Abstract
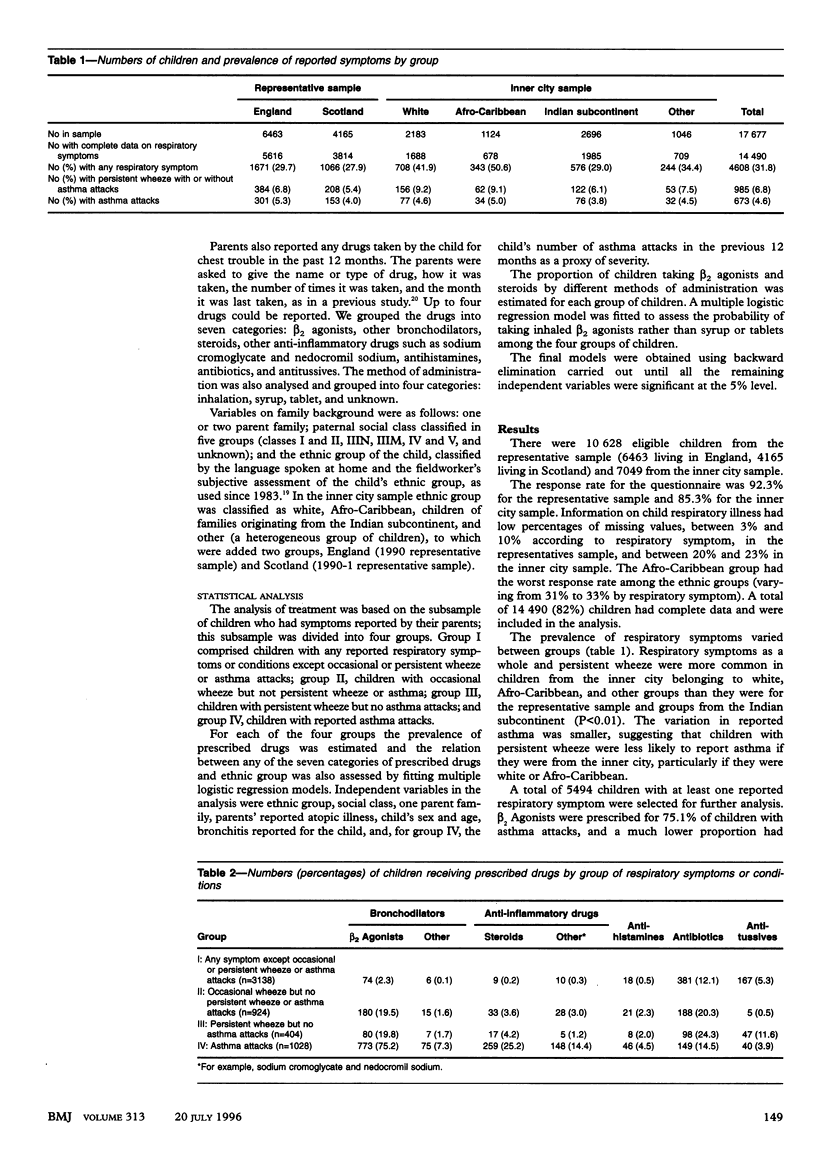
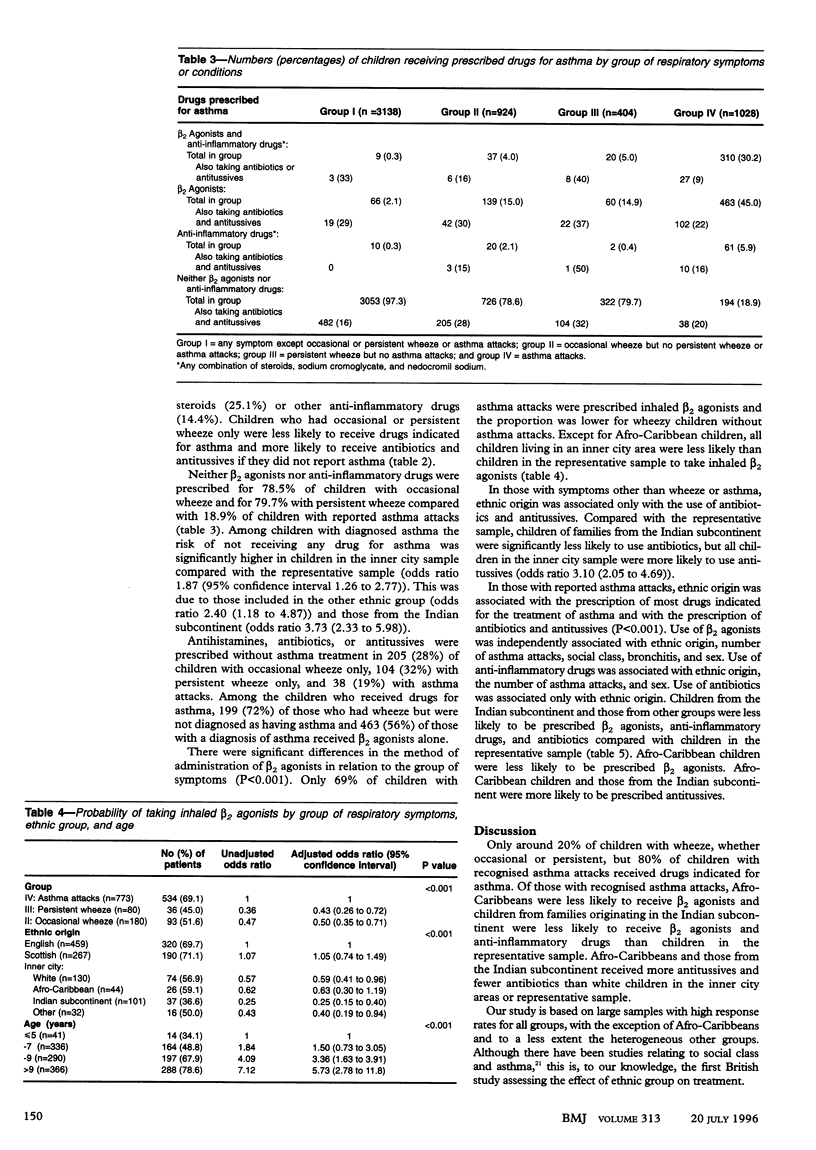
OBJECTIVE--To examine the extent to which the prescription of drugs for asthma adhered to recommended guidelines in 1990-1 and to assess the influence of ethnic group on prescription. DESIGN--Cross sectional. SETTING--Primary schools in England and Scotland in 1990-1. SUBJECTS--Children aged mainly 5-11 years. The representative samples included 10628 children. The inner city sample included 7049 children, 4866 (69%) from ethnic minority groups. For the prevalence estimation 14490 children were included in the analysis (82% of the eligible children). For the treatment analysis a subgroup of 5494 children with respiratory symptoms was selected. MAIN OUTCOME MEASURES--Prevalence of respiratory symptoms and drugs commonly prescribed for asthma, method of administration, inappropriate treatment, and odds ratios to assess the effect of ethnic group on rate of prescription and method of administration. RESULTS--Children with respiratory symptoms in the inner city sample were less likely to be diagnosed as having asthma. Of children with reported asthma attacks, those in inner city areas had a higher risk of not having been prescribed any drug for asthma (odds ratio 1.87 (95% confidence interval 1.26 to 2.77). Overall, 773 (75%) of these children had received a beta 2 agonist, 259 (25%) had received steroids, 148 (14%) had received sodium cromoglycate, and 194 (19%) had received no drug treatment in the previous year. When prescribed, beta 2 agonists were inhaled in 534 (69%) of cases, and this percentage was even lower in ethnic minority groups. Children of Afro-Caribbean and Indian subcontinent origin who had asthma were less likely to receive beta 2 agonists, and those from the Indian subcontinent were less likely to receive anti-inflammatory drugs. Antibiotics were less prescribed and antitussives more prescribed in children from ethnic minority groups than in white children. CONCLUSION--In 1990-1 the risk of underdiagnosis and undertreatment of asthma was higher in children from ethnic minority groups. The implementation of indicators and targets to monitor inequalities in the treatment of asthma in ethnic groups could improve equity and effectiveness in the NHS.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson H. R. Increase in hospital admissions for childhood asthma: trends in referral, severity, and readmissions from 1970 to 1985 in a health region of the United Kingdom. Thorax. 1989 Aug;44(8):614–619. doi: 10.1136/thx.44.8.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balarajan R., Yuen P., Soni Raleigh V. Ethnic differences in general practitioner consultations. BMJ. 1989 Oct 14;299(6705):958–960. doi: 10.1136/bmj.299.6705.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman A., Young L., Peat J. K., Hunt J., Larkin P. Asthma under-recognition and under-treatment in an Australian community. Aust N Z J Med. 1992 Feb;22(1):36–40. doi: 10.1111/j.1445-5994.1992.tb01706.x. [DOI] [PubMed] [Google Scholar]
- Bosco L. A., Gerstman B. B., Tomita D. K. Variations in the use of medication for the treatment of childhood asthma in the Michigan Medicaid population, 1980 to 1986. Chest. 1993 Dec;104(6):1727–1732. doi: 10.1378/chest.104.6.1727. [DOI] [PubMed] [Google Scholar]
- Burney P. G. Strategy for asthma. BMJ. 1991 Sep 7;303(6802):571–573. doi: 10.1136/bmj.303.6802.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr W., Zeitel L., Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am J Public Health. 1992 Jan;82(1):59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett J. E., Mulder J., Wong-Toi H. Reasons for racial differences in A & E attendance rates for asthma. N Z Med J. 1989 Mar 22;102(864):121–124. [PubMed] [Google Scholar]
- Gergen P. J., Weiss K. B. Changing patterns of asthma hospitalization among children: 1979 to 1987. JAMA. 1990 Oct 3;264(13):1688–1692. [PubMed] [Google Scholar]
- Gill P. S., Johnson M. Ethnic monitoring and equity. BMJ. 1995 Apr 8;310(6984):890–890. doi: 10.1136/bmj.310.6984.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill R. A., Standen P. J., Tattersfield A. E. Asthma, wheezing, and school absence in primary schools. Arch Dis Child. 1989 Feb;64(2):246–251. doi: 10.1136/adc.64.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill R. A., Standen P. J., Tattersfield A. E. Asthma, wheezing, and school absence in primary schools. Arch Dis Child. 1989 Feb;64(2):246–251. doi: 10.1136/adc.64.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kun H. Y., Oates R. K., Mellis C. M. Hospital admissions and attendances for asthma--a true increase? Med J Aust. 1993 Sep 6;159(5):312–313. doi: 10.5694/j.1326-5377.1993.tb137867.x. [DOI] [PubMed] [Google Scholar]
- Mitchell E. A. International trends in hospital admission rates for asthma. Arch Dis Child. 1985 Apr;60(4):376–378. doi: 10.1136/adc.60.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell E. A. Racial inequalities in childhood asthma. Soc Sci Med. 1991;32(7):831–836. doi: 10.1016/0277-9536(91)90309-z. [DOI] [PubMed] [Google Scholar]
- Peat J. K., Salome C. M., Sedgwick C. S., Kerrebijn J., Woolcock A. J. A prospective study of bronchial hyperresponsiveness and respiratory symptoms in a population of Australian schoolchildren. Clin Exp Allergy. 1989 May;19(3):299–306. doi: 10.1111/j.1365-2222.1989.tb02387.x. [DOI] [PubMed] [Google Scholar]
- Phin S., Oates R. K. Variations in the treatment of childhood asthma. Med J Aust. 1993 Nov 15;159(10):662–666. doi: 10.5694/j.1326-5377.1993.tb138080.x. [DOI] [PubMed] [Google Scholar]
- Rona R. J., Altman D. G. National study of health and growth: standards of attained height, weight and triceps skinfold in English children 5 to 11 years old. Ann Hum Biol. 1977 Nov;4(6):501–523. doi: 10.1080/03014467700002511. [DOI] [PubMed] [Google Scholar]
- Rona R. J., Chinn S. National Study of Health and Growth: social and biological factors associated with height of children from ethnic groups living in England. Ann Hum Biol. 1986 Sep-Oct;13(5):453–471. doi: 10.1080/03014468600008631. [DOI] [PubMed] [Google Scholar]
- Speight A. N., Lee D. A., Hey E. N. Underdiagnosis and undertreatment of asthma in childhood. Br Med J (Clin Res Ed) 1983 Apr 16;286(6373):1253–1256. doi: 10.1136/bmj.286.6373.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strachan D. P., Anderson H. R., Limb E. S., O'Neill A., Wells N. A national survey of asthma prevalence, severity, and treatment in Great Britain. Arch Dis Child. 1994 Mar;70(3):174–178. doi: 10.1136/adc.70.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer W. M., Osborne M. L., Buist A. S. Temporal trends in hospital-based episodes of asthma care in a health maintenance organization. Am Rev Respir Dis. 1993 Feb;147(2):347–353. doi: 10.1164/ajrccm/147.2.347. [DOI] [PubMed] [Google Scholar]
- Warner J. O., Götz M., Landau L. I., Levison H., Milner A. D., Pedersen S., Silverman M. Management of asthma: a consensus statement. Arch Dis Child. 1989 Jul;64(7):1065–1079. doi: 10.1136/adc.64.7.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner J. O. Review of prescribed treatment for children with asthma in 1990. BMJ. 1995 Sep 9;311(7006):663–666. doi: 10.1136/bmj.311.7006.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S. R. Patient and physician behavior models related to asthma care. Med Care. 1993 Mar;31(3 Suppl):MS49–MS60. doi: 10.1097/00005650-199303001-00008. [DOI] [PubMed] [Google Scholar]
- Wissow L. S., Gittelsohn A. M., Szklo M., Starfield B., Mussman M. Poverty, race, and hospitalization for childhood asthma. Am J Public Health. 1988 Jul;78(7):777–782. doi: 10.2105/ajph.78.7.777. [DOI] [PMC free article] [PubMed] [Google Scholar]


