddling clothes. In the absence of more precise direct measures of birth weight, chest circumference is recommended over foot length for the identification of LBW infants.
Sponsorship
The National Institute of Child Health and Human Development; the Saving Newborn Lives Initiative, Save the Children – US and the Office of Heath and Nutrition, United States Agency for International Development (see Acknowledgements).
Keywords: anthropometric surrogates, low birth weight, chest circumference, foot length, Nepal
Introduction
Birth weight is the single most important predictor of neonatal mortality in developing countries (Save the Children Federation, 2001). Although little progress has been made in recent decades to reduce global rates of low birth weight (LBW, <2500 g), available evidence suggests that improved care of LBW infants may substantially improve survival (Bhutta et al., 2005; Darmstadt et al., 2005a). In resource-poor settings where most infants are born in the home, effective community-based interventions may be targeted to LBW babies and will likely be delivered by minimally trained community health workers (CHWs) or traditional birth attendants. In order for targeted interventions to be practical, methods for the identification of LBW infants in the home must be low cost and usable by CHWs.
In these settings, few infants will have birth weight measured in a health facility and accurate scales are rarely available in the community. Therefore, efforts have been made to identify more easily measured anthropometric surrogates for birth weight. A number of studies have focused on measuring the circumference of the head, chest, mid upper-arm, thigh or calf and observed the correlation with continuous measurements on a gold standard weighing scale (Bhargava et al., 1985; Ramji et al., 1986; Singh et al., 1988; Ngowi et al., 1993; WHO Collaborative Study of Birth Weight Surrogates, 1993; Raymond et al., 1994; Arisoy and Sarman, 1995; Kapoor et al., 1996; Dhar et al., 2002; Naik et al., 2003). In general, chest circumference has performed better than other measures and has been recommended for continued investigation (ACC/SCN, 2000), although investigators have demonstrated correlations between birth weight and mid upper-arm circumference (Sauerborn et al., 1990), calf (Gupta et al., 1996; Samal and Swain, 2001) or thigh (Sharma et al., 1989) that are as strong as with chest circumference.
Studies of neonatal foot length have mainly examined the utility of this measure as a surrogate for crown-to-heel length and birth weight to facilitate estimates of body surface area for use in dosing regimens (James et al., 1979; Mathur et al., 1984; Gohil et al., 1991). Only rarely have measurements of foot length and birth weight been directly compared (Daga et al., 1988), or specific cutoffs for foot lengths been evaluated as a method to identify LBW babies (Daga et al., 1988; Hirve and Ganatra, 1993). Like chest circumference, it is easier to sight the line of measurement when determining foot length compared with mid upper-arm, calf or thigh circumference. Foot length measures can also be performed without exposing the infant to hypothermia risk.
Although the proposed implementation context for these surrogates is the community, with few exceptions (Hirve and Ganatra, 1993; Hossain et al., 1994) studies of anthropometric surrogates have been conducted in hospitals. These studies likely overestimated the correlation between these surrogate measures and birth weight because they used limited numbers of highly trained personnel (Bhargava et al., 1985; Sharma et al., 1989; Huque and Hussain, 1991; Walraven et al., 1994; Arisoy and Sarman, 1995; Ahmed et al., 2000). Furthermore, infants born and/or measured in hospitals may not be representative of those born in the community.
Most neonatal deaths occur in the community (Lawn et al., 2005) and some interventions, including vitamin A supplementation (Rahmathullah et al., 2003), newborn skin cleansing with chlorhexidine (Tielsch et al., 2005) and topical emollient therapy (Darmstadt et al., 2004, 2005b), may be targeted preferentially to LBW infants to reduce mortality risk. Thus, continued efforts are required to describe optimal methods for identifying these high-risk infants in the community. In Sarlahi district of South-central Nepal, in the flatlands close to the Indian border, 95% of infants are born in the home and approximately 30% are LBW (Christian et al., 2003; Tielsch et al., 2005). In this district, a large community-based trial studied the effect of newborn skin and umbilical cord cleansing with chlorhexidine (Tielsch et al., 2005; Mullany et al., 2006b). Further collection of birth weights with a high-precision digital neonatal scale provided an opportunity to compare the utility of foot length and chest circumference as surrogates for identifying LBW infants in the community.
Methods
This study was carried out by the Nepal Nutrition Intervention Project, Sarlahi (NNIPS). The NNIPS surveillance area consists of 30 Village Development Committees, in Sarlahi district of Southern Nepal. The predominately rural farming communities of this district share cultural, social and economic characteristics common to a large area of northern India, Northwestern Bangladesh and Southern Nepal. The population is composed mostly of peasant farmers or laborers and their families and is considered a poor area even in Nepal with almost three-fourths of the population below the poverty line (Pradhan et al., 1999). Over 95% of infants are born in the home without the assistance of skilled birth attendants. Throughout the parent trial, women were enrolled and followed during pregnancy, and newborn infants were visited in the home periodically during the neonatal period by non-medical field workers. At the first home visit after delivery, birth weight was collected as a comparative measure of neonatal mortality risk across treatment groups. Weight was measured using a digital scale with precision of 2 g (SECA Digital Scale Model 727).
Before the study, all workers (n = 11) were trained in conducting the anthropometric measurements using a pictorial manual, demonstrations and practice measurements with a group of 10 infants. Additionally, all workers were observed directly and given constructive feedback and advice by one of the authors (LCM) during the first week of household visits. Between March and June 2004, workers additionally explained the procedures and aims of the anthropometrical surrogates study, and informed consent was obtained.
Chest circumference was measured to the nearest 0.1 cm at the level of the nipples during mid-stage of expiration of breath, using an insertion tape (Ross Laboratories, Colombus, OH, USA) In order to measure foot length, the worker placed the newborn's right heel on a stabilizing board, with the sole of the foot pressed flat against a vertical rule. A sliding level with fiberglass view-window was depressed until the tip of the infant's toe touched the window. At that point, the level was secured and the worker recorded the level (to the nearest 0.1 cm) of the window relative to the vertical rule. Both anthropometric measures were repeated three times; the median of the three measurements for each of the anthropometric indicators was used in analyses. Lastly, the workers weighed the infants using the gold standard digital scale. Before each measurement, the scale was calibrated using reference weights of 1000 and 1100 g.
The eligible sample consisted of all infants enrolled in the parent trial from March to June 2004. The required sample size (n = 1070) was based on the number of infants necessary to estimate sensitivity of a priori cutoffs for foot length or chest circumference to within 5%. Assumptions included a 30% prevalence of LBW (based on data from the previous year), type I error equal to 5% and a minimum sensitivity of 70%.
Data were entered into a SQL Server 7.0 (Microsoft Corp., Redmond, WA, USA) database and analyzed using Stata version 8.0 (StataCorp., College Station, TX, USA). Only infants with data for the digital scale and both of the anthropometric measures collected within 72 h of birth were included in the analysis. For the first set of analyses, infants were defined as LBW if the gold standard weight measurement using the digital scale was <2500 g. For each infant, this binary variable (normal vs LBW) was created from the continuous weight measurements recorded using the gold standard digital scale. Over a range of a priori selected cutoffs for foot length and chest circumference, each newborn was again classified as LBW or normal and the two binary variables were compared. Sensitivity, specificity, and positive and negative predictive values were estimated over the range of cutoff values for both neonatal foot length and chest circumference. The initial criterion for selecting the optimal cutoff value was that which maximized the average of sensitivity and specificity. This can also be interpreted as the value that maximized the probability that the surrogate measure would distinguish between LBW and normal infants (Hanley and McNeil, 1982). Cutoff values near this point, however, were also considered for selection, as slightly more importance can be placed on identifying LBW infants (i.e. sensitivity may be more important than specificity).
These analyses were repeated, using very low birth weight (VLBW) as the weight cutoff. Here, infants were defined as VLBW if the gold standard digital scale measure was <2000 g, and over a range of cutoffs for foot length and chest circumference, the anthropometric surrogates and the gold standard weight classification were compared. Throughout this paper, the term LBW refers to all infants <2500 g (including those <2000 g), whereas the term VLBW refers to all infants <2000 g.
Time of birth and time of measurement of the anthropometric surrogates and birth weight were also recorded. As the age at measurement varied within the first 3 days of life, a stratified analysis (<24 vs 24−72 h) of the utility of these surrogate measures in identifying weight class was also conducted.
Approval for this study was obtained from the Nepal Health Research Council of the Ministry of Health/Nepal and the Committee on Human Research of the Johns Hopkins Bloomberg School of Public Health.
Results
Between 5 March and 30 June 2004, 1890 infants were born in the study area and were eligible for enrollment in the study. Among these, the mothers of nine infants declined to participate, and data for chest circumference, foot length or both were missing for 10. Of the remaining 1871 infants, weight data were missing for four infants, 55 were measured with a backup digital scale with reduced precision and 172 were older than 72 h when measurements were collected. The remaining 1640 (87.7%) infants were included in the data analysis. The range of the three measurements taken for each infant was calculated to assess the repeatability of the measures. For chest circumference and foot length, the within-infant range of measures was ≤0.2 cm in 97.5 and 98.4% of infants, respectively.
According to the scale measurements, there were 469 infants with birth weight <2500 g, for a total LBW prevalence estimate of 28.6% (95% confidence interval (CI): 26.4−30.9%). Of these LBW infants, 80 were <2000 g (4.9% (95% CI: 3.9−6.0%)). There were approximately equal numbers of male (50.1%) and female (49.9%) infants, and the mean and median age at measurement was 20.4 and 17.6 h, respectively. A summary of birth weight and anthropometric characteristics (mean, median and range of chest circumference and foot length) for normal, LBW (including VLBW) and VLBW infants are shown in Table 1.
Table 1.
Summary measures of weight, chest circumference and foot length of study infants
|
Birth weight category |
|||
|---|---|---|---|
| VLBW (<2000 g) | LBW (<2500 g) | Normal (≥2500 g) | |
| Number of infants | 80 | 469 | 1171 |
| Birth weight | |||
| Mean (g) | 1810.7 | 2226.1 | 2914.1 |
| s.d. (g) | 175.6 | 235.3 | 278.9 |
| Median (g) | 1874 | 2296 | 2876 |
| Range (g) | 1254−1998 | 1254−2498 | 2501−4098 |
| Chest circumference | |||
| Mean (cm) | 26.6 | 28.7 | 31.6 |
| s.d. (cm) | 1.4 | 1.4 | 1.3 |
| Median (cm) | 26.7 | 29.0 | 31.5 |
| Range (cm) | 22.8−29.2 | 22.8−32.2 | 26.2−37.1 |
| Foot length | |||
| Mean (cm) | 6.5 | 6.8 | 7.3 |
| s.d. (cm) | 0.4 | 0.4 | 0.3 |
| Median (cm) | 6.5 | 6.9 | 7.3 |
| Range (cm) | 5.7−7.4 | 5.7−7.7 | 6.1−8.4 |
Abbreviations: LBW, low birth weight; VLBW, very low birth weight; s.d., standard deviation.
The gold standard digital scale weights were plotted against the chest circumference and foot length measures as shown in Figure 1a and b, respectively. The sensitivity, specificity, and positive and negative predictive values for classifying infants into LBW status for a range of cutoffs of chest circumference and foot length are shown in Table 2. Only values for chest circumference where both sensitivity and specificity exceed 70% are included. The chest circumference value that maximized the average of sensitivity and specificity was 30.2 cm. For a cutoff rule of 30.3 cm, however, chest circumference was 91% sensitive and 83% specific for classification of LBW in this sample. To achieve greater than 95% sensitivity, however, all infants with chest circumference values less than 30.7 cm had to be included, resulting in concomitant decreases in specificity (<75%) and positive predictive value (<60%). Similarly, the optimal cutoff value for foot length was 7.1 cm, and if increased beyond 7.2 cm (81% sensitive, 69% specific), the specificity of LBW categorization was considerably impacted (≤56%). In order to reach the same level of sensitivity as the optimal chest circumference cutoff of 30.3 cm, the cutoff for foot length had to be increased to 7.4 cm, but this resulted in substantial loss of specificity (<45%).
Figure 1.
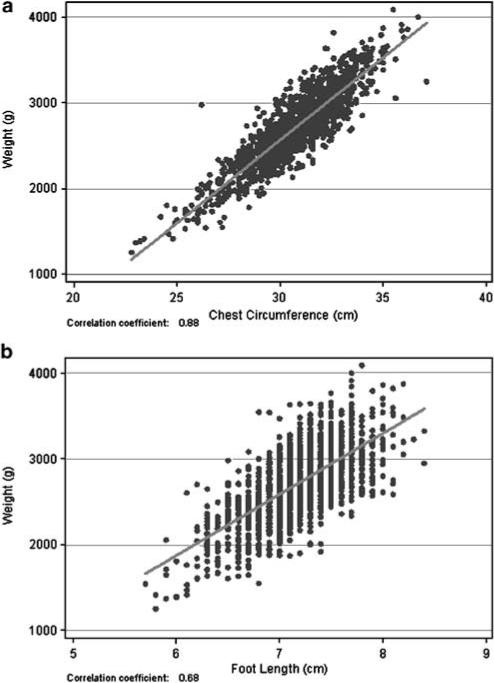
Scatter plots of (a) chest circumference and (b) foot length measures vs birth weight (n = 1640).
Table 2.
Sensitivity, specificity and predictive values for chest circumference and foot length as surrogates for low birth weight (<2500 g) for range of cutoff values
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
|---|---|---|---|---|
| Chest circumference (cm) | ||||
| 29.7 | 73.8 | 94.6 | 84.6 | 90.0 |
| 29.8 | 79.7 | 92.7 | 81.5 | 92.0 |
| 29.9 | 79.7 | 92.7 | 81.5 | 92.0 |
| 30.0 | 81.9 | 91.8 | 80.0 | 92.7 |
| 30.1 | 84.4 | 89.4 | 76.2 | 93.5 |
| 30.2 | 86.8 | 87.5 | 73.6 | 94.3 |
| 30.3 | 90.6 | 83.3 | 68.5 | 95.7 |
| 30.4 | 90.6 | 83.3 | 68.5 | 95.7 |
| 30.5 | 92.3 | 80.9 | 65.9 | 96.3 |
| 30.6 | 94.2 | 77.0 | 62.2 | 97.1 |
| 30.7 | 95.1 | 74.3 | 59.7 | 97.4 |
| 30.8 | 96.4 | 71.0 | 57.1 | 98.0 |
| 30.9 | 96.4 | 71.0 | 57.1 | 98.0 |
| Foot length (cm) | ||||
| 6.8 | 36.9 | 96.6 | 81.2 | 79.3 |
| 6.9 | 47.1 | 94.2 | 76.5 | 81.6 |
| 7.0 | 57.4 | 90.0 | 69.7 | 84.1 |
| 7.1 | 73.1 | 80.4 | 59.9 | 88.2 |
| 7.2 | 81.2 | 69.6 | 51.7 | 90.3 |
| 7.3 | 88.7 | 56.4 | 44.9 | 92.6 |
| 7.4 | 94.5 | 43.7 | 40.2 | 95.2 |
| 7.5 | 97.4 | 32.7 | 36.7 | 97.0 |
A similar analysis of sensitivity, specificity and predictive values for chest circumference and foot length cutoffs for identifying infants <2000 g is shown in Table 3. Positive predictive values quickly decrease with small deviations from 100% specificity, because of the low overall prevalence of VLBW. Within the selected range, the optimal cutoff for chest circumference was <28.4 cm. At this value, both sensitivity and specificity was high (95 and 94%, respectively). A cutoff of 6.9 cm for foot length identified 88% of infants <2000 g with high specificity (86%).
Table 3.
Sensitivity, specificity and predictive values for chest circumference and foot length as surrogates for <2000 g for range of cutoff values
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
|---|---|---|---|---|
| Chest circumference (cm) | ||||
| 27.8 | 82.5 | 97.8 | 65.3 | 99.1 |
| 27.9 | 83.8 | 97.6 | 63.8 | 99.2 |
| 28.0 | 83.8 | 97.6 | 63.8 | 99.2 |
| 28.1 | 88.8 | 96.8 | 58.7 | 99.4 |
| 28.2 | 90.0 | 96.2 | 54.5 | 99.5 |
| 28.3 | 92.5 | 94.7 | 47.1 | 99.6 |
| 28.4 | 95.0 | 93.7 | 43.4 | 99.7 |
| 28.5 | 95.0 | 93.7 | 43.4 | 99.7 |
| 28.6 | 96.3 | 92.3 | 39.1 | 99.8 |
| 28.7 | 96.3 | 91.5 | 36.8 | 99.8 |
| 28.8 | 96.3 | 90.4 | 33.9 | 99.8 |
| 28.9 | 97.5 | 90.0 | 33.3 | 99.9 |
| 29.0 | 97.5 | 90.0 | 33.3 | 99.9 |
| 29.1 | 98.8 | 88.4 | 30.4 | 99.9 |
| 29.2 | 98.8 | 87.2 | 28.4 | 99.9 |
| 29.3 | 100.0 | 84.6 | 24.9 | 100.0 |
| Foot length (cm) | ||||
| 6.5 | 47.5 | 98.1 | 56.7 | 97.3 |
| 6.6 | 51.3 | 96.5 | 42.7 | 97.5 |
| 6.7 | 63.8 | 94.2 | 35.9 | 98.1 |
| 6.8 | 77.5 | 90.3 | 29.1 | 98.7 |
| 6.9 | 87.5 | 86.0 | 24.2 | 99.3 |
| 7.0 | 92.5 | 80.0 | 19.2 | 99.5 |
| 7.1 | 95.0 | 68.1 | 13.3 | 99.6 |
| 7.2 | 96.3 | 57.7 | 10.4 | 99.7 |
| 7.3 | 97.5 | 45.6 | 8.4 | 99.7 |
Non-parametric receiver operating characteristic (ROC) analyses were conducted to compare the overall utility of foot length and chest circumference. ROC curves for the identification of LBW infants for both anthropometric measures are displayed in Figure 2. The overall area under the curve for chest circumference was significantly higher than for foot length (0.95 vs 0.85, respectively, P<0.0001). For the identification of infants <2000 g, chest circumference was again superior to foot length (area under the curve = 0.99 vs 0.93), although the difference between the curves for VLBW infants was less, and the estimated area under the curve was relatively high for both surrogates. These curves are consistent with data provided in Tables 2 and 3, and demonstrate that both surrogate measures are more useful for distinguishing between VLBW and non-VLBW infants than between LBW and non-LBW infants.
Figure 2.
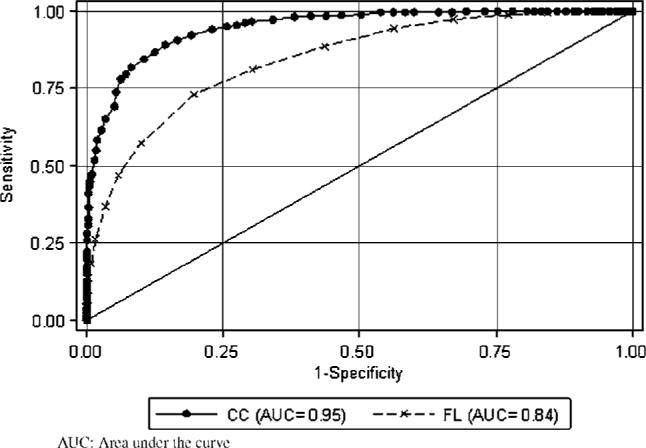
Comparison of chest circumference (CC) and foot length (FL) as surrogates for low birth weight using non-parametric ROC curves.
There were 1162 (71%) infants measured within the first 24 h of life. Results stratified by age at measurement are shown in Table 4. The sensitivity and specificity of chest circumference at the optimal cut-points described above, and the overall area under the ROC curve, are similar across the age groups for both LBW and VLBW identification. For foot length, the similarity between age groups holds true for the identification of LBW, whereas the validity of the surrogate measure may be decreased in the older infants when identifying VLBW. There was insufficient power, however, to detect this difference statistically.
Table 4.
Sensitivity and specificity at optimal cutoffs and overall area under the ROC curve, stratified by age at measurement
| <24 h (n = 1162) | 24−72 h (n = 478) | |
|---|---|---|
| Chest circumference | ||
| LBW vs normal | ||
| Sens/spec at 30.3 cm | 90, 84 | 92, 81 |
| Overall AUC | 0.95 | 0.95 |
| VLBW vs non-VLBW | ||
| Sens/spec at 28.4 cm | 94, 94 | 89, 94 |
| Overall AUC | 0.99 | 0.98 |
| Foot length | ||
| LBW vs normal | ||
| Sens/spec at 7.1 cm | 80, 71 | 77, 76 |
| Overall AUC | 0.85 | 0.84 |
| VLBW vs non-VLBW | ||
| Sens/spec at 6.9 cm | 93, 82 | 78, 84 |
| Overall AUC | 0.95 | 0.88 |
Abbreviations: AUC, area under the curve; LBW, low birth weight; ROC, receiver operating characteristic; VLBW, very low birth weight
Conclusions
Unlike data from most previous studies of anthropometric measures that have been hospital based, data in this study were collected among newborns within the home and were restricted to infants less than 72 h of age. These data from over 1600 infants demonstrate that neonatal chest circumference measures collected in a low-resource community can be utilized to establish cutoffs for identifying LBW infants with a balance of high sensitivity and specificity. Furthermore, compared to the use of foot length, classification rules based on chest circumference measures were more sensitive and specific for identifying LBW infants. The superior performance of chest circumference over foot length is in line with the conclusions of previous studies that chest circumference is the optimal anthropometric measure for establishing cutoffs for the identification of LBW infants (WHO Collaborative Study of Birth Weight Surrogates, 1993; Walraven et al., 1994; Naik et al., 2003).
Chest circumference measures were also superior to foot length measures for the identification of babies <2000 g, although the difference in validity was less pronounced than for the distinction between LBW and normal weight (≥2500 g) infants. The overall area under the ROC curve was high for both chest circumference and foot length for the identification of VLBW infants, and a foot-length cutoff point (6.9 cm) with relatively high sensitivity and specificity could be identified. This suggests that the use of foot length may still be useful or even preferable for the identification of very small newborn infants. This is especially true given that measuring the chest circumference of infants requires the removal of swaddling clothes, whereas the foot length measures do not. Given that the consequences of exposure and subsequent hypothermia may be greater in very small infants, community-based efforts focusing on the identification of such infants could, by using foot length measures, avoid inadvertently contributing to hypothermia risk.
For use in low-resource settings, any anthropometric device must be inexpensive and easy to maintain. Color-coded insertion tapes for measurement of chest circumference can be easily made using locally available materials (Singh et al., 1988). Similarly, the materials used in this study for measuring foot length were constructed using inexpensive materials found locally, and followed inexpensive models previously described in the literature (Mathur et al., 1984; Ramachandran, 1986; Daga et al., 1988).
There were limitations to this study. The same workers who collected the anthropometric measures also recorded the gold standard digital scale birth weight, potentially introducing observer bias. We attempted to minimize this by requiring the workers to record the anthropometric measures before recording infant weight. Not all infants were measured at the time of birth, and infant weight can vary considerably during the first 72 h of life (MacDonald et al., 2003; Wright and Parkinson, 2004). Our stratified analysis suggests that, in this population, similar conclusions regarding optimal cutoffs for foot length and chest circumference may be drawn during this time period. These data do not, however, provide for a more detailed analysis of the impact of delayed surrogate measurements, as the measurement of birth weight was similarly delayed for infants <24 h of age. As foot length and chest circumference measures over this short time period are unlikely to vary to the same degree as body weight, the sensitivity and specificity estimates for any particular selected cutoff rule may not reflect the validity of that measure at the time of birth. In a community-based program where such measures are utilized to identify LBW infants, the time of measurement may, however, be similar to the range of measures in this study, suggesting that our non-stratified estimates of surrogate validity are reflective of what would be encountered during routine programmatic use.
As has been pointed out previously (Mullany et al., 2006a), the use of any anthropometric surrogate for LBW identification in the community will be limited by the need for establishing community-specific classification rules. Such rules can be established, however, with little cost, and including a training module for the measurement of chest circumference or foot length could be included when updating the skills of community-based outreach workers in neonatal health programs. The non-medical field workers in this study may be similar in ability to health workers in such programs, but standardization of larger numbers of workers, or extending the use of these measures to traditional birth attendants may require more intensive training, and/or cutoff rules with less precision (e.g., 0.5 cm for chest circumference).
Recent investigations have identified a number of simple, inexpensive, effective interventions for reducing mortality specifically among high-risk LBW infants, including vitamin A supplementation (Rahmathullah et al., 2003), full-body cleansing of newborns (Tielsch et al., 2005) and topical emollient therapy (Darmstadt et al., 2004, 2005b). As these interventions are low cost, any optimal anthropometric surrogate should be selected based on high sensitivity, as opposed to high specificity. In the absence of a low-cost scale such as the recently validated hand-held scale ‘Birthweigh III’ (Mullany et al., 2006a), or other more precise direct measures of weight, chest circumference is recommended over foot length, based on its comparative validity relative to gold standard digital measures, and the overall ease of measurement. If the focus of such identification programs is on infants <2000 g, foot length measures could be used to minimize exposure of infants to hypothermia risk.
Acknowledgements
This study was supported by grants from the National Institutes of Health, National Institute of Child Health and Human Development (HD44004 and HD38753); Save the Children – US through a grant from The Bill & Melinda Gates Foundation (810-2054); and cooperative agreements between the Johns Hopkins Bloomberg School of Public Health and the Office of Health, Infectious Diseases and Nutrition, Global Health Bureau, United States Agency for International Development (HRN-A-00-97-00015-00, GHS-A-00-03-000019-00). We thank Vishwajeet Kumar for development and provision of the foot length boards used in this study.
Footnotes
Guarantor: LC Mullany.
Contributors: LCM – concept, design, implementation, quality control, data management, analysis, interpretation and writing of manuscript; GLD – concept, design, interpretation and writing of manuscript; SKK – design, implementation, quality control, review and approval of manuscript; SCL – design, implementation, quality control, review and approval of manuscript; JMT – concept, design, interpretation and writing of manuscript.
References
- ACC/SCN . Low Birthweight: Report of a Meeting in Dhaka, Bangladesh on 14−17 June 1999. In: Pojda J, Kelley L, editors. Nutrition Policy Paper No. 18. ACC/SCN in collaboration with ICDDR,B; Geneva: 2000. [Google Scholar]
- Ahmed FU, Karim E, Bhuiyan SN. Mid-arm circumference at birth as predictor of low birth weight and neonatal mortality. J Biosoc Sci. 2000;32:487–493. doi: 10.1017/s0021932000004879. [DOI] [PubMed] [Google Scholar]
- Arisoy AE, Sarman G. Chest and mid-arm circumferences: identification of low birth weight newborns in Turkey. J Trop Pediatr. 1995;41:34–37. doi: 10.1093/tropej/41.1.34. [DOI] [PubMed] [Google Scholar]
- Bhargava SK, Ramji S, Kumar A, Mohan M, Marwah J, Sachdev HP. Mid-arm and chest circumferences at birth as predictors of low birth weight and neonatal mortality in the community. BMJ. 1985;291:1617–1619. doi: 10.1136/bmj.291.6509.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta ZA, Darmstadt GL, Hasan B, Haws R. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: review of the evidence. Pediatrics. 2005;115:519–617. doi: 10.1542/peds.2004-1441. [DOI] [PubMed] [Google Scholar]
- Christian P, Khatry SK, Katz J, Pradhan EK, LeClerq SC, Shrestha SR, et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. BMJ. 2003;15:571–576. doi: 10.1136/bmj.326.7389.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daga SR, Daga AS, Patole S, Kadam S, Mukadam Y. Foot length measurement from foot print for identifying a newborn at risk. J Trop Pediatr. 1988;34:16–19. doi: 10.1093/tropej/34.1.16. [DOI] [PubMed] [Google Scholar]
- Darmstadt GL, Badrawi N, Law PA, Alam A, Ahmed S, Husein MH, et al. Topical therapy with sunflower seed oil prevents nosocomial infections and mortality in premature babies in Egypt: a randomized, controlled clinical trial. Pediatr Infect Dis J. 2004;23:719–725. doi: 10.1097/01.inf.0000133047.50836.6f. [DOI] [PubMed] [Google Scholar]
- Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005a;365:977–988. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- Darmstadt GL, Saha SK, Ahmed AS, Chowdhury MA, Law PA, Ahmed S, et al. Effect of topical treatment with skin barrier-enhancing emollients on nosocomial infections in preterm infants in Bangladesh: a randomised controlled trial. Lancet. 2005b;365:1039–1045. doi: 10.1016/S0140-6736(05)71140-5. [DOI] [PubMed] [Google Scholar]
- Dhar B, Mowlah G, Nahar S, Islam N. Birth-weight status of newborns and its relationship with other anthropometric parameters in a public maternity hospital in Dhaka, Bangladesh. J Health Popul Nutr. 2002;20:36–41. [PubMed] [Google Scholar]
- Gohil JR, Sosi M, Vani SN, Desai AB. Footlength measurement in the neonate. Indian J Pediatr. 1991;58:675–677. doi: 10.1007/BF02820189. [DOI] [PubMed] [Google Scholar]
- Gupta V, Hatwal SK, Mathur S, Tripathi VN, Sharma SN, Saxena SC, et al. Calf circumference as a predictor of low birth weight babies. Indian J Pediatr. 1996;33:119–121. [PubMed] [Google Scholar]
- Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- Hirve SS, Ganatra BR. Foot tape measure for identification of low birth weight newborns. Indian J Pediatr. 1993;30:25–29. [PubMed] [Google Scholar]
- Hossain MM, Habib M, DuPont HL. Association between birth weight and birth arm circumference of neonates in rural Egypt. Indian J Pediatr. 1994;61:81–87. doi: 10.1007/BF02753565. [DOI] [PubMed] [Google Scholar]
- Huque F, Hussain AM. Detection of low birth-weight new born babies by anthropometric measurements in Bangladesh. Indian J Pediatr. 1991;58:223–231. doi: 10.1007/BF02751125. [DOI] [PubMed] [Google Scholar]
- James DK, Dryburgh EH, Chiswick ML. Foot length – a new and potentially useful measurement in the neonate. Arch Dis Child. 1979;54:226–230. doi: 10.1136/adc.54.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapoor SK, Kumar G, Anand K. Use of mid-arm and chest circumferences to predict birth weight in rural north India. J Epidemiol Community Health. 1996;50:683–686. doi: 10.1136/jech.50.6.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawn JE, Cousens S, Zupan J. Four million neonatal deaths: Where? When? Why? Neonatal Survival Series Paper 1. Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- Macdonald PD, Ross SR, Grant L, Young D. Neonatal weight loss in breast and formula fed infants. Arch Dis Child Fetal Neonatal Ed. 2003;88:F472–F476. doi: 10.1136/fn.88.6.F472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur A, Tak SK, Kothari P. ‘Foot length’ – a newer approach in neonatal anthropometry. J Trop Pediatr. 1984;30:333–336. doi: 10.1093/tropej/30.6.333. [DOI] [PubMed] [Google Scholar]
- Mullany LC, Darmstadt GL, Coffey P, Khatry SK, LeClerq SC, Tielsch JM. A low-cost, color-coded, hand-held spring scale accurately categorizes birth weight in low-resource settings. Arch Dis Child. 2006a;91:410–413. doi: 10.1136/adc.2005.088781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullany LC, Darmstadt GL, Khatry SK, Katz J, LeClerq SC, Shrestha SR, et al. Topical applications of chlorhexidine to the umbilical cord for prevention of omphalitis and neonatal mortality in Southern Nepal: a community-based, cluster-randomized trial. Lancet. 2006b;367:910–918. doi: 10.1016/S0140-6736(06)68381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik DB, Kulkarni AP, Aswar NR. Birth weight and anthropometry of newborns. Indian J Pediatr. 2003;70:145–146. doi: 10.1007/BF02723742. [DOI] [PubMed] [Google Scholar]
- Ngowi JA, Redding-Lallinger R, Hirji KF. An assessment of the use of anthropometric measures for predicting low birth weight. J Trop Pediatr. 1993;39:356–360. doi: 10.1093/tropej/39.6.356. [DOI] [PubMed] [Google Scholar]
- Pradhan EK, LeClerq SC, Khatry SK, Adhikari RK, Ram RM, West KP, Jr, et al. A Window to Child Health in the Terai, NNIPS Monograph No. 1. Nepal Nutrition Intervention Project – Sarlahi; Kathmandu, Nepal: 1999. [Google Scholar]
- Rahmathullah L, Tielsch JM, Thulasiraj RD, Katz J, Coles C, Devi S, et al. Impact of supplementing newborn infants with vitamin A on early infant mortality: community based randomised trial in Southern India. BMJ. 2003;327:254–259. doi: 10.1136/bmj.327.7409.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran CR. A simple device for measurement of foot length in neonates. J Trop Pediatr. 1986;32:267–268. doi: 10.1093/tropej/32.5.268. [DOI] [PubMed] [Google Scholar]
- Ramji S, Marwah J, Satyanarayana L, Kapani V, Mohan M, Bhargava SK. Neonatal thigh circumference as an alternative indicator of low birth weight. Indian J Med Res. 1986;83:653–654. [PubMed] [Google Scholar]
- Raymond EG, Tafari N, Troendle JF, Clemens JD. Development of a practical screening tool to identify preterm, low-birthweight neonates in Ethiopia. Lancet. 1994;344:524–527. doi: 10.1016/s0140-6736(94)91905-4. [DOI] [PubMed] [Google Scholar]
- Samal GC, Swain AK. Calf circumference as an alternative to birth weight for identification of low birth weight babies. Indian J Pediatr. 2001;38:275–277. [PubMed] [Google Scholar]
- Sauerborn R, Ouiminga RM, Kone B, Sama R, Oepen C, Ebrahim GJ. Neonatal mid-upper-arm circumference is a valid proxy for birth-weight. Trop Med Parasitol. 1990;41:65–67. [PubMed] [Google Scholar]
- Save the Children Federation . Saving Newborn Lives. State of the World's Children; 2001. World Health Organization 2001 Estimates; pp. 1–49. [Google Scholar]
- Sharma JN, Saxena S, Sharma U. Thigh circumference at birth as the best predictor of low birth weight babies. Indian J Pediatr. 1989;26:18–21. [PubMed] [Google Scholar]
- Singh M, Paul VK, Deorari AD, Anandalakshmi PN, Sundaram KR. Simple tricoloured measuring tapes for identification of low birthweight babies by community health workers. Ann Trop Paediatr. 1988;8:87–91. doi: 10.1080/02724936.1988.11748546. [DOI] [PubMed] [Google Scholar]
- Tielsch JM, Darmstadt GL, Mullany LC, Khatry SK, Katz J, LeClerq SC. A Community-Based, Randomized Trial of Newborn Washing with Chlorhexidine on Neonatal Mortality in Southern Nepal. Pediatric Academic Societies. 2005 doi: 10.1542/peds.2006-1192. (Annual Meeting, May 14 2005 (Abstract)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walraven GE, Mkanje RJ, van Roosmalen J, van Dongen PW, Dolmans WM. Chest circumference as a screening method for low birth weight in newborns in rural Tanzania. Trop Geogr Med. 1994;46:14–16. [PubMed] [Google Scholar]
- WHO Collaborative Study of Birth Weight Surrogates Use of a simple anthropometric measurement to predict birth weight. Bull World Health Organ. 1993;71:157–163. [PMC free article] [PubMed] [Google Scholar]
- Wright CM, Parkinson KN. Postnatal weight loss in term infants: what is ‘normal’ and do growth charts allow for it? Arch Dis Child Fetal Neonatal Ed. 2004;89:F254–F257. doi: 10.1136/adc.2003.026906. [DOI] [PMC free article] [PubMed] [Google Scholar]


