Abstract
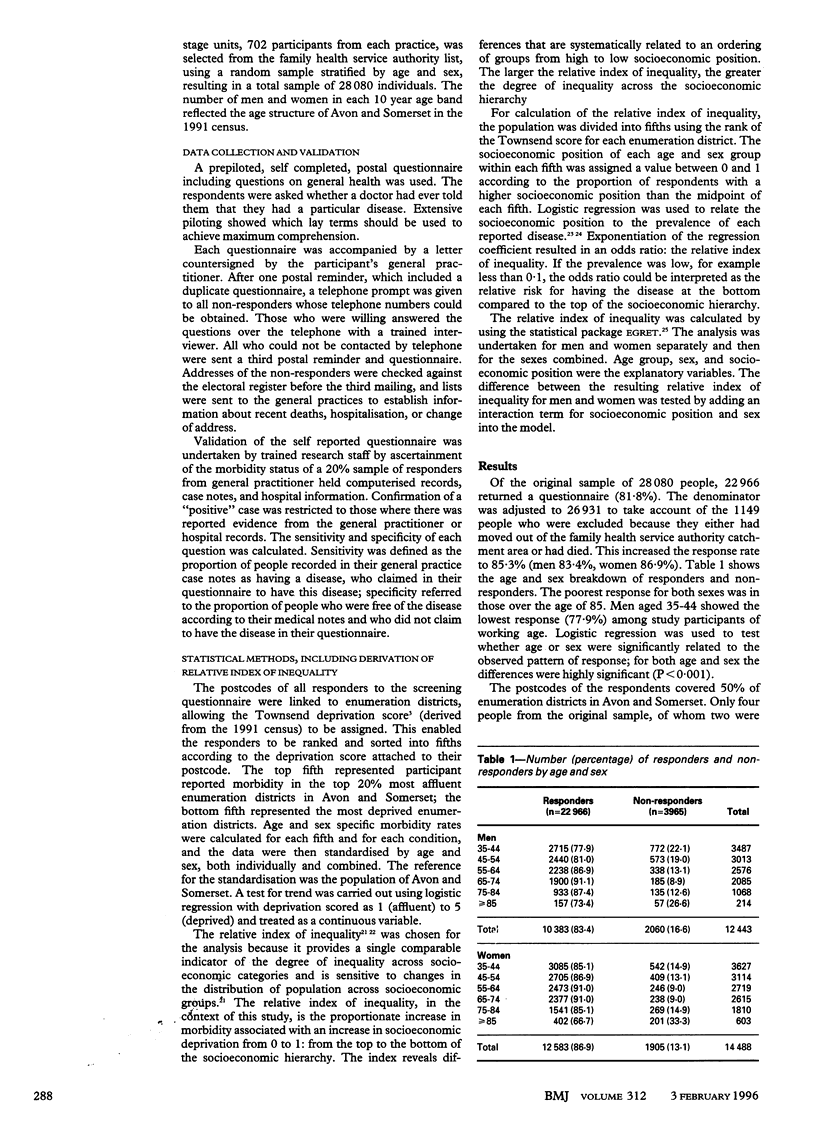
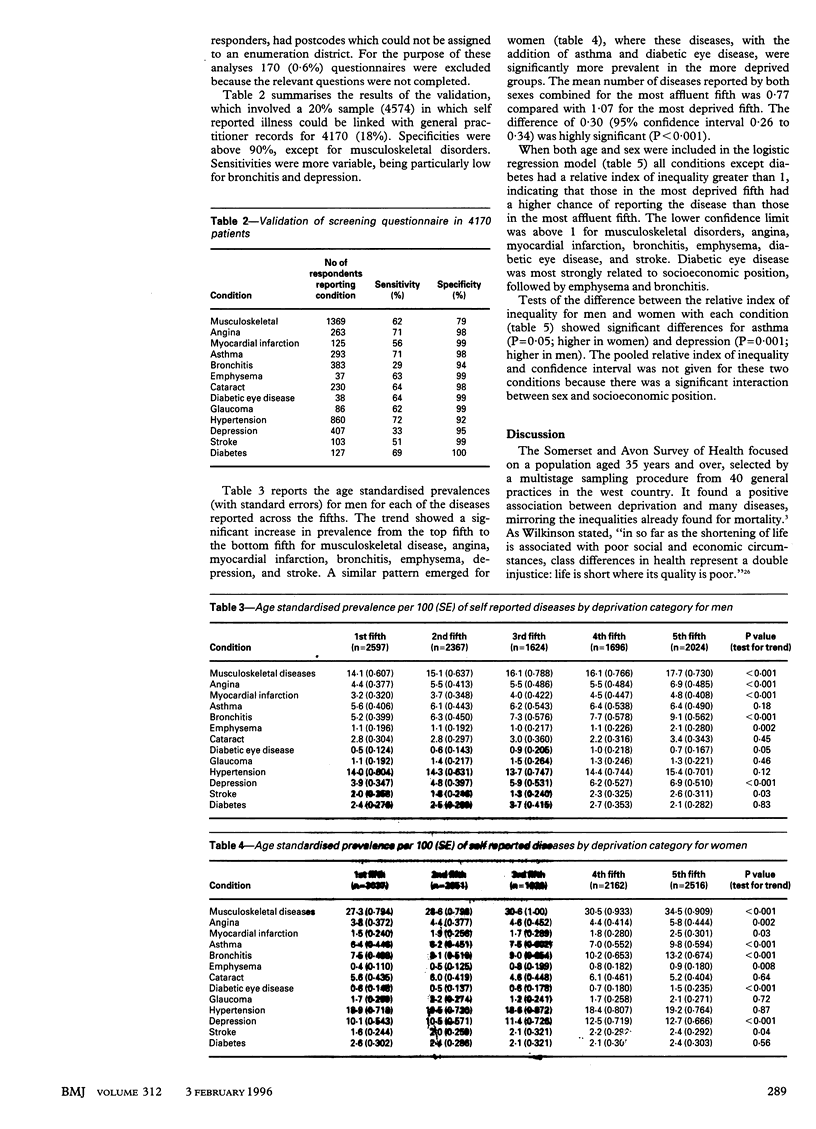
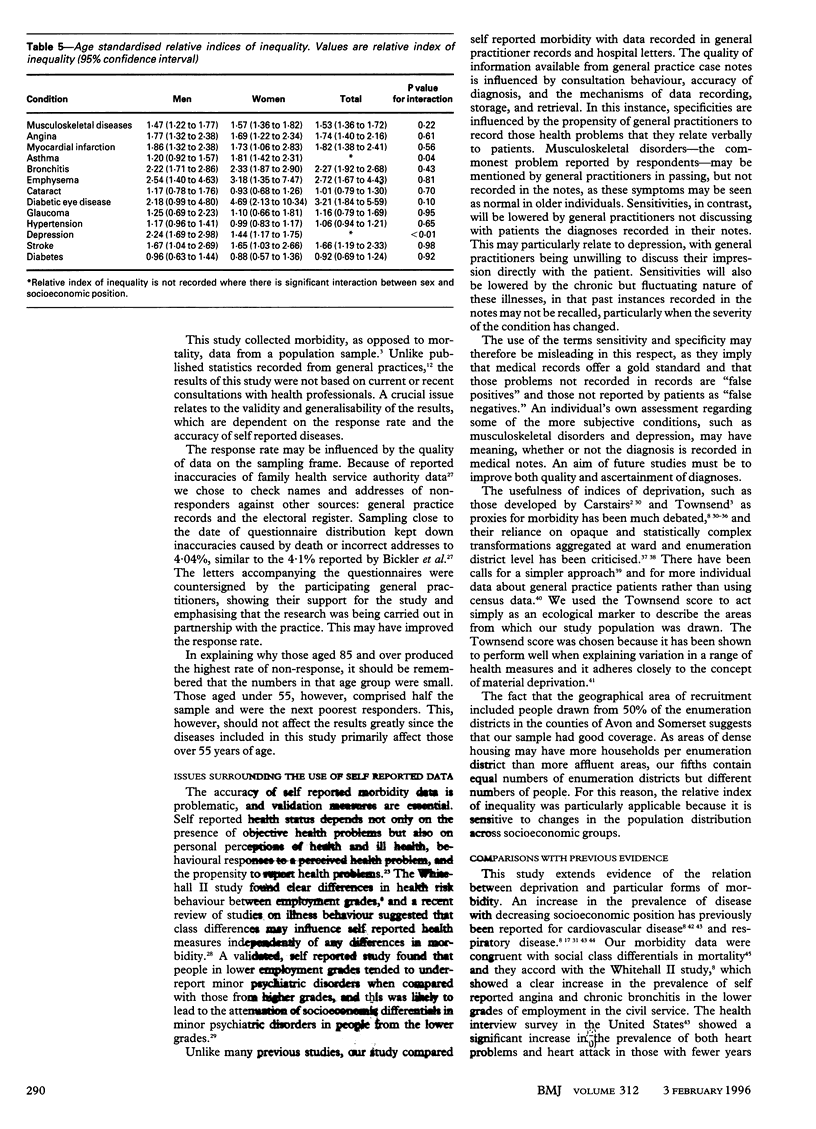
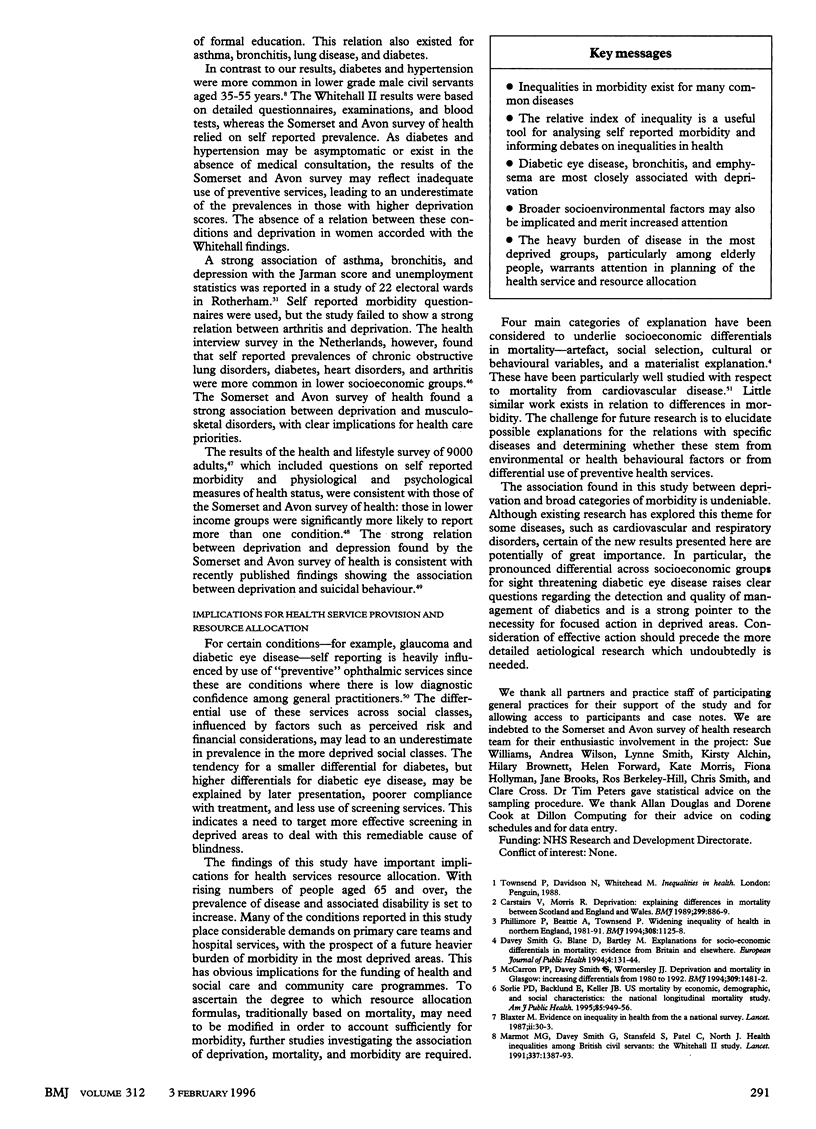
OBJECTIVE: To investigate the association between cause specific morbidity and deprivation in order to inform the debates on inequalities in health and health services resource allocation. DESIGN: Cross sectional postal questionnaire survey ascertaining self reported health status, with validation of a 20% sample through general practitioner and hospital records. SETTING: Inner city, urban, and rural areas of Avon and Somerset. SUBJECTS: Stratified random sample of 28,080 people aged 35 and over from 40 general practices. MAIN OUTCOME MEASURES: Age and sex standardised prevalence of various diseases; Townsend deprivation scores were assigned by linking postcodes to enumeration districts. Relative indices of inequality were calculated to estimate the magnitude of the association between socioeconomic position and morbidity. RESULTS: The response rate was 85.3%. The prevalence of most of the conditions rose with increasing material deprivation. The relative index of inequalilty, for both sexes combined, was greater than 1 for all conditions except diabetes. The conditions most strongly associated with deprivation were diabetic eye disease (relative index of inequality 3.21; 95% confidence interval 1.84 to 5.59), emphysema (2.72; 1.67 to 4.43) and bronchitis (2.27; 1.92 to 2.68). The relative index of inequality was significantly higher in women for asthma (P < 0.05) and in men for depression (P < 0.01). The mean reporting of prevalent conditions was 1.07 for the most deprived fifth of respondents and 0.77 in the most affluent fifth (P < 0.001). CONCLUSIONS: Material deprivation is strongly linked with many common diseases. NHS resource allocation should be modified to reflect such morbidity differentials.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ben-Shlomo Y., White I., McKeigue P. M. Prediction of general practice workload from census based social deprivation scores. J Epidemiol Community Health. 1992 Oct;46(5):532–536. doi: 10.1136/jech.46.5.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickler G., Sutton S. Inaccuracy of FHSA registers: help from electoral registers. BMJ. 1993 May 1;306(6886):1167–1167. doi: 10.1136/bmj.306.6886.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaxter M. Evidence on inequality in health from a national survey. Lancet. 1987 Jul 4;2(8549):30–33. doi: 10.1016/s0140-6736(87)93062-5. [DOI] [PubMed] [Google Scholar]
- Bucquet D., Curtis S. Socio-demographic variation in perceived illness and the use of primary care: the value of community survey data for primary care service planning. Soc Sci Med. 1986;23(7):737–744. doi: 10.1016/0277-9536(86)90122-x. [DOI] [PubMed] [Google Scholar]
- Carstairs V., Morris R. Deprivation: explaining differences in mortality between Scotland and England and Wales. BMJ. 1989 Oct 7;299(6704):886–889. doi: 10.1136/bmj.299.6704.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis S. E. Use of survey data and small area statistics to assess the link between individual morbidity and neighbourhood deprivation. J Epidemiol Community Health. 1990 Mar;44(1):62–68. doi: 10.1136/jech.44.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Featherstone P. I., James C., Hall M. S., Williams A. General practitioners' confidence in diagnosing and managing eye conditions: a survey in south Devon. Br J Gen Pract. 1992 Jan;42(354):21–24. [PMC free article] [PubMed] [Google Scholar]
- Gunnell D. J., Peters T. J., Kammerling R. M., Brooks J. Relation between parasuicide, suicide, psychiatric admissions, and socioeconomic deprivation. BMJ. 1995 Jul 22;311(6999):226–230. doi: 10.1136/bmj.311.6999.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopton J. L., Howie J. G., Porter A. M. Social indicators of health needs for general practice: a simpler approach. Br J Gen Pract. 1992 Jun;42(359):236–240. [PMC free article] [PubMed] [Google Scholar]
- Hutchinson A., Foy C., Sandhu B. Comparison of two scores for allocating resources to doctors in deprived areas. BMJ. 1989 Nov 4;299(6708):1142–1144. doi: 10.1136/bmj.299.6708.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessop E. G. Individual morbidity and neighbourhood deprivation in a non-metropolitan area. J Epidemiol Community Health. 1992 Oct;46(5):543–546. doi: 10.1136/jech.46.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelleher C. Health promotion: shades of Lewis Carroll. J Epidemiol Community Health. 1995 Feb;49(1):1–4. doi: 10.1136/jech.49.1.1-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowy A. Are deprivation indicators a proxy for morbidity? J Public Health Med. 1994 Mar;16(1):113–114. doi: 10.1093/oxfordjournals.pubmed.a042912. [DOI] [PubMed] [Google Scholar]
- Mackenbach J. P. Socioeconomic inequalities in health in The Netherlands: impact of a five year research programme. BMJ. 1994 Dec 3;309(6967):1487–1491. doi: 10.1136/bmj.309.6967.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. G., Smith G. D., Stansfeld S., Patel C., North F., Head J., White I., Brunner E., Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991 Jun 8;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Mays N., Chinn S. Relation between all cause standardised mortality ratios and two indices of deprivation at regional and district level in England. J Epidemiol Community Health. 1989 Jun;43(2):191–199. doi: 10.1136/jech.43.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarron P. G., Smith G. D., Womersley J. J. Deprivation and mortality in Glasgow: changes from 1980 to 1992. BMJ. 1994 Dec 3;309(6967):1481–1482. doi: 10.1136/bmj.309.6967.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris R., Carstairs V. Which deprivation? A comparison of selected deprivation indexes. J Public Health Med. 1991 Nov;13(4):318–326. [PubMed] [Google Scholar]
- O'Donnell O., Propper C. Equity and the distribution of UK National Health Service resources. J Health Econ. 1991 May;10(1):1–19. doi: 10.1016/0167-6296(91)90014-e. [DOI] [PubMed] [Google Scholar]
- Payne J. N., Coy J., Milner P. C., Patterson S. Are deprivation indicators a proxy for morbidity? A comparison of the prevalence of arthritis, depression, dyspepsia, obesity and respiratory symptoms with unemployment rates and Jarman scores. J Public Health Med. 1993 Jun;15(2):161–170. doi: 10.1007/BF02959657. [DOI] [PubMed] [Google Scholar]
- Payne J. N., Coy J., Patterson S., Milner P. C. Is use of hospital services a proxy for morbidity? A small area comparison of the prevalence of arthritis, depression, dyspepsia, obesity, and respiratory disease with inpatient admission rates for these disorders in England. J Epidemiol Community Health. 1994 Feb;48(1):74–78. doi: 10.1136/jech.48.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters T. J., Eachus J. I. Achieving equal probability of selection under various random sampling strategies. Paediatr Perinat Epidemiol. 1995 Apr;9(2):219–224. doi: 10.1111/j.1365-3016.1995.tb00135.x. [DOI] [PubMed] [Google Scholar]
- Phillimore P., Beattie A., Townsend P. Widening inequality of health in northern England, 1981-91. BMJ. 1994 Apr 30;308(6937):1125–1128. doi: 10.1136/bmj.308.6937.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus T., Callahan L. F., Burkhauser R. V. Most chronic diseases are reported more frequently by individuals with fewer than 12 years of formal education in the age 18-64 United States population. J Chronic Dis. 1987;40(9):865–874. doi: 10.1016/0021-9681(87)90186-x. [DOI] [PubMed] [Google Scholar]
- Reading R., Openshaw S., Jarvis S. Are multidimensional social classifications of areas useful in UK health service research? J Epidemiol Community Health. 1994 Apr;48(2):192–200. doi: 10.1136/jech.48.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldon T. A., Smith G. D., Bevan G. Weighting in the dark: resource allocation in the new NHS. BMJ. 1993 Mar 27;306(6881):835–839. doi: 10.1136/bmj.306.6881.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shewry M. C., Smith W. C., Woodward M., Tunstall-Pedoe H. Variation in coronary risk factors by social status: results from the Scottish Heart Health Study. Br J Gen Pract. 1992 Oct;42(363):406–410. [PMC free article] [PubMed] [Google Scholar]
- Smith G. D., Bartley M., Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990 Aug 18;301(6748):373–377. doi: 10.1136/bmj.301.6748.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G. D. Second thoughts on the Jarman index. BMJ. 1991 Feb 16;302(6773):359–360. doi: 10.1136/bmj.302.6773.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G. D., Shipley M. J., Rose G. Magnitude and causes of socioeconomic differentials in mortality: further evidence from the Whitehall Study. J Epidemiol Community Health. 1990 Dec;44(4):265–270. doi: 10.1136/jech.44.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie P. D., Backlund E., Keller J. B. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995 Jul;85(7):949–956. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend P., Simpson D., Tibbs N. Inequalities in health in the city of Bristol: a preliminary review of statistical evidence. Int J Health Serv. 1985;15(4):637–663. doi: 10.2190/AN09-8R52-UE6B-VWUU. [DOI] [PubMed] [Google Scholar]
- Wagstaff A., Paci P., van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33(5):545–557. doi: 10.1016/0277-9536(91)90212-u. [DOI] [PubMed] [Google Scholar]
- Wagstaff A., Van Doorslaer E. Measuring inequalities in health in the presence of multiple-category morbidity indicators. Health Econ. 1994 Jul-Aug;3(4):281–289. doi: 10.1002/hec.4730030409. [DOI] [PubMed] [Google Scholar]


