Abstract
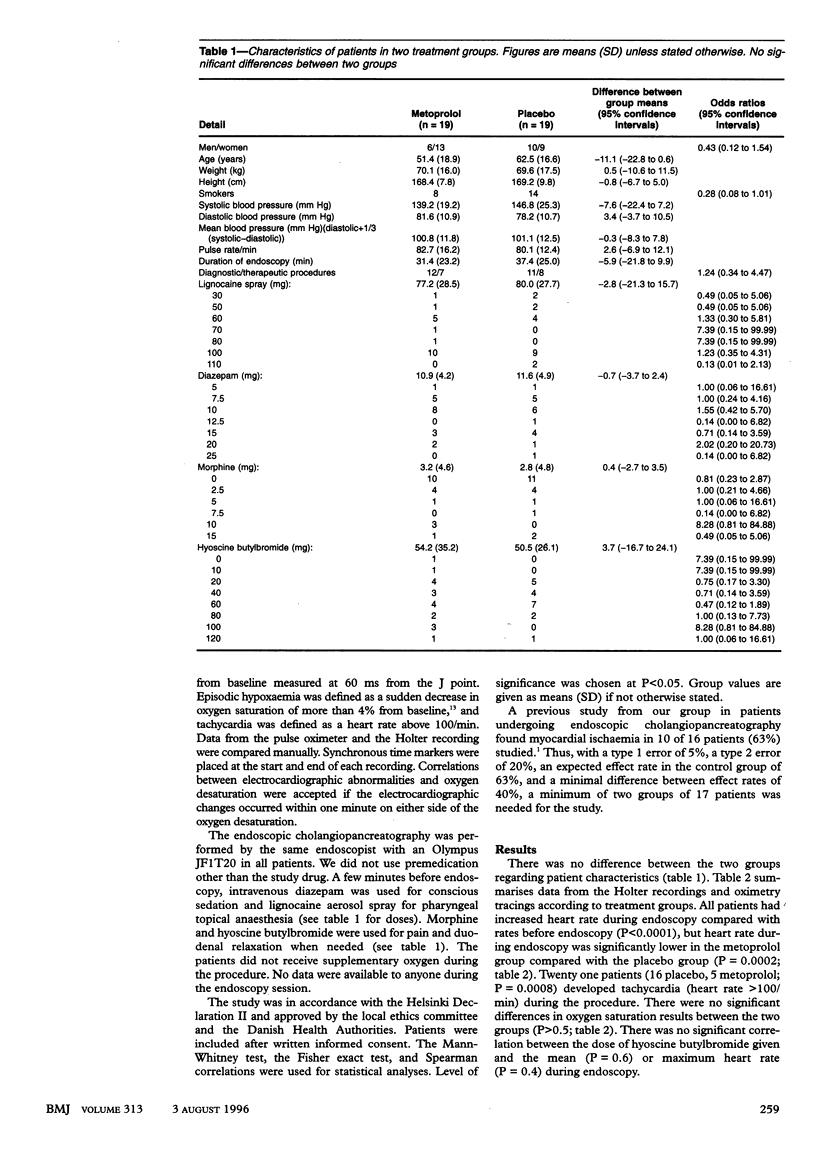
OBJECTIVE--To evaluate the effect of metoprolol, a beta adrenergic blocking drug, on the occurrence of myocardial ischaemia during endoscopic cholangiopancreatography. DESIGN--Double blind, randomised, controlled trial. SETTING--University Hospital. SUBJECTS--38 (two groups of 19) patients scheduled for endoscopic cholangiopancreatography. INTERVENTIONS--Metoprolol 100 mg or placebo as premedication two hours before endoscopy. MAIN OUTCOME MEASURES--Heart rate, arterial oxygen saturation by continuous pulse oximetry, ST segment changes during endoscopic cholangiopancreatography (an ST segment deviation > 1 mV was defined as myocardial ischaemia), electrocardiogram monitored continuously with a Holter tape recorder. RESULTS--All patients had increased heart rate during endoscopy compared with rate before endoscopy, but heart rate during endoscopy was significantly lower in the metoprolol group compared with the placebo group (P = 0.0002). Twenty one patients (16 placebo, 5 metoprolol; P = 0.0008) developed tachycardia (heart rate > 100/min) during the procedure, and 11 patients (10 placebo, 1 metoprolol; P = 0.003) developed myocardial ischaemia. One patient in the placebo group had an acute inferolateral myocardial infarction. In the 10 other patients with signs of myocardial ischaemia during endoscopy the ST deviation disappeared when the endoscope was retracted. In all patients myocardial ischaemia was related to increases in heart rate, and 10 of the 11 patients had tachycardia coherent with myocardial ischaemia. CONCLUSIONS--Metoprolol prevented myocardial ischaemia during endoscopic cholangiopancreatography, probably through lowering the heart rate. Thus, tachycardia seems to be a key pathogenic factor in the development of myocardial ischaemia during endoscopy.
Full text
PDF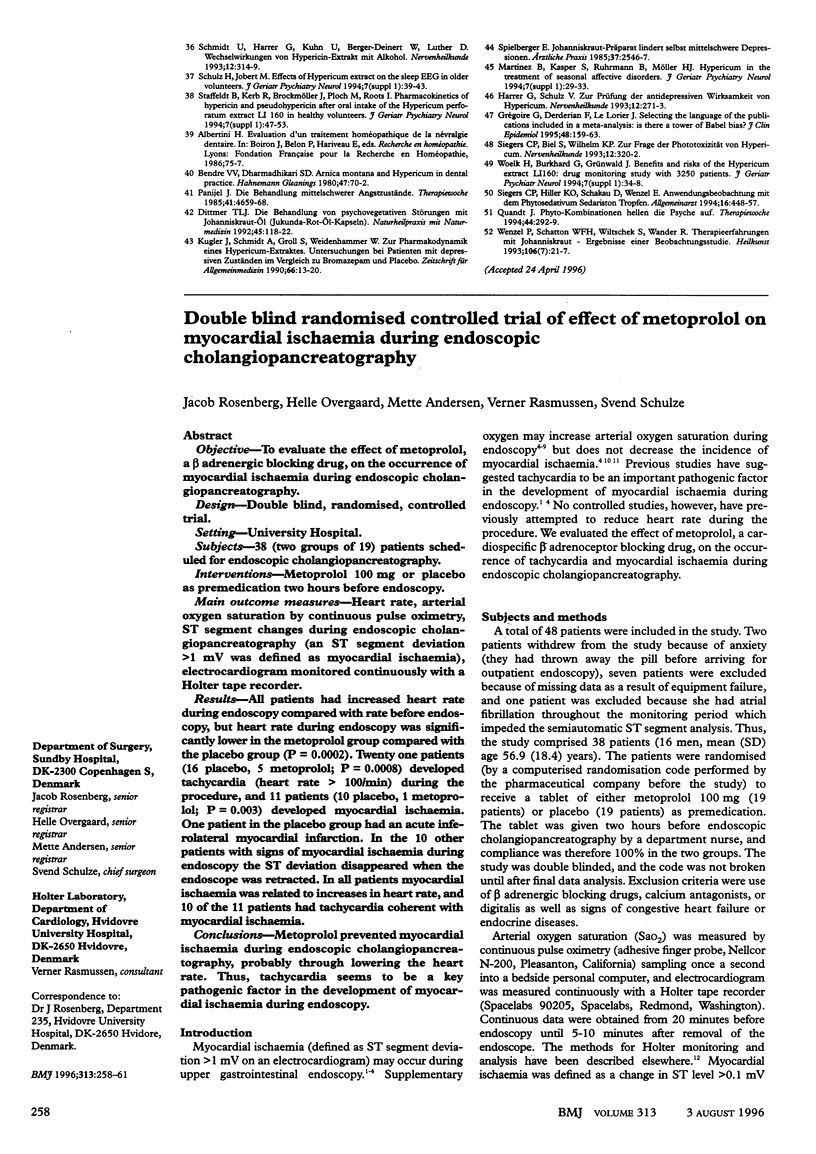

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bell G. D., Bown S., Morden A., Coady T., Logan R. F. Prevention of hypoxaemia during upper-gastrointestinal endoscopy by means of oxygen via nasal cannulae. Lancet. 1987 May 2;1(8540):1022–1024. doi: 10.1016/s0140-6736(87)92282-3. [DOI] [PubMed] [Google Scholar]
- Bell G. D., McCloy R. F., Charlton J. E., Campbell D., Dent N. A., Gear M. W., Logan R. F., Swan C. H. Recommendations for standards of sedation and patient monitoring during gastrointestinal endoscopy. Gut. 1991 Jul;32(7):823–827. doi: 10.1136/gut.32.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling T. E., Hadjiminas C. L., Polson R. J., Baron J. H., Foale R. A. Effects of supplemental oxygen on cardiac rhythm during upper gastrointestinal endoscopy: a randomised controlled double blind trial. Gut. 1993 Nov;34(11):1492–1497. doi: 10.1136/gut.34.11.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita R., Kumura F. Arrythmias and ischemic changes of the heart induced by gastric endoscopic procedures. Am J Gastroenterol. 1975 Jul;64(1):44–48. [PubMed] [Google Scholar]
- Griffin S. M., Chung S. C., Leung J. W., Li A. K. Effect of intranasal oxygen on hypoxia and tachycardia during endoscopic cholangiopancreatography. BMJ. 1990 Jan 13;300(6717):83–84. doi: 10.1136/bmj.300.6717.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines D. J., Bibbey D., Green J. R. Does nasal oxygen reduce the cardiorespiratory problems experienced by elderly patients undergoing endoscopic retrograde cholangiopancreatography? Gut. 1992 Jul;33(7):973–975. doi: 10.1136/gut.33.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakobsen C. J., Blom L. Effect of pre-operative metoprolol on cardiovascular and catecholamine response and bleeding during hysterectomy. Eur J Anaesthesiol. 1992 May;9(3):209–215. [PubMed] [Google Scholar]
- Jakobsen C. J., Blom L. Pre-operative assessment of anxiety and measurement of arterial plasma catecholamine concentrations. The effect of oral beta-adrenergic blockade with metoprolol. Anaesthesia. 1989 Mar;44(3):249–252. doi: 10.1111/j.1365-2044.1989.tb11236.x. [DOI] [PubMed] [Google Scholar]
- Jurell K. R., O'Connor K. W., Slack J., Fraiz J., Shaar C. J., Kent L., Callon R. Effect of supplemental oxygen on cardiopulmonary changes during gastrointestinal endoscopy. Gastrointest Endosc. 1994 Nov-Dec;40(6):665–670. [PubMed] [Google Scholar]
- Mackenzie J. W., Bird J. Timolol: a non-sedative anxiolytic premedicant for day cases. BMJ. 1989 Feb 11;298(6670):363–364. doi: 10.1136/bmj.298.6670.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray A. W., Morran C. G., Kenny G. N., Macfarlane P., Anderson J. R. Examination of cardiorespiratory changes during upper gastrointestinal endoscopy. Comparison of monitoring of arterial oxygen saturation, arterial pressure and the electrocardiogram. Anaesthesia. 1991 Mar;46(3):181–184. doi: 10.1111/j.1365-2044.1991.tb09404.x. [DOI] [PubMed] [Google Scholar]
- Pasternack P. F., Grossi E. A., Baumann F. G., Riles T. S., Lamparello P. J., Giangola G., Primis L. K., Mintzer R., Imparato A. M. Beta blockade to decrease silent myocardial ischemia during peripheral vascular surgery. Am J Surg. 1989 Aug;158(2):113–116. doi: 10.1016/0002-9610(89)90357-7. [DOI] [PubMed] [Google Scholar]
- Rosenberg J., Jørgensen L. N., Rasmussen V., Vibits H., Hansen P. E. Hypoxaemia and myocardial ischaemia during and after endoscopic cholangiopancreatography: call for further studies. Scand J Gastroenterol. 1992 Aug;27(8):717–720. doi: 10.3109/00365529209000147. [DOI] [PubMed] [Google Scholar]
- Rosenberg J. Late postoperative hypoxaemia. Mechanisms and clinical implications. Dan Med Bull. 1995 Feb;42(1):40–46. [PubMed] [Google Scholar]
- Rosenberg J., Rasmussen V., von Jessen F., Ullstad T., Kehlet H. Late postoperative episodic and constant hypoxaemia and associated ECG abnormalities. Br J Anaesth. 1990 Nov;65(5):684–691. doi: 10.1093/bja/65.5.684. [DOI] [PubMed] [Google Scholar]
- Rosenberg J., Stausholm K., Andersen I. B., Pedersen M. H., Brinch K., Rasmussen V., Matzen P. No effect of oxygen therapy on myocardial ischaemia during gastroscopy. Scand J Gastroenterol. 1996 Feb;31(2):200–205. doi: 10.3109/00365529609031986. [DOI] [PubMed] [Google Scholar]
- Wesslén O., Hallhagen S., Ekroth R., Jagenburg R., Joachimsson P. O., Nordgren L., Nyström S. O., Tydén H. High-dose intravenous beta 1-blockade in patients early after cardiac operations. Negative inotropism versus myocardial oxygen economy. J Thorac Cardiovasc Surg. 1992 Dec;104(6):1672–1678. [PubMed] [Google Scholar]


