Abstract
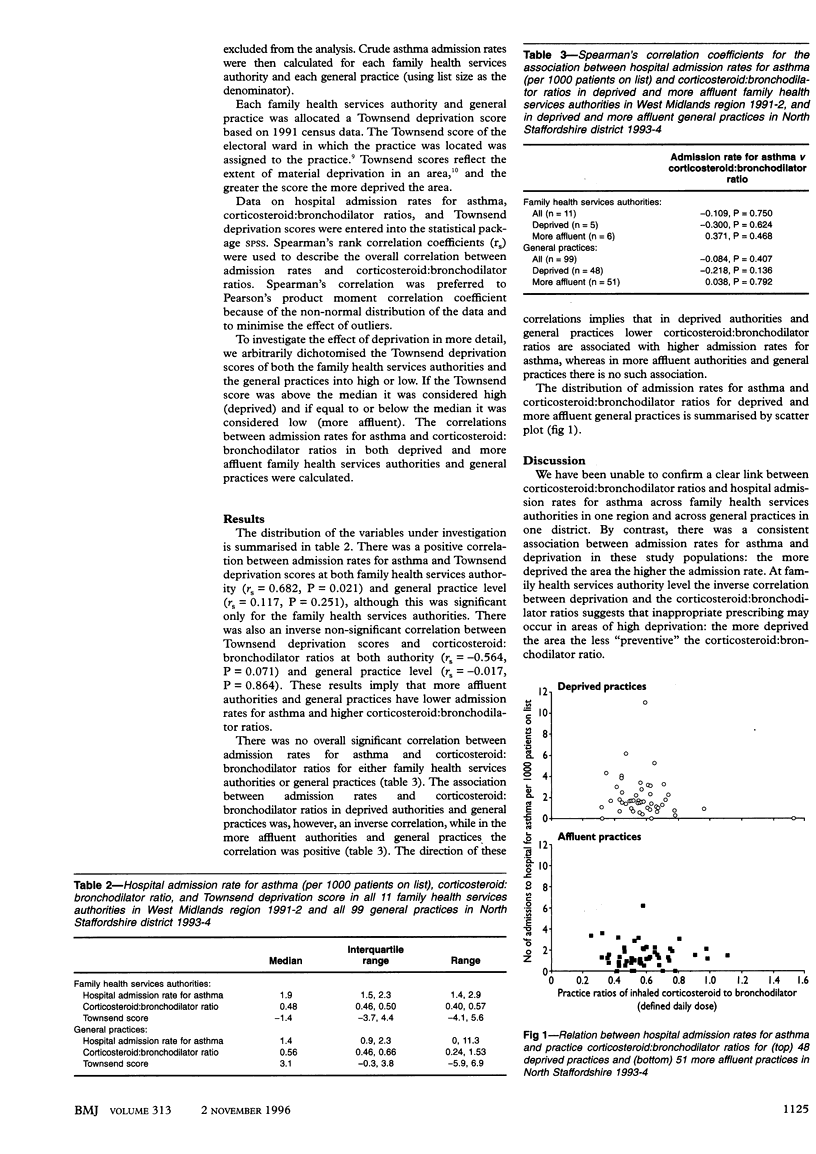
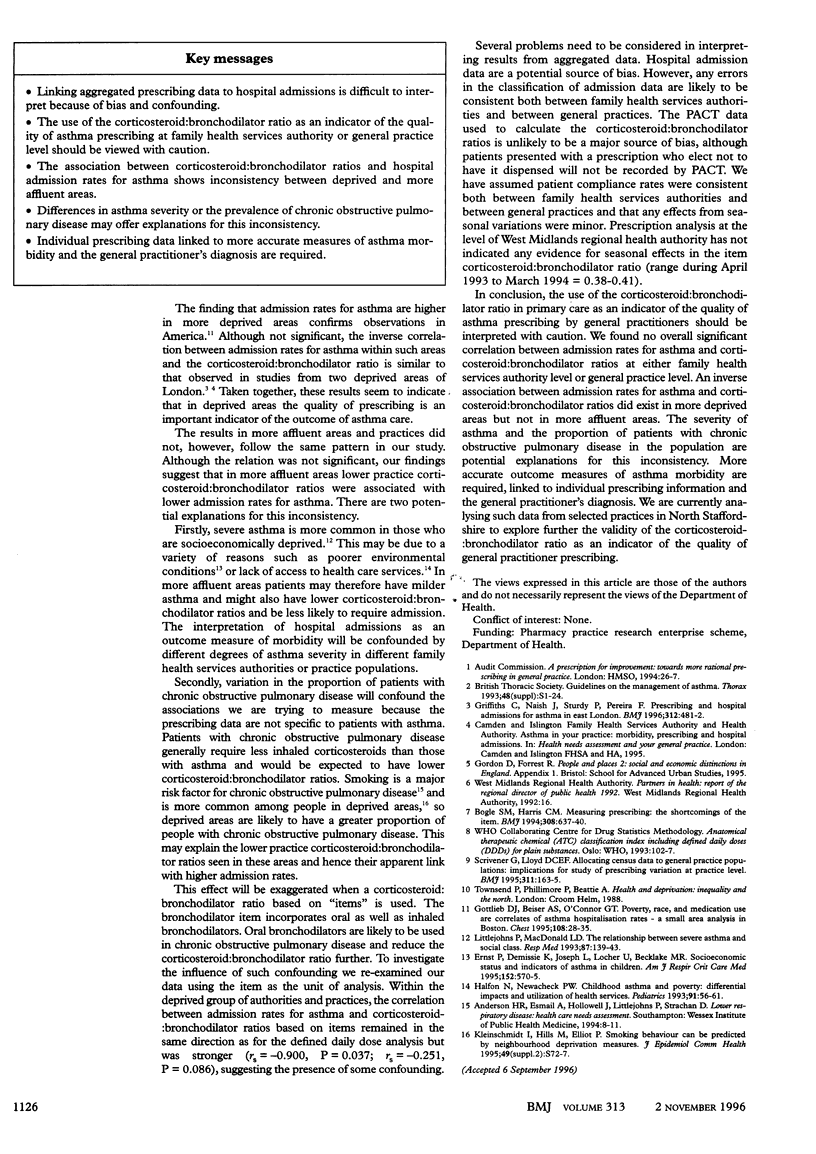
OBJECTIVE: To investigate the ratio of inhaled corticosteroid to bronchodilator as a measure of the quality of asthma prescribing by general practitioners. DESIGN: Ecological cross sectional study linking general practitioner asthma prescribing with hospital admission data and a measure of deprivation. SUBJECTS: 11 family health services authorities in the West Midlands region and 99 general practices in North Staffordshire. MAIN OUTCOME MEASURES: Hospital admission rates for asthma; the ratio of inhaled corticosteroid to bronchodilator; and Townsend deprivation scores. RESULTS: No overall significant correlation was found between admission rates for asthma and corticosteroid:bronchodilator ratios for family health services authorities (Spearman's rs = -0.109, P = 0.750) or general practices (rs = -0.084, P = 0.407). In deprived family health services authority areas and general practices an inverse non-significant correlation existed between admission rates for asthma and corticosteroid:bronchodilator ratios (rs = -0.300, P = 0.624; rs = -0.218, P = 0.136). In contrast, in more affluent areas and general practices a positive non-significant correlation existed between admission rates and corticosteroid:bronchodilator ratios (rs = 0.371, P = 0.468; rs = 0.038, P = 0.792). CONCLUSION: Although the corticosteroid:bronchodilator ratio may be a valid indicator of the quality of prescribing for individual patients with asthma, caution should be applied in interpreting aggregated ratios. Differences in the severity of asthma or the prevalence of chronic obstructive pulmonary disease may explain inconsistent associations between admission rates for asthma and corticosteroid:bronchodilator ratios in family health services authorities and general practices with different deprivation scores.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bogle S. M., Harris C. M. Measuring prescribing: the shortcomings of the item. BMJ. 1994 Mar 5;308(6929):637–640. doi: 10.1136/bmj.308.6929.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb D. J., Beiser A. S., O'Connor G. T. Poverty, race, and medication use are correlates of asthma hospitalization rates. A small area analysis in Boston. Chest. 1995 Jul;108(1):28–35. doi: 10.1378/chest.108.1.28. [DOI] [PubMed] [Google Scholar]
- Griffiths C., Naish J., Sturdy P., Pereira F. Prescribing and hospital admissions for asthma in east London. BMJ. 1996 Feb 24;312(7029):481–482. doi: 10.1136/bmj.312.7029.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfon N., Newacheck P. W. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993 Jan;91(1):56–61. [PubMed] [Google Scholar]
- Littlejohns P., Macdonald L. D. The relationship between severe asthma and social class. Respir Med. 1993 Feb;87(2):139–143. doi: 10.1016/0954-6111(93)90142-m. [DOI] [PubMed] [Google Scholar]
- Scrivener G., Lloyd D. C. Allocating census data to general practice populations: implications for study of prescribing variation at practice level. BMJ. 1995 Jul 15;311(6998):163–165. doi: 10.1136/bmj.311.6998.163. [DOI] [PMC free article] [PubMed] [Google Scholar]


