Abstract
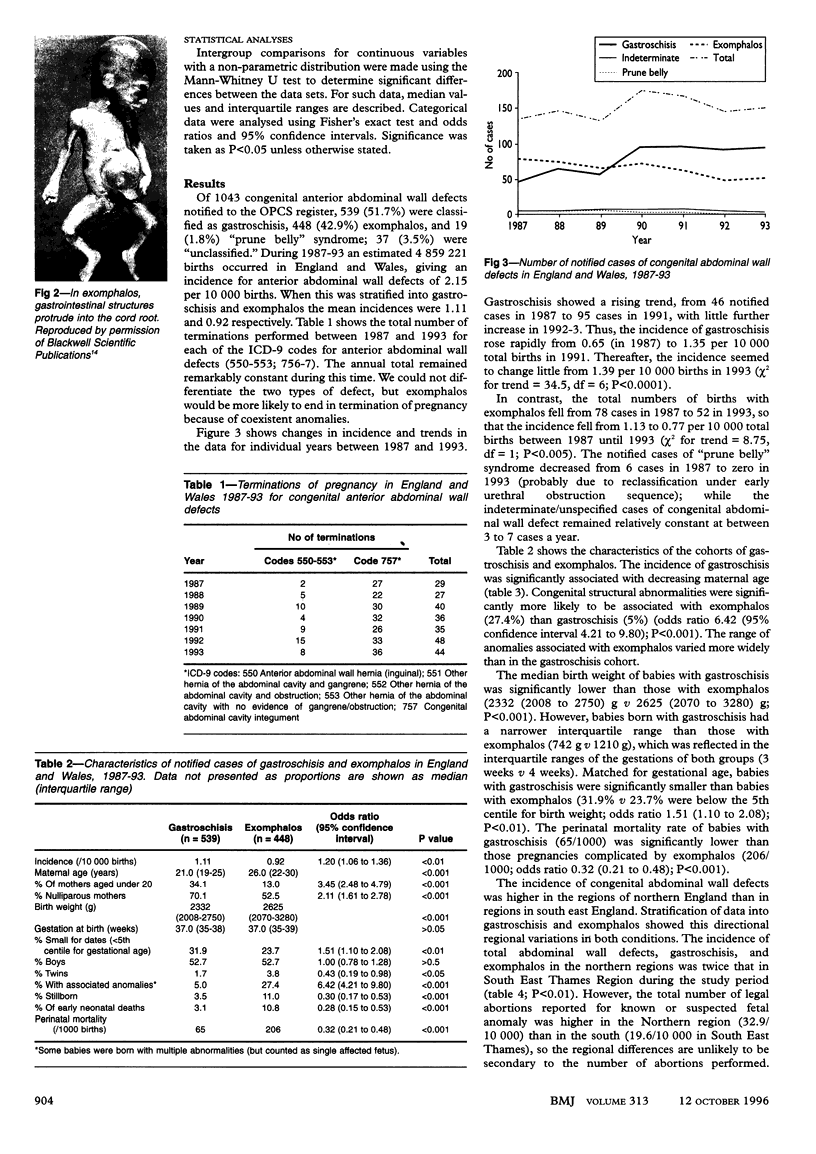
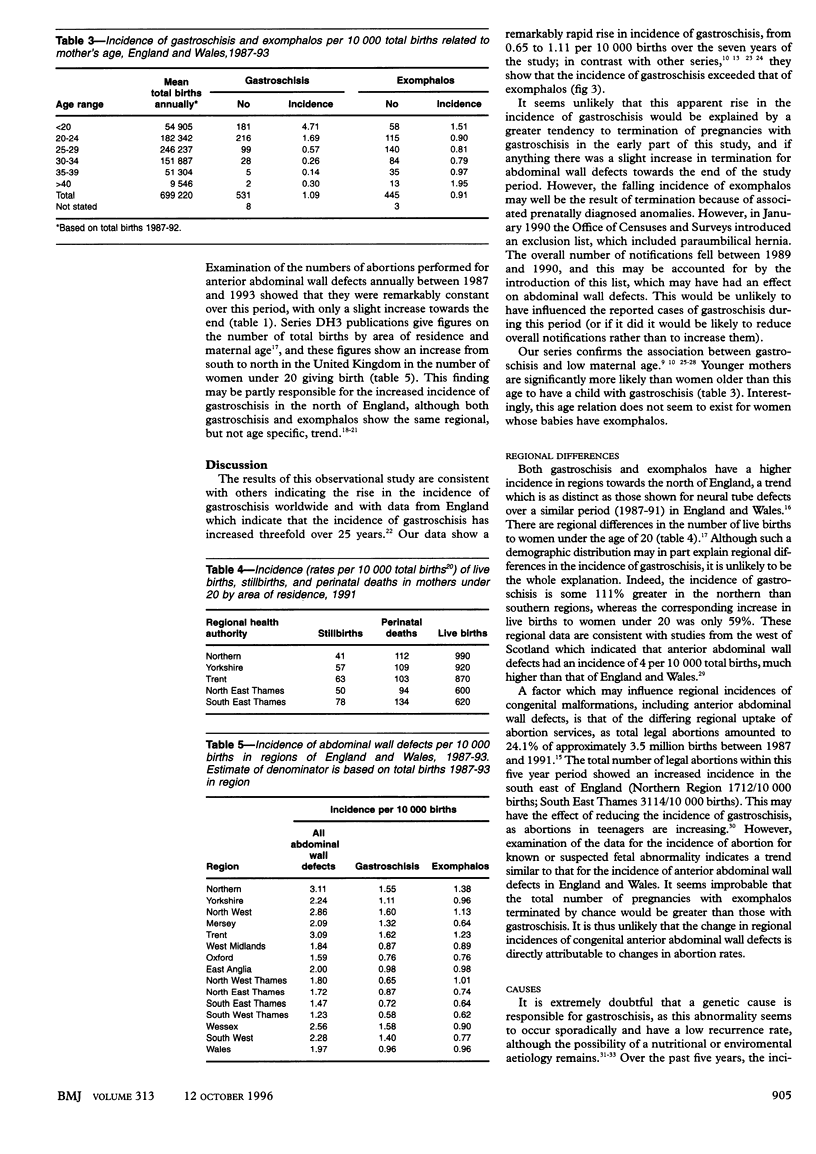
OBJECTIVES: Analysis of incidence and characteristics of congenital abdominal wall defects, with special reference to the differences between the incidence of gastroschisis and exomphalos (omphalocele). DESIGN: Retrospective analysis using data from the Office of Population Censuses and Surveys (recoded to differentiate exomphalos and gastroschisis) and the National Congenital Malformation Notification Scheme. SETTING: England and Wales, 1987 to 1993. RESULTS: 1043 congenital anterior abdominal wall defects were notified within the seven year study period. Of these, 539 were classified as gastroschisis, 448 as exomphalos, 19 as "prune belly syndrome," and 37 as "unclassified." Gastroschisis doubled in incidence from 0.65 in 1987 to 1.35 per 10,000 total births in 1991, with little further change; the incidence of exomphalos decreased from 1.13 to 0.77 per 10000 births. The overall incidence of notified congenital abdominal wall defects was 2.15 per 10000 total births. Gastroschisis was associated with a lower overall maternal age than exomphalos and with a significantly lower proportion of additional reported congenital malformations (5.0%) than in the cohort with exomphalos (27.4%) (odds ratio 0.14, 95% confidence interval 0.09 to 0.22; P < 0.001). The sex ratio of the two cohorts was the same. The incidence of gastroschisis and exomphalos was higher in the northern regions of England than in the south east of the country. CONCLUSIONS: The national congenital malformation notification system showed an increasing trend in the incidence of fetuses born with gastroschisis and a progressive decreasing incidence of exomphalos in England and Wales between 1987 and 1993. Although the reasons for this are likely to be multifactorial, a true differential change seems likely. The observed increase in incidence of gastroschisis relative to exomphalos and the differentiation in maternal age have implications for resource management within the NHS and warrant further epidemiological monitoring. Regional differences may be due to a dietary or environmental factor, which requires further study.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baird P. A., MacDonald E. C. An epidemiologic study of congenital malformations of the anterior abdominal wall in more than half a million consecutive live births. Am J Hum Genet. 1981 May;33(3):470–478. [PMC free article] [PubMed] [Google Scholar]
- Calzolari E., Volpato S., Bianchi F., Cianciulli D., Tenconi R., Clementi M., Calabro A., Lungarotti S., Mastroiacovo P. P., Botto L. Omphalocele and gastroschisis: a collaborative study of five Italian congenital malformation registries. Teratology. 1993 Jan;47(1):47–55. doi: 10.1002/tera.1420470109. [DOI] [PubMed] [Google Scholar]
- Doyle P. E., Beral V., Botting B., Wale C. J. Congenital malformations in twins in England and Wales. J Epidemiol Community Health. 1991 Mar;45(1):43–48. doi: 10.1136/jech.45.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisancho A. R., Matos J., Flegel P. Maternal nutritional status and adolescent pregnancy outcome. Am J Clin Nutr. 1983 Nov;38(5):739–746. doi: 10.1093/ajcn/38.5.739. [DOI] [PubMed] [Google Scholar]
- Goldbaum G., Daling J., Milham S. Risk factors for gastroschisis. Teratology. 1990 Oct;42(4):397–403. doi: 10.1002/tera.1420420408. [DOI] [PubMed] [Google Scholar]
- Hemminki K., Saloniemi I., Kyyrönen P., Kekomäki M. Gastroschisis and omphalocele in Finland in the 1970s: prevalence at birth and its correlates. J Epidemiol Community Health. 1982 Dec;36(4):289–293. doi: 10.1136/jech.36.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollabaugh R. S., Boles E. T., Jr The management of gastroschisis. J Pediatr Surg. 1973 Apr;8(2):263–270. doi: 10.1016/s0022-3468(73)80094-6. [DOI] [PubMed] [Google Scholar]
- Hoyme H. E., Higginbottom M. C., Jones K. L. The vascular pathogenesis of gastroschisis: intrauterine interruption of the omphalomesenteric artery. J Pediatr. 1981 Feb;98(2):228–231. doi: 10.1016/s0022-3476(81)80640-3. [DOI] [PubMed] [Google Scholar]
- Hoyme H. E., Jones M. C., Jones K. L. Gastroschisis: abdominal wall disruption secondary to early gestational interruption of the omphalomesenteric artery. Semin Perinatol. 1983 Oct;7(4):294–298. [PubMed] [Google Scholar]
- Knox E. G., Armstrong E. H., Lancashire R. The quality of notification of congenital malformations. J Epidemiol Community Health. 1984 Dec;38(4):296–305. doi: 10.1136/jech.38.4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOORE T. C. GASTROSCHISIS WITH ANTENATAL EVISCERATION OF INTESTINES AND URINARY BLADDER. Ann Surg. 1963 Aug;158:263–269. doi: 10.1097/00000658-196308000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOORE T. C., STOKES G. E. Gastroschisis; report of two cases treated by a modification of the gross operation for omphalocele. Surgery. 1953 Jan;33(1):112–120. [PubMed] [Google Scholar]
- Martínez-Frías M. L., Salvador J., Prieto L., Zaplana J. Epidemiological study of gastroschisis and omphalocele in Spain. Teratology. 1984 Jun;29(3):377–382. doi: 10.1002/tera.1420290308. [DOI] [PubMed] [Google Scholar]
- Mayer T., Black R., Matlak M. E., Johnson D. G. Gastroschisis and omphalocele. An eight-year review. Ann Surg. 1980 Dec;192(6):783–787. doi: 10.1097/00000658-198012000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore T. C. Gastroschisis and omphalocele: clinical differences. Surgery. 1977 Nov;82(5):561–568. [PubMed] [Google Scholar]
- Morrow R. J., Whittle M. J., McNay M. B., Raine P. A., Gibson A. A., Crossley J. Prenatal diagnosis and management of anterior abdominal wall defects in the west of Scotland. Prenat Diagn. 1993 Feb;13(2):111–115. doi: 10.1002/pd.1970130205. [DOI] [PubMed] [Google Scholar]
- Payne J. N. Limitations of the OPCS congenital malformation notification system illustrated by examination of congenital malformations of the cardiovascular system in districts within the Trent Region. Public Health. 1992 Nov;106(6):437–448. doi: 10.1016/s0033-3506(05)80458-5. [DOI] [PubMed] [Google Scholar]
- Roeper P. J., Harris J., Lee G., Neutra R. Secular rates and correlates for gastroschisis in California (1968-1977). Teratology. 1987 Apr;35(2):203–210. doi: 10.1002/tera.1420350206. [DOI] [PubMed] [Google Scholar]
- Swerdlow A. J., Melzer D. The value of England and Wales congenital malformation notification scheme data for epidemiology: male genital tract malformations. J Epidemiol Community Health. 1988 Mar;42(1):8–13. doi: 10.1136/jech.42.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]