Abstract
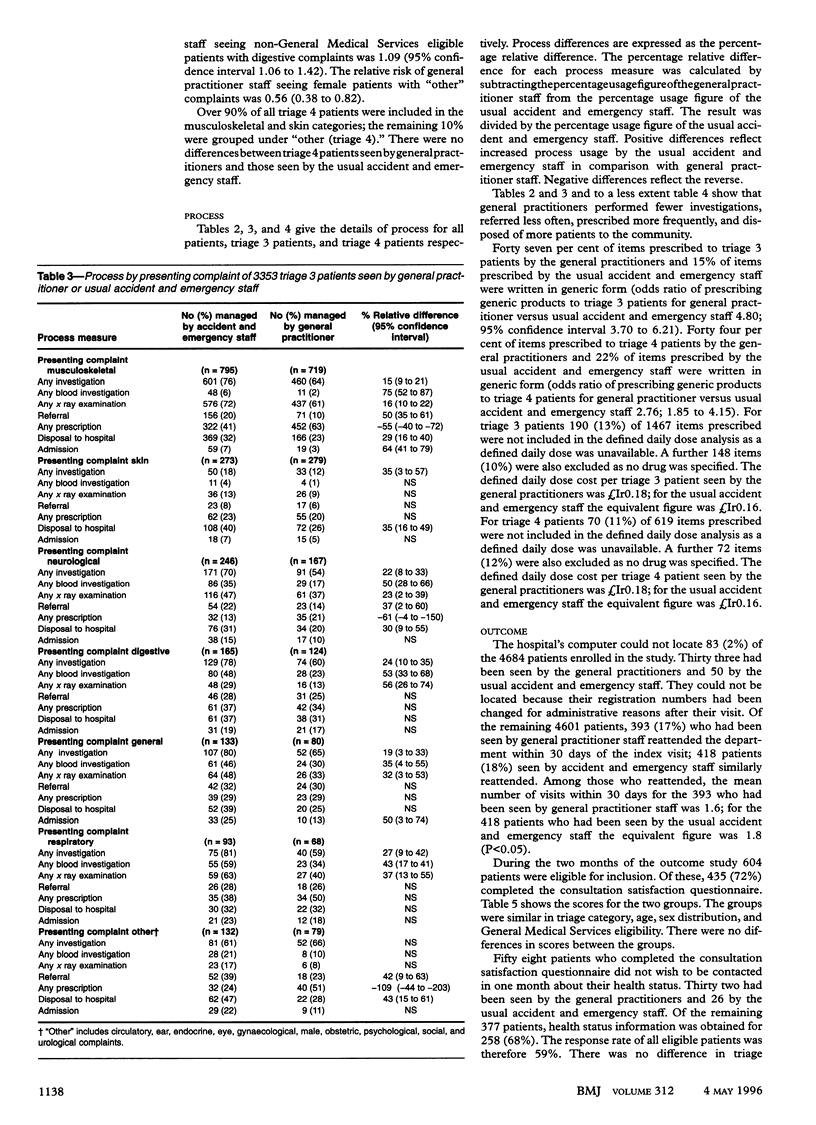
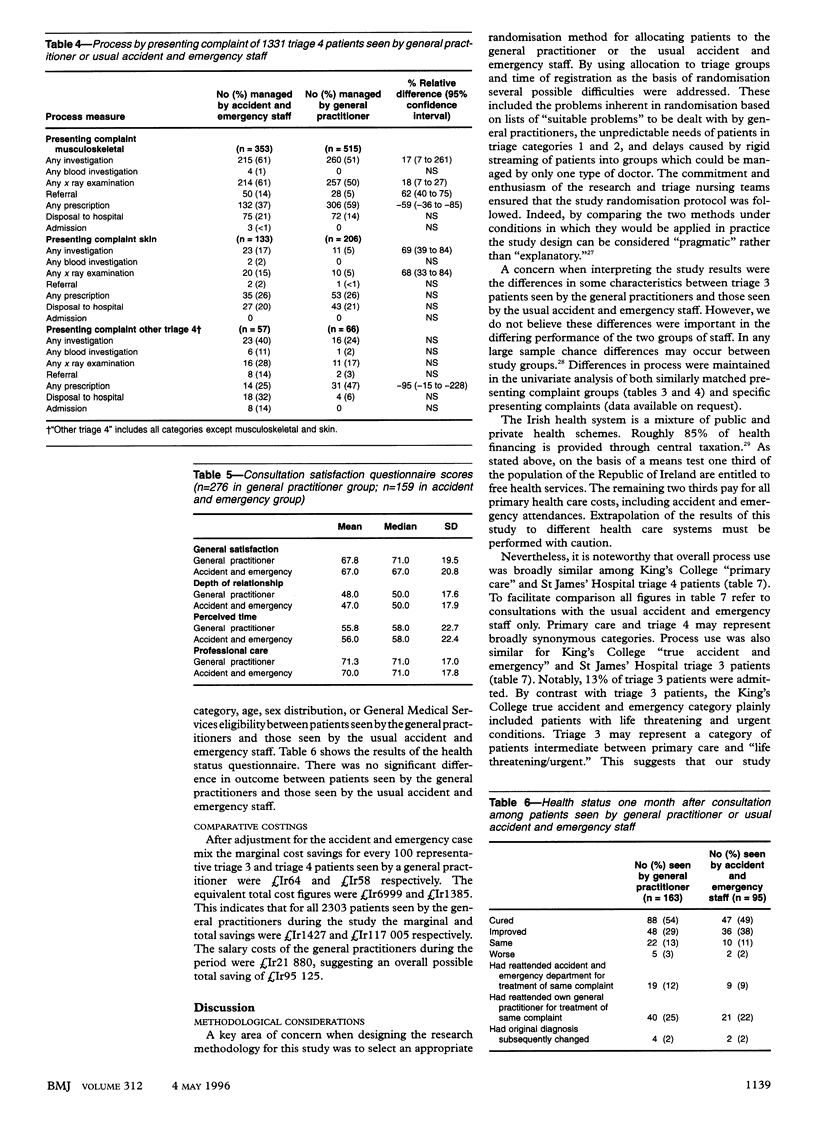
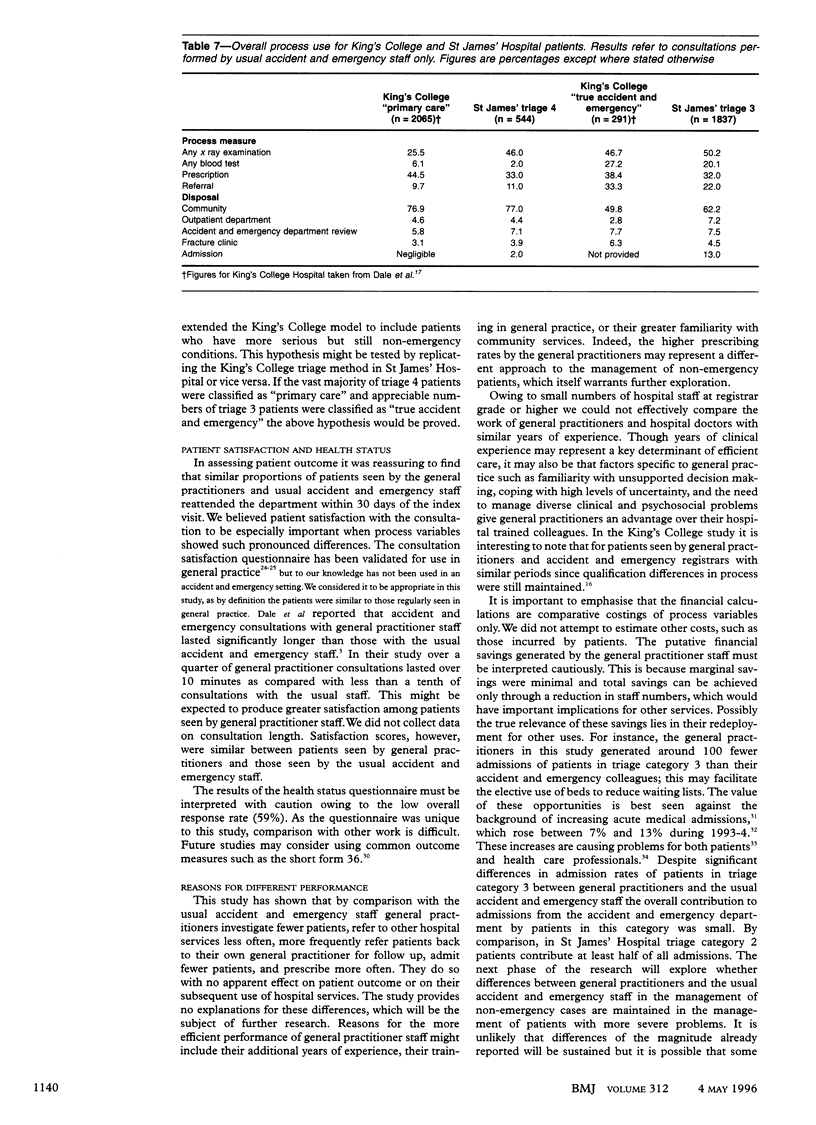
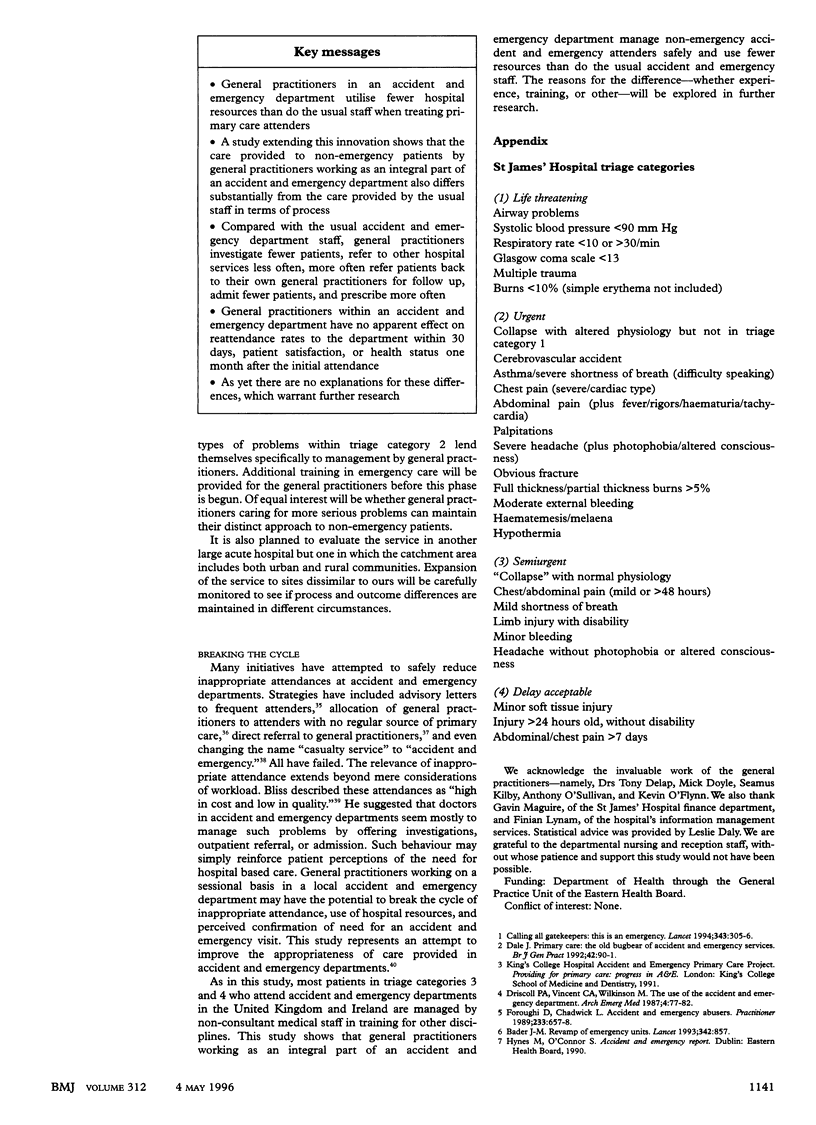
OBJECTIVE--To see whether care provided by general practitioners to non-emergency patients in an accident and emergency department differs significantly from care by usual accident and emergency staff in terms of process, outcome, and comparative cost. DESIGN--A randomised controlled trial. SETTING--A busy inner city hospital's accident and emergency department which employed three local general practitioners on a sessional basis. PATIENTS--All new attenders categorised by the triage system as "semiurgent" or "delay acceptable." 66% of all attenders were eligible for inclusion. MAIN OUTCOME MEASURES--Numbers of patients undergoing investigation, referral, or prescription; types of disposal; consultation satisfaction scores; reattendance to accident and emergency department within 30 days of index visit; health status at one month; comparative cost differences. RESULTS--4684 patients participated. For semiurgent patients, by comparison with usual accident and emergency staff, general practitioners investigated fewer patients (relative difference 20%; 95% confidence interval 16% to 25%), referred to other hospital services less often (39%; 28% to 47%), admitted fewer patients (45%; 32% to 56%), and prescribed more often (41%; 30% to 54%). A similar trend was found for patients categorised as delay acceptable and (in a separate analysis) by presenting complaint category. 393 (17%) patients who had been seen by general practitioner staff reattended the department within 30 days of the index visit; 418 patients (18%) seen by accident and emergency staff similarly reattended, 435 patients (72% of those eligible) completed the consultation satisfaction questionnaire and 258 (59% of those eligible) provided health status information one month after consultation. There were no differences between patients managed by general practitioners and those managed by usual staff regarding consultation satisfaction questionnaire scores or health status. For all patients seen by general practitioners during the study, estimated marginal and total savings were Ir1427 pounds and Ir117,005 pounds respectively. CONCLUSION--General practitioners working as an integral part of an accident and emergency department manage non-emergency accident and emergency attenders safely and use fewer resources than do usual accident and emergency staff.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armstrong A. M., Pennycook A. G., Swann I. J. Unplanned re-attendance in the accident and emergency department. Scott Med J. 1991 Aug;36(4):111–114. doi: 10.1177/003693309103600405. [DOI] [PubMed] [Google Scholar]
- Baker R. Development of a questionnaire to assess patients' satisfaction with consultations in general practice. Br J Gen Pract. 1990 Dec;40(341):487–490. [PMC free article] [PubMed] [Google Scholar]
- Baker R. The reliability and criterion validity of a measure of patients' satisfaction with their general practice. Fam Pract. 1991 Jun;8(2):171–177. doi: 10.1093/fampra/8.2.171. [DOI] [PubMed] [Google Scholar]
- Baker R., Whitfield M. Measuring patient satisfaction: a test of construct validity. Qual Health Care. 1992 Jun;1(2):104–109. doi: 10.1136/qshc.1.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bindman A. B. Triage in accident and emergency departments. BMJ. 1995 Aug 12;311(7002):404–404. doi: 10.1136/bmj.311.7002.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliss H. A. Primary care in the emergency room: high in cost and low in quality. N Engl J Med. 1982 Apr 22;306(16):998–998. doi: 10.1056/nejm198204223061626. [DOI] [PubMed] [Google Scholar]
- Brook R. H. Appropriateness: the next frontier. BMJ. 1994 Jan 22;308(6923):218–219. doi: 10.1136/bmj.308.6923.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale J., Green J., Reid F., Glucksman E., Higgs R. Primary care in the accident and emergency department: II. Comparison of general practitioners and hospital doctors. BMJ. 1995 Aug 12;311(7002):427–430. doi: 10.1136/bmj.311.7002.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale J., Green J., Reid F., Glucksman E. Primary care in the accident and emergency department: I. Prospective identification of patients. BMJ. 1995 Aug 12;311(7002):423–426. doi: 10.1136/bmj.311.7002.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale J. Primary care: the old bugbear of accident and emergency services. Br J Gen Pract. 1992 Mar;42(356):90–91. [PMC free article] [PubMed] [Google Scholar]
- Dillner L. Emergency delays need urgent attention. BMJ. 1995 Feb 4;310(6975):283–283. doi: 10.1136/bmj.310.6975.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driscoll P. A., Vincent C. A., Wilkinson M. The use of the accident and emergency department. Arch Emerg Med. 1987 Jun;4(2):77–82. doi: 10.1136/emj.4.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foldes S. S., Fischer L. R., Kaminsky K. What is an emergency? The judgments of two physicians. Ann Emerg Med. 1994 Apr;23(4):833–840. doi: 10.1016/s0196-0644(94)70322-1. [DOI] [PubMed] [Google Scholar]
- George S., Read S., Westlake L., Fraser-Moodie A., Pritty P., Williams B. Differences in priorities assigned to patients by triage nurses and by consultant physicians in accident and emergency departments. J Epidemiol Community Health. 1993 Aug;47(4):312–315. doi: 10.1136/jech.47.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansagi H., Carlsson B., Olsson M., Edhag O. Trial of a method of reducing inappropriate demands on a hospital emergency department. Public Health. 1987 Mar;101(2):99–105. doi: 10.1016/s0033-3506(87)80046-x. [DOI] [PubMed] [Google Scholar]
- Hobbs R. Rising emergency admissions. BMJ. 1995 Jan 28;310(6974):207–208. doi: 10.1136/bmj.310.6974.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins C., Bartholomew J., Gelder F., Morrell D. Arranging hospital admission for acutely ill patients: problems encountered by general practitioners. Br J Gen Pract. 1994 Jun;44(383):251–254. [PMC free article] [PubMed] [Google Scholar]
- Kaliszer M., McCormick J. New casualty attenders at a Dublin hospital. Ir Med J. 1975 Apr 12;68(7):159–164. [PubMed] [Google Scholar]
- Lerman B., Kobernick M. S. Return visits to the emergency department. J Emerg Med. 1987 Sep-Oct;5(5):359–362. doi: 10.1016/0736-4679(87)90138-7. [DOI] [PubMed] [Google Scholar]
- McCabe J. B. What is an emergency, and who wants to know? Ann Emerg Med. 1994 Apr;23(4):872–873. doi: 10.1016/s0196-0644(94)90004-3. [DOI] [PubMed] [Google Scholar]
- Mosley M. Ulcer wars. BMJ. 1994 Jul 9;309(6947):132–132. doi: 10.1136/bmj.309.6947.132b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz D., Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. J Chronic Dis. 1967 Aug;20(8):637–648. doi: 10.1016/0021-9681(67)90041-0. [DOI] [PubMed] [Google Scholar]
- Straus J. H., Orr S. T., Charney E. Referrals from an emergency room to primary care practices at an urban hospital. Am J Public Health. 1983 Jan;73(1):57–61. doi: 10.2105/ajph.73.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J. E. Measuring patients' views: the optimum outcome measure. BMJ. 1993 May 29;306(6890):1429–1430. doi: 10.1136/bmj.306.6890.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson A., Kazantzis G., Williams D. J., Dewar R. A., Bristow K. M., Miller D. L. Attendance at a London casualty department. J R Coll Gen Pract. 1977 Dec;27(185):727–733. [PMC free article] [PubMed] [Google Scholar]



