Abstract
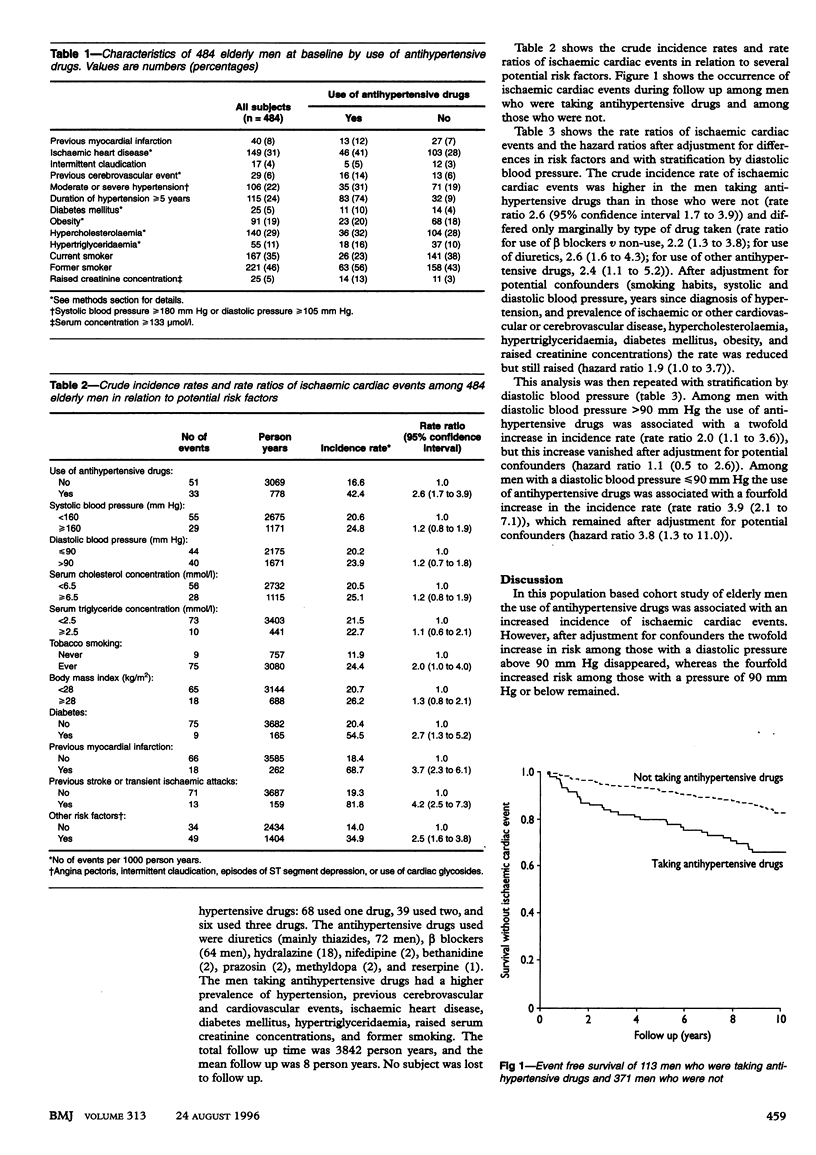
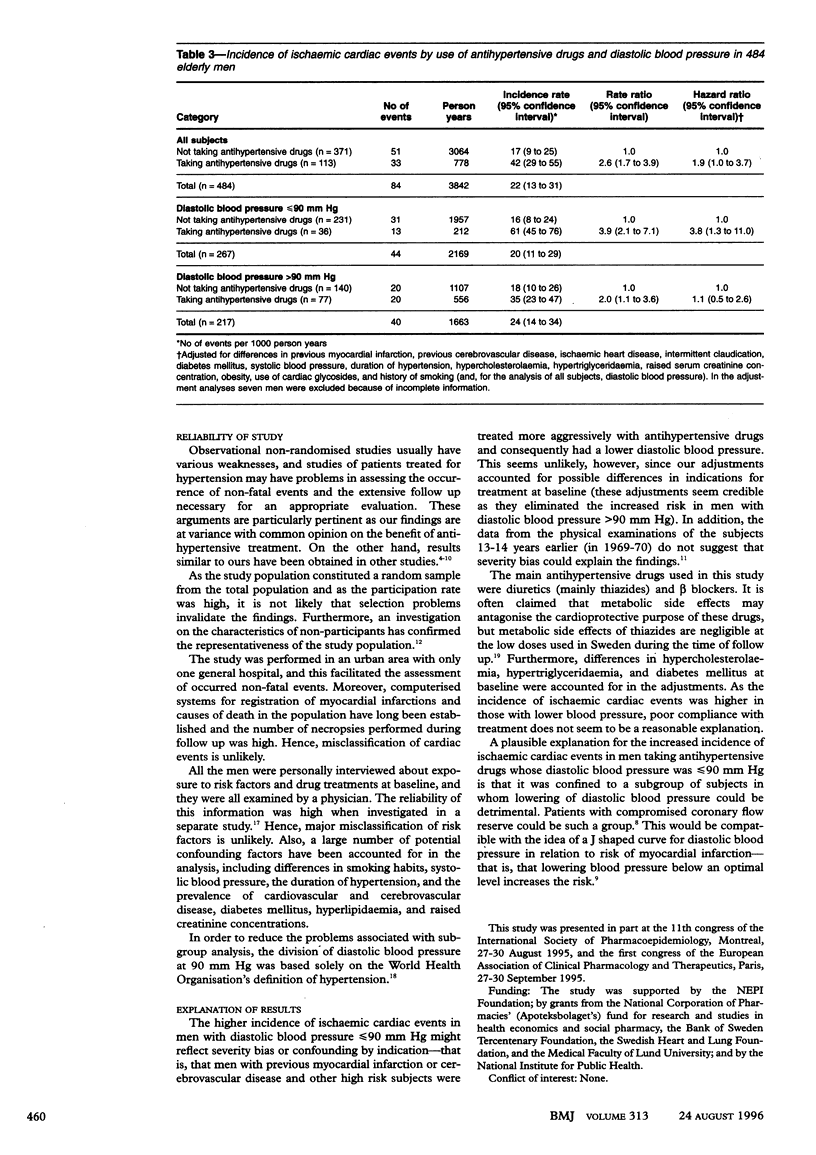
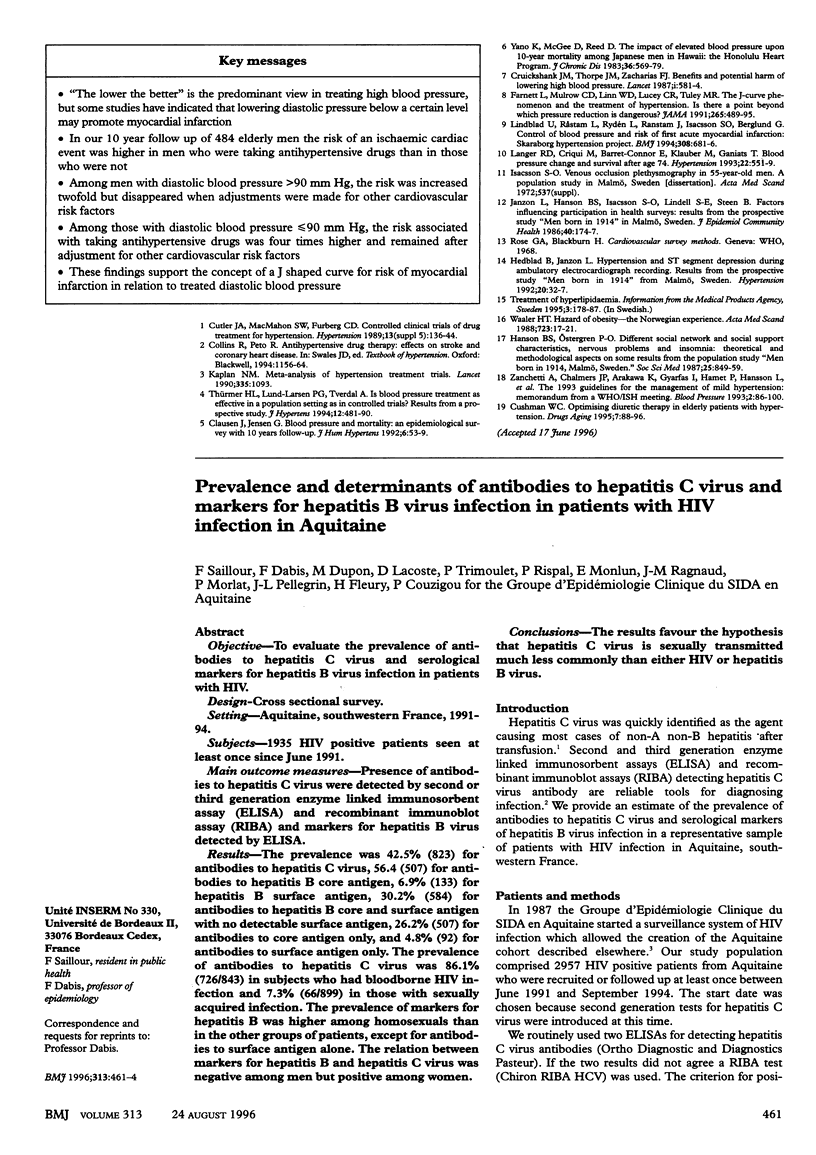
OBJECTIVE: To analyse the association between use of antihypertensive treatment, diastolic blood pressure, and long term incidence of ischaemic cardiac events in elderly men. DESIGN: Population based cohort study. Baseline examination in 1982-3 and follow up for up to 10 years. SETTING: Malmŏ, Sweden. SUBJECTS: 484 randomly selected men born in 1914 and living in Malmŏ during 1982. MAIN OUTCOME MEASURES: Observational comparisons of incidence rates and rate and hazard ratios of ischaemic cardiac events (myocardial infarction or death due to chronic ischaemic cardiac disease). RESULTS: The crude incidence rate of ischaemic cardiac events was higher in those subjects who were taking antihypertensive drugs than in those who were not (rate ratio 2.6 (95% confidence interval 1.7 to 3.9)). After adjustment for potential confounders (differences in baseline smoking habits, blood pressure, time since diagnosis of hypertension, ischaemic or other cardiovascular disease, hypercholesterolaemia, hypertriglyceridaemia, diabetes mellitus, obesity, and raised serum creatinine concentration) this rate was reduced but still raised (hazard ratio 1.9 (1.0 to 3.7)). In men with diastolic blood pressure > 90 mm Hg, antihypertensive treatment was associated with a twofold increase in the incidence of ischaemic cardiac events (rate ratio 2.0 (1.1 to 3.6)), which vanished after adjustment for potential confounders (hazard ratio 1.1 (0.5 to 2.6)). In those subjects with diastolic blood pressure < or = 90 mm Hg, antihypertensive treatment was associated with fourfold increase in incidence (rate ratio 3.9 (2.1 to 7.1)), which remained after adjustment for potential confounders (hazard ratio 3.8 (1.3 to 11.0)). CONCLUSION: Antihypertensive treatment may increase the risk of myocardial infarction in elderly men with treated diastolic blood pressures < or = 90 mm Hg.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Clausen J., Jensen G. Blood pressure and mortality: an epidemiological survey with 10 years follow-up. J Hum Hypertens. 1992 Feb;6(1):53–59. [PubMed] [Google Scholar]
- Cruickshank J. M., Thorp J. M., Zacharias F. J. Benefits and potential harm of lowering high blood pressure. Lancet. 1987 Mar 14;1(8533):581–584. doi: 10.1016/s0140-6736(87)90231-5. [DOI] [PubMed] [Google Scholar]
- Cushman W. C. Optimising diuretic therapy in elderly patients with hypertension. Drugs Aging. 1995 Aug;7(2):88–96. doi: 10.2165/00002512-199507020-00003. [DOI] [PubMed] [Google Scholar]
- Farnett L., Mulrow C. D., Linn W. D., Lucey C. R., Tuley M. R. The J-curve phenomenon and the treatment of hypertension. Is there a point beyond which pressure reduction is dangerous? JAMA. 1991 Jan 23;265(4):489–495. [PubMed] [Google Scholar]
- Hanson B. S., Ostergren P. O. Different social network and social support characteristics, nervous problems and insomnia: theoretical and methodological aspects on some results from the population study 'men born in 1914', Malmö, Sweden. Soc Sci Med. 1987;25(7):849–859. doi: 10.1016/0277-9536(87)90043-8. [DOI] [PubMed] [Google Scholar]
- Hedblad B., Janzon L. Hypertension and ST segment depression during ambulatory electrocardiographic recording. Results from the prospective population study 'men born in 1914' from Malmö, Sweden. Hypertension. 1992 Jul;20(1):32–37. doi: 10.1161/01.hyp.20.1.32. [DOI] [PubMed] [Google Scholar]
- Janzon L., Hanson B. S., Isacsson S. O., Lindell S. E., Steen B. Factors influencing participation in health surveys. Results from prospective population study 'Men born in 1914' in Malmö, Sweden. J Epidemiol Community Health. 1986 Jun;40(2):174–177. doi: 10.1136/jech.40.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer R. D., Criqui M. H., Barrett-Connor E. L., Klauber M. R., Ganiats T. G. Blood pressure change and survival after age 75. Hypertension. 1993 Oct;22(4):551–559. doi: 10.1161/01.hyp.22.4.551. [DOI] [PubMed] [Google Scholar]
- Lindblad U., Råstam L., Rydén L., Ranstam J., Isacsson S. O., Berglund G. Control of blood pressure and risk of first acute myocardial infarction: Skaraborg hypertension project. BMJ. 1994 Mar 12;308(6930):681–686. doi: 10.1136/bmj.308.6930.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thürmer H. L., Lund-Larsen P. G., Tverdal A. Is blood pressure treatment as effective in a population setting as in controlled trials? Results from a prospective study. J Hypertens. 1994 Apr;12(4):481–490. [PubMed] [Google Scholar]
- Waaler H. T. Hazard of obesity--the Norwegian experience. Acta Med Scand Suppl. 1988;723:17–21. doi: 10.1111/j.0954-6820.1987.tb05924.x. [DOI] [PubMed] [Google Scholar]
- Yano K., McGee D., Reed D. M. The impact of elevated blood pressure upon 10-year mortality among Japanese men in Hawaii: the Honolulu Heart Program. J Chronic Dis. 1983;36(8):569–579. doi: 10.1016/0021-9681(83)90145-5. [DOI] [PubMed] [Google Scholar]
- Zanchetti A., Chalmers J. P., Arakawa K., Gyarfas I., Hamet P., Hansson L., Julius S., MacMahon S., Mancia G., Ménard J. The 1993 guidelines for the management of mild hypertension: memorandum from a WHO/ISH meeting. Blood Press. 1993 Jun;2(2):86–100. doi: 10.3109/08037059309077535. [DOI] [PubMed] [Google Scholar]


