Abstract
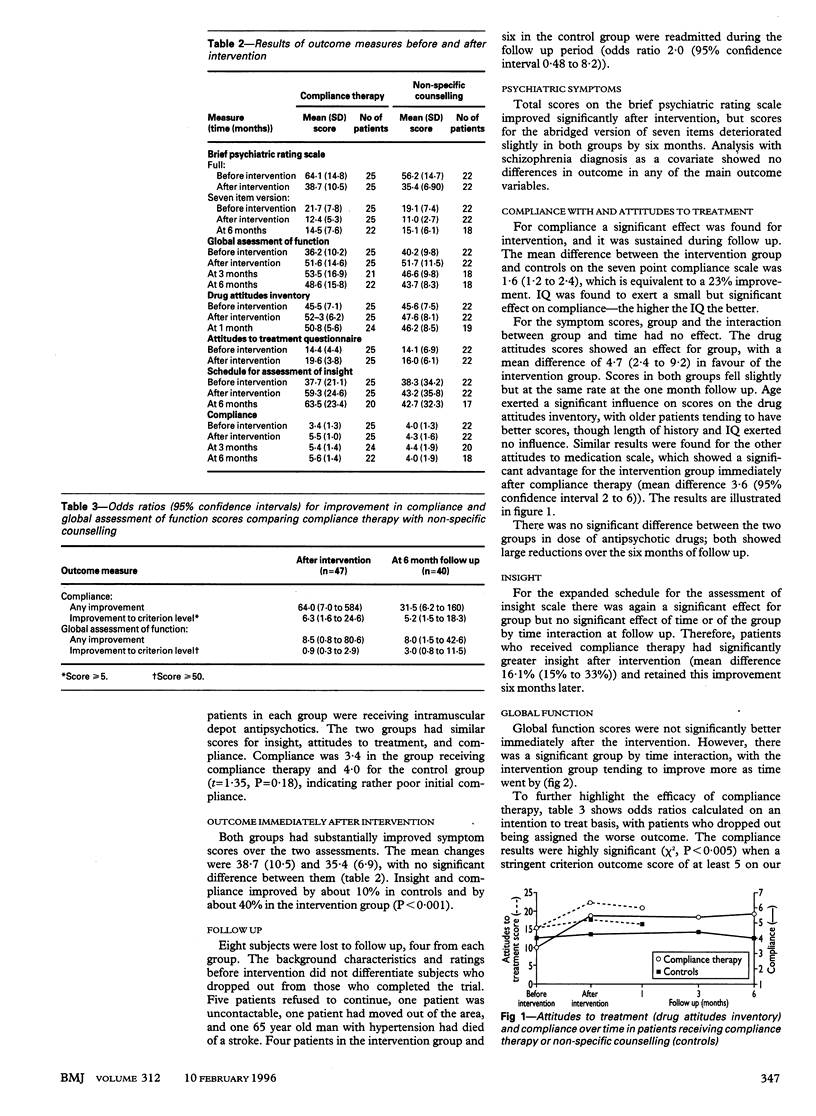
OBJECTIVE--To determine whether compliance therapy, a cognitive-behavioural intervention, could improve compliance with treatment and hence social adjustment in acutely psychotic inpatients, and if so, whether the effect persisted six months later. DESIGN--Randomised controlled trial of compliance therapy and non-specific counselling, each comprising 4-6 sessions lasting 10-60 minutes. SETTING--Acute psychiatric admissions ward serving an inner London catchment area. SUBJECTS--47 patients with psychosis. MAIN OUTCOME MEASURES--Informant and observer reported measure of compliance; observer assessed global functioning after intervention and three and six months later; self-rated attitudes to drug treatment after the intervention and one month later; symptom scores after intervention and six months later. RESULTS--25 patients received compliance therapy and showed significantly greater improvements in their attitudes to drug treatment and in their insight into illness and compliance with treatment compared with the control group. These gains persisted for six months. The intervention group was 5.2 times more likely than the control group to reach a criterion level of compliance (95% confidence interval 1.5 to 18.3). Global functioning showed a tendency to improve more in the intervention group after a delay (odds ratio 3.0 (0.8 to 11.5) to reach the criterion level at six months). Four subjects given compliance therapy and six in the control group were readmitted during follow up (odds ratio 2.0 (0.48 to 8.2)). CONCLUSIONS--Compliance therapy is a pragmatic method for improving compliance with drug treatment in psychotic inpatients and its gains persist for at least six months. Overall functioning may also be enhanced.
Full text
PDF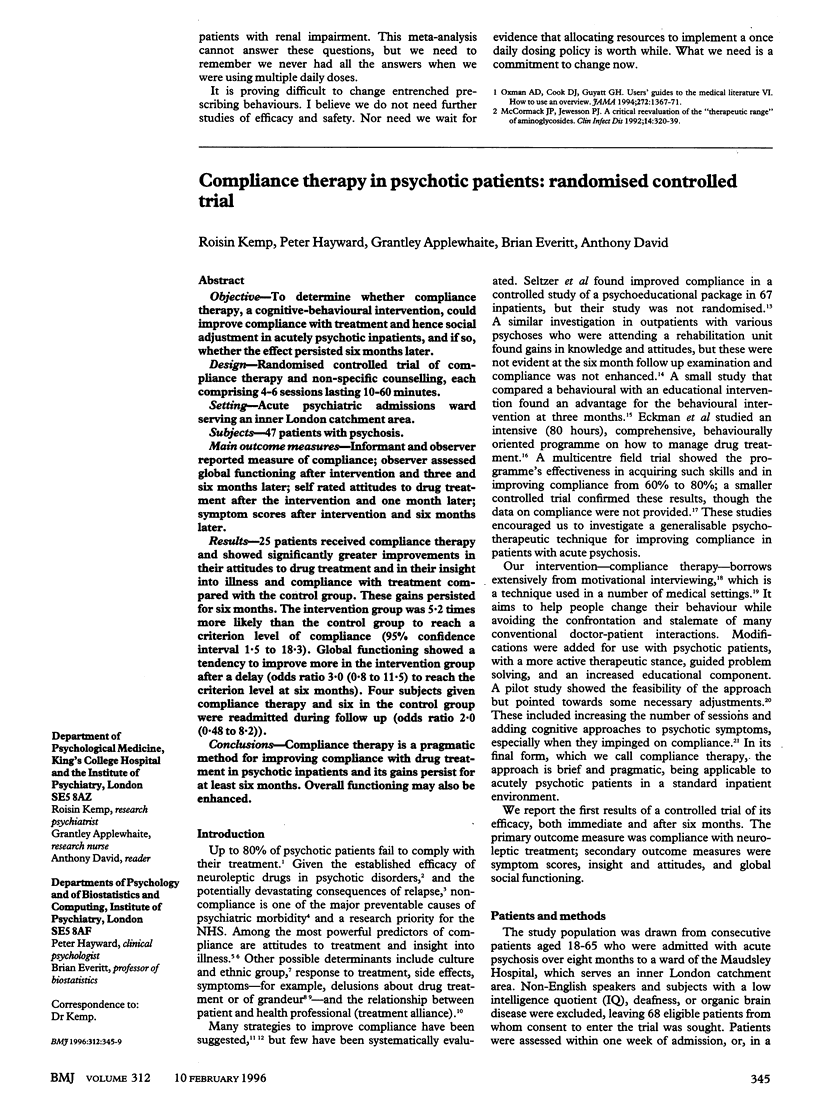



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Babiker I. E. Noncompliance in schizophrenia. Psychiatr Dev. 1986 Winter;4(4):329–337. [PubMed] [Google Scholar]
- Barnes T. R. A rating scale for drug-induced akathisia. Br J Psychiatry. 1989 May;154:672–676. doi: 10.1192/bjp.154.5.672. [DOI] [PubMed] [Google Scholar]
- Boczkowski J. A., Zeichner A., DeSanto N. Neuroleptic compliance among chronic schizophrenic outpatients: an intervention outcome report. J Consult Clin Psychol. 1985 Oct;53(5):666–671. doi: 10.1037//0022-006x.53.5.666. [DOI] [PubMed] [Google Scholar]
- Corrigan P. W., Liberman R. P., Engel J. D. From noncompliance to collaboration in the treatment of schizophrenia. Hosp Community Psychiatry. 1990 Nov;41(11):1203–1211. doi: 10.1176/ps.41.11.1203. [DOI] [PubMed] [Google Scholar]
- David A. S. Insight and psychosis. Br J Psychiatry. 1990 Jun;156:798–808. doi: 10.1192/bjp.156.6.798. [DOI] [PubMed] [Google Scholar]
- David A., Buchanan A., Reed A., Almeida O. The assessment of insight in psychosis. Br J Psychiatry. 1992 Nov;161:599–602. doi: 10.1192/bjp.161.5.599. [DOI] [PubMed] [Google Scholar]
- Eckman T. A., Liberman R. P., Phipps C. C., Blair K. E. Teaching medication management skills to schizophrenic patients. J Clin Psychopharmacol. 1990 Feb;10(1):33–38. doi: 10.1097/00004714-199002000-00006. [DOI] [PubMed] [Google Scholar]
- Eckman T. A., Wirshing W. C., Marder S. R., Liberman R. P., Johnston-Cronk K., Zimmermann K., Mintz J. Technique for training schizophrenic patients in illness self-management: a controlled trial. Am J Psychiatry. 1992 Nov;149(11):1549–1555. doi: 10.1176/ajp.149.11.1549. [DOI] [PubMed] [Google Scholar]
- Endicott J., Spitzer R. L., Fleiss J. L., Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976 Jun;33(6):766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Frison L., Pocock S. J. Repeated measures in clinical trials: analysis using mean summary statistics and its implications for design. Stat Med. 1992 Sep 30;11(13):1685–1704. doi: 10.1002/sim.4780111304. [DOI] [PubMed] [Google Scholar]
- Garety P. A., Kuipers L., Fowler D., Chamberlain F., Dunn G. Cognitive behavioural therapy for drug-resistant psychosis. Br J Med Psychol. 1994 Sep;67(Pt 3):259–271. doi: 10.1111/j.2044-8341.1994.tb01795.x. [DOI] [PubMed] [Google Scholar]
- Goldstein M. J. Psychosocial strategies for maximizing the effects of psychotropic medications for schizophrenia and mood disorder. Psychopharmacol Bull. 1992;28(3):237–240. [PubMed] [Google Scholar]
- Hogan T. P., Awad A. G., Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983 Feb;13(1):177–183. doi: 10.1017/s0033291700050182. [DOI] [PubMed] [Google Scholar]
- Hoge S. K., Appelbaum P. S., Lawlor T., Beck J. C., Litman R., Greer A., Gutheil T. G., Kaplan E. A prospective, multicenter study of patients' refusal of antipsychotic medication. Arch Gen Psychiatry. 1990 Oct;47(10):949–956. doi: 10.1001/archpsyc.1990.01810220065008. [DOI] [PubMed] [Google Scholar]
- Kane J. M. Problems of compliance in the outpatient treatment of schizophrenia. J Clin Psychiatry. 1983 Jun;44(6 Pt 2):3–6. [PubMed] [Google Scholar]
- Kelly G. R., Mamon J. A., Scott J. E. Utility of the health belief model in examining medication compliance among psychiatric outpatients. Soc Sci Med. 1987;25(11):1205–1211. doi: 10.1016/0277-9536(87)90367-4. [DOI] [PubMed] [Google Scholar]
- Lukoff D., Liberman R. P., Nuechterlein K. H. Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophr Bull. 1986;12(4):578–602. doi: 10.1093/schbul/12.4.578. [DOI] [PubMed] [Google Scholar]
- Marder S. R., Mebane A., Chien C. P., Winslade W. J., Swann E., Van Putten T. A comparison of patients who refuse and consent to neuroleptic treatment. Am J Psychiatry. 1983 Apr;140(4):470–472. doi: 10.1176/ajp.140.4.470. [DOI] [PubMed] [Google Scholar]
- McEvoy J. P., Applebaum P. S., Apperson L. J., Geller J. L., Freter S. Why must some schizophrenic patients be involuntarily committed? The role of insight. Compr Psychiatry. 1989 Jan-Feb;30(1):13–17. doi: 10.1016/0010-440x(89)90113-2. [DOI] [PubMed] [Google Scholar]
- Sellwood W., Tarrier N. Demographic factors associated with extreme non-compliance in schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 1994 Jul;29(4):172–177. doi: 10.1007/BF00802014. [DOI] [PubMed] [Google Scholar]
- Seltzer A., Roncari I., Garfinkel P. Effect of patient education on medication compliance. Can J Psychiatry. 1980 Dec;25(8):638–645. doi: 10.1177/070674378002500807. [DOI] [PubMed] [Google Scholar]
- Simpson G. M., Angus J. W. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]
- Van Putten T., Crumpton E., Yale C. Drug refusal in schizophrenia and the wish to be crazy. Arch Gen Psychiatry. 1976 Dec;33(12):1443–1446. doi: 10.1001/archpsyc.1976.01770120047004. [DOI] [PubMed] [Google Scholar]
- Van Putten T. Why do schizophrenic patients refuse to take their drugs? Arch Gen Psychiatry. 1974 Jul;31(1):67–72. doi: 10.1001/archpsyc.1974.01760130049008. [DOI] [PubMed] [Google Scholar]


