Abstract
Objective
We evaluate the 6-month efficacy of Keep Active Minnesota, a phone and mail-based physical activity maintenance intervention designed for use with adults age 50 to 70 years who have increased their physical activity (PA) within the past year.
Method
Participants (N=1,049) recruited in 2004 and 2005 from one large managed care organization in Minnesota, were randomly assigned to either treatment (KAM; N=523), or usual care (UC; N=526) with PA assessed using the CHAMPS questionnaire, and expressed as kcal/wk expenditures.
Results
Total PA at baseline was similar for KAM and UC participants (p < .44) as was moderate/vigorous PA (p < .21). Maintenance of PA was higher among KAM participants whose mean 6 month change in total kcal/wk energy expenditure was −91 , compared to −683 for UC participants (p < .002). Mean 6 month change in kcal/wk expenditure in moderate or vigorous activities was −49 for KAM participants, compared to −612 for UC participants (p < .001).
Conclusions
This phone- and mail-based PA maintenance intervention is efficacious at maintaining PA at 6 months.
Keywords: intervention studies, motor activity, behavioral research, health maintenance organizations, randomized controlled trial
Introduction
Substantial data document the benefits of physical activity (PA), particularly in older adults. Positive effects of moderate intensity PA have been demonstrated with respect to a variety of outcomes that are particularly salient in older adult populations, including: functional status(Unger et al., 1997, Brach et al., 2004), balance(Lord et al., 1995), weight management(Hills and Byrne, 1998), insulin sensitivity and glucose tolerance(Mayer-Davis et al., 1998, Tuomilehto et al., 2001, Cox et al., 2004), inflammatory markers(Colbert et al., 2004), blood pressure(Pescatello et al., 2004), cognitive function(Weuve et al., 2004), reduced risk of hip fracture in postmenopausal women (Feskanich et al., 2002), lower body arthritis pain(Hughes et al., 2004), and cardiovascular fitness.(Dunn et al., 1999, Stofan et al., 1998, Blair et al., 1992) Physical activity also has a beneficial impact on quality of life through its impact on physical and mental health status(McAuley et al., 2006, Elavsky et al., 2005), and most recently, objectively measured, free-living activity energy expenditure has been shown to reduce mortality risk in healthy older adults.(Manini et al., 2006)
Yet, sedentary behavior remains a significant and serious health problem in the U.S. and is particularly prevalent among older adults. The 2005 Behavioral Risk Factor Surveillance System (BRFSS) documents that among adults age 45−54, more than half (52%) were obtaining less than recommended levels of physical activity, with the same being true for 55% of adults age 55−64.(Centers for Disease Control and Prevention (CDC), 2005) Healthy People 2010 (Objective 22−1) aims to reduce to 20% or less the proportion of persons reporting no leisure-time PA.(DHHS, 2000) To accomplish this objective, health plans and public health policy makers are seeking strategies to increase levels of PA in a broad spectrum of the U.S. population. Such interventions must be low cost, produce long-term behavior changes, and be able to deeply penetrate the target population.
Complementary strategies to reach national PA goals include efforts to increase the number of sedentary individuals who initiate PA and efforts to increase the number of physically active individuals who successfully maintain beneficial levels of PA for a substantial length of time. The importance of efforts to maintain PA is underscored by recent reports that roughly half of older adults who initiate a program of PA discontinue within three months.(Dishman, 1994) These data, coupled with the observation that prevalence of sedentary behavior increases with age,(CDC, 2005) suggests that population levels of PA may be substantially increased by preventing currently active individuals from falling below recommended levels of physical activity. It is problematic, therefore, that most prior efforts to promote PA have not focused more on maintenance. Efforts to increase physical activity among the sedentary are certainly worthwhile, but we feel it is a mistake to assume that those already attempting to be physically active are not also at risk of relapse into more sedentary habits.
Most physicians are painfully aware of the flux over time in their patients' health-related behaviors and the inability of many patients to sustain healthy lifestyles.(Helseth et al., 1999) The efficacy of clinic-based approaches to increasing PA is equivocal, with some studies indicating positive results,(Eaton and Menard, 1998) but the majority reporting lack of benefit.(Bull et al., 1999, Goldstein et al., 1999, Walsh et al., 1999) More recent studies linking brief primary care based advice/counseling with referrals to phone-based counseling by activity specialists have demonstrated substantial promise, with positive effects on potential determinants of PA(van Sluijs et al., 2005), on short-term increases in PA(Harrison et al., 2005, Pinto et al., 2005b), sustained increases in PA, and on health related quality of life(Anderson et al., 2005b) and functioning(Kerse et al., 2005). However, approaches to increasing PA that start in the clinic are relatively expensive, difficult to implement in busy practice settings, and have limited reach to some patient populations.
Population based approaches may be a more effective and efficient strategy to increase levels of PA in adults. A recent review of the literature suggests that home-based and group-based interventions increase activity in the short-term, and supports the hypothesis that community based interventions may be viable alternatives to clinic based approaches.(Van der Bij et al., 2002) With a few exceptions(Castro et al., 2001, McAuley et al., 2007), most intervention efforts have remained focused on PA initiation (Pinto et al., 2005a, Motl et al., 2005, Rejeski et al., 2005, Stewart et al., 2001b, Ackermann et al., 2005, Morgan, 2005, Cyarto et al., 2004, Leveille et al., 1998, Stewart et al., 1998, Harrison et al., 2005, Kerse et al., 2005) and a greater emphasis on maintenance of increased PA levels is needed, as ongoing participation in PA is necessary to sustain health benefits. More programs are needed for older adults that incorporate moderate intensity PA and are simple, convenient to engage in, relatively inexpensive, and noncompetitive .(King et al., 2000)
We address these issues by evaluating the efficacy of a population-based approach to promoting PA maintenance among currently active older adults whose baseline level of activity represented an increase within the past year. Participants randomized into the intervention were offered an interactive telephone and mail-based physical activity support program. Moreover, focusing on this group allows us to intervene with individuals at a point in their life-course when the prevention of disease onset and slowdown in the pace of disease progression can often be achieved through primary and secondary prevention.(Knowler et al., 2002, Hansson et al., 1998) Participants were recruited as inclusively as possible from membership in a health plan in order to maximize the generalizability of findings. Our primary goal was to assess the extent to which the intervention would help participants maintain the level of activity they reported at baseline, over a period of two years. We present here the primary and secondary outcomes at the six-month follow-up point and intervention participation data.
The analyses of physical activity at 6 months were conducted after study recruitment was completed so that neither the sample size, the assignment of participants to study groups, nor the manner in which the intervention was delivered could possibly be influenced by knowledge of the short term impact of the intervention on physical activity. Moreover, the outcomes examined are independent of the overall study outcomes at 24 months. Thus what we present here are not interim analyses, even though intervention and follow-up measurements were ongoing at the time they were conducted.
Hypothesis 1
Intervention group participants will maintain kcal expenditure from baseline to 6 months, relative to a drop in kcal expenditure among the usual care comparison group.
Hypothesis 2
PA maintenance at 6 months will be higher among intervention group participants than among those in the usual care group
Methods
Target Population
The study was conducted among 50−70 year old members of one large managed care organization (HealthPartners) in the Minneapolis/St. Paul metropolitan area.
Eligibility, Sampling, and Recruitment
We used health plan administrative records to identify members who were ages 50 through 70 and had been enrolled in the health plan for at least 11 of the 12 months prior to screening for study eligibility. Among those meeting the enrollment criteria, those who shared a household with an enrolled participant, those with a modified Charlson comorbidity score > 3 (a standard index of comorbidity calculated using prior year diagnoses of a broad range of serious medical conditions),(Rush et al., 2000, Charlson et al., 1994) as well as those who had diagnoses of coronary heart disease (CHD), congestive heart failure (CHF), atrial or ventricular arrhythmias, cardiac arrest, or had an implantable defribillator were excluded. Members who reported that they were currently accumulating at least 30 minutes of moderate or vigorous PA a day at least 2 days per week on average over the past four weeks, and had increased to this level of PA within the past 12 months, no matter whether on their own or through a program, were considered study eligible. The minimum of two days per week of moderate intensity PA is a clinically relevant cutoff, since regular PA at this level has been shown to generate significant improvements in functional capacity, fasting insulin levels, and other health-related variables(Bouchard et al., 1994, Haskell, 1994, Irwin et al., 2000) and to reduce risk of Type 2 diabetes in women.(Hu et al., 1999)
Recruitment was initiated through a direct mailing procedure, supplemented by “self referral” recruitment, facilitated through study advertisement. Direct mailings were sent to random samples of age-eligible health plan members not meeting the exclusion criteria. The mailings assessed their interest in study participation, and included brief screening questions about their current level of physical activity. Interested members were asked to complete the brief screener and return to us in business reply envelopes. Eligible members were contacted by telephone to confirm their interest in study participation and to conduct an initial consent discussion. Following this discussion, consent forms were mailed to interested individuals who were asked to read, sign, and return a consent form. When completed consent forms were received a baseline telephone interview was scheduled with the participant, upon completion of which the subject was randomized to either the treatment or control condition.
Brief advertisements for the study were included in one issue of a regular, quarterly mailing sent to all HealthPartners members, as well as on the HealthPartners website. E-mail advertising of the study was conducted in several large employer groups that purchase health insurance from HealthPartners. Advertisements included basic information about the study, age and physical activity eligibility criteria and a phone number that they used to contact study personnel. Individuals contacting this number were screened by phone to determine their eligibility with respect to their physical activity and their health status. Those found eligible were engaged in a brief consent discussion and proceeded through the enrollment process in the same manner as those recruited by direct mail. Including a pilot phase running from September 2004 through November 2004, recruitment occurred over 15 months, ending in December of 2005.
Design
We randomized N=1,049 subjects (1:1) to either the PA treatment condition (KAM) or a usual care control group (UC). Participants were randomized by the study coordinator as they enrolled according to a schedule pre-determined by the study statistician and unobservable to the staff conducting randomization, based on a random number table embedded in the backend of the recruitment tracking database. Blocks of 20 were used to maintain study arm balance throughout the recruitment period. Participants in both groups self-reported their physical activity levels at baseline and at 6, 12 and 24 month follow-ups so that the primary study outcomes, absolute level of physical activity expressed as kcal/wk of energy expenditure and maintenance of physical activity levels relative to baseline, could be assessed over the course of the two years following baseline. Study group assignment was not revealed to the phone interviewers collecting the self-report data.
KAM Intervention Description
Participants randomized into the intervention were offered an interactive telephone and mail-based physical activity support program. The intervention was based primarily on the principles of Bandura's Social Cognitive Theory (SCT).(Bandura, 1986, Bandura, 2004) and relapse prevention theory.(Marlatt and Gordon, 1985) Because the focus of the intervention was on maintenance as opposed to initiation, intervention strategies were weighted heavily toward self-management, including cognitive (goal setting, identification of barriers and problem solving), behavioral (self-monitoring through use of pedometers & log-books, use of environmental cues), and environmental (phone coach support, development and leverage of social support) strategies. The core component of the intervention is a seven session course delivered over the phone by activity coaches with a background in exercise science and training in behavior change theory.
Following completion of the course, participants receive monthly follow-up calls for the remainder of the first year of study participation and then bi-monthly calls for the second year. Additional intervention components include motivational campaigns and a lending library of physical activity resources. This report focuses on the core 7 session course; subsequent reports of 12- and 24-month outcomes will describe the other intervention components in detail.
After randomization, intervention participants were invited to attend an in-person group orientation session to meet their activity coach and other study staff, to review the study goals and materials and to discuss the intervention process. Sessions were held about once a month and everyone who attended the session received a copy of the course workbook, a 52 week log book for monitoring activity and recording goals, a t-shirt with the study logo and a Yamax pedometer. Those who were unable to attend an in-person orientation received the information over the phone and the course materials were mailed.
Each course workbook session included topics to be covered during the phone coaching session, instructional material, assignments for participants to work through on their own and goal setting. Participants were encouraged to use their pedometer to monitor their physical activity, however, they could also choose to self-monitor their physical activity in whatever way would be useful to them (e.g., minutes, miles). Course session topics included: the benefits of physical activity; goal setting and the development of an action plan; a discussion of types of physical activity and exercise; overcoming barriers to physical activity, problem solving and enhancing self-efficacy; social support; healthy eating; relapse prevention; and developing an action plan for long term maintenance.
The sessions were scheduled at the participant's convenience, designed to last about 20 minutes, to take place about twice a month and to be personalized for each participant based on their current physical activity level, physical activity goals and any barriers they were experiencing, including injury or health limitations. Participants received the same set of core intervention materials, however, they were occasionally sent supplementary materials to support their physical activity goals (e.g., information on strength training, classes in their local community). Additionally, in fewer than ten cases, a participant's physician was consulted to ensure that it was safe to continue taking part in the intervention.
The course sessions were set up so that goals from the last session were initially reviewed along with any questions or concerns about previous topics. Then the topic of the session along with the accompanying homework was discussed. Activity coaches provided feedback and encouragement, helped with problem solving and encouraged the participant to revise their physical activity goals, if needed.
Measures
All primary and secondary outcome measures were collected during a 45 minute telephone interview administered prior to randomization (baseline) and 6 months later. Follow-up interviews were scheduled at the participant's convenience 5 to 7 months post-baseline. Participant responses were recorded by the interviewer onto an optically scannable form that was scanned following administration.
Primary outcomes
The primary outcome measures in these analyses were kilocalories expended per week on a range of activities (total kcal/wk) and kilocalories expended per week on a subset of moderate and vigorous activities (moderate kcal/wk), calculated at baseline and 6 months; and maintenance of PA at 6 months relative to baseline (maintenance). Both kcal expenditure measures were computed using the CHAMPS instrument, designed for use in adult populations such as this one to assess the self-reported frequency and duration of a range of common activities and convert these reports into weekly kcal expenditure.(Stewart et al., 2001a) The CHAMPS instrument has demonstrated acceptable reliability with ICCs for moderate intensity activities of 0.67, 0.76, and 0.81−0.88 at six months, two weeks, and one week, respectively. Higher intensity activities demonstrate more modest ICCs of 0.66, 0.62, and 0.34−0.45 at six months, two weeks, and one week, respectively.(Stewart et al., 2001a, Cyarto et al., 2006) The instrument has also demonstrated adequate discriminant and construct validity, correlates well with other measures of physical activity and is sensitive to change.(Stewart et al., 2001a) Participants were coded as having maintained PA if at 6 months their moderate kcal expenditure was at least 1500kcal/wk and at least 80% of that expended at baseline.
Secondary outcomes
PA outcomes at baseline and 6 months assessed whether participants met CDC/ACSM physical activity recommendations of 30 minutes of moderate activity 5 or more days per week (moderate); 20 minutes of vigorous activity at least 3 days per week (vigorous); and moderate or vigorous activity recommendations.(Pate et al., 1995) Body mass index (BMI; kg/m2) was calculated from baseline and 6 month self-reported height and weight.
Predictors
Randomly assigned treatment group (KAM n=523, UC n=526) was the sole predictor in the primary and secondary efficacy analyses. Additional analyses among intervention participants assessed whether amount of participation in the KAM intervention was associated with physical activity levels or maintenance. Two predictors indicated whether participants were early completers, having completed 0−6 (n=315) or all 7 (n=208) KAM sessions prior to the 6 month follow-up; or had completed 1−4 (n=119) or 5−7 (n=365) KAM sessions by this time.
Analysis plan
Preliminary examination of the kcal expenditure measures at baseline and 6 months revealed outlying observations at each time point. Kcal expenditure observations greater than 5 standard deviations from the median at each time point were excluded from the analyses (total kcal n=3 at baseline, n=2 at 6 months; moderate kcal n=4 at baseline, n=4 at 6 months). Kcal and maintenance outcomes were missing at 6 months from n= 35 control and n=28 intervention participants who did not complete the 6 month survey, p=.38.
We used a general linear mixed model regression (time within participant, unspecified covariance structure, restricted maximum likelihood estimation) to test the hypothesis that KAM participants maintained kcal expenditure from baseline to 6 months, relative to a drop in kcal expenditure among the UC participants. Total and moderate kcal were separately predicted from the time at which kcal was measured (6 months, baseline), which varied within participants, and randomized treatment group (KAM, UC), which varied across participants. This intent to treat approach ensured that all available kcal observations, excluding those greater than 5 SD above median, from all randomized participants were used to estimate model parameters (n=2031 total kcal observations; n=2028 moderate kcal observations).
The UC group and baseline measurement were the reference categories in the mixed regression models. The KAM parameter tested whether the KAM and UC groups were different at baseline while the 6month parameter tested whether the UC group increased or decreased PA at 6 months relative to baseline. The 6month*KAM interaction parameter tested whether there was a larger increase, or a smaller decline, in expended kcal/wk from baseline to 6 months among KAM compared to UC participants, which would point to success of the KAM intervention in helping participants maintain physical activity.
Sample size was based on that which would be needed to detect a time (24 month vs. baseline observation) by treatment (KAM vs. UC) interaction at .80 power (two-tailed, alpha = 0.05) on the total kcal/wk variable in a two group repeated measures ANOVA. We assumed a common standard deviation of 1500 kcals/wk at each of 4 time points and a first order autoregressive residual covariance structure. These parameters suggested that N=349 per study arm would be needed to detect the interaction of primary interest . Assuming non-differential 70% retention across study groups, we recruited N=500 per arm.
Results
Sample Characteristics
With respect to age and race/ethnicity, those who enrolled in the trial were reasonably representative of the pool of age eligible health plan members from which we recruited, who were themselves reflective of the local community. Enrollees were age 57 on average, which is identical to the average age of the pool of potentially eligible respondents in the age range 50 through 70 identified in the health plan. While 94% of study participants self identified as white, 3% identified as black, 1% as Asian, and 1% as other, mixed-race, or did not answer this question. Hispanic or Latino participants comprised 2% of enrollees. As is often the case in behavioral intervention studies, women were more likely to participate than men. Specifically, while 72% of participants were female, only 49% of the total recruitment pool was female.
Randomization was successful in creating groups that were similar on numerous demographic characteristics. Table 1 demonstrates that at baseline the typical participant was about 57 years old, female, White, overweight(BMI ≥ 25 kg/m2), working full time, and college educated. Many were participating in another physical activity program and few reported fair or poor functional health status. The only observed difference between the groups was that fewer KAM participants self-identified as White (95.6 vs. 92.4%, p<.05).
Table 1.
Participant Characteristics as Mean and Standard Error or Percent by KAM and Usual Care Groups
| UC | KAM | All | |
|---|---|---|---|
| N | 526 | 523 | 1049 |
| age at baseline | 57.1(.22) | 57.1(.22) | 57.1(.16) |
| female | 71.9 | 72.9 | 72.4 |
| BMI, kg/m2 | 27.7(.24) | 27.5(.23) | 27.6(.17) |
| White | 95.6 | 92.4* | 94.0 |
| Black | 2.8 | 3.8 | 3.3 |
| American Indian | 0.2 | 0.2 | 0.2 |
| Asian | 0.6 | 1.2 | 0.9 |
| Multiple | 0.6 | 1.2 | 0.9 |
| Other | 0.0 | 0.6 | 0.3 |
| Unknown | 0.2 | 0.8 | 0.5 |
| Hispanic / Latino | 1.2 | 2.5 | 1.8 |
| employed full time | 76.6 | 77.1 | 76.8 |
| 4 year degree or more | 65.8 | 67.7 | 66.7 |
| participating in another activity program | 35.2 | 34.7 | 35.0 |
| functional health status fair or poor | 5.7 | 6.7 | 6.2 |
KAM vs. UC, p<.05
(Study conducted in participants recruited from one health plan in Minnesota during 2004 and 2005.)
Primary outcomes by treatment group
The upper half of Table 2 displays for total and moderate kcal the baseline and 6 month means and standard errors by treatment group as well as the significance of the treatment (KAM vs. UC), time (6 months vs. baseline) and treatment*time (6 months vs. baseline among KAM vs. UC) parameters. The proportion who maintained PA at 6 months and the significance of the treatment effect are also displayed. The lower half of Table 2 displays similar information for the secondary outcomes, percent meeting ACSM recommendations and mean BMI.
Table 2.
Mean and standard error or percent for primary and secondary outcomes by KAM and UC groups at baseline and 6 months, and significance (2-tailed t- or chi-squared test) of KAM, 6 month and KAM*6 month parameters.
| Usual Care | KAM | parameter | |||||
|---|---|---|---|---|---|---|---|
| baseline | 6 months | baseline | 6 months | KAM | 6 months | KAM*6 months | |
| N | 526 | 491 | 523 | 495 | |||
| primary outcomes |
|
|
|
|
|
|
|
| total | 4781 | 4108 | 4643 | 4549 | p=.44 | p<.001 | p<.002 |
| kcal/week | (114.0) | (121.9) | (109.2) | (119.2) | |||
| moderate | 2898 | 2287 | 2730 | 2680 | p=.20 | p<.001 | p<.001 |
| kcal/week | (93.7) | (92.0) | (83.4) | (90.6) | |||
| maintenance | 36.3 | 50.8 | p<.001 | ||||
| secondary outcomes |
|
|
|
|
|
|
|
| moderate PA | 27.8 | 28.5 | 21.4 | 33.5 | p<.03 | p=.82 | p<.004 |
| 5+ days/week | |||||||
| vigorous PA | 35.0 | 42.5 | 36.7 | 47.3 | p=.58 | p<.02 | p=.52 |
| 3+ days/week | |||||||
| BMI (kg/m2) | 27.70 | 27.67 | 27.53 | 27.36 | p=.59 | p=.20 | p=.54 |
| (.24) | (.25) | (.23) | (.24) | ||||
(Study conducted in participants recruited from one health plan in Minnesota during 2004 and 2005.)
Total kcal expenditure was not different between UC (M=4781) and KAM (M=4643) participants at baseline, βKAM = −124, t = −0.77, ns. However, total kcal expenditure dropped markedly between baseline and 6 months among UC participants (M=4108), β6months = −673, t = −5.19, p<.001, but much less among KAM participants (M=4549), βKAM*6months = 570, t = 3.11, p<.002. A similar pattern of effects obtained for moderate and vigorous activity. Moderate kcal expenditure between the UC (M=2898) and KAM (2730) participants was not significantly different at baseline, βKAM = −160, t = −1.27, ns. Between baseline and 6 months, UC participants reduced their moderate kcal expenditure (M=2287), β6months = −603, t = −6.09, p<.001 significantly more than KAM participants (M=2680), βKAM*6months = 544, t = 3.89, p<.001 . The intervention also appeared to be effective in helping participants maintain moderate to vigorous activity. About half of the KAM participants (50.8%) maintained PA at 6 months compared to 36.3% of UC participants (odds ratio 1.81, χ2 = 20.67,p<.0001).
Secondary outcomes by treatment group
The intervention was effective in helping KAM participants increase the number of days per week on which they engaged in at least 30 minutes of moderate intensity activity. More participants in the UC (27.8%) than the KAM (21.4%) group engaged in 30 minutes of moderate activity at least 5 days per week at baseline, bKAM = −.350, t = −2.25, p<.03. The proportion of UC meeting the ACSM moderate activity criterion remained stable among the UC participants (28.5%), b6months = .032, t = 0.22, ns, but increased (33.5%) among KAM participants, bKAM*6months = .604, t = 2.97, p<.004.
The proportion of participants meeting ACSM recommendations for vigorous activity was not influenced by the intervention. At baseline, 35.0% of UC and 36.7% of KAM participants reported engaging in 20 minutes of vigorous activity at least 3 days per week, bKAM = .079, t = 0.55, ns. Both groups reported increases in vigorous activity (UC 42.5%, KAM 47.3%), b6months = .336, t = 2.53, p<.02, but this increase was not significantly larger among KAM participants, bKAM*6months = .121, t = 0.65, ns. There were no differences in self-reported BMI at baseline or 6 months among UC or KAM participants.
Primary outcomes by intervention participation
Ninety two percent (n=484) of participants assigned to the intervention condition completed at least one phone course session by the six month measurement point. The mean number of course sessions completed by intervention participants was 5.12 (SE=.10) with 39.8% of intervention participants completing the 7 session phone course during this time period. Relative to participants who only completed 1−4 of the phone course sessions (n=119), those who completed 5−7 sessions (n=365) were older, had lower BMI, were less likely to be employed full time or report a fair or poor functional health status, and were more likely to have a 4 year degree. Table 3 shows associations between level of intervention participation and physical activity and weight outcomes. Participants who completed the 7 session phone course prior to the 6 month follow-up reported a significantly larger increase in total (p < .006) and moderate (p<.01) kcal expenditure relative to those who did not complete the phone course. Course completers also lost significantly more weight (p < .03) compared to those who had not yet completed the course. Level of course participation was also moderately associated with physical activity outcomes. Participants who completed 5−7 sessions reported significantly more increase in total (p<.02) and moderate (p<.005) kcal expenditure between baseline and 6 months relative to those who had only completed 1−4 sessions at the six month measurement point. No significant weight change differences were observed between these two groups of participants.
Table 3.
Mean and standard error or percent for physical activity and weight outcomes by phone course status at baseline and 6 months, and significance (2-tailed t-test) of complete, 6 month and complete*6 month parameters.
| completed course prior to 6 month follow-up | |||||||
|---|---|---|---|---|---|---|---|
| not complete | complete | parameter | |||||
| baseline | 6 months | baseline | 6 months | complete | 6 months | complete*6 months | |
| total | 4797 | 4427 | 4411 | 4718 | p<.08 | p<.02 | p=.006 |
| kcal/week | (146.8) | (159.9) | (160.5) | (178.0) | |||
| moderate | 2832 | 2582 | 2577 | 2818 | p=.12 | p<.04 | p<.01 |
| kcal/week | (106.7) | (120.3) | (133.4) | (137.4) | |||
| BMI (kg/m2) | 27.7 | 27.6 | 27.3 | 27.0 | p=.48 | p=.87 | p<.03 |
| (0.32) | (0.34) | (0.33) | (0.32) | ||||
| course status at 6 months1 | |||||||
|---|---|---|---|---|---|---|---|
| 1−4 sessions | 5−7 sessions | parameter | |||||
| baseline | 6 months | baseline | 6 months | 5−7 sessions | 6 months | 5−7 sessions*6 months | |
| total | 4921 | 4327 | 4462 | 4565 | p<.08 | p=.02 | p<.02 |
| kcal/week | (254.0) | (285.4) | (125.3) | (132.3) | |||
| moderate | 2859 | 2328 | 2621 | 2728 | p=.22 | p<.01 | p<.005 |
| kcal/week | (174.4) | (200.8) | (99.2) | (102.5) | |||
| BMI (kg/m2) | 28.7 | 28.7 | 27.1 | 26.9 | p<.004 | p=.97 | p=.21 |
| (0.56) | (0.61) | (0.26) | (0.26) | ||||
Excludes participants who completed 0 sessions.
(Study conducted in participants recruited from one health plan in Minnesota during 2004 and 2005.)
Discussion
This relatively low intensity telephone and mail-based physical activity maintenance intervention is one of the first studies to attempt to maintain physical activity levels among adults ages 50 to 70 years who had recently increased their physical activity in a community setting. Focusing on maintenance instead of adoption of physical activity, the intervention was designed to increase the proportion of adults age 50 to 70 years who maintained physical activity levels in the recommended range. Compared to UC subjects, those who received the intervention had significantly higher mean energy expenditures (roughly 450 Kcal/week) 6 months after randomization, after adjusting for baseline energy expenditure. The magnitude of the difference in PA between groups is statistically significant and sufficient to be clinically meaningful. We observed modest weight losses that were comparable between intervention and control subjects. Within the intervention group, those who completed the phone coaching course lost significantly more weight than those who did not complete the course.
Client satisfaction with the intervention was high with low dropout in both in the intervention (3.4%) and control (4.8%) groups, indicating that differences observed were unlikely due to differential drop out, and that the intervention strategy may have wide appeal to eligible adults.
The intervention is based on a theoretical model specifically developed to address issues related to PA maintenance. This model included consideration of factors that predispose those who are physically active to quit, including injury, changes in motivational level, lack of accountability, and lack of encouragement. This model appears to be relatively effective as a guide for successful intervention strategies, which could be developed for other target groups of adults and adapted to other behavioral outcomes. By focusing on maintenance of PA, we intentionally recruited subjects to the study who were at a more advanced stage of change and who may have been more highly motivated than is typical of participants in prior PA interventions. By contrast, our use of direct mail recruitment as the first line recruitment strategy may have reduced the volunteer bias that often results from less proactive, more traditional recruitment strategies such as use of advertisements. Although we, too, made use of advertisement and self-referrals as a second line recruitment strategy, only 21% of those enrolled came to the study through self-referral.
Thus far, only one published randomized controlled study has demonstrated a long-term (2 year) improved activity outcome following a lifestyle intervention approach (versus a traditional structured exercise approach) to increase PA(Dunn et al., 1999). In this study, previously sedentary healthy adults effectively increased their lifestyle based PA over the first 6 months of treatment and subsequently maintained this gain over the following 18 months. This study was limited to middle-aged adults, and participants were required to attend weekly meetings for the first 16 weeks, then biweekly until week 24. This relatively resource intensive approach is not likely to meet the cost and penetration criteria for a successful population-based intervention,(Glasgow et al., 1999) suggesting the need for alternative methods. Telephone-based counseling is one promising alternative approach with an increasing evidence base(Eakin et al., 2007). As emphasized earlier, maintaining PA in those already active may be as important, or more important, than effective interventions to initiate activity in the sedentary. For this reason, the intervention we report, with its promising short-term results, represents an important advance in the overall effort to raise levels of PA in the U.S. population. In addition, while the success of health care providers at increasing physical activity among patient populations has been mixed, our findings suggest a possible role for health care providers in maintaining physical activity gains by encouraging continued PA efforts among their currently active patients through efforts such as verbal support and encouragement and positive role modeling. Given the time pressure and demands already placed on primary care physicians, implementing sustainable phone based coaching programs will likely require the development of parallel support systems, integrated with primary care, but with dedicated staff specially trained to perform these functions to whom clinicians may refer their patients.(O'Connor and Pronk, 1998, Pronk and O'Connor, 1997, Pronk et al., 2002a) Examples of attempts to accomplish this include the work of HealthPartners own Health Behavior Group, and at a national level, the Green Prescription program in New Zealand.(Kerse et al., 2005) Clearly, at this point, dissemination research is a logical next step in moving such programs into population health practice(Eakin et al., 2007), one component of which includes building the business case for such programs by documenting the costs of behavioral factors such as inactivity and overweight/obesity.(Pronk et al., 2002b, Pronk et al., 1999, Anderson et al., 2005a, Jeffery et al., 2003, Martinson et al., 2003, Sherwood et al., 2006)
The interpretation of the data are limited by several factors. First, the intervention requires evaluation over longer follow-up periods, which is now underway. Second, generalization of results to other populations should be done with caution due to the likelihood of self-selection that is a threat to external validity in most clinical trials, as well as the added potential for self-selection stemming from the fact that our inclusion criteria required participants to be currently physically active at an increased level relative to some point in the recent past. Third, although the intervention appealed to a large number of those eligible to enroll in the study, multiple strategies are needed to assure the broad population penetration needed to increase overall population levels of PA. Fourth, it should be noted that the comparisons of subgroup results within the intervention condition presented in Table 3 are observational, precluding inferences about causation. Finally, although this was a low-intensity intervention, the costs of it are not negligible, affordability should be considered for those identified as potential payers, and the significance of the results will be need to be assessed in the context of a planned cost-effectiveness analysis, once longer term impact on PA is fully assessed.
Despite these limitations, the results are interesting and have important clinical and public health implications, because they demonstrate both the practicality and the short-term efficacy of an intervention specifically designed to maintain PA in those who are already active. It is likely that the only feasible way to reach national PA goals is to couple interventions that maintain activity with others that effectively encourage initiation and adoption of PA among the sedentary. Thus, the demonstration of a promising and conceptually coherent approach to PA maintenance adds a potentially efficacious strategy to the relatively few proven strategies already available for increasing PA in the adult population.
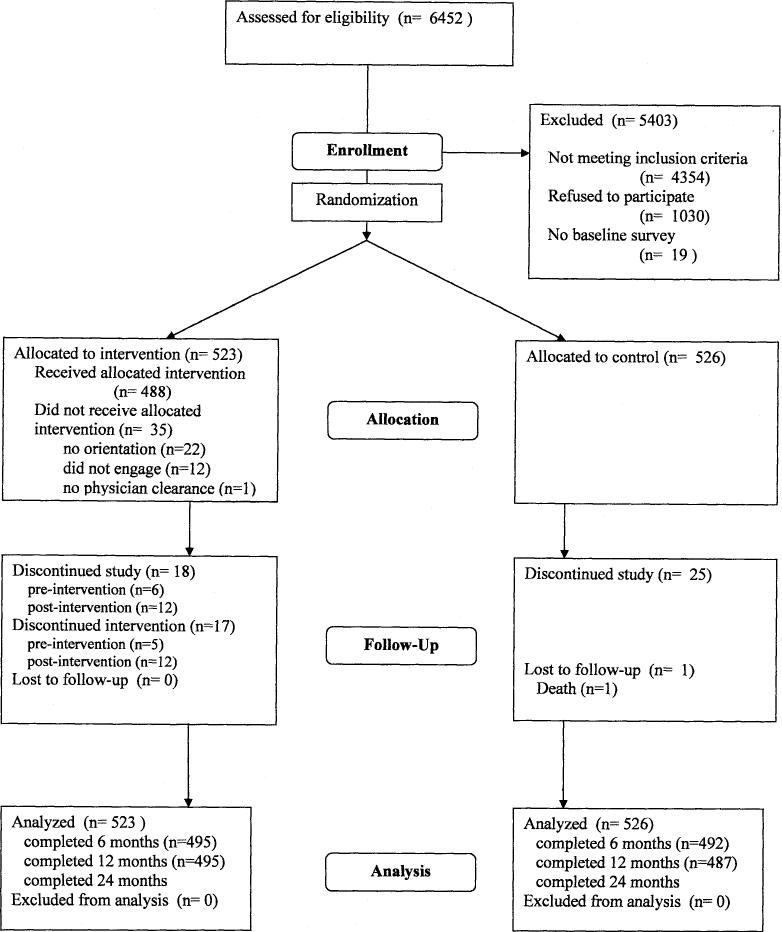
Figure I.
flow of participants through the trial
Acknowledgments
This study was supported by a grant from the National Institute on Aging (R01 AG023410). The project was initiated and analyzed by the study investigators. For her capable project management during the study startup period we thank Kirsten Hase. We would also like to thank Karen Speicher, Jessica Boerboom, Colleen Flattum, and Stephanie Williams for their invaluable contributions as telephone coaches and counselors on the study.
Human Participation Protection This study was reviewed and approved by Regions Hospital Institutional Review Board.
Support: NIH, National Institute on Aging
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Precis: A phone- and mail-based PA maintenance intervention is effective at maintaining PA at 6 months in a sample of N=1,049 adults aged 50−70.
Supplementary Material
References
- ACKERMANN RT, DEYO RA, LOGERFO JP. Prompting primary providers to increase community exercise referrals for older adults: a randomized trial. J Am Geriatr Soc. 2005;53:283–9. doi: 10.1111/j.1532-5415.2005.53115.x. [DOI] [PubMed] [Google Scholar]
- ANDERSON LH, MARTINSON BC, CRAIN AL, PRONK NP, WHITEBIRD RR, FINE L, O'CONNOR PJ. Health Care Charges Associated with Physical Inactivity, Overweight, and Obesity. Prev Chronic Dis [serial online] 2005a:2. [PMC free article] [PubMed] [Google Scholar]
- ANDERSON RT, KING A, STEWART AL, CAMACHO F, REJESKI WJ. Physical activity counseling in primary care and patient well-being: Do patients benefit? Ann Behav Med. 2005b;30:146–54. doi: 10.1207/s15324796abm3002_7. [DOI] [PubMed] [Google Scholar]
- BANDURA A. Social Foundations of Thought and Action: A social cognitive theory; Englewood Cliffs, NJ, Prentice Hall. 1986. [Google Scholar]
- BANDURA A. Health Promotion by Social Cognitive Means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- BLAIR SN, KOHL HW, GORDON NF, PAFFENBARGER RS., JR. How much physical activity is good for health? Annu Rev Public Health. 1992;13:99–126. doi: 10.1146/annurev.pu.13.050192.000531. [DOI] [PubMed] [Google Scholar]
- BOUCHARD C, SHEPHARD R, STEPHENS T. Physical Activity, fitness and health: International proceedings and consensus statement. Human Kinetics Publishers Inc; Champaign, IL: 1994. [Google Scholar]
- BRACH JS, SIMONSICK EM, KRITCHEVSKY S, YAFFE K, NEWMAN AB. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52:502–9. doi: 10.1111/j.1532-5415.2004.52154.x. [DOI] [PubMed] [Google Scholar]
- BULL F, JAMROZIK K, BLANKSBY B. Tailored advice on exercise--Does it make a difference? Am J Prev Med. 1999;16:230–239. doi: 10.1016/s0749-3797(98)00160-3. [DOI] [PubMed] [Google Scholar]
- CASTRO CM, KING AC, BRASSINGTON GS. Telephone versus mail interventions for maintenance of physical activity in older adults. Health Psychol. 2001;20:438–44. [PubMed] [Google Scholar]
- CDC Trends in Leisure-Time Physical Inactivity by Age, Sex, and Race/Ethnicity --- United States, 1994−−2004. MMWR. 2005 Online: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5439a5.htm. [PubMed]
- CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC) Behavioral Risk Factor Surveillance System Survey Data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2005. [Google Scholar]
- CHARLSON M, SZATROWSKI TP, PETERSON J, GOLD J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- COLBERT LH, VISSER M, SIMONSICK EM, TRACY RP, NEWMAN AB, KRITCHEVSKY SB, PAHOR M, TAAFFE DR, BRACH J, RUBIN S, HARRIS TB. Physical activity, exercise, and inflammatory markers in older adults: findings from the health, aging and body composition study. J Am Geriatr Soc. 2004;52:1098–104. doi: 10.1111/j.1532-5415.2004.52307.x. [DOI] [PubMed] [Google Scholar]
- COX KL, BURKE V, MORTON AR, BEILIN LJ, PUDDEY IB. Independent and additive effects of energy restriction and exercise on glucose and insulin concentrations in sedentary overweight men. Am J Clin Nutr. 2004;80:308–316. doi: 10.1093/ajcn/80.2.308. [DOI] [PubMed] [Google Scholar]
- CYARTO EV, MARSHALL AL, DICKINSON RK, BROWN WJ. Measurement properties of the CHAMPS physical activity questionnaire in a sample of older Australians. J Sci Med Sport. 2006;9:319–26. doi: 10.1016/j.jsams.2006.03.001. [DOI] [PubMed] [Google Scholar]
- CYARTO EV, MOORHEAD GE, BROWN WJ. Updating the evidence relating to physical activity intervention studies in older people. J Sci Med Sport. 2004;7:30–8. doi: 10.1016/s1440-2440(04)80275-5. [DOI] [PubMed] [Google Scholar]
- DHHS . Healthy People 2010: Volume II. second edition U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion (ODPHP); Washington, DC: 2000. [Google Scholar]
- DISHMAN R. Motivating older adults to exercise. Southern Medical Journal. 1994;87:S79–S82. [PubMed] [Google Scholar]
- DUNN A, MARCUS B, KAMPERT J, GARCIA M, KOHL H, BLAIR S. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespriatory fitness. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- EAKIN EG, LAWLER SP, VANDELANOTTE C, OWEN N. Telephone Interventions for Physical Activity and Dietary Behavior Change: A Systematic Review. American Journal of Preventive Medicine. 2007;32:419. doi: 10.1016/j.amepre.2007.01.004. [DOI] [PubMed] [Google Scholar]
- EATON CB, MENARD LM. A systematic review of physical activity promotion in primary care office settings. Br J Sports Med. 1998;32:11–6. doi: 10.1136/bjsm.32.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ELAVSKY S, MCAULEY E, MOTL RW, KONOPACK JF, MARQUEZ DX, HU L, JEROME GJ, DIENER E. Physical Activity Enhances Long-Term Quality of Life in Older Adults: Efficacy, Esteem, and Affective Influences. Ann Behav Med. 2005;30:138–145. doi: 10.1207/s15324796abm3002_6. [DOI] [PubMed] [Google Scholar]
- FESKANICH D, WILLETT W, COLDITZ G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. 2002;288:2300–6. doi: 10.1001/jama.288.18.2300. [DOI] [PubMed] [Google Scholar]
- GLASGOW RE, VOGT TM, BOLES SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLDSTEIN M, PINTO B, MARCUS B, LYNN H, JETTE A, RAKOWSKI W, MCDERMOTT S, DEPUE J, MILAN F, DUBE C, TENNSTEDT S. Physician-based physical activity counseling for middle-aged and older adults: A randomized trial. Ann Behav Med. 1999;21:40–47. doi: 10.1007/BF02895032. [DOI] [PubMed] [Google Scholar]
- HANSSON L, ZANCHETTI A, CARRUTHERS SG, DAHLOF B, ELMFELDT D, JULIUS S, MENARD J, RAHN KH, WEDEL H, WESTERLING S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- HARRISON RA, ROBERTS C, ELTON PJ. Does primary care referral to an exercise programme increase physical activity one year later? A randomized controlled trial. J Public Health (Oxf) 2005;27:25–32. doi: 10.1093/pubmed/fdh197. [DOI] [PubMed] [Google Scholar]
- HASKELL W. Dose-response issues from a biological perspective. In: Bouchard, Shephard, Stephens, editors. Physical activity, fitness, and health: International proceedings and consensus statement. Human Kinetics; 1994. pp. 1030–1039. [Google Scholar]
- HELSETH L, SUSSMAN S, CRABTREE B, O'CONNOR P. Primary care physicians' perceptions of diabetes management. A balancing act. J Fam Pract. 1999;48:37–42. [PubMed] [Google Scholar]
- HILLS AP, BYRNE NM. Exercise prescription for weight management. Proc Nutr Soc. 1998;57:93–103. doi: 10.1079/pns19980015. [DOI] [PubMed] [Google Scholar]
- HU F, SIGAL R, RICH-EDWARDS J, COLDITZ G, SOLOMON C, WILLETT W, SPEIZER F, MANSON J. Walking compared with vigorous physical activity and risk of type 2 diabetes in women. JAMA. 1999;282:1433–1439. doi: 10.1001/jama.282.15.1433. [DOI] [PubMed] [Google Scholar]
- HUGHES SL, SEYMOUR RB, CAMPBELL R, POLLAK N, HUBER G, SHARMA L. Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist. 2004;44:217–28. doi: 10.1093/geront/44.2.217. [DOI] [PubMed] [Google Scholar]
- IRWIN M, MAYER-DAVIS E, ADDY C, PATE R, DURSTINE J, STOLARCZYK L, AINSWORTH B. Moderate-intensity physical activity and fasting insulin levels in women: The cross-cultural activity participation study. Diabetes Care. 2000;23:449. doi: 10.2337/diacare.23.4.449. [DOI] [PubMed] [Google Scholar]
- JEFFERY RW, SHERWOOD NE, BRELJE J, PRONK NP, BOYLE RG, BOUCHER JL, HASE K. Mail and Phone Interventions for Weight Loss in a Managed-Care Setting: Weigh-To-Be One-Year Outcomes. Int J Obes Relat Metab Disord. 2003;27:1584–92. doi: 10.1038/sj.ijo.0802473. [DOI] [PubMed] [Google Scholar]
- KERSE N, ELLEY CR, ROBINSON E, ARROLL B. Is physical activity counseling effective for older people? A cluster randomized, controlled trial in primary care. J Am Geriatr Soc. 2005;53:1951–6. doi: 10.1111/j.1532-5415.2005.00466.x. [DOI] [PubMed] [Google Scholar]
- KING AC, PRUITT LA, PHILLIPS W, OKA R, RODENBURG A, HASKELL WL. Comparative effects of two physical activity programs on measured and perceived physical functioning and other health-related quality of life outcomes in older adults. J Gerontol A Biol Sci Med Sci. 2000;55:M74–83. doi: 10.1093/gerona/55.2.m74. [DOI] [PubMed] [Google Scholar]
- KNOWLER WC, BARRETT-CONNOR E, FOWLER SE, HAMMAN RF, LACHIN JM, WALKER EA, NATHAN DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LEVEILLE SG, WAGNER EH, DAVIS C, GROTHAUS L, WALLACE J, LOGERFO J, KENT D. Preventing disability and managing chronic illness in frail older adults: a randomized trial of a community-based partnership with primary care [see comments]. J Am Geriatr Soc. 1998;46:1191–8. doi: 10.1111/j.1532-5415.1998.tb04533.x. [DOI] [PubMed] [Google Scholar]
- LORD S, WARD J, WILLIAMS P, STRUDWICK M. The effects of a 12 month exercise trial on balance, strength and falls in older women: a randomized controlled trial. J Am Geriatr Soc. 1995;43:1198–1206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- MANINI TM, EVERHART JE, PATEL KV, SCHOELLER DA, COLBERT LH, VISSER M, TYLAVSKY F, BAUER DC, GOODPASTER BH, HARRIS TB. Daily Activity Energy Expenditure and Mortality Among Older Adults. JAMA. 2006;296:171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- MARLATT G, GORDON J. Relapse prevention: maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. [Google Scholar]
- MARTINSON BC, CRAIN AL, PRONK NP, O'CONNOR PJ, MACIOSEK MV. Changes in physical activity and short-term changes in health care charges: a prospective cohort study of older adults. Prev Med. 2003;37:319–326. doi: 10.1016/s0091-7435(03)00139-7. [DOI] [PubMed] [Google Scholar]
- MAYER-DAVIS EJ, D'AGOSTINO R,, JR., KARTER AJ, HAFFNER SM, REWERS MJ, SAAD M, BERGMAN RN. Intensity and amount of physical activity in relation to insulin sensitivity: the Insulin Resistance Atherosclerosis Study. JAMA. 1998;279:669–74. doi: 10.1001/jama.279.9.669. [DOI] [PubMed] [Google Scholar]
- MCAULEY E, KONOPACK JF, MOTL RW, MORRIS KS, DOERKSEN SE, ROSENGREN KR. Physical activity and quality of life in older adults: influence of health status and self-efficacy. Ann Behav Med. 2006;31:99–103. doi: 10.1207/s15324796abm3101_14. [DOI] [PubMed] [Google Scholar]
- MCAULEY E, MORRIS KS, MOTL RW, HU L, KONOPACK JF, ELAVSKY S. Long-term follow-up of physical activity behavior in older adults. Health Psychol. 2007;26:375–80. doi: 10.1037/0278-6133.26.3.375. [DOI] [PubMed] [Google Scholar]
- MORGAN O. Approaches to increase physical activity: reviewing the evidence for exercise-referral schemes. Public Health. 2005;119:361–70. doi: 10.1016/j.puhe.2004.06.008. [DOI] [PubMed] [Google Scholar]
- MOTL RW, KONOPACK JF, MCAULEY E, ELAVSKY S, JEROME GJ, MARQUEZ DX. Depressive Symptoms Among Older Adults: Long-Term Reduction After a Physical Activity Intervention. J Behav Med. 2005:1–10. doi: 10.1007/s10865-005-9005-5. [DOI] [PubMed] [Google Scholar]
- O'CONNOR P, PRONK N. Integrating population health concepts, clinical guidelines and ambulatory medical systems to improve diabetes care. J Ambulatory Care Manage. 1998;21:67–73. doi: 10.1097/00004479-199801000-00009. [DOI] [PubMed] [Google Scholar]
- PATE R, PRATT M, BLAIR S, HASKELL W, MACERA C, BOUCHARD C, BUCHNER D, ETTINGER W, HEATH G, KING A, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine [see comments]. JAMA. 1995;273:402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- PESCATELLO LS, FRANKLIN BA, FAGARD R, FARQUHAR WB, KELLEY GA, RAY CA. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36:533–53. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- PINTO BM, FRIERSON GM, RABIN C, TRUNZO JJ, MARCUS BH. Home-based physical activity intervention for breast cancer patients. J Clin Oncol. 2005a;23:3577–87. doi: 10.1200/JCO.2005.03.080. [DOI] [PubMed] [Google Scholar]
- PINTO BM, GOLDSTEIN MG, ASHBA J, SCIAMANNA CN, JETTE A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med. 2005b;29:247–55. doi: 10.1016/j.amepre.2005.06.016. [DOI] [PubMed] [Google Scholar]
- PRONK N, O'CONNOR P. Systems approach to population health improvement. J Ambulatory Care Manage. 1997;20:24–31. doi: 10.1097/00004479-199710000-00005. [DOI] [PubMed] [Google Scholar]
- PRONK NP, BOUCHER JL, GEHLING E, BOYLE RG, JEFFERY RW. A platform for population-based weight management: description of a health plan-based integrated systems approach. Am J Manag Care. 2002a;8:847–57. [PubMed] [Google Scholar]
- PRONK NP, GOODMAN MJ, O'CONNOR PJ, MARTINSON BC. Relationship between modifiable health risks and short-term health care charges. JAMA. 1999;282:2235–9. doi: 10.1001/jama.282.23.2235. [DOI] [PubMed] [Google Scholar]
- PRONK NP, O'CONNOR PJ, MARTINSON BC. Population health and active living: Economic potential of physical activity promotion. American Journal of Medicine & Sports. 2002b;4:51–57. [Google Scholar]
- REJESKI WJ, FIELDING RA, BLAIR SN, GURALNIK JM, GILL TM, HADLEY EC, KING AC, KRITCHEVSKY SB, MILLER ME, NEWMAN AB, PAHOR M. The lifestyle interventions and independence for elders (LIFE) pilot study: Design and methods. Contemp Clin Trials. 2005;26:141–54. doi: 10.1016/j.cct.2004.12.005. [DOI] [PubMed] [Google Scholar]
- RUSH W, O'CONNOR P, GOODMAN M. Validation of a modified Charlson score for using health plan claims data; Minneapolis, Fourth annual Minnesota Health Services Research Conference.2000. [Google Scholar]
- SHERWOOD NE, JEFFERY RW, PRONK NP, BOUCHER JL, HANSON A, BOYLE R, BRELJE K, HASE K, CHEN V. Mail and phone interventions for weight loss in a managed-care setting: weigh-to-be 2-year outcomes. Int J Obes. 2006;30:1565. doi: 10.1038/sj.ijo.0803295. [DOI] [PubMed] [Google Scholar]
- STEWART AL, MILLS KM, KING AC, HASKELL WL, GILLIS D, RITTER PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001a;33:1126–41. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- STEWART AL, MILLS KM, SEPSIS PG, KING AC, MCLELLAN BY, ROITZ K, RITTER PL. Evaluation of CHAMPS, a physical activity promotion program for older adults. Ann Behav Med. 1998;19:353–61. doi: 10.1007/BF02895154. [DOI] [PubMed] [Google Scholar]
- STEWART AL, VERBONCOEUR CJ, MCLELLAN BY, GILLIS DE, RUSH S, MILLS KM, KING AC, RITTER P, BROWN BW, JR., BORTZ WM., 2ND Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. 2001b;56:M465–70. doi: 10.1093/gerona/56.8.m465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STOFAN JR, DIPIETRO L, DAVIS D, KOHL HW, 3RD, BLAIR SN. Physical activity patterns associated with cardiorespiratory fitness and reduced mortality: the Aerobics Center Longitudinal Study. Am J Public Health. 1998;88:1807–13. doi: 10.2105/ajph.88.12.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TUOMILEHTO J, LINDSTROM J, ERIKSSON JG, VALLE TT, HAMALAINEN H, ILANNE-PARIKKA P, KEINANEN-KIUKAANNIEMI S, LAAKSO M, LOUHERANTA A, RASTAS M, SALMINEN V, AUNOLA S, CEPAITIS Z, MOLTCHANOV V, HAKUMAKI M, MANNELIN M, MARTIKKALA V, SUNDVALL J, UUSITUPA M, THE FINNISH DIABETES PREVENTION STUDY GROUP Prevention of Type 2 Diabetes Mellitus by Changes in Lifestyle among Subjects with Impaired Glucose Tolerance. N Engl J Med. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- UNGER JB, JOHNSON CA, MARKS G. Functional decline in the elderly: evidence for direct and stress- buffering protective effects of social interactions and physical activity. Ann Behav Med. 1997;19:152–60. doi: 10.1007/BF02883332. [DOI] [PubMed] [Google Scholar]
- VAN DER BIJ AK, LAURANT MGH, WENSING M. Effectiveness of physical activity interventions for older adults: A review. Am J Prev Med. 2002;22:120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- VAN SLUIJS EMF, VAN POPPEL MNM, TWISK JWR, CHIN A PAW MJ, CALFAS KJ, VAN MECHELEN W. Effect of a Tailored Physical Activity Intervention Delivered in General Practice Settings: Results of a Randomized Controlled Trial. Am J Public Health. 2005;95:1825–1831. doi: 10.2105/AJPH.2004.044537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WALSH J, SWANGARD D, DAVIS T, MCPHEE S. Exercise counseling by primary care physicians in the era of managed care. Am J Prev Med. 1999;16:307–313. doi: 10.1016/s0749-3797(99)00021-5. [DOI] [PubMed] [Google Scholar]
- WEUVE J, KANG JH, MANSON JE, BRETELER MMB, WARE JH, GRODSTEIN F. Physical Activity, Including Walking, and Cognitive Function in Older Women. JAMA. 2004;292:1454–1461. doi: 10.1001/jama.292.12.1454. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.