Abstract
Objectives
The objectives of this study were to characterize the clinical performance and wear characteristics of lithia-disilicate-based ceramic crowns.
Methods
Thirty posterior crowns were made using the heat-pressing technique and lithia-disilicate-based core ceramic. Subjects were recalled annually. The quality of crowns and adjacent gingival tissues were examined using nine criteria for acceptability. All crowns were examined and ranked from 4 (Excellent) to 1 (Unacceptable) for each criterion. Impressions were made for replica models at each appointment. Wear characteristics of dental ceramic and enamel were obtained by comparing the surface of the original model with the follow-up model using a laser scanner.
Results
Twenty nine subjects returned for the one-year recall examination. The maximum clenching force for the 30 subjects ranged from 125 to 815 N. All clinical criteria were ranked good to excellent at the one-year recall exam and no fractures were observed. The mean occlusal wear volumes for the ceramic crowns after one year were 0.19 (0.065) mm3 for premolar sites and 0.34 (0.08) mm3 for molar sites. The mean occlusal wear volumes of opposing enamel after one year were 0.21 (0.06) mm3 for premolar teeth and 0.50 (0.22) mm3 for molar teeth. The mean occlusal wear volume of ceramic molar crowns was significantly lower than the volume of enamel wear of the opposing teeth (p≤0.05).
Conclusions
The quality of the overall prostheses and the gingival tissues were acceptable after one year. The mean occlusal wear volume of ceramic molar crowns was significantly lower than the enamel wear volume of the opposing teeth.
Keywords: clinical performance, ceramic crown, wear volume
Introduction
Dental ceramics have been widely used for construction of fixed dental prostheses for decades because they have several advantages such as their aesthetic quality and excellent biocompatibility. Clinical performance in posterior areas of metal-ceramic systems has been satisfactory from aesthetic and fracture resistance viewpoints. However, when used in anterior teeth, metal-ceramic prostheses are not as aesthetic as all-ceramic prostheses, which generally exhibit greater translucency and potentially have no visible metal substructure. These aesthetic advantages of all-ceramic systems combined with their excellent fracture resistance when used in anterior tooth sites have increased the demand for all-ceramic restorations.
The major disadvantages of ceramic materials are their low tensile strength, relatively low fracture toughness, and abrasiveness to opposing enamel [1–3]. These shortcomings limit their use in dental applications where high chewing and clenching forces are involved. The fracture resistance of dental ceramics and the wear characteristics of some dental porcelain and ceramics for all-ceramic systems have been reported in several studies [2–6]. Most of these reports represent in vitro studies that used some clinically relevant parameters as the test variables. The test results for ceramics and enamel have been presented as height loss, area loss, or volume loss. Also, several clinical studies have been performed to evaluate the clinical survival and performance of all-ceramic crowns [7–11]. Clinical performance of all-ceramic crowns is generally excellent in the anterior region and failure percentages range from 0 to 4% after 2 to11 years, respectively [7–9]. Failure percentages of posterior all-ceramic crowns ranged from 1 to 14% after 4 to 11 years, respectively. These failure values are greater than those for metal-ceramic restorations, which ranged from 2.3 to11% after 7.5 to 10 years, respectively [7–13]. The compositions of ceramics used in dentistry vary from a weak material with fracture toughness of 1 MPa•m1/2 to tougher materials having fracture toughness of 5–9 MPa•m1/2 [14–15]. Clinical performance of a ceramic crown is related to its mechanical properties. Tough materials are assumed to perform well and data from clinical studies appear to correlate roughly with the fracture toughness and strength of the core ceramics [7–12].
The data from several wear tests indicate that ceramic prostheses cause more wear to opposing enamel than do dental alloys, even though the failure mechanisms responsible for excessive wear of enamel caused by ceramic prostheses have not been conclusively identified [4–6]. It is uncertain whether data obtained from the in vitro studies are clinically relevant [16,17]. Wear is a progressive phenomenon associated with several factors [18]. Wear of enamel caused by ceramic prosthesis is a major concern because it is associated with the clinical success of the restoration.
The objectives of this study were to characterize the clinical performance and wear characteristics of all-ceramic posterior crowns. The wear rates of all-ceramic crowns and opposing enamel in selected patients were quantified. The relationship of each subject’s maximum clenching force to wear volume was also analyzed.
Materials and methods
Thirty adult subjects, of good to excellent overall dental health, were recruited from the pool of subjects on the waiting list of the Faculty of Dentistry, Mahidol University. These subjects were screened to exclude individuals with poor medical health. All selected subjects had healthy periodontal tissues, were free of active periodontal disease and caries, and showed no evidence of bruxing. For these 30 adult subjects, five were men and 25 were women with ages ranging between 20 to 56 years. Eligible subjects had at least one posterior endodontically treated tooth opposed by natural dentition in the maxillary or mandibular arch. This endodontically treated tooth was used as an abutment for an all-ceramic crown. After obtaining informed consent, a maximum of two crowns were placed per patient.
Prior to the preparation of the abutment tooth, the maximum clenching force capability of each subject was determined using a bite force gauge. The abutment tooth was prepared for a cast post and core as a foundation for the glass-ceramic crown. After the final preparation, an impression was made of the prepared tooth using a double impression technique with a polyvinyl siloxane impression material. A temporary acrylic resin crown was cemented on the prepared tooth using temporary cement (non-eugenol cement). The following minimal guidelines for the final tooth preparation were followed; axial tooth reduction of 1 mm, shoulder or deep chamfer design, occlusal reduction of 1.5–2 mm, and rounded inner angles/edges/transitions. The treatment and evaluation procedures were performed by three prosthodontists. Calibration between examiners was made using thorough discussion for the details ranking of each criterion to obtain agreement between examiners. Cross-examination between two examiners was performed randomly to obtain consistent evaluation.
The ceramic material used in this study was a lithia-disilicate-based all-ceramic system (Ivoclar Vivadent, Schaan, Liechtenstein). Thirty crowns were made using a layering technique according to the manufacturer’s instructions. Ceramic crowns were cemented using either temporary cement or resin cement. The crowns were divided into three groups as follows.
Group 1: Ten crowns were cemented with Variolink II resin cement (Ivoclar Vivadent).
Group 2: Ten crowns were cemented with temporary cement. These ten crowns were retrieved after one year of insertion. Ten new all-ceramic crowns were made for this group and cemented with Variolink II resin cement.
Group 3: Ten crowns were cemented with temporary cement. These ten crowns will be retrieved after two years of service. Ten new all-ceramic crowns will be made and cemented with Variolink II resin cement.
After try-in and occlusal adjustment, each crown was glazed before insertion. Patients were informed that the temporarily cemented crowns would function as effectively as “permanently” cemented crowns. After cementation, impressions were made using polyvinyl siloxane for the upper and lower arches. The models were poured using synthetic stone (Fujirock, GC, Japan). These models were marked as baseline models. The patients were recalled after one year and two years. At the recall appointments, impressions were made for replica models. The occlusal contacts were observed and photographically recorded.
Examinations of the overall prosthesis, the marginal area, the adjacent gingival tissues, and the occlusion were evaluated at baseline, one year and two years. The following data were recorded: 1) gingival health; 2) occlusion; 3) secondary caries; 4) integrity of the restoration; 5) sensitivity to mastication; 6) facial and lingual marginal adaptation; 7) facial or lingual marginal discoloration; 8) contour and proximal contact of the restoration; and 9) patient satisfaction with the prosthesis or prostheses. One or two standard radiographs were taken of the abutment tooth at each recall. The resulting X-ray films were used for diagnostic purposes to determine periodontal health and the presence or absence of secondary caries and resin overhangs. The quality of crowns and tissues were examined at baseline and at each recall appointment for acceptability. Rankings of each criterion were made from 1 to 4; 4 = excellent, 3 = good, 2 = unacceptable, needs replacement in the near future, 1 = unacceptable, needs immediate replacement.
Wear analysis
Wear characteristics of ceramic crowns and enamel were obtained by comparing the surface of the original model with the follow-up model. The volume loss was determined using a 3-D laser scanner (Etkon, Willytec GmbH, Gräfelfing, Germany). The precision of this device is ±20 μm. The wear patterns of dental ceramic surfaces were characterized using a scanning electron microscope (SEM).
Statistical analysis
All data were analyzed using Student’s t-test to determine the differences between mean wear volumes for the crowns and opposing teeth observed at baseline and those at each recall time.
Results
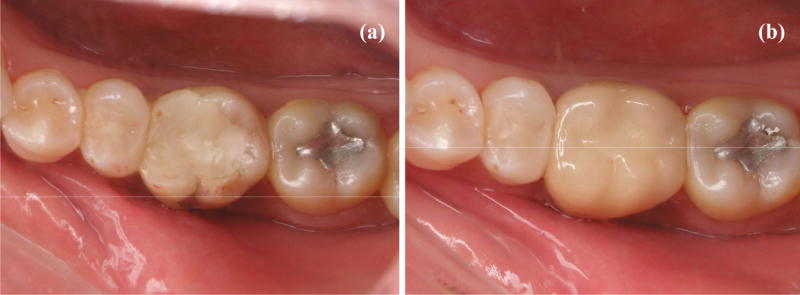
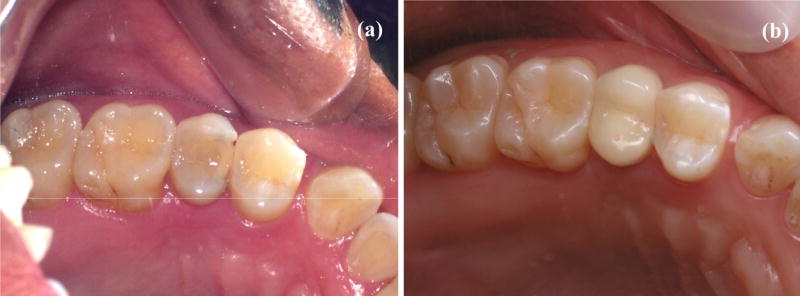
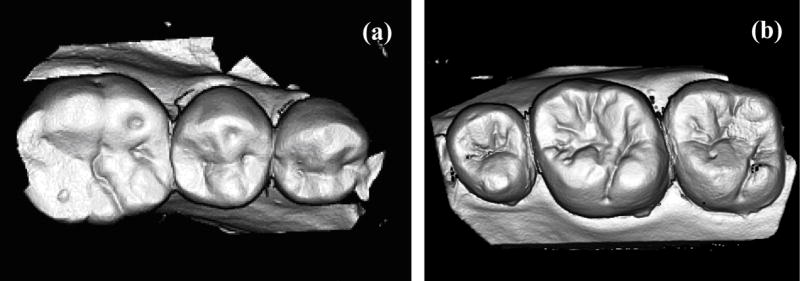
The quality of crowns and tissues were examined at baseline and one-year recall appointments and the results are summarized in Table 1. Twenty nine subjects returned for one-year recall examination. There were sixteen molar crowns and thirteen premolars. The overall clinical performance of ceramic crowns was rated good to excellent after one year. No fractures were observed. Representative photographs of the ceramic crowns are shown in Figure 1–2.
Table 1.
The quality of crowns and tissues examined after one year.
| Parameters | Number of subjects | |||
|---|---|---|---|---|
| 4 | 3 | 2 | 1 | |
| 1. gingival health | 21 | 8 | - | - |
| 2. occlusion | 29 | - | - | - |
| 3. integrity of restoration | 29 | - | - | - |
| 4. secondary caries | 29 | - | - | - |
| 5. facial and lingual marginal adaptation | 29 | - | - | - |
| 6. facial or lingual marginal discoloration | 29 | - | - | - |
| 7. sensitivity to temperature and mastication | 29 | - | - | - |
| 8. contour and proximal contact of the restoration | 29 | - | - | - |
| 9. patient satisfaction | 15 | 14 | - | - |
4 = Excellent, 3 = good, 2 = need replacement in the future, 1 = need immediate replacement
Figure 1.
Representative photographs of an abutment second premolar tooth (a) before treatment, (b) at the one-year recall exam.
Figure 2.
Representative photographs of an abutment molar tooth (a) before treatment, (b) at the one-year recall.
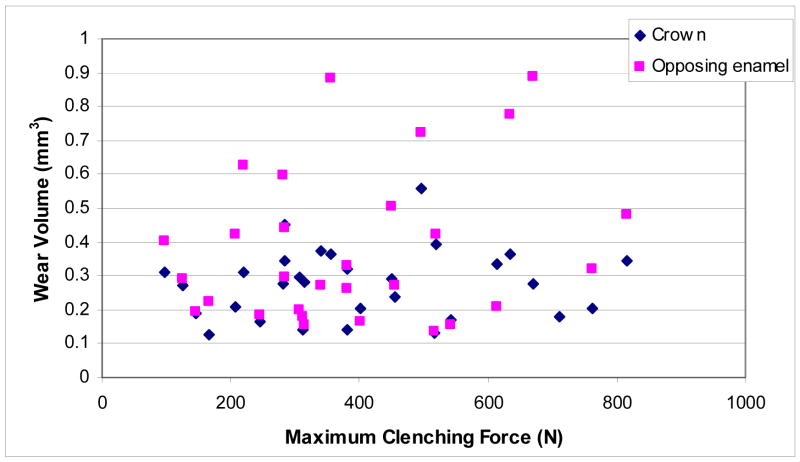
The maximum clenching force for the 30 subjects ranged between 125 and 815 N. These values are within normal limits reported from a previous review [19]. The mean maximum clenching force was 394 ± 193 N. The relationship of each subject’s maximum clenching force to wear volume was analyzed using linear regression analysis (Fig. 3). The results showed that there was no significant relationship between maximum clenching force and the wear rate of enamel (R2 = 0.08) or ceramic crowns (R2 = 0.02).
Figure 3.
Wear volume of ceramic crowns and opposing enamel.
Wear analysis
After one year the mean occlusal wear volumes of enamel were 0.21 ± 0.06 mm3 for premolar teeth and 0.50 ± 0.22 mm3 for molar teeth, respectively. This was not significantly higher (p>0.05) than the volume of enamel wear for the contralateral teeth (0.20 ± 0.09 mm3 for premolars and 0.4 ± 0.16 mm3 for molars). The mean occlusal wear volumes of ceramic crowns after 1 year were 0.19 ± 0.06 mm3 for premolars and 0.34 ± 0.08 mm3 for molars, respectively (Table 2). The mean occlusal wear volume of ceramic molar crowns was significantly lower than the enamel wear of the opposing natural tooth (p≤0.05). The representative laser-scan images of ceramic crowns and opposing teeth are shown in Figures 4 to 6. The vertical height loss of opposing enamel for both premolar and molar teeth was higher than those of ceramic crowns.
Table 2.
Mean occlusal wear of ceramic crowns and opposing enamel.
| Group | Wear volume (mm3) | Wear height (μm) |
|---|---|---|
| Premolar (crown) | 0.19 (0.06) | 29 (12) |
| Molar (crown) | 0.34 (0.08) | 36 (34) |
| Premolar (enamel) | 0.21 (0.06) | 46 (13) |
| Molar (enamel) | 0.50 (0.22) | 65 (29) |
Figure 4.
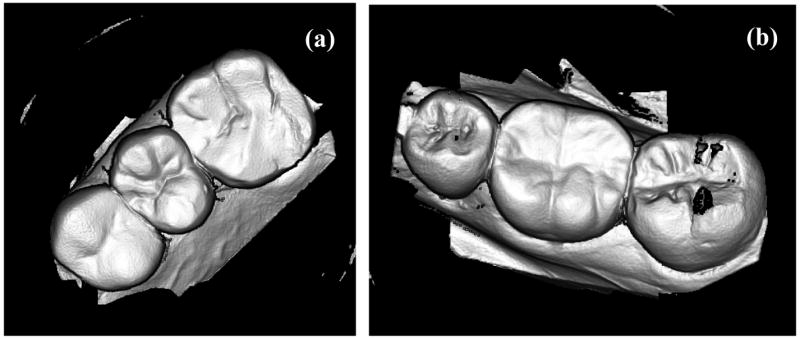
Laser-scan images of a first premolar ceramic crown (a) and a molar ceramic crown (b)
Figure 6.
Laser-scan images of (a) a premolar tooth and (b) a molar tooth that have been worn by a ceramic crown after one year.
Discussion
The overall clinical performance of hot-pressed ceramic crowns was rated good to excellent after one year. One subject was missing from the study and these data were not used for analyzing the results. No fracture or evidence of secondary caries was observed in this study. The success rate of hot-pressed ceramic crowns was 100% after one year and this result was in agreement with the results from a previous study [20]. Fracture of dental ceramics is the most common type of failure for ceramic prostheses because of their low tensile strength and their generally low fracture toughness of the ceramic layers. The fracture rates of 2.7 to 30% after 1.5–14 years have been reported for all-ceramic crowns [7,9,21–22]. A high failure rate of all-ceramics limits their use in dentistry even though their aesthetic quality is superior to that of metal-ceramic restorations. For metal-ceramic prostheses, the failure rate is lower and the fracture of ceramic veneers is not as significant as that observed in other studies. Follow-up of the crowns in this study is necessary for further conclusions to be made.
Enamel wear is a progressive phenomenon associated with several factors, including the physical, microstructural and surface characteristics of ceramic restorations [18]. For all-ceramic restorations, excessive wear of opposing enamel is another concern for the dental practitioner, in addition to its low fracture resistance. Loss of anatomic form caused by wear can alter functions of the masticatory system. Other investigators used wear machines to simulate the chewing movements in the oral environment [6,23–25]. However, there is no evidence to show that in vitro wear testing can predict the amount or pattern of clinical wear of enamel caused by ceramic prostheses.
A 3D Laser-scanner (Willytec GmbH, Gräfelfing, Germany) was used in this study. It can be used to measure wear on replicas to an accuracy of ± 20 μm. Generally, the scanner [26–28] uses a laser beam that is projected through a special optic system onto the surface being studied. For the instrument used in this study, the reflection of the beam is observed at an angle of 25° by a high resolution CCD camera based on the principle of the light-slit microscope. After scanning, it allows 3-D superimposition of images using at least three reference points or areas and quantifies the spatial differences between the two images. This machine also allows measurement of wear in three dimensions, thereby giving a more realistic view of the clinical characteristics of wear and the potential mechanisms involved.
The mean volumes of enamel wear obtained from this study were 0.21 ± 0.06 mm3 for premolar teeth and 0.50 ± 0.22 mm3 for molar teeth after one year. These values were not significantly higher than the enamel wear of the contralateral teeth (p>0.05). This indicates a comparable wear rate between opposing enamel and the controls after one year. Although the results from this study indicate that these ceramic crowns did not cause significant wear of the opposing enamel after one year, these data must be verified with the results obtained from the two-year recall examination.
The mean occlusal wear volume of ceramic crowns was lower than that of the tooth enamel, especially for the molar site. Hot-pressed ceramic core material used in this study was based on the lithia-disilicate composition. The veneering material that opposed the enamel was glass-based with fracture toughness of 0.7 ± 0.1 MPa m1/2 and hardness of 5.3 GPa [29]. The fracture toughness of tooth enamel is 0.77 MPa m1/2 and the hardness is 3.23 GPa [12]. The fracture toughness values of veneering material and tooth enamel were comparable, but surface hardness of the veneering material was higher. Higher hardness suggests a greater resistance to surface scratching or damage caused by other restorative materials. However, hardness is not the only factor that can affect wear characteristics. It is known that wear of dental materials is associated with several factors, and its mechanisms are not well identified. Therefore, more information regarding results from the long-term clinical study and the material’s properties are required for identifying the relationship between wear volume and associated parameters.
The amount of dental porcelain, castable ceramic and enamel wear obtained from previous in vitro studies varied from 0.03 to 0.6 mm3 after 150,000–300,000 loading cycles [30–32]. In these studies, the authors assumed that 250,000 cycles simulated one year of clinical wear under normal intraoral conditions [31–32]. Applied loads of 13.4 to 30 N at frequency of 4 Hz were used as clinically-relevant parameters. Vertical wear depth and area loss were also used to determine the amount of wear for restorative materials [23, 33–35]. The mean area increase of enamel varied from 0.16 to 0.82 mm2 after 25,000 loading cycles at a load of 40 N [33]. The mean wear depth of enamel ranged from 0.23 to 1.19 mm after 10,000–100,000 loading cycles at a load of 4–40 N [23, 34–35]. The mean wear depths of porcelain varied from 3.7 to 74 μm.
Most of the previous in vitro methods used for wear measurement were performed in two dimensions. The change in height of the tooth structure was measured and the amount of wear was calculated. Those results were quite variable depending on the testing conditions. Also, the loss of vertical height and area reduction cannot be adjusted to determine the three-dimensional wear volume. The anatomy of tooth structure exhibits contours with cusps and grooves. Variations in the shape and size of natural teeth are substantial. Large areas may be associated with a small loss of height or vice versa. This makes comparison between the wear values from these in vitro studies and the values obtained from this study very difficult because of the variability of wear conditions.
To date, there is limited information about enamel or ceramic wear. Few clinical studies for wear determination have been conducted because it is a time-consuming process. However, the data obtained from such clinical trials are extremely useful and readily applicable to the design and development of dental ceramic materials, especially when results from in vitro studies vary depending on the testing conditions. As previously mentioned, wear is a destructive phenomenon associated with patient-related and dentist-related factors. This makes the wear process a very difficult task to simulate or to identify the basis of wear mechanisms. Wear data from the present study can be used for initial analysis but preliminary records and more information are required from future wear studies as a foundation for design and development of well-performing dental ceramics.
Conclusions
The overall clinical performance of hot-pressed ceramic crowns was rated good to excellent after one year. No fracture or secondary carious lesions were observed in this study. Even though fracture was not observed in this study, follow-up of these crowns is necessary for long-term conclusions to be made.
The mean occlusal wear volumes of enamel opposing ceramic were 0.21 ± 0.06 mm3 for premolar teeth and 0.50 ± 0.22 mm3 for molar teeth after 1 year. The mean occlusal wear volumes of ceramic crowns were 0.19 ± 0.06 mm3 for premolar sites and 0.34 ± 0.08 mm3 for molar sites after 1 year. The mean occlusal wear volume of ceramic molar crowns was significantly lower than the enamel wear of the opposing tooth but the mean occlusal wear volume of ceramic premolar crowns was not significantly different from that of opposing enamel.
Statistical analysis showed that there was no significant relationship between the maximum clenching force and the amount of occlusal wear or the mean wear rate of enamel or ceramic assuming a linear model.
Figure 5.
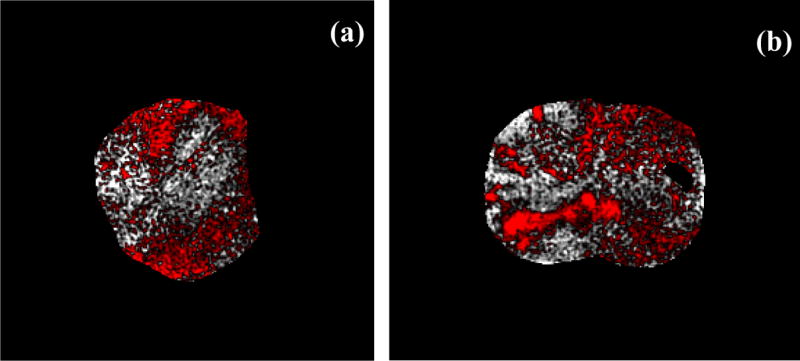
Laser-scan images of ceramic crowns after matching the baseline model with the one-year model of a premolar crown (a) and a molar crown (b). The red area indicates the negative volume or wear volume.
Figure 7.
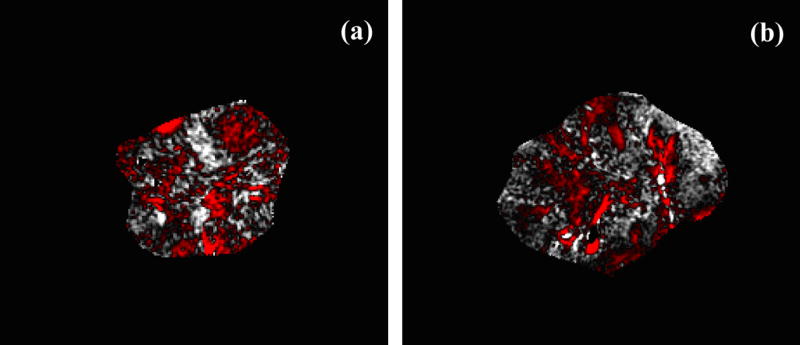
Laser-scan images of opposing teeth after matching between the baseline and one- year models for (a) a premolar tooth and (b) a molar tooth. The red area indicates the negative volume or wear volume.
Acknowledgments
This study was supported by Thailand Research Fund Grant No. MRG 4780066 and NIH-NIDCR Grant DE06672. The authors gratefully acknowledge the help of the following individuals: J. Gatetiean, L. Punya, S. Chamnanpood, and C. Promsrichan.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anusavice KJ, Esquivel-Upshaw J. Less abrasive ceramic esthetic materials. In: Duke ES, editor. The Changing Practice of Restorative Dentistry. Indiana University School of Dentistry, publisher; Indianapolis, IN: 2002. pp. 215–236. [Google Scholar]
- 2.Cattell MJ, Clarke RL, Lynch EJ. The transverse strength, reliability and microstructural features of four dental ceramics- Part I. J Dent. 1997;25:399–407. doi: 10.1016/s0300-5712(96)00058-9. [DOI] [PubMed] [Google Scholar]
- 3.Scherrer SS, De Rijk WG, Belser UC. Fracture resistance of human enamel and three all-ceramic crown systems on extracted teeth. Int J Prosthodont. 1996;9:580–585. [PubMed] [Google Scholar]
- 4.Metzler KT, Woody RD, Miller AW, III, Miller BH. In vitro investigation of the wear of human enamel by dental porcelain. J Prosthet Dent. 1999;81:356–64. doi: 10.1016/s0022-3913(99)70280-5. [DOI] [PubMed] [Google Scholar]
- 5.Al-Hiyasat AS, Saunders WP, Smith GM. Three-body wear associated with three ceramics and enamel. J Prosthet Dent. 1999;82:476–481. doi: 10.1016/s0022-3913(99)70037-5. [DOI] [PubMed] [Google Scholar]
- 6.Seghi RR, Rosenstiel SF, Bauer P. Abrasion of human enamel by different dental ceramics in vitro. J Dent Res. 1991;70(3):221–225. doi: 10.1177/00220345910700031301. [DOI] [PubMed] [Google Scholar]
- 7.Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quintessence Int. 2002;33(7):503–510. [PubMed] [Google Scholar]
- 8.Odman P, Andersson B. Procera AllCeram crowns followed for 5 to 10.5 years: a prospective clinical study. Int J Prosthodont. 2001;14(6):504–509. [PubMed] [Google Scholar]
- 9.Lehner C, Studer S, Brodbeck U, Scharer P. Short-term results of IPS-Empress full-porcelain crowns. J Prosthodont. 1997;6(1):20–30. doi: 10.1111/j.1532-849x.1997.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 10.Segal BS. Retrospective assessment of 546 all-ceramic anterior and posterior crowns in a general practice. J Prosthet Dent. 2001;85(6):544–550. doi: 10.1067/mpr.2001.115180. [DOI] [PubMed] [Google Scholar]
- 11.Haselton DR, Diaz-Arnold AM, Hillis SL. Clinical assessment of high-strength all-ceramic crowns. J Prosthet Dent. 2000;83(4):396–401. doi: 10.1016/s0022-3913(00)70033-3. [DOI] [PubMed] [Google Scholar]
- 12.Coornaert J, Adriaens P, De Boever Long-term clinical study of porcelain-fused-to-gold restorations. J Prosthet Dent. 1984;51:338–342. doi: 10.1016/0022-3913(84)90217-8. [DOI] [PubMed] [Google Scholar]
- 13.Walton TR. An up to 15-year longitudinal study of 515 metal-ceramic FPDs: part 1. outcome. Int J Prosthodont. 2002;15:439–445. [PubMed] [Google Scholar]
- 14.Quinn JB, Sundar V, Lloyd IK. Influence of microstructure and chemistry on the fracture toughness of dental ceramics. Dent Mater. 2003;19:603–611. doi: 10.1016/s0109-5641(03)00002-2. [DOI] [PubMed] [Google Scholar]
- 15.Guazzato M, Albakry M, Ringer SP, Swain MV. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II Zirconia-based dental ceramics. Dent Mater. 2004;20:449–456. doi: 10.1016/j.dental.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Kelly JR, Tesk JA, Sorensen JA. Failure of all-ceramic fixed partial dentures in vitro and in vivo: analysis and modeling. J Dent Res. 1995;74:1253–1258. doi: 10.1177/00220345950740060301. [DOI] [PubMed] [Google Scholar]
- 17.Kelly JR. Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent. 1999;81:652–661. doi: 10.1016/s0022-3913(99)70103-4. [DOI] [PubMed] [Google Scholar]
- 18.Oh W, DeLong R, Anusavice KJ. Factors affecting enamel and ceramic wear: A literature review. J Prosthet Dent. 2002;87:451–459. doi: 10.1067/mpr.2002.123851. [DOI] [PubMed] [Google Scholar]
- 19.Anusavice KJ. Phillips’ science of dental materials. 11. St Louis: W.B. Saunders; 2003. pp. 655–720. [Google Scholar]
- 20.Marquardt P, Strub JR. Survival rate of IPS Empress 2 all-ceramic crowns and fixed partial dentures: Results of a 5-year prospective clinical study. Quintessence Int. 2006;37:253–259. [PubMed] [Google Scholar]
- 21.Fradeani M, Aquilano A. Clinical experience with empress crowns. Int J Prosthodont. 1997;10:241–247. [PubMed] [Google Scholar]
- 22.Gemalmaz D, Ergin S. Clinical evaluation of all-ceramic crowns. J Prosthet Dent. 2002;87(2):189–196. doi: 10.1067/mpr.2002.120653. [DOI] [PubMed] [Google Scholar]
- 23.Ehrnford L, Derand T, Larsson LA, Svensson A. An abrasion test for composite resins. J Dent Res. 1980;59:716–720. doi: 10.1177/00220345800590040801. [DOI] [PubMed] [Google Scholar]
- 24.Hacker C, Wagner W, Razzoog M. An in vitro investigation of the wear of enamel on porcelain and gold in saliva. J Prosthet Dent. 1996;75:14–17. doi: 10.1016/s0022-3913(96)90412-6. [DOI] [PubMed] [Google Scholar]
- 25.Al-Hiyasat AS, Saunders WP, Sharkey S, Smith G, Gilmour WH. The abrasive effect of glazed, unglazed, and polished porcelain on the wear of human enamel, and the influence of carbonated soft drinks on the rate of wear. Int J Prosthodont. 1997;10:269–282. [PubMed] [Google Scholar]
- 26.Perry R, Kugel G, Kunzelmann K-H, Flessa H, Estafan D. Composite restoration wear analysis: Conventional methods vs. three-dimensional laser digitizer. J Am Dent Assoc. 2000;131:1472–1477. doi: 10.14219/jada.archive.2000.0060. [DOI] [PubMed] [Google Scholar]
- 27.Mehl A, Gloger W, Kunzelmann K-H, Hickel R. A new optical 3-D device for the detection of wear. J Dent Res. 1997;76:1799–1807. doi: 10.1177/00220345970760111201. [DOI] [PubMed] [Google Scholar]
- 28.Folwaczny M, Mehl A, Kunzelmann KH, Hickel R. Determination of changes on tooth-colored cervical restorations in vivo using a three-dimensional laser scanning device. Eur J Oral Sci. 2000;108:233–238. doi: 10.1034/j.1600-0722.2000.108003233.x. [DOI] [PubMed] [Google Scholar]
- 29.Della Bona A. Interfacial adhesion of dental, ceramic-resin systems. Dissertation, University of Florida; Gainesville, FL: 2001. [Google Scholar]
- 30.Palmer DS, Barco MT, Pelleu GB, McKinney JE. Wear of human enamel against a commercial castable restorative material. J Prosthet Dent. 1991;65:192–195. doi: 10.1016/0022-3913(91)90161-o. [DOI] [PubMed] [Google Scholar]
- 31.DeLong R, Pintado MR, Douglas WH. The wear of enamel opposing shaded ceramic restorative materials: An in vitro study. J Prosthet Dent. 1992;68:42–48. doi: 10.1016/0022-3913(92)90282-f. [DOI] [PubMed] [Google Scholar]
- 32.Magne P, Oh WS, Pintado MR, DeLong R. Wear of enamel and veneering ceramics after laboratory and chairside finishing procedures. J Prosthet Dent. 1999;82:669–679. doi: 10.1016/s0022-3913(99)70008-9. [DOI] [PubMed] [Google Scholar]
- 33.Ratledge DK, Smith BG, Wilson RF. The effects of restorative materials on the wear of human enamel. J Prosthet Dent. 1994;72:194–203. doi: 10.1016/0022-3913(94)90080-9. [DOI] [PubMed] [Google Scholar]
- 34.Al-Hiyasat AS, Saunders WP, Sharkey S, Smith G, Gilmour WH. Investigation of human enamel wear against four dental ceramics and gold. J Dent. 1998;26:487–95. doi: 10.1016/s0300-5712(97)00041-9. [DOI] [PubMed] [Google Scholar]
- 35.Al-Hiyasat AS, Saunders WP, Sharkey S, Smith G, Gilmour WH. The abrasive effect of glazed, unglazed, and polished porcelain on the wear of human enamel, and the influence of carbonated soft drinks on the rate of wear. Int J Prosthodont. 1997;10:269–282. [PubMed] [Google Scholar]