Abstract
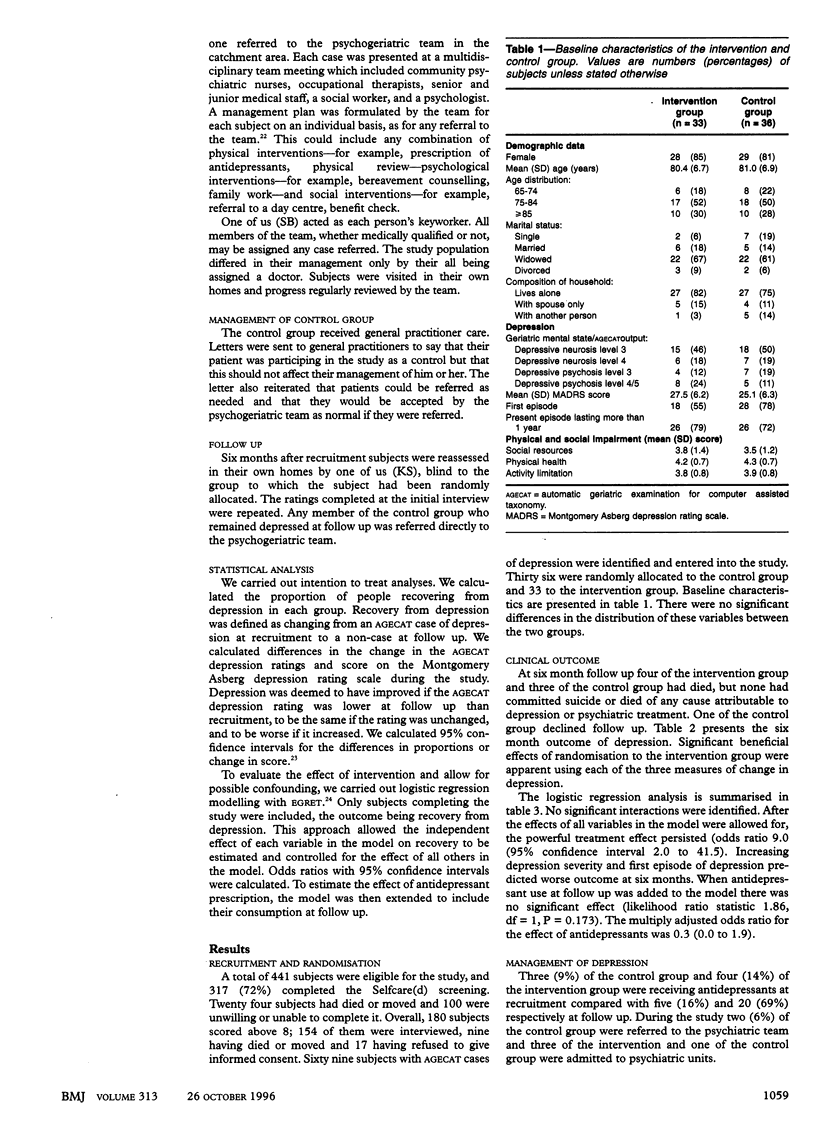
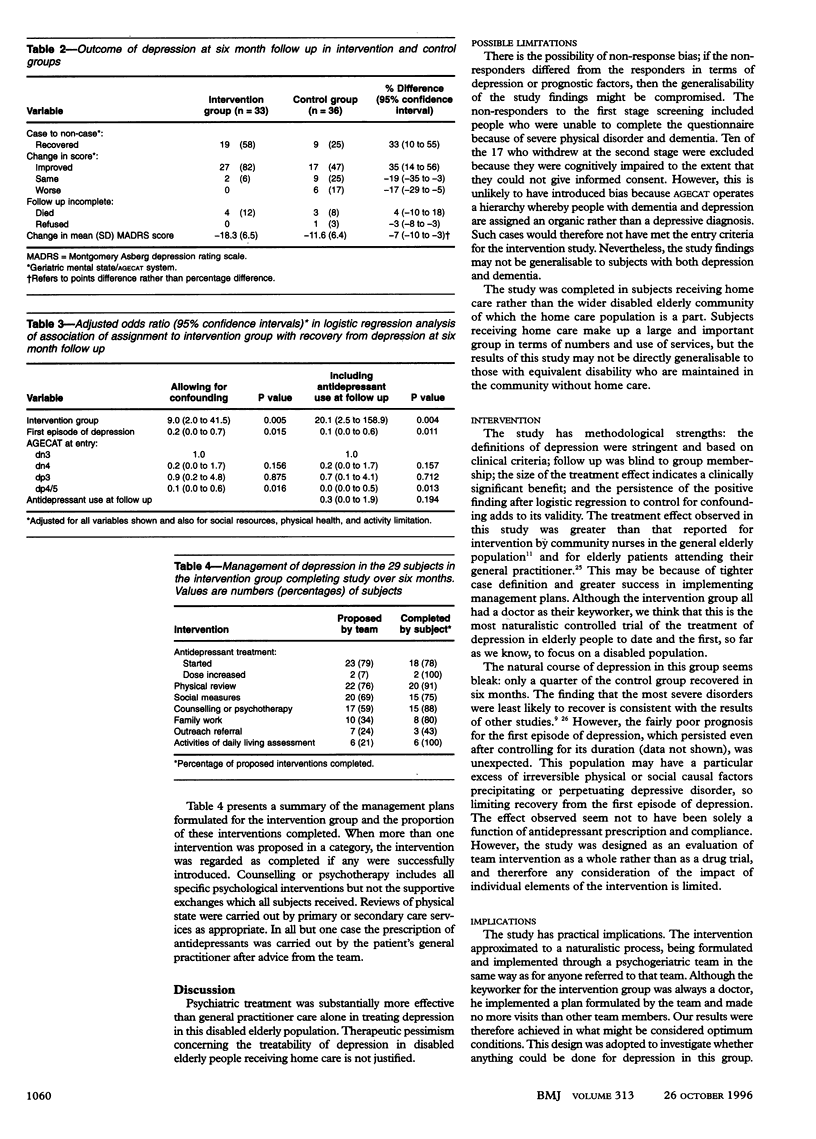
OBJECTIVE: To investigate the efficacy of intervention by a psychogeriatric team in the treatment of depression in elderly disabled people receiving home care from their local authority. DESIGN: Randomised controlled trial with blind follow up six months after recruitment. SETTING: Community of south east London. SUBJECTS: 69 people aged 65 or over who received home care and were depressed according to criteria of the standardised automatic geriatric examination for computer assisted taxonomy (AGECAT). 33 were randomly allocated to an intervention group and 36 to a control group. INTERVENTION: Members of the intervention group received an individual package of care that was formulated by the community psychogeriatric team in their catchment area and implemented by a researcher working as a member of that team. The control group received normal general practitioner care. MAIN OUTCOME MEASURES: Recovery from depression (AGECAT case at recruitment but non-case at follow up). RESULTS: Data were analysed on an intention to treat basis. 19 (58%) of the intervention group recovered compared with only nine (25%) of the control group, a difference of 33% (95% confidence interval 10% to 55%). This powerful treatment effect persisted after controlling for possible confounders in logistic regression analysis, with members of the intervention group more likely than members of the control group to have recovered at follow up (odds ratio 9.0 (2.0 to 41.5)). This did not seem to be a simple effect of antidepressant prescription: use of antidepressants at follow up did not have a significant effect (multiply adjusted odds ratio 0.3 (0.0 to 1.9)). CONCLUSIONS: Depression is treatable in elderly people receiving home care. Therapeutic nihilism based on an assumed poor response to treatment in these socially isolated, disabled elderly people in the community is not supported.
Full text
PDF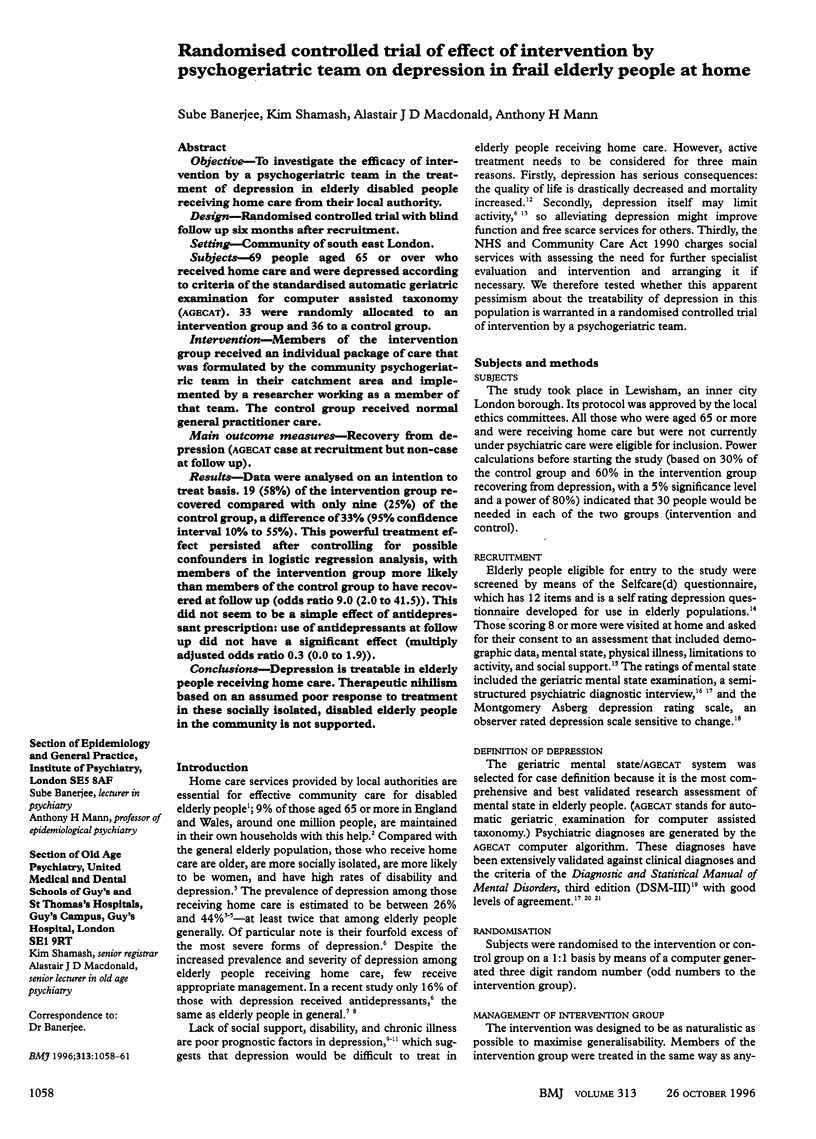

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldwin R. C., Jolley D. J. The prognosis of depression in old age. Br J Psychiatry. 1986 Nov;149:574–583. doi: 10.1192/bjp.149.5.574. [DOI] [PubMed] [Google Scholar]
- Banerjee S., Macdonald A. Mental disorder in an elderly home care population: associations with health and social service use. Br J Psychiatry. 1996 Jun;168(6):750–756. doi: 10.1192/bjp.168.6.750. [DOI] [PubMed] [Google Scholar]
- Blanchard M. R., Waterreus A., Mann A. H. The nature of depression among older people in inner London, and the contact with primary care. Br J Psychiatry. 1994 Mar;164(3):396–402. doi: 10.1192/bjp.164.3.396. [DOI] [PubMed] [Google Scholar]
- Blazer D., Williams C. D. Epidemiology of dysphoria and depression in an elderly population. Am J Psychiatry. 1980 Apr;137(4):439–444. doi: 10.1176/ajp.137.4.439. [DOI] [PubMed] [Google Scholar]
- Burnett J. W., Calton G. J., Burnett H. W. Jellyfish envenomation syndromes. J Am Acad Dermatol. 1986 Jan;14(1):100–106. doi: 10.1016/s0190-9622(86)70013-3. [DOI] [PubMed] [Google Scholar]
- Copeland J. R., Davidson I. A., Dewey M. E., Gilmore C., Larkin B. A., McWilliam C., Saunders P. A., Scott A., Sharma V., Sullivan C. Alzheimer's disease, other dementias, depression and pseudodementia: prevalence, incidence and three-year outcome in Liverpool. Br J Psychiatry. 1992 Aug;161:230–239. doi: 10.1192/bjp.161.2.230. [DOI] [PubMed] [Google Scholar]
- Copeland J. R., Dewey M. E., Griffiths-Jones H. M. A computerized psychiatric diagnostic system and case nomenclature for elderly subjects: GMS and AGECAT. Psychol Med. 1986 Feb;16(1):89–99. doi: 10.1017/s0033291700057779. [DOI] [PubMed] [Google Scholar]
- Copeland J. R., Kelleher M. J., Kellett J. M., Gourlay A. J., Gurland B. J., Fleiss J. L., Sharpe L. A semi-structured clinical interview for the assessment of diagnosis and mental state in the elderly: the Geriatric Mental State Schedule. I. Development and reliability. Psychol Med. 1976 Aug;6(3):439–449. doi: 10.1017/s0033291700015889. [DOI] [PubMed] [Google Scholar]
- Iliffe S., Haines A., Gallivan S., Booroff A., Goldenberg E., Morgan P. Assessment of elderly people in general practice. 1. Social circumstances and mental state. Br J Gen Pract. 1991 Jan;41(342):9–12. [PMC free article] [PubMed] [Google Scholar]
- Iliffe S., Tai S. S., Haines A., Booroff A., Goldenberg E., Morgan P., Gallivan S. Assessment of elderly people in general practice. 4. Depression, functional ability and contact with services. Br J Gen Pract. 1993 Sep;43(374):371–374. [PMC free article] [PubMed] [Google Scholar]
- Mann A. H., Jenkins R., Belsey E. The twelve-month outcome of patients with neurotic illness in general practice. Psychol Med. 1981 Aug;11(3):535–550. doi: 10.1017/s0033291700052855. [DOI] [PubMed] [Google Scholar]
- Montgomery S. A., Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979 Apr;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]


