Abstract
Persistence on treatment affects the efficacy of antihypertensive treatment. We prospectively investigated the persistence on therapy and the extent of blood pressure (BP) control in 347 hypertensive patients (age 59.4 ± 6 years) randomly allocated to a first-line treatment with: angiotensin-converting enzyme (ACE) inhibitors, calcium-channel blockers (CCBs), ß-blockers, angiotensin-II receptor blockers (ARBs), or diuretics and followed-up for 24-months. Persistence on treatment was higher in patients treated with ARBs (68.5%) and ACE inhibitors (64.5%) vs CCBs (51.6%; p < 0.05), β-blockers (44.8%, p < 0.05), and diuretics (34.4%, p < 0.01). No ARB, ACE inhibitor, β-blocker, or diuretic was associated with a higher persistence in therapy compared with the other molecules used in each therapeutic class. The rate of persistence was significantly higher in patients treated with lercanidipine vs others CCBs (59.3% vs 46.6%, p < 0.05). Systolic and diastolic BP was decreased more successfully in patients treated with ARBs (−11.2/−5.8 mmHg), ACE inhibitors (−10.5/−5.1 mmHg), and CCBs (−8.5/−4.6 mmHg) compared with ß-blockers (−4.0/−2.3 mmHg p < 0.05) and diuretics (−2.3/−2.1 mmHg, p < 0.05). No ARB, ACE inhibitor, β-blocker, or diuretic was associated with a higher BP control compared with the other molecules used in each therapeutic class. A trend toward a better BP control was observed in response to lercanidipine vs other CCBs (p = 0.059). The present results confirm the importance of persistence on treatment for the management of hypertension in clinical practice.
Keywords: hypertension, antihypertensive drugs, persistence, blood pressure
Introduction
Reduction of blood pressure (BP) level through antihypertensive drugs is associated with a significant decrease in cardiovascular disease morbidity and mortality (JNC VII 2003; Staessen et al 2005). A comprehensive review of the impact of antihypertensive treatment reports that nearly 75% of hypertensive patients worldwide actually do not achieve a satisfactory BP according to guidelines (Wolf-Maier et al 2004). This indicates that the actual benefits of BP-lowering treatment are less than predicted, with a persistently elevated morbidity and mortality (Erdine et al 2006) and an increase in health care costs (McCombs et al 1994) associated with hypertension.
A major (and modifiable) reason for lack of BP control is failure by patients to take the medications as prescribed. Appropriate use of medications includes compliance (taking medications at the prescribed intervals and dosing regimen) and persistence (continuous use of medications for the specified treatment time period), which, for hypertension, should be maintained life-long (Burnier 2006). Poor compliance and persistence with antihypertensive medications is one likely explanation for the discrepancy between the efficacy of drug treatment established through clinical trials and the results observed in clinical practice (Fujita et al 2006). Compliance with antihypertensive treatment is influenced by many factors, including tolerability of the medication, complexity of the drug regimen, cost of the therapy, characteristics of the medical system and physician, and the asymptomatic nature of hypertension (David 2006). In many hypertensive patients, poor compliance has been attributed to high rate of adverse effects and/or worsening of quality of life (Ambrosioni et al 2000).
Previous studies assessing determinants of the discontinuation of drug therapy were often limited by small sample size, short duration of follow-up, and lack of generalizability to the population treated in community-practice settings. Indeed, most of these studies were conducted as part of large-scale clinical trials (SHEP Group 1991) or of specific population cohorts (Monane et al 1997; Okano et al 1997). In many instances, the studies were retrospective and pre-dated the introduction of the newest classes of better-tolerated antihypertensive agents, such as the angiotensin II receptor blockers (ARBs) that are characterized by an improved tolerability when compared with the older ones such as diuretics and β-blockers (Jones et al 1995).
A retrospective study based on the analysis of refill records of outpatients (n = 21,723 subjects) who have recently started an antihypertensive therapy showed that the continuation of the initially prescribed therapy can be influenced by the drug class. Indeed, the proportion of patients continuing with the initial class of antihypertensive drugs after 12-months of follow-up was significantly higher with ARBs (64% of patients) and angiotensin-converting enzyme (ACE) inhibitors (58%) in comparison with calcium-channel blockers (CCBs) (50%), β-blockers (43%), and thiazide diuretics (38%) (Blooms 1998). These results were also confirmed in a large sample of the Italian population by analyzing all prescriptions of antihypertensive drugs by general practitioners over a 2-year period. The persistence on treatment was greater for patients starting with ARBs while the prescription of diuretics or complex regimens was associated with a withdrawal of treatment in as much as 70% of the population (Poluzzi et al 2005).
However, none of these studies has prospectively investigated the problem of the persistence on treatment with the different classes of antihypertensive drugs or has assessed whether the differences in persistence on treatment might directly influence the extent of BP control in clinical practice. Furthermore, no data have been published about the possibility that differences in the long-term persistence on antihypertensive treatment can be detected among drugs with a different tolerability profile within the same class. This could be a relevant problem for some families of antihypertensive drugs such as the dihydropyridines CCBs, which have evolved from the first-generation, short-acting compounds, to agents with long plasma and receptor half-life with a more favorable clinical profile and a better compliance (Messerli 2002).
The objective of the present study was to prospectively evaluate the long-term persistence on antihypertensive treatment of different classes of first-line antihypertensive drugs prescribed as monotherapy in patients with mild to moderate hypertension. A secondary aim was to investigate whether a difference in persistence on treatment influenced BP control.
Patients and methods
The study was carried out in a cohort of 347 uncomplicated mild to moderate hypertensive patients (systolic blood pressure [SBP] 140–159 mmHg and diastolic BP [DBP] 90–109 mmHg) consecutively referred to our Hypertension Clinic for a clinical evaluation of their hypertension. The following patient characteristics were used as inclusion criteria: (1) age >8 and ≤80 years, (2) no antihypertensive treatment during the last 6 months, (3) no history of major cardiovascular diseases (previous stroke, myocardial infarction, heart failure, major arrhythmias) requiring complex pharmacological treatment, (4) no history of intolerance or hypersensitivity for specific classes of antihypertensive drugs, (5) lack of compelling indications for a specific class of antihypertensive drugs according to ESH-ESC Guidelines (ESH-ESC 2003), (6) capacity to comply with the study protocol. Patients were randomly allocated to treatment with one of the following classes of antihypertensive drugs: ACE inhibitors, ARBs, CCBs, diuretics, and ß-blockers, according to a single-blind study design. Patients treated with CCBs were randomly stratified to lercanidipine in comparison with any other CCB according to a 1:1.5 proportion so that 46 patients were finally treated with lercanidipine. No methodological constraint was applied to the choice of CCBs other than lercanidipine. Lercanidipine was chosen as comparator because of its apparently higher tolerability in respect of other dihydropyridines (Beckey et al 2007). We have not carried out comparisons in the other used classes of antihypertensive drugs, because the internal difference in term of tolerability is not so objectively valuable.
Before the inclusion in the study all patients underwent a complete clinical cardiovascular examination including BP measurement and standard 12-lead electrocardiogram. Resting supine and standing SBP and DBP were measured by mercury sphygmomanometer to the nearest 2 mmHg. The mean of 3 consecutive BP determinations at 1-min intervals was recorded. An identical procedure was used for the assessment of heart rate. Secondary causes of hypertension have been excluded with clinical and biochemical evaluation according to a standardized protocol including determination of plasma renin activity, plasma aldosterone, renal function, and electrolyte balance. Patients were followed up at 6-month intervals and for a cumulative period of 24 months from randomization. BP and heart rate were measured at each scheduled visit according to the baseline procedure. At the same time-interval any change in the initially prescribed therapy and the relative causes were reported in the case report form. Persistence with antihypertensive treatment has been simply defined as the continued use of a medication or medications according to initial prescription (ie, no discontinuation) over the period of follow-up. Persistence has been determined as a dichotomous variable at the specified time-intervals of the protocol. The proportion of patients persistent at any scheduled interval and the average duration of persistence (ie, the average time from treatment initiation to discontinuation) were then calculated. In patients in whom the treatment was discontinued before the end of follow-up, persistence was quantified as the time-interval between randomization and treatment discontinuation. If no discontinuation occurred, persistence was censored at the end of the follow-up. In those patients who did not show a significant reduction of SBP values (≥10%) by monotherapy after 6 months of treatment, a second drug was added. For the purpose of the data analysis they have been considered according to their initial treatment allocation. Patients who needed the addition of a third drug to control BP have been excluded from the study.
The study protocol was approved by the Ethics Committee of the St. Orsola-Malpighi Hospital and all patients provided written informed consent to participate before inclusion in the study.
Outcome variables
The main study outcome was the proportion of patients who persisted with the initially prescribed antihypertensive treatment in each drug class and over the cumulative period of 24 months. We considered as “not persistent” all those patients who withdrew from treatment as well as those who switched to a different class of drugs. Secondary objectives were: (1) the extent of SBP and DBP decrease in the different subgroups of patients, (2) the comparison between the persistence on treatment between patients treated with lercanidipine vs other first-line antihypertensive drugs including the other CCBs.
Statistical analysis
Results are expressed as means ± SD. Statistical analysis was carried out by using a SPSS statistical package (version 9.6.2 for Windows; SPSS Inc., Chicago, IL, USA). The study sample size was calculated according to the hypothesis of a difference between ARBs and diuretics of 25% in terms of persistence on treatment with an alpha-error of 0.05 and a power of the study of 80%. Drop-out rate was estimated at 10%. The data have been analyzed according to an intention-to-treat approach by considering any patients according to their initial drug allocation. Observed differences in continuation of initial therapy were compared between ARBs and the antihypertensive drug class having the next highest rate of continuation using unadjusted, two-sided, chi-square tests and an alpha level of 0.05. The odds ratio (OR) for continuation with the initial drug therapy was then calculated by logistic regression. Potential predictors of persistence tested in the logistic regression model included age (≥65 and <65-years), sex, antihypertensive drug class (ARBs, ACE inhibitors, CCBs, β-blockers, thiazide diuretics), and dosing frequency (once or twice per day). Confidence intervals (CIs) for the estimated ORs and significance tests for the differences from the null value were calculated using estimated standard errors.
Results
The baseline characteristics of the study population (n = 347) and the distribution of first-line antihypertensive drugs are reported in Table 1. One-hundred and ninety-six patients were men and 151 were women. The mean age was 58 ± 6 and 62 ± 5 years respectively: no differences were observed among the different subgroups for age, gender distribution, and baseline SBP and DBP. Thiazide diuretic and non-lercanidipine CCBs were equally prescribed as initial drug in 18.1% of the population, followed by ACE inhibitors and β-blockers (17.5%), and ARBs (15.2%). Lercanidipine was prescribed as first-line antihypertensive therapy in 13.2% of patients. About 80% (78.1%) of the patients have been treated with monotherapy for the whole period of observation. Combination treatment was used in a small proportion of patients enrolled in the study (n = 15/347) without significant differences among the various subgroups (Table 1) in the number of patients treated, antihypertensive drug distribution, or drop-in rate (data not shown).
Table 1.
Baseline characteristics of the population
| Diuretics | β-blockers | ACEI | ARB | CCB | Overall | |
|---|---|---|---|---|---|---|
| Pts n. | 63 | 61 | 61 | 53 | 63 | 347 |
| Age (yr) | 59.1 ± 5 | 59.7 ± 6 | 59.6 ± 5 | 58.9 ± 6 | 59.3 ± 6 | 59.4 ± 6 |
| Age > 65 yr (%) | 21(33.3) | 19 (31.1) | 22 (36.0) | 17 (32.0) | 25 (39.7) | 122 (35.1) |
| Gender (M/F) | 36/27 | 34/27 | 32/29 | 30/23 | 38/25 | 206/141 |
| SBP (mmHg) | 156 ± 15 | 157.2 ± 13 | 152.5 ± 12 | 154.3 ± 13 | 153.3 ± 12 | 154.1 ± 12 |
| DBP (mmHg) | 99.3 ± 9 | 100.2 ± 7 | 98.7 ± 8 | 99.1 ± 7 | 97.4 ± 7 | 99.1 ± 7 |
| Heart rate (bpm) | 78 ± 3 | 77 ± 5 | 78 ± 5 | 76 ± 4 | 79 ± 5 | 78.2 ± 4 |
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-II receptor blocker; CCB, calcium-channel blocker.
At 24 months, the percentage of subjects continuing their initial ARB (68.5%) and ACE inhibitor (61.5%) medication was higher than the percentage of those continuing the treatment with CCBs (51.6%; p < 0.05), β-blockers (48.8%, p < 0.05), and thiazide diuretics (34.4%, p < 0.01) (Figure 1). The main reason for drug discontinuation was the occurrence of adverse effects in over two-thirds of the population not achieving the primary end-point of persistence. The main duration of persistence with treatment was: 20.3 ± 9 months for ARBs, 18.7 ± 8 months for ACE inhibitors, 17.1 ± 9 months for CCBs, and 15.8 ± 8 and 14.1 ± 9 months for ß-blockers and thiazide diuretics, respectively (p < 0.005 for trend). No ARB, ACE inhibitor, β-blocker, or diuretic was associated with a higher persistence in therapy compared with the other molecules used in each therapeutic class. Among the subgroup of patients treated with CCBs the rate of stay-on-therapy was higher in those treated with lercanidipine (59.3% vs 46.6%, p < 0.05 vs others CCBs).
Figure 1.
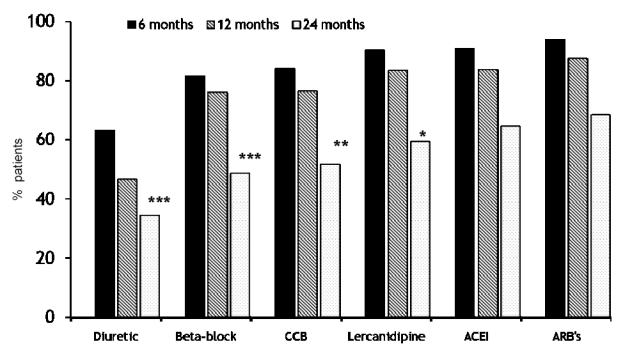
Rate of persistence on treatment after 6,12, and 24 months in different subgroups of patients treated with angiotension-II receptor blockers (ARBs), angiotensin-converting enzyme inhibitors (ACEIs), calcium channel blockers (CCBs), lercanidipine, ß-blockers, and diuretics. *, **, ***p < 0.05, 0.01, 0.005 vs ARBs.
In the logistic regression model of persistence on treatment using ARBs as reference term, patients taking ACE inhibitors were more likely to continue their initial antihypertensive therapy (ACE inhibitors: OR = 0.94, 95% CI: 0.79–0.99) followed by users of CCBs (OR = 0.76; 95% CI: 0.54–0.85), β-blockers (OR = 0.67; 95% CI: 0.57–0.79), and thiazide diuretics (OR = 0.56; 95% CI: 0.38–0.84). Patients treated with lercanidipine (OR = 0.84, 95% CI: 0.61–0.88) were more likely to persist on treatment than patients taking other CCBs (OR = 0.70; 95% CI: 0.51–0.79). There was a clinically uncertain but statistically significant relationship between female sex and continuation of the initial therapy (OR = 1.08; 95% CI: 1.02–1.15, p = 0.006). Age ≥65-years was associated with higher persistence (OR = 0.79; 95% CI: 0.74–0.84; p = 0.001) while the prescription of drugs requiring multiple doses increased the rate of discontinuation when compared with once-daily dosing (OR = 1.40; 95% CI: 1.29–1.52; p = 0.0001).
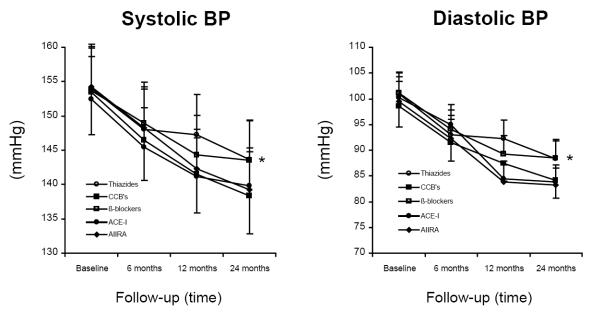
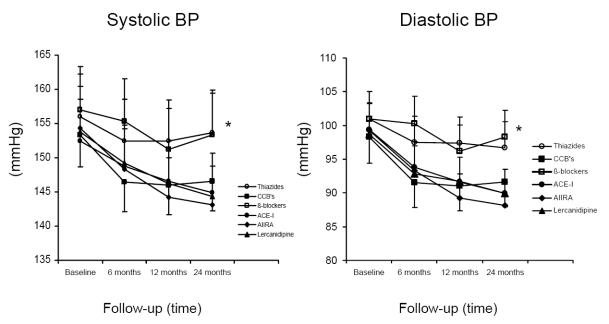
The decrease of SBP and DBP in response to treatment was largely proportional to the rate of persistence on treatment and greater in patients treated with ARBs, ACE inhibitors, and CCBs (Figure 2). The difference was clearly enhanced in those patients in whom the initial treatment was not replaced by a different antihypertensive drug after discontinuation (Figure 3). No ARB, ACE inhibitor, β-blocker, or diuretic was associated with a higher BP control compared with the other molecules used in each therapeutic class. The treatment with lercanidipine was associated with a trend toward a better BP control vs other CCBs with a difference that achieved a statistical significance after 24 months of treatment.
Figure 2.
Systolic blood pressure decrease over 24 months in the overall population of patients (n = 347) initially allocated to the different classes of antihypertensive drugs. *p < 0.05 vs other drug classes.
Abbreviations: ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin-II receptor blockers; CCBs, calcium channel blockers.
Figure 3.
Systolic blood pressure decrease over 24 months in the selected population of patients allocated to different drug classes and not replacing the antihypertensive treatment after withdrawal.
*p < 0.05 vs other drug classes.
Abbreviations: ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin-II receptor blockers; CCBs, calcium channel blockers.
Discussion
The results of the present study confirm that the rate of persistence on initial antihypertensive treatment is prospectively higher for hypertensive patients treated with ARBs and ACE inhibitors as first-line drugs. The extent of persistence on treatment might significantly differ within patients treated with compounds belonging to the same class of drugs but bearing a different tolerability profile (eg, CCBs). In addition, the study supports the evidence that the extent of persistence on treatment influences the clinical outcome of antihypertensive therapy, with a larger BP decrease in those patients treated with drugs leading to a higher rate of stay-on-therapy.
The present findings are in agreement with previously published data demonstrating that the highest rate of long-term (24 months) compliance with antihypertensive therapy can be achieved in patients treated with drugs inhibiting the renin-angiotensin system and CCBs (Blooms 1998). Conversely, Jones et al (1995), who analyzed the United Kingdom MediPlus primary care database, excluded any significant difference in the 6-month rate of continuation in patients treated with the four major classes of antihypertensive drugs (ie, thiazide diuretics, beta-blockers, calcium antagonists, and ACE inhibitors). Unfortunately, most of the available data are retrospective in nature (Blooms 1998; Perrault et al 2005) or based on a short period of observation (Jones 1995) and do not allow any definite conclusion about the differences in persistence with the antihypertensive treatment in clinical practice. Some prospective evidence might be achieved by the analysis of data collected in clinical trials that usually describe a rate of persistence higher than that reported by the present study and ranging from 80% to 90% over a period of 3–5 years (Black et al 1987; Grimm et al 1997). However, large-scale clinical trials usually tend to overestimate the rate of persistence on antihypertensive treatment because of selection bias and behavior reinforcement. And consequently their results cannot be directly applied to clinical practice. The results of the present study have been achieved in a sample of unselected hypertensive patients, treated in agreement with the ESH-ESC European Guidelines (ESH-ESC 2003), and describe a situation largely comparable with the real setting of daily clinical practice.
Interestingly, our results confirm that the rate of stay-on-therapy is higher for the patients treated with the better-tolerated antihypertensive drugs (eg, ARBs, ACE inhibitors). This is in agreement with the clinical observation that for many patients the worsening of the quality of life that follows the use of antihypertensive medications is even more disturbing than the symptomless elevation of BP and might result in the discontinuation of poorly tolerated drugs. We also suggest the possibility that the relationship between the tolerability profile of a drug and the patient’s persistence on treatment might be demonstrated within the same class of antihypertensive drugs. In particular a direct comparison of patients allocated to treatment with CCBs showed a greater persistence on therapy in those subjects treated with lercanidipine whose tolerability profile has been repeatedly demonstrated to be superior when compared with other drugs of the same class (Bang et al 2003; Borghi 2005).
Our findings suggest the importance of persistence on treatment for the management of hypertension. In particular, the higher the proportion of patients who persist on treatment the greater the BP decrease in response to antihypertensive drugs. This supports the hypothesis that the overall impact of the BP-lowering treatment in clinical practice may actually result from the interaction between the absolute antihypertensive effect of drugs and their capacity to positively promote the persistence on treatment. In the hypertensive cohort of the Brisighella Heart Study the proportion of patients who achieved effective BP control over time was directly proportional to the use of ACE inhibitors as first-line drugs and inversely related to the prescription of diuretics (Borghi et al 2004). The better BP control was associated with a lower rate of major cardiovascular events, including coronary artery disease and stroke. Unfortunately, no information on compliance with treatment has been collected in the Brisighella study and, as with all epidemiologic observational studies, this hypothesis requires confirmation in other investigational settings.
Some limitations could reduce the confidence in our observations. In the present study the rate of compliance to treatment was assessed only indirectly as the rate of discontinuation of prescribed treatment and we do not have any specific information about prescription filling or pill count. However, the study was aimed at investigating the extent of persistence on treatment in the “real world” and for this reason we have decided to exclude from the protocol any measure of drug compliance and to focus on the rate of discontinuation as measure of “clinical” compliance. A further limitation is represented by the fact that the study has separately considered only one CCB (lercanidipine) to support the hypothesis that the persistence on treatment might significantly differ among compounds belonging to the same class. The reason for such a choice was the large amount of data that suggests a measurable difference between the tolerability profile of lercanidipine and other CCBs (Basile 2004). Since most of the difference is due to a lower rate of subjective adverse events in patients treated with lercanidipine (from 40% to 50%), this would have increased the chance of detecting a significant difference in the proportion of patients persisting on the same treatment over time.
In conclusion, the results of the present study support a close relationship between the tolerability profile of the different classes of antihypertensive drugs and the long-term persistence on treatment; and show that the rate of stay-on-therapy can significantly differ among patients treated with several classes of first-line antihypertensive drugs with different tolerability profiles even within the same pharmacological family, and that the higher the persistence on treatment the better the extent of BP control in clinical practice. Additional studies are needed to assess whether these differences will be maintained in the following years and whether the differences are associated with better health outcomes.
Disclosures
None of the authors has significant conflict of interest by the publication of this paper. Some years ago, Prof Borghi received funding to support research on lercanidipine efficacy and safety in clinical practice.
References
- Ambrosioni E, Leonetti G, Pessina AC, et al. Patterns of hypertension management in Italy: results of a pharmacoepidemiological survey on antihypertensive therapy. Scientific Committee of the Italian Pharmacoepidemiological Survey on Antihypertensive Therapy. J Hypertens. 2000;18:1691–9. doi: 10.1097/00004872-200018110-00023. [DOI] [PubMed] [Google Scholar]
- Bang LM, Chapman TM, Goa KL. Lercanidipine: a review of its efficacy in the management of hypertension. Drugs. 2003;63:2449–72. doi: 10.2165/00003495-200363220-00013. [DOI] [PubMed] [Google Scholar]
- Basile J. The role of existing and newer calcium channel blockers in the treatment of hypertension. J Clin Hypertens. 2004;6:621–29. doi: 10.1111/j.1524-6175.2004.03683.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckey C, Lundy A, Lutfi N. Lercanidipine in the treatment of hypertension. Ann Pharmacother. 2007;41:465–73. doi: 10.1345/aph.1H299. [DOI] [PubMed] [Google Scholar]
- Black DM, Brand RJ, Greenlick M, et al. Compliance to treatment for hypertension in elderly patients: The SHEP pilot study. J Gerontol. 1987;42:552–7. doi: 10.1093/geronj/42.5.552. [DOI] [PubMed] [Google Scholar]
- Blooms BS. Continuation of initial antihypertensive medication after 1-year of therapy. Clin Ther. 1998;20:671–81. doi: 10.1016/s0149-2918(98)80130-6. [DOI] [PubMed] [Google Scholar]
- Borghi C, Dormi A, D’Addato S, et al. Brisighella Heart Study Working Party. 2004. Trends in blood pressure control and antihypertensive treatment in clinical practice: the Brisighella Heart Study. J Hypertens. 2004;22:1707–16. doi: 10.1097/00004872-200409000-00014. [DOI] [PubMed] [Google Scholar]
- Borghi C. Lercanidipine in hypertension. Vasc Health Risk Manag. 2005;1:173–82. [PMC free article] [PubMed] [Google Scholar]
- Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190–6. doi: 10.1016/j.amjhyper.2006.04.006. [DOI] [PubMed] [Google Scholar]
- David DS. Compliance with hypertensive therapy. Hypertension. 2006;48:E16. doi: 10.1161/01.HYP.0000239674.65561.7f. [DOI] [PubMed] [Google Scholar]
- Erdine S, Ari O, Zanchetti A, et al. ESH-ESC guidelines for the management of hypertension. Herz. 2006;31:331–8. doi: 10.1007/s00059-006-2829-3. [DOI] [PubMed] [Google Scholar]
- ESH-ESC. European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. Guidelines Committee. J Hypertens. 2003;21:1011–53. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- Fujita T, Shimamoto K, Wu Z, et al. What are the major challenges in getting patients to the optimal BP goal? Difficulties in educating doctors and patients. Int J Clin Pract Suppl. 2006;150:20–2. [Google Scholar]
- Grimm RH, Jr, Grandits GA, Cutler JA, et al. Relationships of quality-of-life measures to long-term lifestyle and drug treatment in the Treatment of Mild Hypertension Study. Arch Intern Med. 1997;157:638–48. [PubMed] [Google Scholar]
- JNC VII. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Jones JK, Gorkin L, Lian JF, et al. Discontinuation or and changes in treatment after start or new courses or antihypertensive drugs: a study or a United Kingdom population. BMJ. 1995;311:293–5. doi: 10.1136/bmj.311.7000.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCombs IS, Nichol MB, Newman CM, et al. The costs or interrupting antihypertensive drug therapy in a Medicaid Population. Med Care. 1994;32:214–26. doi: 10.1097/00005650-199403000-00003. [DOI] [PubMed] [Google Scholar]
- Messerli FH. Calcium antagonists in hypertension: from hemodynamics to outcomes. Am J Hypertens. 2002;15:94S–97S. doi: 10.1016/s0895-7061(02)02950-3. [DOI] [PubMed] [Google Scholar]
- Monane M, Bohn RL, Gurwitz JH, et al. The effects or initial drug choice and comorbidity on antihypertensive therapy compliance: Results from a population based study in the elderly. Am J Hypertens. 1997;10:697–704. doi: 10.1016/s0895-7061(97)00056-3. [DOI] [PubMed] [Google Scholar]
- Okano GJ, Rascati KL, Wilson JP, et al. Patterns or antihypertensive use among patients in the US Department or Defence database initially prescribed an angiotensin-converting enzyme inhibitor or calcium channel blocker. Clin Ther. 1997;19:1433–44. doi: 10.1016/s0149-2918(97)80017-3. [DOI] [PubMed] [Google Scholar]
- Poluzzi E, Strahinja P, Vargiu A, et al. Initial treatment of hypertension and adherence to therapy in general practice in Italy. Eur J Clin Pharmacol. 2005;61:603–9. doi: 10.1007/s00228-005-0957-y. [DOI] [PubMed] [Google Scholar]
- SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: Final results of the Systolic Hypertension in the Elderly Program (SHEP) JAMA. 1991;265:3255–64. [PubMed] [Google Scholar]
- Staessen JA, Li Y, Thijs L, et al. Blood pressure reduction and cardiovascular prevention: an update including the 2003–2004 secondary prevention trials. Hypertens Res. 2005;28:385–407. doi: 10.1291/hypres.28.385. [DOI] [PubMed] [Google Scholar]
- Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43:10–17. doi: 10.1161/01.HYP.0000103630.72812.10. [DOI] [PubMed] [Google Scholar]