Abstract
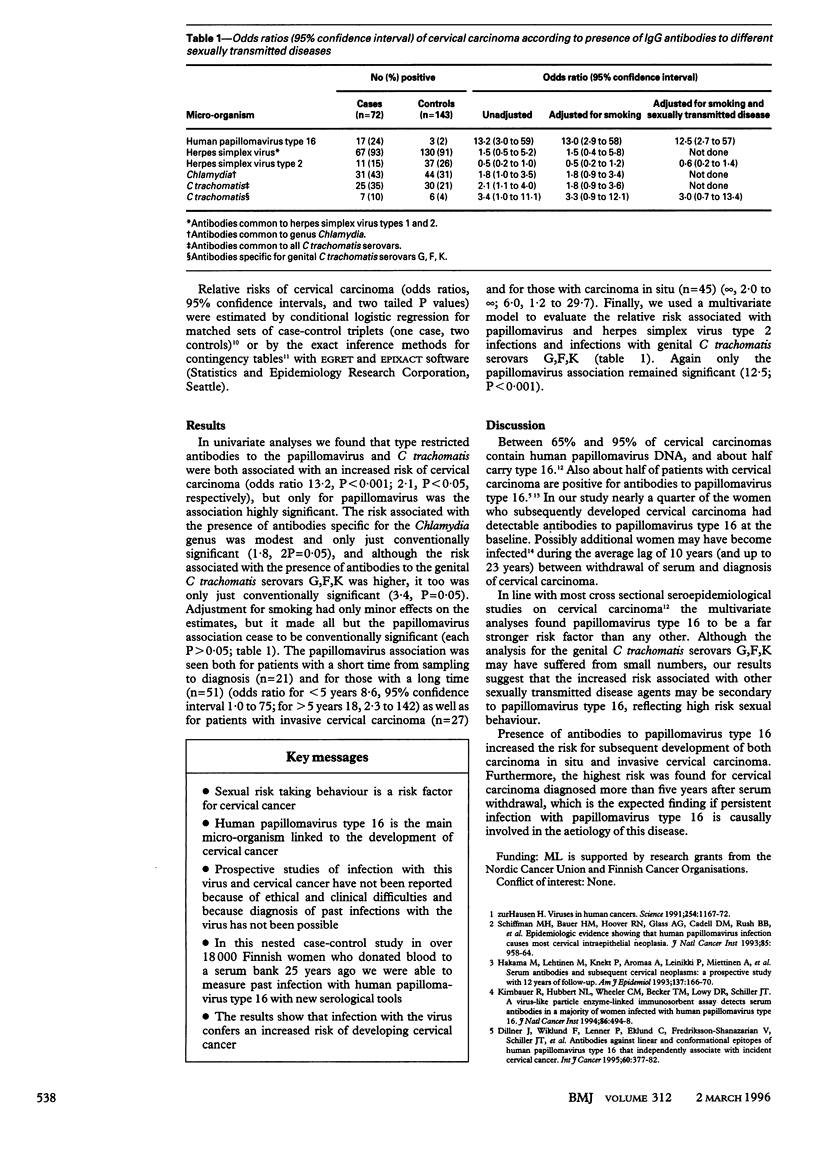
OBJECTIVE--To study human papillomavirus type 16 in the aetiology of cervical carcinoma. DESIGN--Within a cohort of 18814 Finnish women followed up to 23 years a nested case-control study was conducted based on serological diagnosis of past infection with human papillomavirus type 16. SUBJECTS--72 women (27 with invasive carcinoma and 45 with in situ carcinoma) and 143 matched controls were identified during the follow up. MAIN OUTCOME MEASURE--Relative risk of cervical carcinoma in presence of IgG antibodies to human papillomavirus type 16. RESULTS--After adjustment for smoking and for antibodies to various other agents of sexually transmitted disease, such as herpes simplex virus type 2 and Chlamydia trachomatis, the only significant association was with infection with human papillomavirus type 16 (odds ratio 12.5; 95% confidence interval 2.7 to 57, 2P<0.001). CONCLUSION--This prospective study provides epidemiological evidence that infection with human papillomavirus type 16 confers an excess risk for subsequent development of cervical carcinoma.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dillner J., Lenner P., Lehtinen M., Eklund C., Heino P., Wiklund F., Hallmans G., Stendahl U. A population-based seroepidemiological study of cervical cancer. Cancer Res. 1994 Jan 1;54(1):134–141. [PubMed] [Google Scholar]
- Dillner J., Wiklund F., Lenner P., Eklund C., Frederiksson-Shanazarian V., Schiller J. T., Hibma M., Hallmans G., Stendahl U. Antibodies against linear and conformational epitopes of human papillomavirus type 16 that independently associate with incident cervical cancer. Int J Cancer. 1995 Jan 27;60(3):377–382. doi: 10.1002/ijc.2910600318. [DOI] [PubMed] [Google Scholar]
- Hakama M., Lehtinen M., Knekt P., Aromaa A., Leinikki P., Miettinen A., Paavonen J., Peto R., Teppo L. Serum antibodies and subsequent cervical neoplasms: a prospective study with 12 years of follow-up. Am J Epidemiol. 1993 Jan 15;137(2):166–170. doi: 10.1093/oxfordjournals.aje.a116656. [DOI] [PubMed] [Google Scholar]
- Hanna L., Keshishyan H. Chlamydial antigens stabilized with formalin for use in the micro-immunofluorescence test. J Clin Microbiol. 1980 Sep;12(3):409–412. doi: 10.1128/jcm.12.3.409-412.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirnbauer R., Hubbert N. L., Wheeler C. M., Becker T. M., Lowy D. R., Schiller J. T. A virus-like particle enzyme-linked immunosorbent assay detects serum antibodies in a majority of women infected with human papillomavirus type 16. J Natl Cancer Inst. 1994 Apr 6;86(7):494–499. doi: 10.1093/jnci/86.7.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehtinen M., Rantala I., Aine R., Miettinen A., Laine S., Heinonen P., Teisala K., Punnonen R., Paavonen J. B cell response in Chlamydia trachomatis endometritis. Eur J Clin Microbiol. 1986 Oct;5(5):596–598. doi: 10.1007/BF02017713. [DOI] [PubMed] [Google Scholar]
- Nonnenmacher B., Hubbert N. L., Kirnbauer R., Shah K. V., Muñoz N., Bosch F. X., de Sanjosé S., Viscidi R., Lowy D. R., Schiller J. T. Serologic response to human papillomavirus type 16 (HPV-16) virus-like particles in HPV-16 DNA-positive invasive cervical cancer and cervical intraepithelial neoplasia grade III patients and controls from Colombia and Spain. J Infect Dis. 1995 Jul;172(1):19–24. doi: 10.1093/infdis/172.1.19. [DOI] [PubMed] [Google Scholar]
- Schiffman M. H., Bauer H. M., Hoover R. N., Glass A. G., Cadell D. M., Rush B. B., Scott D. R., Sherman M. E., Kurman R. J., Wacholder S. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst. 1993 Jun 16;85(12):958–964. doi: 10.1093/jnci/85.12.958. [DOI] [PubMed] [Google Scholar]
- zur Hausen H. Viruses in human cancers. Science. 1991 Nov 22;254(5035):1167–1173. doi: 10.1126/science.1659743. [DOI] [PubMed] [Google Scholar]



