Abstract
Background
AMPK is a promising pharmacological target in relation to metabolic disorders partly due to its non-insulin dependent glucose uptake promoting role in skeletal muscle. Of the 2 catalytic α-AMPK isoforms, α2 AMPK is clearly required for stimulation of glucose transport into muscle by certain stimuli. In contrast, no clear function has yet been determined for α1 AMPK in skeletal muscle, possibly due to α-AMPK isoform signaling redundancy. By applying low-intensity twitch-contraction and H2O2 stimulation to activate α1 AMPK, but not α2 AMPK, in wildtype and α-AMPK transgenic mouse muscles, this study aimed to define conditions where α1 AMPK is required to increase muscle glucose uptake.
Methodology/Principal Findings
Following stimulation with H2O2 (3 mM, 20 min) or twitch-contraction (0.1 ms pulse, 2 Hz, 2 min), signaling and 2-deoxyglucose uptake were measured in incubated soleus muscles from wildtype and muscle-specific kinase-dead AMPK (KD), α1 AMPK knockout or α2 AMPK knockout mice. H2O2 increased the activity of both α1 and α2 AMPK in addition to Akt phosphorylation, and H2O2-stimulated glucose uptake was not reduced in any of the AMPK transgenic mouse models compared with wild type. In contrast, twitch-contraction increased the activity of α1 AMPK, but not α2 AMPK activity nor Akt or AS160 phosphorylation. Glucose uptake was markedly lower in α1 AMPK knockout and KD AMPK muscles, but not in α2 AMPK knockout muscles, following twitch stimulation.
Conclusions/Significance
These results provide strong genetic evidence that α1 AMPK, but not α2 AMPK, Akt or AS160, is necessary for regulation of twitch-contraction stimulated glucose uptake. To our knowledge, this is the first report to show a major and essential role of α1 AMPK in regulating a physiological endpoint in skeletal muscle. In contrast, AMPK is not essential for H2O2-stimulated muscle glucose uptake, as proposed by recent studies.
Introduction
AMP activated protein kinase (AMPK) is emerging as an attractive target in both prophylaxis and treatment of metabolic disorders, including obesity and type 2 diabetes[1]. Key to its beneficial effects, AMPK promotes GLUT4 translocation and glucose uptake into skeletal muscle by a signaling cascade independent of the classical insulin-signaling cascade through PI3K-Akt[1].
Using AMPK signaling-deficient transgenic mouse models, various research groups have demonstrated that the skeletal muscle enriched catalytic α2 AMPK isoform is necessary to increase glucose uptake into skeletal muscle with certain stimuli, including 5-aminoimidazole-4-carboxamide ribonucleoside (AICAR), hypoxia and metabolic uncoupling[2]–[4]. Furthermore, both α2 AMPK and Akt signaling phosphorylate the Rab-GAP protein AS160, a probable regulator of GLUT4 translocation during contraction and insulin-stimulation[5], [6]. Together with studies showing α1 AMPK activation without an increase in glucose uptake during AICAR-stimulation in α2 AMPK knockout muscle (KO)[3], [7], [8], this suggests that α1 AMPK does not regulate glucose uptake.
Meanwhile, recent studies in incubated rat muscles have challenged the sovereignty of α2 AMPK in stimulating glucose uptake by demonstrating that the increase in glucose uptake elicited by hydrogen peroxide (H2O2) and low-intensity short-duration twitch-contraction is paralleled by an increase in α1 AMPK activity but not α2 AMPK activity[9], [10]. This paradigm was supported by another report in incubated mouse muscle, where H2O2-stimulated AMPK activation and glucose uptake coincided[11]. Reminiscent of Twitch/H2O2-stimulation, an α1 AMPK-exclusive activation profile was found in mouse soleus muscle stimulated with the sarcoplasmic reticulum (SR) Ca2+-releasing agent, caffeine[12]. Importantly, kinase-dead (KD) AMPK expression inhibited caffeine-stimulated glucose uptake[12]. However, the KD AMPK transgenic model reduces both α1 and α2 AMPK activity[13] and does not allow conclusions to be drawn about the relative importance of these to glucose uptake regulation. Therefore, whether increasing α1 AMPK activity, pharmacologically or by transcutaneous neuromuscular stimulation as suggested recently[14], can actually improve glucose homeostasis remains controversial as the studies above did not establish a causal relationship between α1 AMPK activation and glucose uptake.
Because both H2O2-stimulation and short-duration twitch-contraction appeared useful to activate α1 AMPK without activating α2 AMPK[9], [10], these stimuli were applied to incubated wildtype, α1 AMPK KO, α2 AMPK KO and kinase-dead (KD) AMPK muscles to answer whether alpha1 AMPK is necessary to increase glucose uptake in these conditions. Our data provides genetic evidence that α1 AMPK, but not α2 AMPK, Akt or AS160, is required for twitch-contraction stimulated glucose uptake. On the other hand, AMPK does not appear essential for H2O2-stimulated muscle glucose uptake, as proposed by recent studies.
Results
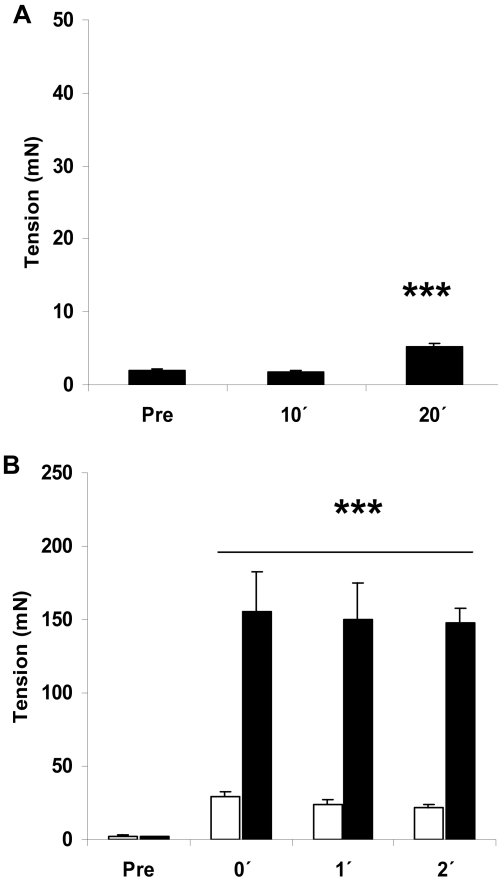
Initial characterization of twitch-contraction and H2O2-stimulated tension-development and signaling
H2O2-stimulation (3 mM) did not affect resting tension for the first 10 min, but slightly increased tension development from 10 to 20 min of stimulation (Figure 1A). Force-production during twitch-contraction reached an initial peak level around 30 mN and remained constant throughout the 2 min stimulation period (Figure 1B). Note that the peak force during the twitch-protocol is around 1/5 of the peak force observed during tetanic contraction of mouse soleus muscle (also shown in Figure 1B for comparison), emphasizing the difference between this and the more commonly used tetanic stimulation protocols [3], [15], [16].
Figure 1. Tension-measurements.
Tension-development during A) H2O2 stimulation (3 mM, 20 min) and B) twitch (white bars: 0.1 ms, 2 Hz, 2 min) and tetanic (black bars: 0.2 ms, 100 Hz, 1s/15s, 2 min) stimulation in mouse soleus muscles (n = 5–8). *** p<0.001 vs. pre.
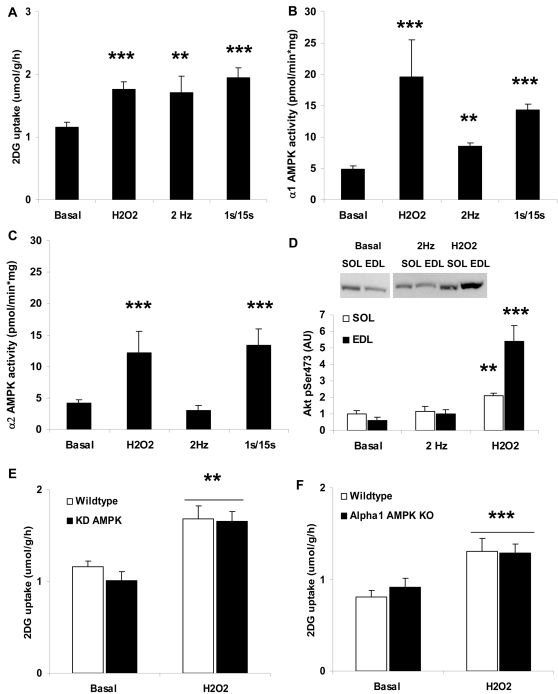
Both 3 mM H2O2 for 20 min or twitch-contraction for 2 min increased glucose uptake to a similar extent as mild tetanic contraction for 10 min in incubated mouse soleus (Figure 2A). While twitch-contraction stimulated only α1 AMPK activity, H2O2 increased both α1 and α2 AMPK activities (Figure 2B and 2C). As has been demonstrated in rat epitroclearis muscle [10], prolonging 2Hz-stimulation to 5 min caused a significant increase in both α1 and α2 AMPK activity in mouse soleus muscle, making this time point useless to isolate α1 AMPK activation (α1 AMPK activity basal: 1.7 2 Hz, 5 min: 2.9, p = 0.008 α2 AMPK activity basal: 1.3 2 Hz, 5 min: 2.1, p = 0.013, n = 7). Previously, H2O2 has been shown to cause activation of many proteins in skeletal muscle, including Akt[17]. In our hands, H2O2, but not twitch-contraction, elicited a significantly ∼1 fold higher Akt phosphorylation in soleus (Figure 2D). To directly compare with the paper by Sandström and colleagues[11], we also measured H2O2-stimulated Akt phosphorylation in Extensor Digitorum Longus (EDL) muscles which was ∼4–5 fold higher compared with basal (Figure 2D). H2O2 stimulation of glucose uptake did not differ between wild type and either α1 AMPK KO (Figure 2E) or KD AMPK muscles (Figure 2F). Together, these results show that H2O2 stimulation of glucose uptake in muscle does not require AMPK catalytic activity and activates at least one other candidate glucose uptake promoting protein.
Figure 2. H2O2 and twitch-contraction stimulated 2-deoxyglucose (2DG) uptake and signaling in mouse soleus muscle.
A) 2DG uptake in basal vs. H2O2 (3 mM, 20 min), twitch contraction (0.1 ms, 2 Hz, 2 min) or tetanic contraction (0.2 ms, 100 Hz, 1s/15s, 10 min)-stimulated muscles (n = 5–12). B) α1 AMPK and C) α2 AMPK activities in basal vs. H2O2 with same conditions as in panel A (n = 6–16). D) Akt Ser473 phosphorylation in basal, twitch-contracted and H2O2-stimulated soleus and EDL muscles (n = 6). E) H2O2-stimulated 2DG uptake in wildtype vs. kinase-dead (KD) AMPK muscles (n = 5–6) and F) wildtype vs. α1 AMPK KO muscles (n = 8). **/*** p<0.01/0.001 vs. basal.
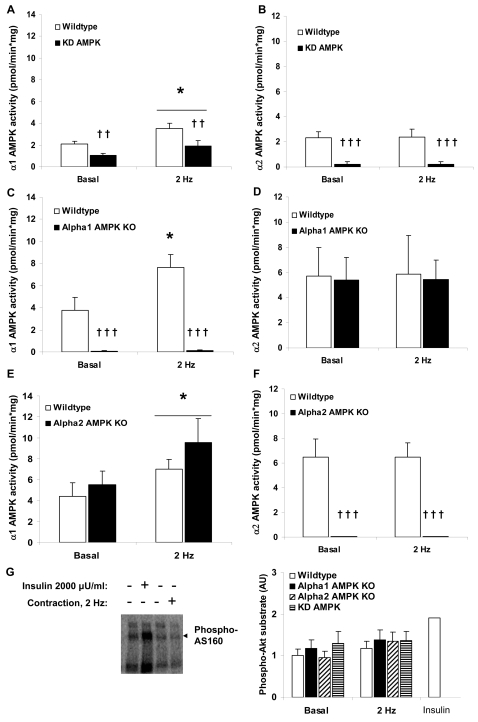
Signaling following twitch contraction in AMPK transgenic mice
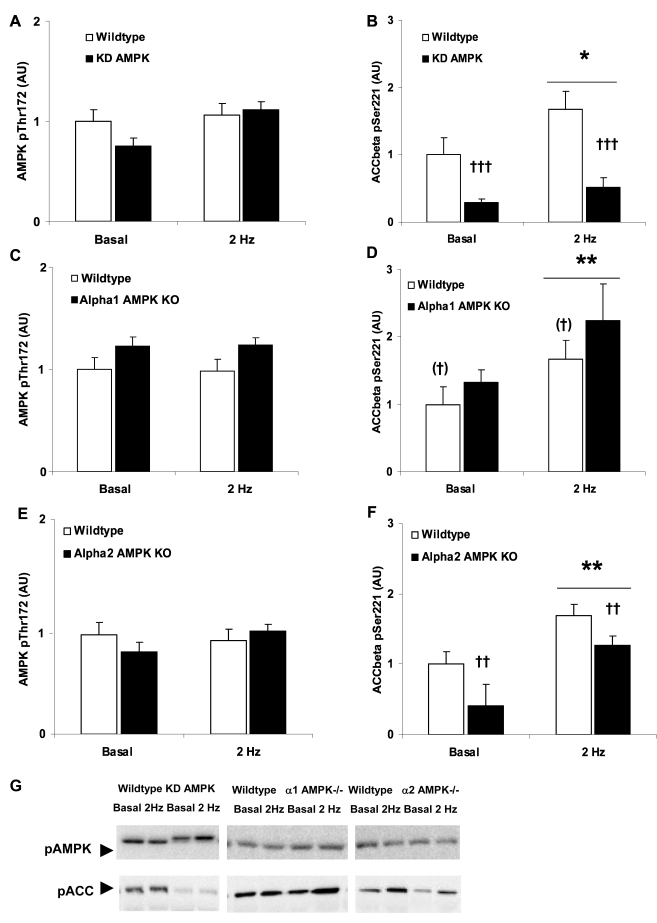
Twitch-contraction increased α1 AMPK activity, but not α2 AMPK activity in wildtype muscles (Figure 3). α1 AMPK activity was ∼50% lower in KD AMPK muscles and absent in α1 AMPK KO muscles, while α2 AMPK activity was nearly absent in KD AMPK muscles and non-detectable in α2 AMPK KO (Figure 3A–3F). No compensatory increase in α2 AMPK activity was detected during twitch-contraction in the α1 AMPK KO muscles (Figure 3D) while the α2 AMPK KO muscles tended to display higher mean levels of basal and twitch-stimulated α1 AMPK activity (Figure 3E). Since neither α2 AMPK nor Akt (Figure 3D) appeared to be activated by the protocol currently employed, we asked whether AS160 phosphorylation, a point of convergence of α2 AMPK and Akt signaling to glucose uptake[6], was different from basal. AS160 phosphorylation was ∼100% higher with insulin-treatment but did not differ between twitch contraction-treated muscles and non-contracted muscles (Figure 3G). Thus, the increase in glucose uptake with twitch-contraction presumably cannot be explained by increased AS160 phosphorylation. No increases in AMPK Thr172 phosphorylation were detected in twitch contraction-stimulated wildtype or AMPK transgenic muscles despite significant increases in ACCβ Ser221 phosphorylation (Fig 4). This supports our previous observation in incubated mouse soleus muscles following sub-contraction threshold caffeine-stimulation, another α1 AMPK-specific stimulus, which likewise does not cause a significant increase in AMPK Thr172 phosphorylation, despite increasing ACCβ Ser221 phosphorylation [12].
Figure 3. Twitch-contraction (0.1 ms, 2 Hz, 2 min) signaling in AMPK transgenic soleus muscles.
A) α1 AMPK and B) α2 AMPK activities in wildtype vs. kinase-dead (KD) AMPK muscles (n = 7–8), C ) α1 AMPK and D) α2 AMPK activities in wildtype vs. α1 AMPK KO muscles (n = 7–10), E ) α1 AMPK and F) α2 AMPK activities E) and F) wildtype vs. α2 AMPK (n = 10). G) Basal and twitch-stimulated AS160 phosphorylation in wildtype vs. AMPK transgenic muscles (n = 6–9). As a positive control, insulin-stimulated (2000 µU/ml, 15 min) soleus was included (n = 1). * p<0.05 vs. basal. ††/††† p<0.01/0.001 genotype main effect.
Figure 4. Twitch-stimulated (0.1 ms, 2 Hz, 2 min) AMPK and ACCβ phosphorylation in mouse soleus muscles.
AMPK Thr172 phosphorylation in. A) wildtype vs. kinase-dead (KD) AMPK muscles (n = 7–8), C) wildtype vs. α1 AMPK KO muscles (n = 9–10) E) wildtype vs. α2 AMPK KO muscles (n = 10). ACCβ Ser221 phosphorylation in B) wildtype vs. kinase-dead (KD) AMPK muscles (n = 7–8), D) wildtype vs. α1 AMPK KO muscles (n = 9–10) F) wildtype vs. α2 AMPK KO muscles (n = 10). */** p<0.05/0.01 vs. basal. ††/††† p<0.01/0.001 genotype-effect. (†) indicates borderline significant genotype-effect, p = 0.06. G) Representative blots
α1 AMPK is required for twitch-contraction stimulated glucose uptake
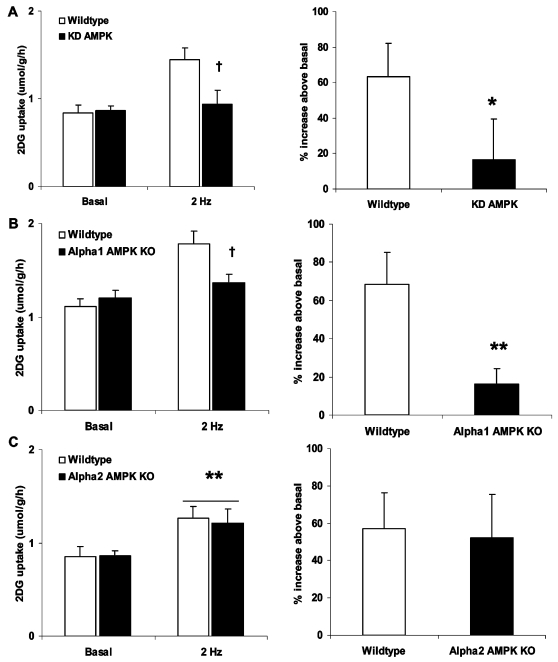
Twitch-contraction elicited a ∼60% increase in glucose uptake above basal in wildtype muscles (Figure 5). The corresponding increases were lower than 20% above basal in both the KD AMPK (Figure 5A) and α1 AMPK KO muscles (Figure 5B), but similar to wildtype in muscles lacking α2 AMPK (Figure 5C). This suggests that α1 AMPK is a required signaling component to glucose uptake stimulation during the low-intensity twitch-contraction regimen.
Figure 5. Twitch-contraction requires α1 AMPK to stimulate glucose uptake.
Twitch contraction (0.1 ms, 2 Hz, 2 min) stimulated 2-deoxyglucose in mouse soleus muscles from either A) wildtype vs. kinase-dead AMPK muscles (n = 10–13) B) wildtype vs. α1 AMPK KO muscles (n = 16–17) C) wildtype vs. α2 AMPK KO muscles (n = 11–12). Absolute values are shown on the left and the corresponding percentage increase above basal for paired muscles is shown on the right. */** p<0.05/0.01 vs. wildtype or basal, † genotype x contraction p<0.05.
Discussion
Stimulation of glucose uptake ex vivo by either H2O2 or twitch-contraction has been proposed to require α1 AMPK, based on correlations between α1 AMPK activity and glucose uptake in isolated rat epitroclearis muscle[9], [10]. This study provides the first clear genetic evidence for a causal link between α1 AMPK and glucose uptake-regulation following twitch-contractions. In contrast, H2O2-stimulated glucose uptake was not affected by reductions in AMPK activity.
To our knowledge, this is the first report of a metabolic regulatory role of α1 AMPK in skeletal muscle. Likely, the key to observing a major role of α1 AMPK in glucose uptake-regulation lies in the use of the low intensity, short duration contraction-regimen, which failed to increase α2 AMPK activity. In a previous study, glucose uptake ex vivo was only ∼20% lower in α1 AMPK KO soleus muscles compared to wildtype following intense tetanic ex vivo contraction (3). We speculate that intense tetanic contraction, like H2O2, activates other potential stimulators of glucose uptake, including Akt[18] and α2 AMPK[3], [13], which may have compensated for lack of α1 AMPK in that study.
A glucose uptake-promoting role of α1 AMPK is not unprecedented. In the rat liver epithelial clone9 cell line, α1 AMPK has thus been shown to be both necessary and sufficient to elicit an increased GLUT1-dependent glucose uptake, possibly due to movement out of detergent-resistant lipid rafts in the plasma membrane [19]–[24]. In skeletal muscle, GLUT4 is no doubt the major insulin and contraction-responsive glucose transporter isoform [25]–[27]. Still, GLUT4 KO mice retain some ability to increase glucose uptake in response to insulin and contraction into isolated muscles. Therefore, although speculative, it is possible that α1 AMPK targets GLUT1 or another non-GLUT4 glucose transporter expressed in skeletal muscle.
The twitch-contraction data support our previous findings, that caffeine-stimulated glucose uptake into mouse soleus muscle is AMPK-dependent[12]. Like twitch-contraction, caffeine-stimulated sarcoplasmic reticulum Ca2+-release activates α1 AMPK and phospho-ACC, but not α2 AMPK or phospho-AMPK, suggesting that the two stimuli are working through the same Ca2+-dependent pathway, proposed to involve the putative muscle-AMPK kinase, CaMKK[12]. A possible link between Ca2+-release by caffeine and AMPK activation is supported by another recent report using perfused rat hindlimb [28]. However, as discussed in a previous paper [12], any change in Ca2+ will perturb energy balance and potentially increase AMP/ATP-ratio. Whether the AMPK activation by caffeine is indeed Ca2+ dependent or can be explained by low-level changes in nucleotides [12] needs careful examination. Regardless, both α1 and α2 AMPK activities increase during in vivo exercise in mice[3] suggesting a physiological signaling role for both isoforms. Also, α1 AMPK expression and activity is increased compared to wildtype in both the whole-body α2 AMPK knockout mice[3] and in mice with muscle-specific deletion of the muscle-AMPK kinase, LKB1[8], further suggesting a compensatory role of α1 AMPK. However, as discussed previously[12], although α1 AMPK amount increases with exercise training[29], its activation during exercise is rarely observed in exercising human quadriceps-muscle. Still, it is conceivable that human muscles other than the principal biopsy-sampling muscle, quadriceps, more readily activate α1 AMPK during contraction. An exercise-study taking biopsies from the human soleus muscle, a method experimentally feasible [30], will be needed to resolve this question.
α1 AMPK activity was only reduced by ∼50% in the KD AMPK muscles yet glucose uptake stimulation by twitch-contraction was largely prevented. However, it has been proposed that residual α1 AMPK activity in the KD AMPK mice and a similar model, the muscle-specific α2i mice, may largely stem from non-muscle tissue present in muscle[2], [4], [13]. Therefore, the partial reduction in α1 AMPK activity could reflect a near-total reduction in muscle α1 AMPK activity. Other possibilities are that KD AMPK expression lowers α1 AMPK activity below a threshold required to increase glucose uptake or that KD AMPK expression affects α1 AMPK location and/or function by degrading α2 AMPK and AMPK-regulatory subunits. A similar paradox is that AICAR-stimulated glucose uptake is abolished in α2 AMPK KO muscles, despite α1 AMPK activity increasing[3]. Together with the current data, one straight-forward interpretation is that α1 AMPK provides a necessary, but not sufficient, signal to increase glucose uptake.
H2O2, working through AMPK, has been proposed to be involved in contraction-stimulated glucose uptake[9], [11]. In other studies, H2O2 concentrations below ∼1 mM do not seem to stimulate glucose uptake[31], [32], but may inhibit insulin-stimulated glucose uptake[31], while higher H2O2 concentrations increase glucose uptake in various muscle model-systems[9], [11]. The physiological range for H2O2 has been reported to be in the range of ∼30–150 µM[33]. Therefore, using mM concentrations to increase glucose uptake is likely not physiologically meaningful and should not be interpreted in this context. Apart from AMPK, H2O2 concentrations ranging from 60 µM-3 mM activate many signaling proteins, including MAPKs[31], [34], insulin receptor, IRS-1 and Akt[17], [31][and present study]. Possible activation mechanisms include reversible inactivation of phosphatases or activation of kinases by cysteine oxidation[35] and increased intracellular Ca2+ due to increased Ca2+-leak[36] and/or decreased uptake into the SR[33]. Furthermore, our finding of a minor increase in resting tension during H2O2 incubation, likely due to increased intracellular Ca2+ and/or increased myofibrillar Ca2+-sensitivity[33], opens up the possibility of metabolism and/or stretch-dependent signaling mechanisms. Based on the above and our studies, we strongly question the specificity and therefore usefulness of H2O2 in characterizing the relative contribution of AMPK or other signaling-molecules to contraction-stimulated glucose uptake. Furthermore, while this study was under revision, it was demonstrated in isolated rat EDL that 600 µM H2O2 potently activated Akt, but not AMPK, and glucose uptake in a wortmannin-sensitive manner [37], lending further support to the non-AMPK dependence of H2O2-stimulated glucose uptake.
Due to breeding difficulties, the α1 AMPK KO strain is currently being backcrossed from the C57BL/6 to the 129/SV mouse strain, and was 4th to 5th generation backcrossed at the time of experimentation (4th generation theoretically 93.75% 129/SV and 6.25% C57BL/6). Genetic background is known to strongly influence effect sizes of various measuring endpoints (see [12] for discussion and references). However, our finding of reduced glucose uptake in both the C57BL/6 KD AMPK mice and the predominantly 129/SV α1 AMPK KO mice, suggests that the dependence of twitch-stimulated glucose uptake on α1 AMPK is not strain-specific.
The band detected by the PAS antibody in mouse soleus muscle is AS160 [38]. Unlike recent studies showing that signaling through AS160 is required for glucose uptake stimulation in adipocytes and muscle[39], twitch-contraction defines a condition where AS160 phosphorylation apparently does not correlate with glucose uptake. This suggests that α1 AMPK, unlike Akt and α2 AMPK[5], [6], is not an AS160-kinase. However, AS160 phosphorylation evaluated with the PAS antibody was recently shown to reflect mostly Thr642 phosphorylation[40]. Therefore, it remains possible that twitch-contraction targets other of the 8 identified AS160 phosphorylation sites[40]. Another possibility is that the change in AS160 phosphorylation measured with PAS following twitch-contraction was below the detection limit.
In conclusion, the present study 1) demonstrates that α1 AMPK activation is necessary to increase muscle glucose uptake following twitch-contraction and 2) provides the first genetic evidence for an essential role of α1 AMPK in contraction-stimulated skeletal muscle glucose uptake. In contrast, H2O2 is not an AMPK-specific stimulus.
Materials and Methods
Animals
Generation of the α1 and α2 AMPK whole-body KO as well as the muscle-specific KD α2 AMPK mice has been described previously [3], [4], [41]. The α1 AMPK KO mice were mixed males and females from 4th and 5th generation backcross of C57Bl/6 onto 129/SV-background. The α2 AMPK KO mice were fully backcrossed (>10th generation) C57Bl/6 males. The KD AMPK mice were mixed males and females from 6th and 7th generation backcross of C57Bl/6 onto C57Bl/6. In all cases, sex and age-matched wild type littermates were used as controls. Female C57Bl/6 mice were used for all other experiments in this study. All mice were 12–18 wks old, when experiments were performed. Experiments were approved by the Danish Animal Experimental Inspectorate and complied with the “European Convention for the Protection of Vertebrate Animals Used for Experiments and Other Scientific Purposes”.
Muscle incubation
Soleus or EDL muscles were obtained from fed anesthetized mice (6 mg of pentobarbital 100 g−1 body weight) and suspended at resting tension (4–5 mN) in incubation-chambers (Multi Myograph system; Danish Myo-Technology, Aarhus, DK) in Krebs-Ringer-Henseleit buffer (KRH) supplemented with 2 mM pyruvate and 8 mM mannitol at 30°C [3]. Muscles were preincubated for 1 h before measuring glucose uptake or signaling. H2O2 (3 mM) in KRH-buffer was added for the last 20 min. Muscle contraction was elicited by electrical stimulation with either 0.1 ms pulses at 2 Hz (∼50 V) for the last 2 or 5 min (termed twitch-contraction throughout this paper) or 1 s trains (0.2 ms, 100 Hz) every 15s for the last 10 min. Force development was measured during all incubations by a force transducer hooked to one end of the muscles.
2-Deoxyglucose Uptake
Following stimulation, glucose uptake was evaluated by measuring accumulation of 3H-labelled 2-deoxyglucose for 10 min, with 14C Mannitol as extracellular space marker[3].
Muscle Analyses
Basal or stimulated muscles were quick-frozen by immersion in liquid nitrogen and processed into lysates[13]. Lysates were subjected to standard immunoblotting techniques[13], using the following phospho-specific antibodies: AMPK Thr172 (Cell Signaling Technology, MA), ACCβ Ser221 (Upstate Biotechnologies, MA), Akt Ser473 (Cell Signaling Technology), and phospho-Akt substrate motif RXRXXS/T (PAS) (Cell Signaling Technology) recognizing phospho-AS160[6].
α1 and α2 AMPK Activity
Isoform-specific α-AMPK activity was measured in vitro in sequential immunoprecipitations from 200 µg of muscle lysate protein using anti-α1 and anti-α2 antibodies using AMARA peptide[13].
Statistical analysis
Results are mean±SEM. Statistical testing was performed using unpaired t-tests or ANOVA with Tukey's honest significant difference post hoc test. An underlined symbol denotes bars that meet the criteria represented by that symbol. Statistical evaluation was performed using SPSS 15.0 for Windows. The significance level was set at α = 0.05.
Acknowledgments
We thank Grahame Hardie (Division of Molecular Physiology, University of Dundee, Dundee, Scotland) and Morris J. Birnbaum (Howard Hughes Medical Institute and The Department of Medicine, University of Pennsylvania School of Medicine, Philadelphia, PA) for providing antibodies and transgenic mice essential to this study.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The study was supported by the Novo Nordisk Research Foundation, The Danish Diabetes Association, an Integrated Project (LSHM-CT-2004-005272) funded by the European Commission, The Lundbeck Foundation, The Copenhagen Muscle Research Centre and The Danish Medical and Natural Sciences Research Councils. Jørgen F. P. Wojtaszewski was supported by a Hallas Møller Fellowship from The Novo Nordisk Foundation.
References
- 1.Kahn BB, Alquier T, Carling D, Hardie DG. AMP-activated protein kinase: Ancient energy gauge provides clues to modern understanding of metabolism. Cell Metabolism. 2005;1:15–25. doi: 10.1016/j.cmet.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Fujii N, Hirshman MF, Kane EM, Ho RC, Peter LE, et al. AMP-activated Protein Kinase {alpha}2 Activity Is Not Essential for Contraction- and Hyperosmolarity-induced Glucose Transport in Skeletal Muscle. J Biol Chem. 2005;280:39033–39041. doi: 10.1074/jbc.M504208200. [DOI] [PubMed] [Google Scholar]
- 3.Jørgensen SB, Viollet B, Andreelli F, Frosig C, Birk JB, et al. Knockout of the alpha2 but Not alpha1 5′-AMP-activated Protein Kinase Isoform Abolishes 5-Aminoimidazole-4-carboxamide-1-beta-4-ribofuranosidebut Not Contraction-induced Glucose Uptake in Skeletal Muscle. J Biol Chem. 2004;279:1070–1079. doi: 10.1074/jbc.M306205200. [DOI] [PubMed] [Google Scholar]
- 4.Mu J, Brozinick JT, Jr., Valladares O, Bucan M, Birnbaum MJ. A role for AMP-activated protein kinase in contraction- and hypoxia-regulated glucose transport in skeletal muscle. Mol Cell. 2001;7:1085–1094. doi: 10.1016/s1097-2765(01)00251-9. [DOI] [PubMed] [Google Scholar]
- 5.Kramer HF, Witczak CA, Fujii N, Jessen N, Taylor EB, et al. Distinct Signals Regulate AS160 Phosphorylation in Response to Insulin, AICAR, and Contraction in Mouse Skeletal Muscle. Diabetes. 2006;55:2067–2076. doi: 10.2337/db06-0150. [DOI] [PubMed] [Google Scholar]
- 6.Treebak JT, Glund S, Deshmukh A, Klein DK, Long YC, et al. AMPK-mediated AS160 phosphorylation in skeletal muscle is dependent on AMPK catalytic and regulatory subunits. Diabetes. 2006;55:2051–2058. doi: 10.2337/db06-0175. [DOI] [PubMed] [Google Scholar]
- 7.Koh HJ, Arnolds DE, Fujii N, Tran TT, Rogers MJ, et al. Skeletal Muscle-Selective Knockout of LKB1 Increases Insulin Sensitivity, Improves Glucose Homeostasis, and Decreases TRB3. Mol Cell Biol. 2006;26:8217–8227. doi: 10.1128/MCB.00979-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sakamoto K, McCarthy A, Smith D, Green KA, Grahame HD, et al. Deficiency of LKB1 in skeletal muscle prevents AMPK activation and glucose uptake during contraction. EMBO J. 2005;24:1810–1820. doi: 10.1038/sj.emboj.7600667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toyoda T, Hayashi T, Miyamoto L, Yonemitsu S, Nakano M, et al. Possible involvement of the alpha1 isoform of 5′AMP-activated protein kinase in oxidative stress-stimulated glucose transport in skeletal muscle. Am J Physiol Endocrinol Metab. 2004;287:E166–E173. doi: 10.1152/ajpendo.00487.2003. [DOI] [PubMed] [Google Scholar]
- 10.Toyoda T, Tanaka S, Ebihara K, Masuzaki H, Hosoda K, et al. Low-intensity contraction activates the {alpha}1-isoform of 5′-AMP-activated protein kinase in rat skeletal muscle. Am J Physiol Endocrinol Metab. 2006;290:E583–E590. doi: 10.1152/ajpendo.00395.2005. [DOI] [PubMed] [Google Scholar]
- 11.Sandstrom ME, Zhang SJ, Bruton J, Silva JP, Reid MB, et al. Role of reactive oxygen species in contraction-mediated glucose transport in mouse skeletal muscle. J Physiol (Lond) 2006;575:251–262. doi: 10.1113/jphysiol.2006.110601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jensen TE, Rose AJ, Hellsten Y, Wojtaszewski JF, Richter EA. Caffeine-induced Ca2+ release increases AMPK-dependent glucose uptake in rodent soleus muscle. Am J Physiol Endocrinol Metab. 2007;293:E286–E292. doi: 10.1152/ajpendo.00693.2006. [DOI] [PubMed] [Google Scholar]
- 13.Jensen TE, Rose AJ, Jorgensen SB, Brandt N, Schjerling P, et al. Possible CaMKK-dependent regulation of AMPK phosphorylation and glucose uptake at the onset of mild tetanic skeletal muscle contraction. Am J Physiol Endocrinol Metab. 2007;292:E1308–E1317. doi: 10.1152/ajpendo.00456.2006. [DOI] [PubMed] [Google Scholar]
- 14.Putman CT, Martins KJB, Gallo ME, Lopaschuk GD, Pearcey JA, et al. {alpha}-Catalytic subunits of 5′AMP-activated protein kinase display fiber-specific expression and are upregulated by chronic low-frequency stimulation in rat muscle. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1325–R1334. doi: 10.1152/ajpregu.00609.2006. [DOI] [PubMed] [Google Scholar]
- 15.Wright DC, Hucker KA, Holloszy JO, Han DH. Ca2+ and AMPK Both Mediate Stimulation of Glucose Transport by Muscle Contractions. Diabetes. 2004;53:330–335. doi: 10.2337/diabetes.53.2.330. [DOI] [PubMed] [Google Scholar]
- 16.Fujii N, Hirshman MF, Kane EM, Ho RC, Peter LE, et al. AMP-activated protein kinase alpha2 activity is not essential for contraction-and hyperosmolarity-induced glucose transport in skeletal muscle. J Biol Chem. 2005 doi: 10.1074/jbc.M504208200. [DOI] [PubMed] [Google Scholar]
- 17.Kim JS, Saengsirisuwan V, Sloniger JA, Teachey MK, Henriksen EJ. Oxidant stress and skeletal muscle glucose transport: roles of insulin signaling and p38 MAPK. Free Radic Biol Med. 2006;41:818–824. doi: 10.1016/j.freeradbiomed.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 18.Sakamoto K, Hirshman MF, Aschenbach WG, Goodyear LJ. Contraction Regulation of Akt in Rat Skeletal Muscle. J Biol Chem. 2002;277:11910–11917. doi: 10.1074/jbc.M112410200. [DOI] [PubMed] [Google Scholar]
- 19.Abbud W, Habinowski S, Zhang JZ, Kendrew J, Elkairi FS, et al. Stimulation of AMP-activated protein kinase (AMPK) is associated with enhancement of Glut1-mediated glucose transport. Arch Biochem Biophys. 2000;380:347–352. doi: 10.1006/abbi.2000.1935. [DOI] [PubMed] [Google Scholar]
- 20.Barnes K, Ingram JC, Porras OH, Barros LF, Hudson ER, et al. Activation of GLUT1 by metabolic and osmotic stress: potential involvement of AMP-activated protein kinase (AMPK). J Cell Sci. 2002;115:2433–2442. doi: 10.1242/jcs.115.11.2433. [DOI] [PubMed] [Google Scholar]
- 21.Rubin D, Ismail-Beigi F. Differential accumulation of Glut1 in the non-DRM domain of the plasma membrane in response to the inhibition of oxidative phosphorylation. Arch Biochem Biophys. 2004;431:224–232. doi: 10.1016/j.abb.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Rubin D, Ismail-Beigi F. Distribution of Glut1 in detergent-resistant membranes (DRMs) and non-DRM domains: effect of treatment with azide. Am J Physiol Cell Physiol. 2003;285:C377–C383. doi: 10.1152/ajpcell.00060.2003. [DOI] [PubMed] [Google Scholar]
- 23.Jing M, Ismail-Beigi F. Critical role of 5′-AMP-activated protein kinase in the stimulation of glucose transport in response to inhibition of oxidative phosphorylation. Am J Physiol Cell Physiol. 2007;292:C477–C487. doi: 10.1152/ajpcell.00196.2006. [DOI] [PubMed] [Google Scholar]
- 24.Jing M, Ismail-Beigi F. Role of 5′-AMP-activated protein kinase in stimulation of glucose transport in response to inhibition of oxidative phosphorylation. Am J Physiol Cell Physiol. 2006;290:C484–C491. doi: 10.1152/ajpcell.00321.2005. [DOI] [PubMed] [Google Scholar]
- 25.Stenbit AE, Burcelin R, Katz EB, Tsao TS, Gautier N, et al. Diverse effects of Glut 4 ablation on glucose uptake and glycogen synthesis in red and white skeletal muscle. J Clin Invest. 1996;98:629–634. doi: 10.1172/JCI118833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryder JW, Kawano Y, Chibalin AV, Rincon J, Tsao TS, et al. In vitro analysis of the glucose-transport system in GLUT4-null skeletal muscle. Biochem J. 1999;342:321–328. [PMC free article] [PubMed] [Google Scholar]
- 27.Zisman A, Peroni OD, Abel ED, Michael MD, Mauvais-Jarvis F, et al. Targeted disruption of the glucose transporter 4 selectively in muscle causes insulin resistance and glucose intolerance. Nat Med. 2000;6:924–928. doi: 10.1038/78693. [DOI] [PubMed] [Google Scholar]
- 28.Raney MA, Turcotte LP. Evidence for the involvement of CaMKII and AMPK in Ca2+-dependent signaling pathways regulating FA uptake and oxidation in contracting rodent muscle. J Appl Physiol. 2008 doi: 10.1152/japplphysiol.01282.2007. [DOI] [PubMed] [Google Scholar]
- 29.Frosig C, Jorgensen SB, Hardie DG, Richter EA, Wojtaszewski JFP. 5′-AMP-activated protein kinase activity and protein expression are regulated by endurance training in human skeletal muscle. Am J Physiol Endocrinol Metab. 2004;286:E411–E417. doi: 10.1152/ajpendo.00317.2003. [DOI] [PubMed] [Google Scholar]
- 30.Daugaard J, Richter E. Muscle- and fibre type-specific expression of glucose transporter 4, glycogen synthase and glycogen phosphorylase proteins in human skeletal muscle. Pfl++gers Archiv European Journal of Physiology. 2004;447:452–456. doi: 10.1007/s00424-003-1195-8. [DOI] [PubMed] [Google Scholar]
- 31.Blair AS, Hajduch E, Litherland GJ, Hundal HS. Regulation of glucose transport and glycogen synthesis in L6 muscle cells during oxidative stress. Evidence for cross-talk between the insulin and SAPK2/p38 mitogen-activated protein kinase signaling pathways. J Biol Chem. 1999;274:36293–36299. doi: 10.1074/jbc.274.51.36293. [DOI] [PubMed] [Google Scholar]
- 32.Derave W, Straumann N, Olek RA, Hespel P. Electrolysis stimulates creatine transport and transporter cell surface expression in incubated mouse skeletal muscle: potential role of ROS. Am J Physiol Endocrinol Metab. 2006;291:E1250–E1257. doi: 10.1152/ajpendo.00060.2006. [DOI] [PubMed] [Google Scholar]
- 33.Andrade FH, Reid MB, Westerblad H. Contractile response of skeletal muscle to low peroxide concentrations: myofibrillar calcium sensitivity as a likely target for redox-modulation. FASEB J. 2001;15:309–311. doi: 10.1096/fj.00-0507fje. [DOI] [PubMed] [Google Scholar]
- 34.Kefaloyianni E, Gaitanaki C, Beis I. ERK1/2 and p38-MAPK signalling pathways, through MSK1, are involved in NF-kappaB transactivation during oxidative stress in skeletal myoblasts. Cell Signal. 2006;18:2238–2251. doi: 10.1016/j.cellsig.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 35.Rhee SG, Bae YS, Lee SR, Kwon J. Hydrogen peroxide: a key messenger that modulates protein phosphorylation through cysteine oxidation. Sci STKE. 2000;2000:E1. doi: 10.1126/stke.2000.53.pe1. [DOI] [PubMed] [Google Scholar]
- 36.Hidalgo C, Sanchez G, Barrientos G, racena-Parks P. A transverse tubule NOX activity stimulates calcium release from isolated triads via RYR1 S-Glutathionylation. J Biol Chem. 2006;M600451200 doi: 10.1074/jbc.M600451200. [DOI] [PubMed] [Google Scholar]
- 37.Higaki Y, Mikami T, Fujii N, Hirshman MF, Koyama K, et al. Oxidative Stress Stimulates Skeletal Muscle Glucose Uptake Through A Phosphatidylinositol-3-kinase-dependent Pathway. Am J Physiol Endocrinol Metab. 2008 doi: 10.1152/ajpendo.00150.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor EB, An D, Kramer HF, Yu H, Fujii NL, et al. Discovery of TBC1D1 as an insulin-, AICAR-, and contraction-stimulated signaling nexus in mouse skeletal muscle. J Biol Chem. 2008 doi: 10.1074/jbc.M708839200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cartee GD, Wojtaszewski JF. Role of Akt substrate of 160 kDa in insulin-stimulated and contraction-stimulated glucose transport. Appl Physiol Nutr Metab. 2007;32:557–566. doi: 10.1139/H07-026. [DOI] [PubMed] [Google Scholar]
- 40.Geraghty KM, Chen S, Harthill JE, Ibrahim AF, Toth R, et al. Regulation of multisite phosphorylation and 14-3-3 binding of AS160 in response to IGF-1, EGF, PMA and AICAR. Biochem J. 2007;407:231–241. doi: 10.1042/BJ20070649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Viollet B, Andreelli F, Jorgensen SB, Perrin C, Geloen A, et al. The AMP-activated protein kinase {alpha}2 catalytic subunit controls whole-body insulin sensitivity. J Clin Invest. 2003;111:91–98. doi: 10.1172/JCI16567. [DOI] [PMC free article] [PubMed] [Google Scholar]