Abstract
Adolescent mothers are at high risk of experiencing intimate partner violence (IPV) which may increase their likelihood of depressive symptoms in adulthood, yet little is known about the long-term effects of IPV on adolescent mothers’ trajectories of depressive symptoms. The study reported here uses prospective data spanning 14 years from a study of 229 adolescent mothers from Washington State, USA to evaluate the effects of adolescent exposure to IPV on the trajectories of depressive symptoms over time, as well as the likelihood of depressive symptoms at age 28 years. After controlling for levels of economic insecurity, the results indicate that adolescent IPV and an early vulnerability to depression were significantly related to the intercept, but not the slope of the adult depressive symptom trajectories. Both cumulative and concurrent IPV predicted the likelihood of depressive symptoms at age 28 years. Follow-up analyses indicate that adolescent IPV is associated with greater levels of adult IPV, and that women who report both adolescent and adult IPV have the highest mean levels of depressive symptoms. These findings suggest that exposure to IPV in adolescence may alter the life course of young women, increasing their risk for continuing exposure to intimate partner violence in adulthood and its concomitant negative mental health effects. Efforts aimed at prevention and early intervention in IPV among adolescent mothers are important components of the clinical care of young mothers.
Keywords: Domestic violence, Adolescent mothers, Poverty, Longitudinal, Latent growth curve modeling, Depression, USA
Introduction
The United States continues to have one of the highest rates of teen pregnancy in the developed world, with almost 750,000 adolescent women becoming pregnant each year (Guttmacher Institute, 2006). While it is important to recognize that adolescent mothers have diverse outcomes that are not uniformly negative (Oxford, Gilchrist, Gillmore, & Lohr, 2006), there is evidence that young mothers are at greater risk for harmful events such as intimate partner violence (IPV), depression and economic insecurity. Understanding how these experiences are related would be directly relevant to the development of prevention and intervention services for pregnant and parent adolescents.
The context of adolescent motherhood is particularly relevant to the study of IPV and its effects because rates of victimization are likely to be higher by virtue of their younger age and because of being pregnant. In terms of age, a recent review of IPV prevalence among adolescent girls found rates of dating violence ranging from 8% to 57% (Hickman, Jaycox, & Arnoff, 2004). Such rates for younger women are typically higher than for those older (AuCoin, 2005; Tjaden & Thoennes, 2000). Additionally, pregnancy is a time when younger women appear to be at even higher risk for experiencing IPV. For instance, three cross-sectional studies of pregnant women have found that women younger than 20 years reported higher rates of IPV than women older than 20 years, with proportions ranging from 18.5% to 20% among young mothers, and 4.4% to 14.2% among older women (Gazmararian et al., 1996; Goodwin et al., 2000; Parker, McFarlane, & Soeken, 1994).
One of the many consequences of IPV is its detrimental effect on women’s mental health, particularly in terms of its association with depressive symptomatology (Golding, 1999). Depression is a serious disorder – it is the second leading cause of Disability Adjusted Life Years (DALYs) lost for women, surpassed only by heart disease in terms of its effect on mortality (Michaud, Murray, & Bloom, 2001). A rich body of cross-sectional research documents increased risk for several mental disorders among women exposed to intimate partner violence with depression as one of the most common diagnoses (see Golding, 1999 for a meta-analysis of this literature). For example, in a nationally representative cross-sectional study, exposure to physical violence by a partner was associated with a 7.5 increase in the odds of having a chronic mental illness such as depression (Coker et al., 2002). Among adolescents, exposure to violence is also associated with increased rates of depression (Kilpatrick et al., 2003). Understanding how IPV increases the risk for depression is of great importance in terms of the prevention and treatment of this disorder among women.
These studies have firmly established the cross-sectional relationship of IPV to depressive symptoms; however, less research is available on the changing effects of IPV on depressive symptoms over time, or the cumulative effects of these experiences for long-term depression outcomes, particularly among adolescent mothers. Two studies have found that initial IPV leads to increased depressive symptoms at a second time point (Ehrensaft, Moffitt, & Caspi, 2006; Zlotnick, Johnson, & Kohn, 2006), but neither study was able to assess whether women continued in abusive relationships over the time studied. Other research does suggest a cumulative effect of IPVexposure for women’s mental health. Although surviving even a single instance of abuse can have serious negative effects, most studies find that the longer the length of the violence, the greater the adverse mental health consequences (Campbell & Soeken, 1999; Golding, 1999).
This body of research has not been able to evaluate two potential alternative explanations for depressive symptoms among adolescent mothers who experience IPV. First, elevated levels of depressive symptoms after IPV may be related to a pre-existing vulnerability to depression. For example, previous research suggests that most adult depressive disorders are preceded by depression during adolescence (Ferdinand & Verhulst, 1995; Pine, Cohen, Gurley, Brook, & Ma, 1998). The experience of adolescent motherhood itself is associated with high levels of moderate to severe depression in the first year after delivery, but these symptoms generally decline over time (Schmidt, Wiemann, Rickert, & Smith, 2006).
Second, these studies do not account for the potentially confounding effects of economic insecurity as a further contributor to depression. Living in poverty is a risk factor both for experiencing IPV (Straus, Gelles, & Steinmetz, 1980) and for increased depressive symptoms. Even within low-income groups, welfare-using mothers report increased levels of depression when compared to non-welfare-using low-income mothers. For instance, anywhere from 22% to 50% of welfare recipients report poor mental health (Olson & Pavetti, 1996), and continued welfare use is correlated with increased levels of depression (Kalil & Danziger, 2000; Lindhorst & Mancoske, 2006). In a cross-sectional analysis of welfare-reliant women, abused women reported almost three times as many mental health disorders as non-abused women, including higher levels of depressive symptoms (Tolman & Rosen, 2001). Although these welfare studies demonstrate the linkage between economic insecurity and depressive symptoms, none of these studies uses prospective, longitudinal data to disentangle the risks associated with IPV and economic insecurity for depressive outcomes over time.
At the critical juncture of their transition to adulthood and parenting responsibilities, the effect of partner violence has the potential to increase depressive symptoms for adolescent mothers, and can contribute to emotional problems in their children. Because depressive disorders are developmental in nature (Fergusson, Horwood, Ridder, & Beautrais, 2005) and because women who have experienced IPV are more likely to develop mental disorders when exposed to subsequent trauma (Breslau, Chilcoat, Kessler, Peterson, & Lucia, 1999), understanding how IPV contributes to depressive symptoms among adolescent mothers can lead to better specified prevention and treatment interventions. In addition, maternal depression moderates a number of important child outcomes, including children’s externalizing behavior (Harnish, Dodge, & Valente, 1995), children’s internalizing behavior (Cicchetti, Rogosch, & Toth, 1998) and their adaptive functioning (Luoma et al., 2001), so preventing depression among adolescent mothers has clear benefits for them and their children.
Study objectives
Despite increasing attention to the dynamics of intimate partner violence in the lives of adolescent mothers, our knowledge about the relationship of IPV to important later life outcomes such as depressive symptomatology is limited in three important ways. First, most research on adolescent or adult IPV is cross-sectional, so very few studies have evaluated how IPV influences mental health over time, particularly its effect on developmental trajectories of depressive symptomatology among at-risk women. Second, analyses of the effect of IPV on depressive symptoms have largely been conducted with adolescent mothers drawn from clinical settings, and these women may have different risk profiles than women in community-based samples. Third, IPV among adolescent mothers occurs within a larger environmental context of risk, such as the likelihood of economic insecurity and pre-existing vulnerabilities to depressive symptoms. We are aware of no studies that evaluate the relative importance that these three risks – IPV, economic insecurity, and a vulnerability to depressive symptoms – pose for the long-term depressive outcomes of adolescent mothers using prospective data over time.
Our analytic goals in this study are twofold: (1) to describe the trajectories of depressive symptomatology experienced during early adulthood (aged 20–27 years) of a group of adolescent mothers, and to examine how these trajectories are affected by adolescent exposure to IPV, within the context of these women’s vulnerability to depressive symptoms and economic insecurity and (2) to estimate the unique cumulative effects of life course exposure to IPV, economic insecurity and early depressive symptoms on the likelihood of being depressed approximately 10 years later. This study examines the effect of all three potential risk factors using prospective data from a community-based longitudinal study of adolescent mothers.
Given the scarcity of data on long-term mental health outcomes for adolescent mothers, and based on our review of the literature, we advance two tentative hypotheses: (1) we anticipate that both adolescent IPV and economic insecurity will have a unique effect on adult trajectories of depressive symptoms, namely by increasing the intercept of these trajectories, controlling for pre-existing levels of depression; and we expect the slope of depressive symptoms to show decrease over time and (2) for those women who experienced IPV in both adolescence and adulthood, we expect the cumulative effect of this disadvantage to increase the likelihood of depressive symptoms in adulthood, above and beyond the effect of a pre-existing vulnerability to depression and long-term economic insecurity.
Method
Participants and procedure
We use data from a 14-year longitudinal study of teenage parenting in this secondary analysis. At enrollment, study participants were unmarried pregnant adolescents, aged 17 years and younger, who planned to carry their babies to term. Participants were recruited from public and private hospital prenatal clinics, public school alternative programs, and social service agencies in three urban counties in the northwest. Parental or guardian consent was obtained for study participants who were not emancipated minors. Because by design participants were not recruited from mental health treatment, drug treatment, or juvenile justice agencies (typical sampling locations for other studies of adolescent mothers), this may be considered a more normative sample of pregnant adolescents who chose to keep their babies. Recruitment procedures included advertising, so a conventional overall response rate could not be calculated. However, approach and consent data were obtained at one of the participating agencies, a large county hospital prenatal clinic, and 76% of those eligible agreed to participate.
The sample is multi-ethnic and relatively low income. The original sample consisted of 240 adolescents who completed an initial interview between June 1988 and January 1990. The sample for the present analyses consisted of 229 (95.4%) of the original sample. Eleven cases were excluded from the analyses because the respondents dropped out of the study in the first 5 years and had no outcome measures. The ethnic make-up of the sample is representative of the ethnic mix of adolescent mothers in Washington State, USA at the time (Seattle – King County Department of Public Health, 1996). The majority of respondents were European American (53%), followed by African American (28%), Native American (6%), Asian American (3%), and other (10%); 8% reported Hispanic ethnicity. At 6 months post-partum, almost half of the respondents (47%) reported that their main source of income was public assistance (welfare). Respondents’ age at enrollment ranged from 12 to 17 years (M = 16.6 years).
Respondents typically provided survey responses through in-person interviews; telephone interviews were conducted with participants who had moved out of the area, averaging 11% over time. Respondents were paid $15–$50 for their participation at each interview. Respondents were assured of the confidentiality of their responses in the consent form, and by the interviewers at the more sensitive sections of the interview; they were also notified the project had a Certificate of Confidentiality from the federal government. Interviews were conducted at 6-month intervals from 6–18 months post-partum and 3.5–6 years post-partum, and at 1-year intervals from 9.5–11.5 years post-partum. (Due to the vagaries of funding, data were not collected between 1994 and 1998.) In total, 14 waves of data were used in our analyses.
Measures
Outcome
Depressive symptoms
Depressive symptoms were measured at each interview using the Brief Symptom Inventory (BSI) depression subscale (Derogatis, 1993). The BSI is a standardized instrument with demonstrated reliability and validity, and is designed to assess psychological functioning. Respondents were asked to indicate how often in the past week each of the following bothered or distressed them: no interest in things, feeling hopeless about the future, feelings of worthlessness, thoughts of ending your life, feeling lonely, and feeling blue. Responses were scored on a five-point scale ranging from 0 (not at all) to 4 (extremely). Item scores were averaged to form the depression subscale score. The alpha reliabilities for these items at each time point ranged from 0.82 to 0.88. In addition, the validity of this measure appears strong because during one of the time points in the study, the Center for Epidemiological Study –Depression (CES-D) scale was also given to the respondents and the correlation between the BSI and CES-D was 0.80.
Predictors and covariates
Intimate partner violence (IPV)
At each time point after respondents turned 18 years old, they were asked to provide an assessment of their experiences with intimate partner violence. Once respondents were aged 18 years, they were asked retrospectively about IPV since pregnancy, after which prospective data were collected. IPV was measured with seven items from the Conflict Tactics Scale which has been used to assess family violence in hundreds of studies (Straus, 1989). The questions asked whether the father of the respondent’s baby, her husband, or any boyfriend or sexual partner had since pregnancy – threatened to hit or throw something at her, threw something at her, pushed/grabbed/shoved/or slapped her, hit her with a fist/object/kicked/or bit her, beat her up, threatened her with a knife or gun, or used a knife or fired a gun at her. Responses were coded as “yes” or “no.” In keeping with recognized research procedures for creating a measure of total violence (Straus, 1989), the sum of the responses represents the IPV score. The alpha reliability for the IPV items at each interview ranged from 0.76 to 0.87.
Economic insecurity
As a proxy for poverty and an indicator of economic insecurity, we assessed whether the respondent used welfare as her primary means of financial support in the past 6 months, and coded this dichotomously.
Vulnerability to depressive symptoms
We used the women’s initial report of their depressive symptoms in the first wave of data collection as a proxy representing their vulnerability to depression. This was the earliest report the women made on their depressive symptoms and was also the period of the highest symptomatology.
Analytic strategy and variable construction
Hypothesis 1
The analytic strategy used to assess trajectories of depressive symptomatology was latent growth curve modeling (LGM) (Muthén, 1997). This is a longitudinal technique that describes growth by identifying trajectories of change over time. These trajectories are mathematically described by parameters called “growth factors.” The two basic growth factors for a trajectory are the intercept (the starting point) and the slope (the change over time). A growth trajectory can be visually represented by charting the average starting point (intercept) and the average change over time (slope). Because each individual will deviate somewhat from the averages, these growth factors each include a variance component. This allows for associations between the growth factors with predictors or outcomes.
LGM is preferred over a repeated measure ANOVA because it describes the average growth, such as the group mean and slope, in a construct (depressive symptoms) while also capturing intra-individual variation in the developmental process; this individual variation is important for theorists seeking to understand and explain the impact of antecedents on a growth process (Duncan, Duncan, Strycker, Li, & Alpert, 1999). Although LGM is similar to a repeated measure analysis, it is more advanced because time-varying covariates can be incorporated into the model (Duncan et al., 1999). For these reasons, LGM is the more appropriate method for the assessment of factors related to the development of depressive symptoms over time, while accounting for the time-varying effects of concurrent intimate partner violence. For the present study, the analysis was accomplished using Mplus version 4.1 with a maximum likelihood estimator which is considered robust under conditions of non-normality (Muthén & Muthén, 2004). Two fit statistics were utilized to assess the fit of the model to the data; the Comparative Fit Index (CFI; Bentler, 1990) which should be 0.90 or greater for appropriate fit and the Residual Mean Squared Error Approximation index (RMSEA; Browne & Cudeck, 1993) which should be less than 0.08 for acceptable fit (MacCallum, Browne, & Sugawara, 1996). In addition, fit is assessed using the model Chi-square; acceptable fit occurs if the Chi-square value divided by the degrees of freedom is less than 3 (Kline, 1998).
For the LGM, the following variables were constructed (see Table 1 for descriptive data on variables for both hypotheses). To construct our outcome variable for Hypothesis 1, the trajectory analysis, the BSI depression subscale score for each of the time points from 20.9 to 27.4 years of age was used.1 Baseline predictors of intercept and slope measured prior to the outcome variable included adolescent IPV (retrospective measure after respondents turned 18), and, as control variables, cumulative adolescent welfare use (welfare use over 4 years) and vulnerability to depression (first BSI subscale score). The time-varying covariate used was concurrent IPV, taken at each of the same time points as the respective measure of depressive symptoms.
Table 1.
Means and standard deviations of study variables
| Construct | Hypothesis 1
|
Hypothesis 2
|
||||
|---|---|---|---|---|---|---|
| Change in depressive symptoms over time
|
Cumulative effect of IPV
|
|||||
| M | SD | M | SD | |||
| Depression | Vulnerability to depressive symptoms at pregnancy (age 16.6 years) | 0.88 | 0.75 | Vulnerability to depressive symptoms at pregnancy (age 16.6 years) | 0.88 | 0.75 |
| Depressive symptoms at (in years) | BSI depressive subscale t-score | |||||
| Age 20.9 | 0.64 | 0.65 | (Age 28.4 years) | 54 | 9.5 | |
| Age 21.4 | 0.60 | 0.70 | ||||
| Age 21.9 | 0.60 | 0.70 | ||||
| Age 22.4 | 0.62 | 0.70 | ||||
| Age 22.9 | 0.67 | 0.75 | ||||
| Age 26.5 | 0.63 | 0.73 | ||||
| Age 27.4 | 0.60 | 0.72 | ||||
| Intimate partner violence | Adolescent IPV | 2.15 | 2.13 | Adolescent IPV | 2.15 | 2.13 |
| IPV at (in years) | Cumulative (age 20.9–27.4 years) | 4.10 | 4.99 | |||
| Age 20.9 | 0.92 | 1.52 | ||||
| Age 21.4 | 0.83 | 1.55 | Concurrent (age 28.4 years) | 0.26 | 0.86 | |
| Age 21.9 | 0.62 | 1.38 | ||||
| Age 22.4 | 0.71 | 1.62 | ||||
| Age 22.9 | 0.47 | 1.12 | ||||
| Age 26.5 | 0.36 | 1.12 | ||||
| Age 27.4 | 0.30 | 1.04 | ||||
| Age 28.4 | 0.26 | 0.86 | ||||
| Economic insecurity (welfare use) | Cumulative adolescent (age 17.4–20.4 years) | 2.22 | 1.46 | Cumulative (age 17.4–27.4 years) | 5.14 | 2.99 |
| Concurrent (age 28.4 years) | 0.10 | 0.30 | ||||
Hypothesis 2
We used OLS regression to assess the association between our predictor variables and the final depressive score outcome. The outcome for this hypothesis was the BSI depression subscale t-score, a standardized score with a mean of 50, and a standard deviation of 10 (Derogatis, 1993), taken at the final time point when respondents were on average age of 28.4 years. A variable was constructed to represent cumulative IPV exposure across seven time points. The total IPV at each time point was summed to create a cumulative index of exposure to IPV in adulthood that occurred prior to the outcome measure of the depressive symptoms at age 28.4 years. Concurrent IPV was the IPV score at age 28.4 years. Adolescent IPV was the same retrospective score described above in the LGM analysis. Cumulative adult welfare was summed over 11 time points from age 17.3 to 27.3 years; concurrent welfare use was measured at age 28.4 years.
Missing data
Of the 229 women, missing data patterns indicated that about a quarter missed at least one wave of data collection over the 10 years of the study. Seventy-six percent of the sample has been interviewed at all 14 time points, representing a high level of retention for a sample composed primarily of low-income women. Retention rates for each wave of data collection ranged from 85.9% to 99.6%. The missing data in this study were managed within the modeling framework using Mplus 4.1 (Muthén & Muthén, 2004). Mplus uses all data that are available to estimate the model using an EM algorithm for a maximum likelihood estimated covariance matrix based on the work of Little and Rubin (2002).
Results
Descriptive results
Means and standard deviations for the variables used are presented in Table 1. In their retrospective assessment of intimate partner violence from pregnancy to the transition to adulthood, 67.2% of adolescent mothers reported at least one episode of victimization. On average, respondents reported decreasing exposure to IPV as time passed, with 15.0% reporting IPV at the final time point. Likewise, use of welfare peaked early, with 63% of women reporting that welfare was their primary source of income at age 20.4 years; this number had fallen to 10.2% at the final time period measured. The mean level of depressive symptoms in the sample is highest at pregnancy, and then remains stable during adulthood. Across the seven time points measured in adulthood, the mean level of depressive symptoms in the sample is 0.62. According to the published norms for the BSI depressive symptoms sub-scale for the adult female community sample (Derogatis, 1993), this figure is one-half standard deviation above the norm, indicating that as a group, this sample of adolescent mothers experienced higher levels of depressive symptoms than a typical community sample of women.
Latent growth curve modeling of depressive symptom trajectories
We estimate the effect of three predictors of variation in depressive symptoms over time while modeling time-varying effects of concurrent IPV at each time point; the three predictors are adolescent IPV, cumulative adolescent welfare use, and vulnerability to depressive symptoms.
The first step in the analysis for the first hypothesis was to identify the overall trajectory of depressive symptoms for the sample. The LGM model was specified such that the factor loading indicates the intercept at the first time point, when respondents were approximately 20.9 years of age. Time was coded to reflect the years at each wave of data collection from the intercept (i.e., the number of years after age 20.9 years). The coefficient for the intercept of the unconditional model was significant (0.57, p ≤ 0.001), while the slope was flat (−0.003, p > 0.05). In addition to estimates of the intercept and slope, LGM also estimates the variance of these parameters, or the amount of variation between individuals’ intercepts and slopes (McLeod & Owens, 2004). The parameters in this sample demonstrated significant variation, indicating that there are individual differences (random effects) in both the initial levels of depressive symptoms and rates of change over time (intercept variance = 0.26, p ≤ 0.001; and slope variance = 0.002, p ≤ 0.05). Model fit indices were within the expected range with a CFI of 0.93, and an RMSEA 0.07. We also compared the growth model above with a single factor only model in which only the intercept was specified (Duncan et al., 1999); the single factor only model did not fit the data better with a non-significant difference in chi-square: Δχ2 = 14.51 (df = 10), thus we retained the full growth model.
The conditional model was tested next; the growth factors (intercept and slope) were specified as an outcome of adolescent IPV, adolescent cumulative welfare use, and vulnerability to depressive symptoms while simultaneously modeling time-varying effects of concurrent IPV on the corresponding time point indicator of depressive symptoms. This model fit the data well with a CFI of 0.90 and an RMSEA of 0.07 with χ2 = 168.2, 80 df, leaving the ratio of chi-square to degrees of freedom = 2.1; all measures of fit are appropriate for model testing (Kline, 1998; MacCallum et al., 1996). We tested interactions between IPV and vulnerability to depression and economic insecurity. These interactions were not significant, so we report the main effects in the remainder of the paper. Table 2 reports the standardized/unstandardized effects of the predictors on the growth factors (intercept and slope) of the depressive symptoms and Table 3 shows the standardized/unstandardized effect of the time-varying covariates. Adolescent exposure to IPV and vulnerability to depressive symptoms were both significant predictors of the intercept of depressive symptoms, but cumulative welfare use was not a significant predictor. None of the predictors had a significant effect on the slope of depressive trajectories. The effect of adolescent exposure to IPV, therefore, increases the initial level of depressive symptoms over and above that of the women’s initial vulnerability to depressive symptoms, but does not affect the rate of change in these symptoms. Analysis of the time-varying covariates further shows that the concurrent association between IPV and depressive symptoms is significant in all but one of the waves studied, indicating that with each unit increase in IPV there was a corresponding increase in depressive symptoms. Thus, our first hypothesis that IPVaffects adult trajectories of depressive symptoms by increasing the starting level (intercept) was supported, but our hypothesis that the slope of depressive symptoms would decrease over time was not upheld.
Table 2.
Effect of predictors on the intercept and slope of depressive symptoms (age 20.9–27.4 years)
| Independent variables | Depression latent growth curve
|
|||||
|---|---|---|---|---|---|---|
| Intercept
|
Slope
|
|||||
| Standardized coefficient | Unstandardized coefficient | SE | Standardized coefficient | Unstandardized coefficient | SE | |
| Adolescent IPV | 0.34*** | 0.23 | 0.05 | −0.16 | −0.01 | 0.01 |
| Cumulative adolescent welfare use | 0.01 | 0.00 | 0.02 | −0.11 | −0.00 | 0.01 |
| Vulnerability to depressive symptoms at pregnancy | 0.33*** | 0.08 | 0.02 | −0.24 | −0.01 | 0.01 |
p ≤ 0.001.
Table 3.
The effect of the time-varying predictor (IPV) on depressive symptoms
| Independent variable: IPV at age (years) | Dependent variable: depressive symptoms
|
||
|---|---|---|---|
| Standardized coefficient | Unstandardized coefficient | SE | |
| 20.9 | 0.14*** | 0.07 | 0.02 |
| 21.4 | 0.06 | 0.03 | 0.02 |
| 21.9 | 0.14** | 0.07 | 0.02 |
| 22.4 | 0.23*** | 0.10 | 0.02 |
| 22.9 | 0.27*** | 0.17 | 0.03 |
| 26.5 | 0.14** | 0.08 | 0.03 |
| 27.4 | 0.19*** | 0.14 | 0.04 |
p ≤ 0.01;
p ≤ 0.001.
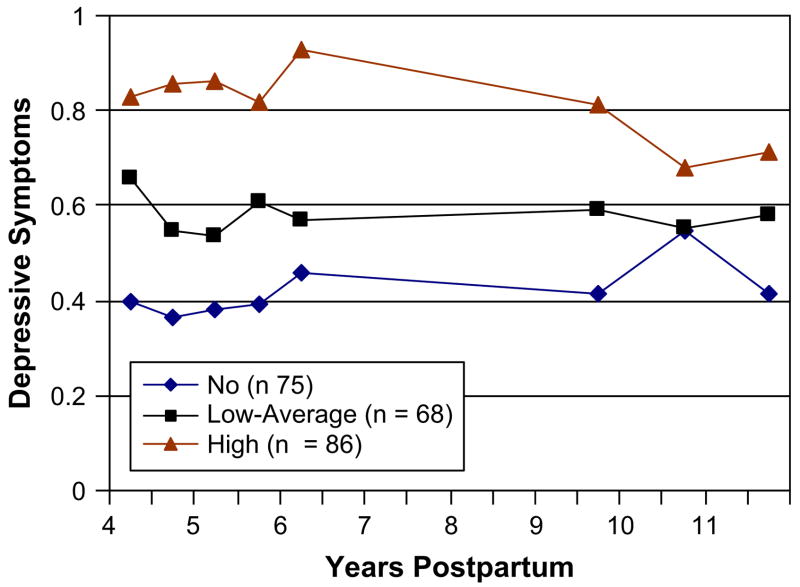
Descriptively, the pattern of depressive symptoms over time is represented in Fig. 1. This figure demonstrates the relationship between the level of adolescent IPV exposure categorized into three groups (those with no adolescent exposure, those with low to average exposure, and those with higher than the mean level of exposure) and the corresponding score on the depressive symptoms subscale. The amount of depressive symptoms experienced is highest for those with the highest IPV scores, and lowest for those not exposed to intimate partner violence in adolescence.
Fig. 1.
Mean of depressive symptoms between 4 and 11.5 years post-partum at three levels of adolescent exposure to IPV: “No” adolescent exposure; some exposure to the mean, denoted “Low-Average”; at the mean or higher, denoted “High”.
Our second hypothesis states that cumulative IPV will have a unique, long-term effect on depressive symptomatology when respondents are nearing age 30 years. Table 4 presents the results of both the linear regression and the correlation matrix used to test this hypothesis; the amount of variance explained is 20% (R2 = 0.20). Table 4 shows that our second hypothesis regarding the cumulative effects of IPV was supported: the higher the level of adult exposure to IPV, the higher the level of depressive symptoms in adulthood. Concurrent IPV at the final wave of data collection was also significantly related to depressive symptoms at the same time point, but neither adolescent IPV nor cumulative welfare use was related to the final depressive symptom outcome.
Table 4.
Linear regression predicting depressive symptom t-score (28.4 years) and correlation matrix
| Linear regression
|
Correlation matrix
|
||||||
|---|---|---|---|---|---|---|---|
| Standardized coefficient | 1 | 2 | 3 | 4 | 5 | 6 | |
| 1) Dependent variable: depressive symptom t-score (age 28.4 years) | |||||||
| Independent variables | — | ||||||
| 2) Vulnerability to depressive symptoms at pregnancy | 0.26*** | 0.29** | — | ||||
| 3) Adolescent IPV | 0.02 | 0.14* | 0.07 | — | |||
| 4) Cumulative adult IPV | 0.23*** | 0.30** | 0.10 | 0.41** | — | ||
| 5) Concurrent IPV | 0.17** | 0.21** | 0.04 | 0.08 | 0.19** | — | |
| 6) Cumulative welfare use | −0.06 | −0.01 | 0.00 | 0.04 | 0.05 | 0.05 | — |
| 7) Concurrent welfare use | 0.10 | 0.13 | 0.06 | −0.03 | 0.07 | 0.11 | 0.27** |
| R2 | 0.20 | ||||||
p ≤5;
p ≤ 0.01;
p ≤ 0.001.
Post hoc analyses
To interpret these findings, we examined the simple correspondence between adolescent exposure to IPV and adult exposure to IPV to address the question of whether the persistently high level of depressive symptoms among the high IPV group was associated with continuing IPV in adulthood. Using the three categories for adolescent IPV noted for Fig. 1 (No, Low-Average, High) and a dichotomously scored variable representing IPV Yes/No in adulthood, we conducted a cross-tabulation analysis. Consistent with our expectation, adolescent and adult exposure to IPV were significantly related, with a chi-square of 27.47 (df = 2). To assess which cells contributed to the significant chi-square analysis, we used EXACON, a statistical module in the SLEIPNER software package developed by Bergman and El-Kouri (1998). This procedure uses a Fisher’s exact test for calculating the probability of an observed cell frequency, conditional on the marginal totals, occurring beyond that which is expected by chance. As expected, those exposed to adolescent IPV were much more likely to experience IPV in adulthood; similarly, those with no adolescent exposure were less likely to experience exposure to IPV in adulthood (table available from authors).
As a final test, we recoded each cell of the cross-tab to represent the experience of adolescent and adult IPV, and used this group in an ANOVA of mean levels of depressive symptoms among the six groups (see Table 5). The ANOVA showed significant differences in the mean level of depressive symptoms; post hoc analyses identified significant differences between those in the high adolescent IPV and adult IPV exposure group and those with either low or no adolescent IPV, and no adult IPV exposure. As expected, the mean level of depressive symptoms was highest for the group that experienced IPV both in adolescence and adulthood, suggesting that the persistence of high depressive symptoms in the high adolescent IPV group is a function of their continued exposure to IPV, and not a long-term traumatic response to events that ended in adolescence.
Table 5.
ANOVA of differences in depressive symptom t-scores between adolescent exposure to IPV and adult exposure to IPV groups
| No adult exposure
|
Adult exposure
|
|||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| No adolescent IPV | 51.13 | 8.58 | 52.71 | 9.28 |
| Low-average adolescent IPV | 49.56 | 6.15 | 56.14a | 9.87 |
| High adolescent IPV | 49.50 | 9.35 | 57.14b,c | 9.58 |
ANOVA F test = 4.63 (5, 213), p < 0.001.
Post hoc Dunnett T3 differences.
Low adolescent exposure to IPV; no adult IPV and low adolescent exposure to IPV; adult IPV.
No adolescent and no adult exposure to IPV and high adolescent exposure to IPV; adult IPV.
Low adolescent exposure to IPV; no adult IPVand high adolescent exposure to IPV; adult IPV.
Discussion
We began our analysis by assessing the long-term effect of adolescent intimate partner violence on later depressive symptom outcomes. Our first hypothesis, that adolescent IPV would have a unique impact on the trajectories of depressive symptoms was supported with regard to the intercept, that is, the level of depression at average age 20.9 years. After controlling for vulnerability to depressive symptoms and early cumulative welfare use as an indicator of economic insecurity, adolescent exposure to IPV significantly increased the intercept of depressive symptoms. We found that the average slope of depressive symptomatology was not predicted by baseline IPV, and, in contrast to previous research (Schmidt et al., 2006), was flat over time. Although beyond the scope of the present study, one avenue of further investigation would be to study the variability in slopes of depressive symptoms, as some women may have increased and other decreased, leading to an average effect showing no change.
The figure demonstrates that those women who reported the highest level of exposure to adolescent IPV had the highest level of depressive symptoms from the outset, and this high level was maintained over the 10 years of the study. Interestingly, IPV, as a time-varying covariate, had a significant concurrent effect on depressive symptoms at every time but one. We know from this finding that depressive symptoms and exposure to IPV co-vary cross-sectionally; however, this analysis cannot discern the direction of that effect. Conceptually, it is plausible that IPV is more likely to cause depression than the reverse.
The findings from the first analysis indicate that exposure to adolescent IPV has an important unique effect on mental health in early adulthood. Our second analysis of the cumulative effect of IPV on depressive symptoms when the mothers were nearing 30 years of age demonstrates the time-ordered linkage between IPV and depressive symptoms. Both cumulative adult IPV and concurrent IPV increased the level of depressive symptoms, even after controlling for adolescent vulnerability to depressive symptoms. In this case, adult depressive symptoms could not be explained solely as a function of the level of adolescent vulnerability to depression identified at pregnancy, but were instead, also a function of exposure to IPV. Further research on the cumulative effects of IPV on other mental health outcomes such as Post-Traumatic Stress Disorder would help clarify other potentially relevant clinical concerns.
Despite several studies that have shown that economic insecurity is associated with increased depressive symptoms, that was not the case in this study. Once pre-existing depression and intimate partner violence were taken into account, economic insecurity was not significantly related to either final depressive outcomes or depressive trajectories. This is a curious finding, since economic insecurity increases the risk for depressive symptoms among women using welfare (Horowtiz & Kerker, 2001; Olson & Pavetti, 1996). However, most studies of welfare-reliant women have not incorporated measures of intimate partner violence, despite the fact that researchers report high levels of IPV among this population (Tolman & Raphael, 2001). Our results indicate that previous findings on the relationship between economic insecurity and poor mental health may be driven in part by the experience of IPV. Alternatively, it may be that our measure of economic insecurity was insufficiently sensitive to variations in income or to the presence of material hardships that might be more closely related to depressive symptoms.
Our findings support and extend previous work on the long-term effects of IPVon women’s mental health. We extend the work of Zlotnick et al. (2006), by demonstrating the consistent concurrent relationship of IPV to depressive symptoms in the trajectory analysis, as well as the cumulative effect of IPV in increasing later levels of depressive symptoms above that of the concurrent abuse indicator. The effect of IPV is maintained even when controlling for other contextual risk factors. We were further able to demonstrate in our post hoc analyses that adolescent IPV is associated with higher levels of adult IPV. These findings suggest that exposure to IPV in adolescence alters the life course of young women, increasing their risk for continuing exposure to intimate partner violence in adulthood and its concomitant negative mental health effects.
Additional research is needed which examines and defines the theoretical processes through which depressive symptoms and IPV are interrelated. Other factors that may be related to both IPV and depressive symptoms such as reduced social support and isolation, physical trauma, and other emotional or psychological consequences apart from depression such as severe anxiety or PTSD should be examined. The National Research Council (2004) notes that disadvantages in one arena of life (such as the impact of gender-based violence) can diminish opportunities in other life domains. From a theoretical standpoint, it may be that IPV in adolescence has a unique effect early in the life course because it shapes other important developmental milestones during the transition to adulthood, notably in the ways that abuse may disadvantage women in other life domains that also affect mental health. As an example, abusive partners often attempt to exert control over women by preventing them from having contact with their larger social network (Dutton, 1992) and impeding activities such as work or schooling (Brush, 2002; Riger & Staggs, 2004). These forms of social control and isolation may further disadvantage women by starting in motion a chain of events that biases women in the direction of mental health problems. Alternatively, early exposure to IPV and its effect on mental health outcomes may predispose young women to avoid other potentially stressful situations such as entering into new social relationships or seeking employment, which in turn reduces social and economic opportunities. If so, an important question for future research is identifying these factors so that appropriate interventions can be developed.
Because adolescent mothers are at particularly high risk for experiencing IPV and depressive symptoms, efforts aimed at prevention of and early intervention in IPV are important components of their clinical care. These results indicate that a top priority in relieving depressive symptoms is assisting young women who are experiencing IPV to end the violence, as overall, depressive symptoms decreased as women reported less exposure to IPV. To be effective in helping abused women, care providers first need to know that a woman is experiencing abuse. Battered women report that they want to be asked by their care providers about their IPV exposure, as long as this exploration is done in a way sensitive to the woman’s need for confidentiality and safety (Hamberger & Phelan, 2004). Care providers are in the position of being able to help young mothers develop safety plans that focus attention on immediate needs such as mobilizing the woman’s social network, and helping her negotiate multiple threats to her well-being (Davies & Lyon, 1998; Lindhorst, Nurius, & Macy, 2005). In addition, access to biopsychosocial interventions that can mitigate depressive symptoms among young battered women is also an important safety net for adolescent mothers coping with violence (Herman, 1992; Rhodes & Levinson, 2003).
As with all studies, this study had some limitations that bear mentioning. This research focuses on adolescent mothers as a high risk group, and as such, it is not generalizable to the broader population of adolescent women. The sample was drawn from a single geographic area of the U.S. Although the sample appears representative of those teenagers who gave birth in this area, we do not know to what extent the findings generalize to adolescent mothers in other regions of the U.S., or other post-industrial countries. The data are based on self-report and may be subject to some error. For example, the BSI depressive symptoms subscale may not measure all important facets of depression, other corroboration of IPV was not obtained, and the measure of economic insecurity, welfare use, may not capture issues of material deprivation that face working poor mothers who are not on welfare. On the other hand, the present research has a number of strengths over previous studies. This research utilizes longitudinal data that are of significantly greater length (across 14 years of the respondents’ lifespan) than other studies of IPV. This sample of adolescent mothers is also community-based, and, therefore, is more representative than samples derived either from battered women’s shelters or from the clinical settings typically used to recruit adolescent mothers. The measures of depressive symptoms and violence exposure used in this study have been used in many other studies, increasing the validity of the findings. Finally, this study uses multivariate analysis to assess the relative influence of IPV, economic insecurity and vulnerability to depression on later mental health outcomes, strengthening our conclusion that IPV has long-term effects on the adult mental health of adolescent mothers.
Acknowledgments
The authors would like to thank Drs. Blair Beadnall and Mary Gillmore for their thoughtful review of this work. An earlier version of this study was presented at the Society for Social Work and Research meeting in San Francisco, CA, January 2007.
Footnotes
This research was supported by the grants DA05208 from the National Institute on Drug Abuse, and MH52400 and 1K01MH72827-01A from the National Institute of Mental Health.
For ease of interpretation, we report the ages of the women at the assessment time points. These time points, however, were timed based on the number of months they were post-partum.
References
- AuCoin K. Family violence in Canada: A statistical profile. Ottawa, Ontario, Canada: Canadian Centre for Justice Statistics and Statistics Canada; 2005. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bergman LR, El-Kouri BM. A statistical package for pattern-oriented analyses (Version 2.0). [Computer software] Stockholm: Stockholm University, Department of Psychology; 1998. SLEIPNER. [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychological Medicine. 1999;29:813–821. doi: 10.1017/s0033291799008612. [DOI] [PubMed] [Google Scholar]
- Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Brush LD. Work-related abuse: a replication, new items and persistent questions. Violence and Victims. 2002;17:743–757. doi: 10.1891/vivi.17.6.743.33720. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Soeken KL. Women’s responses to battering over time: an analysis of change. Journal of Interpersonal Violence. 1999;14:21–40. [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: contributions to the development of attachment insecurity and behavior problems in toddlerhood. Development and Psychopathology. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23:260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Davies J, Lyon E. Safety planning with battered women: Complex lives/difficult choices. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Derogatis LR. SCL-90-R Symptom Checklist-90-R: Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Systems, Inc; 1993. [Google Scholar]
- Duncan T, Duncan S, Strycker L, Li F, Alpert A. An introduction to latent variable growth curve modeling. Mahwah, NJ: Laurance Erlbaum Associates; 1999. [Google Scholar]
- Dutton MA. Empowering and healing the battered woman: A model for assessment and intervention. New York: Springer; 1992. [Google Scholar]
- Ehrensaft MK, Moffitt TE, Caspi A. Is domestic violence followed by an increased risk of psychiatric disorders among women but not among men? A longitudinal cohort study. American Journal of Psychiatry. 2006;163:885–892. doi: 10.1176/ajp.2006.163.5.885. [DOI] [PubMed] [Google Scholar]
- Ferdinand RF, Verhulst FC. Psychopathology from adolescence into young adulthood: an 8-year follow-up study. American Journal of Psychiatry. 1995;152:1586–1594. doi: 10.1176/ajp.152.11.1586. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:1584–1591. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. JAMA. 1996;275:1915–1920. [PubMed] [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: a meta-analysis. Journal of Family Violence. 1999;14:99–132. [Google Scholar]
- Goodwin MM, Gazmararian JA, Johnson CH, Gilbert BC, Saltzman LE the PRAMS Working Group. Pregnancy intendedness and physical abuse around the time of pregnancy: findings from the pregnancy risk assessment monitoring system, 1996–1997. Maternal Child Health Journal. 2000;4:85–92. doi: 10.1023/a:1009566103493. [DOI] [PubMed] [Google Scholar]
- Guttmacher Institute. US teenage pregnancy statistics: National and state trends and trends by race and ethnicity. New York: Guttmacher Institute; 2006. Retrieved August 11, 2007, from http://www.guttmacher.org/pubs/2006/09/12/USTPstats.pdf. [Google Scholar]
- Hamberger KL, Phelan MB. Domestic violence screening and intervention in medical and mental healthcare settings. New York: Springer; 2004. [Google Scholar]
- Harnish JD, Dodge KA, Valente E. Mother-child interaction quality as a partial mediator of the roles of maternal depressive symptomatology and socioeconomic status in the development of child behavior problems. Child Development. 1995;66:739–753. doi: 10.1111/j.1467-8624.1995.tb00902.x. [DOI] [PubMed] [Google Scholar]
- Herman JL. Trauma and recovery: The aftermath of violence– From domestic abuse to political terror. New York: Basic Books; 1992. [Google Scholar]
- Hickman L, Jaycox L, Arnoff J. Dating violence among adolescents: prevalence, gender distribution, and prevention program effectiveness. Trauma, Violence and Abuse. 2004;5:123–142. doi: 10.1177/1524838003262332. [DOI] [PubMed] [Google Scholar]
- Horowitz SM, Kerker BD. Impediments to employment under welfare reform: the importance of physical health and psychosocial characteristics. Women and Health, 32, 1/ 2001;2:101–118. doi: 10.1300/J013v32n01_05. [DOI] [PubMed] [Google Scholar]
- Kalil A, Danziger SK. How teen mothers are faring under welfare reform. Journal of Social Issues. 2000;56:775–798. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. New York: The Gilford Press; 1998. [Google Scholar]
- Lindhorst T, Mancoske RJ. The social and economic impact of sanctions and time limits on recipients of temporary assistance to needy families. Journal of Sociology and Social Welfare. 2006;23:93–114. [PMC free article] [PubMed] [Google Scholar]
- Lindhorst T, Nurius P, Macy R. Contextualized assessment with battered women: strategic safety planning to cope with multiple harms. Journal of Social Work Education. 2005;41(2):371–393. doi: 10.5175/jswe.2005.200200261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. Hoboken, NJ: Wiley & Sons; 2002. [Google Scholar]
- Luoma I, Tamminen T, Kaukonen P, Laippala P, Puura K, Salmelin R, et al. Longitudinal study of maternal depressive symptoms and child well-being. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1367–1374. doi: 10.1097/00004583-200112000-00006. [DOI] [PubMed] [Google Scholar]
- MacCallum R, Browne M, Sugawara H. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1(2):130–149. [Google Scholar]
- McLeod JD, Owens TJ. Psychological well-being in the early life course: variations by socioeconomic status, gender, and race/ethnicity. Social Psychology Quarterly. 2004;67:257–278. [Google Scholar]
- Michaud CM, Murray CJL, Bloom BR. Burden of disease – implications for future research. JAMA. 2001;285:535–539. doi: 10.1001/jama.285.5.535. [DOI] [PubMed] [Google Scholar]
- Muthén B. Latent variable growth modeling with multilevel data. In: Berkane M, editor. Latent variable modeling with applications to causality. New York: Springer Verlag; 1997. pp. 149–161. [Google Scholar]
- Muthén B, Muthén LK. Mplus User’s Guide. 3. Los Angeles, CA: Muthen & Muthen; 2004. [Google Scholar]
- National Research Council. Cumulative disadvantage and racial discrimination. In: Blank RM, Dabady M, Citro CF, editors. Measuring racial discrimination. Washington, DC: The National Academies Press; 2004. [Google Scholar]
- Olson K, Pavetti L. Personal and family challenges to the successful transition from welfare to work. Washington, DC: The Urban Institute; 1996. [Google Scholar]
- Oxford M, Gilchrist L, Gillmore M, Lohr M. Predicting variation in the life course of adolescent mothers as they enter adulthood. Journal of Adolescent Health. 2006;39(1):20–26. doi: 10.1016/j.jadohealth.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Parker B, McFarlane J, Soeken K. Abuse during pregnancy: effects on maternal complications and birth weight in adult and teenage women. Obstetrics & Gynecology. 1994;84:323–328. [PubMed] [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Rhodes KV, Levinson W. Interventions for intimate partner violence against women: clinical applications. JAMA. 2003;289(5):601–605. doi: 10.1001/jama.289.5.601. [DOI] [PubMed] [Google Scholar]
- Riger S, Staggs SL. Welfare reform, domestic violence and employment: what do we know and what do we need to know? Violence Against Women. 2004;10:961–990. [Google Scholar]
- Schmidt RM, Wiemann CM, Rickert VI, Smith EO. Moderate to severe depressive symptoms among adolescent mothers followed four years postpartum. Journal of Adolescent Health. 2006;38:712–718. doi: 10.1016/j.jadohealth.2005.05.023. [DOI] [PubMed] [Google Scholar]
- Seattle – King County Department of Public Health: Epidemiology, Planning and Evaluation Unit. Washington: State Department of Health, Center for Health Statistics; 1996. Unpublished raw data. [Google Scholar]
- Straus M. Manual for the Conflict Tactics Scale (CTS) Durham, NC: University of New Hampshire; 1989. [Google Scholar]
- Straus MA, Gelles RJ, Steinmetz SK. Behind closed doors: Violence in the American family. Garden City, NY: Anchor Press/Doubleday; 1980. [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature and consequences of intimate partner violence: Findings from the National Violence Against Women Survey, NCJ 181867. Washington, DC: National Institute of Justice and Centers for Disease Control; 2000. [Google Scholar]
- Tolman RM, Raphael J. A review of research on welfare and domestic violence. Journal of Social Issues. 2001;56(4):655–682. [Google Scholar]
- Tolman RM, Rosen D. Domestic violence in the lives of women receiving welfare: mental health, substance dependency and economic well-being. Violence Against Women. 2001;7:141–158. [Google Scholar]
- Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. Journal of Interpersonal Violence. 2006;21:262–275. doi: 10.1177/0886260505282564. [DOI] [PubMed] [Google Scholar]