Abstract
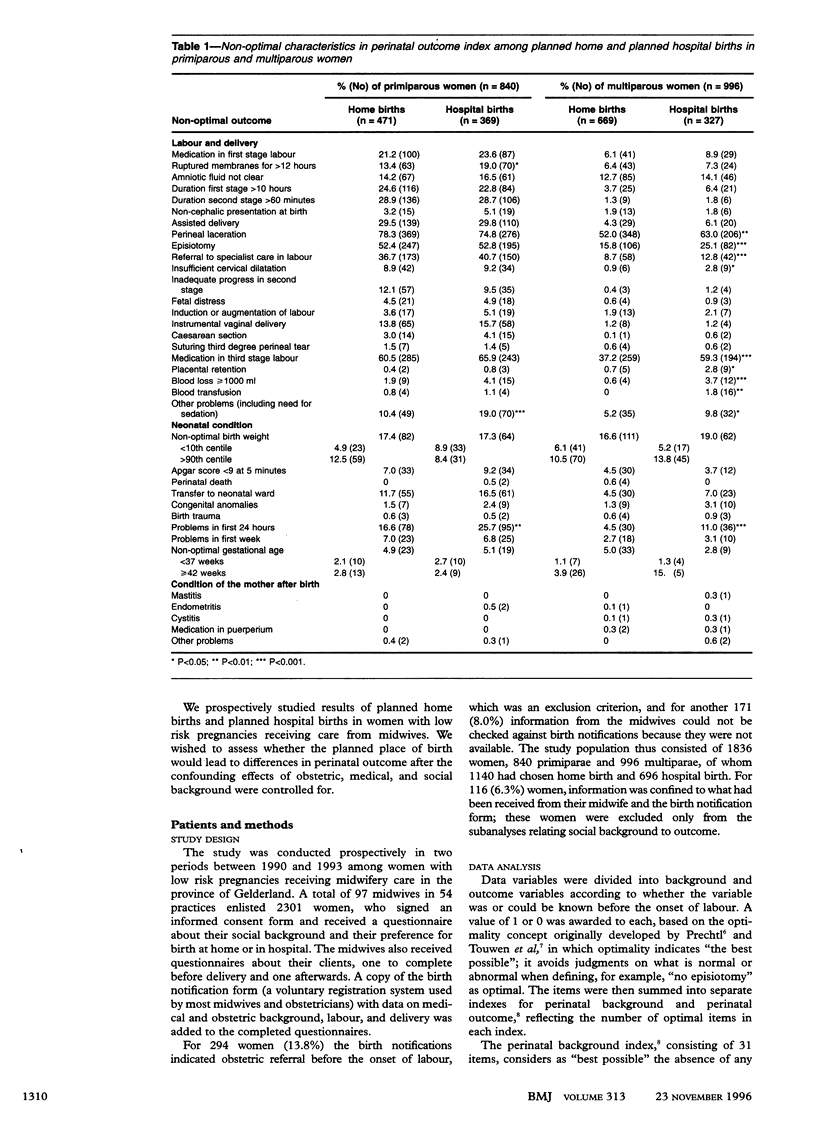
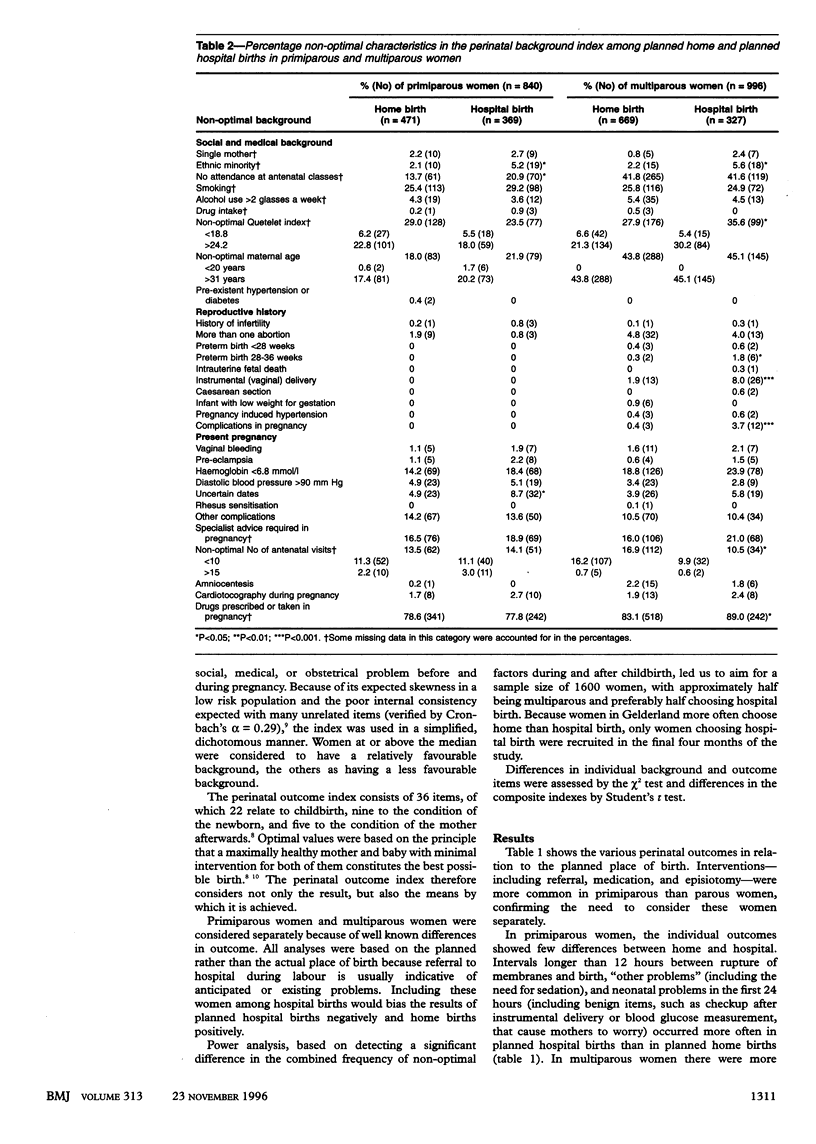
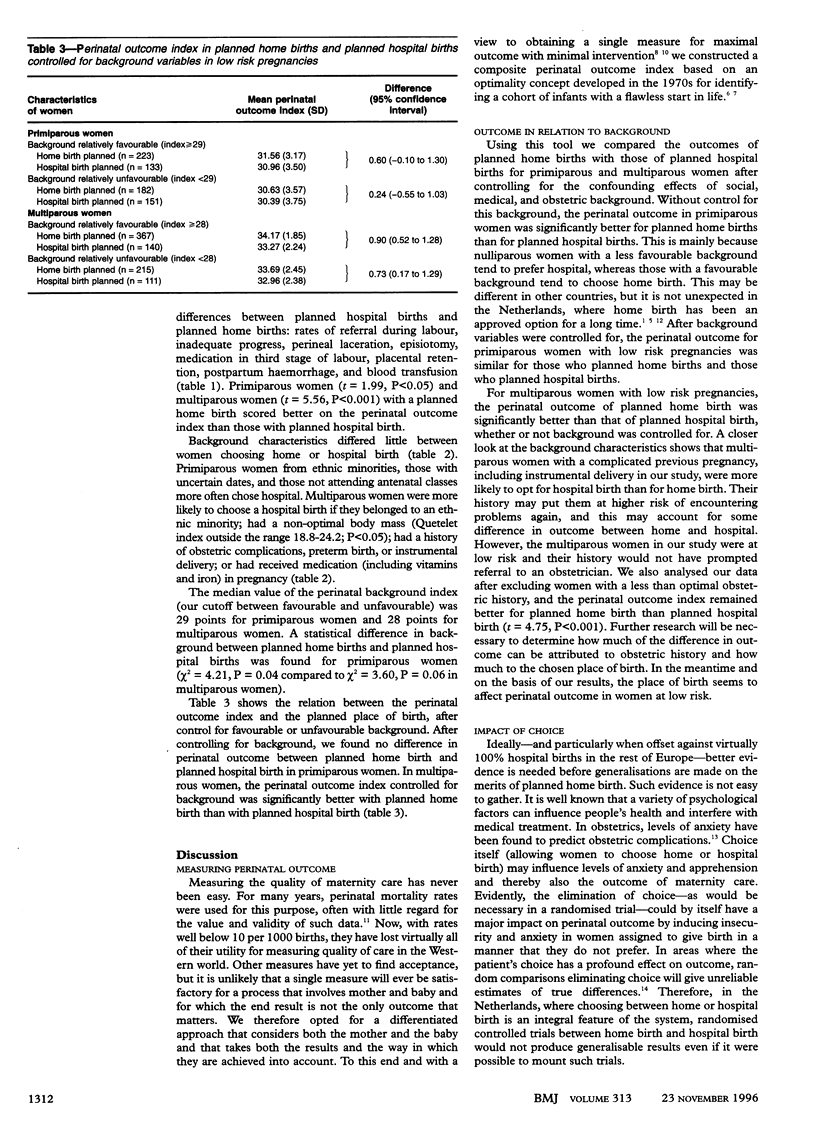
OBJECTIVE: To investigate the relation between the intended place of birth (home or hospital) and perinatal outcome in women with low risk pregnancies after controlling for parity and social, medical, and obstetric background. DESIGN: Analysis of prospective data from midwives and their clients. SETTING: 54 midwifery practices in the province of Gelderland, Netherlands. SUBJECTS: 97 midwives and 1836 women with low risk pregnancies who had planned to give birth at home or in hospital. MAIN OUTCOME MEASURE: Perinatal outcome index based on "maximal result with minimal intervention" and incorporating 22 items on childbirth, 9 on the condition of the newborn, and 5 on the mother after the birth. RESULTS: There was no relation between the planned place of birth and perinatal outcome in primiparous women when controlling for a favourable or less favourable background. In multiparous women, perinatal outcome was significantly better for planned home births than for planned hospital births, with or without control for background variables. CONCLUSIONS: The outcome of planned home births is at least as good as that of planned hospital births in women at low risk receiving midwifery care in the Netherlands.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Crandon A. J. Maternal anxiety and obstetric complications. J Psychosom Res. 1979;23(2):109–111. doi: 10.1016/0022-3999(79)90014-x. [DOI] [PubMed] [Google Scholar]
- Damstra-Wijmenga S. M. Home confinement: the positive results in Holland. J R Coll Gen Pract. 1984 Aug;34(265):425–430. [PMC free article] [PubMed] [Google Scholar]
- McPherson K. The Cochrane Lecture. The best and the enemy of the good: randomised controlled trials, uncertainty, and assessing the role of patient choice in medical decision making. J Epidemiol Community Health. 1994 Feb;48(1):6–15. doi: 10.1136/jech.48.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prechtl H. F. The optimality concept. Early Hum Dev. 1980 Sep;4(3):201–205. doi: 10.1016/0378-3782(80)90026-2. [DOI] [PubMed] [Google Scholar]
- Touwen B. C., Huisjes H. J., Jurgens-van der Zee A. D., Bierman-van Eendenburg M. E., Smrkovsky M., Olinga A. A. Obstetrical condition and neonatal neurological morbidity. An analysis with the help of the optimality concept. Early Hum Dev. 1980 Sep;4(3):207–228. doi: 10.1016/0378-3782(80)90027-4. [DOI] [PubMed] [Google Scholar]
- Treffers P. E., Eskes M., Kleiverda G., van Alten D. Home births and minimal medical interventions. JAMA. 1990 Nov 7;264(17):2203, 2207-8. doi: 10.1001/jama.264.17.2203. [DOI] [PubMed] [Google Scholar]
- Wiegers T. A., Keirse M. J., Berghs G. A., van der Zee J. An approach to measuring quality of midwifery care. J Clin Epidemiol. 1996 Mar;49(3):319–325. doi: 10.1016/0895-4356(95)00549-8. [DOI] [PubMed] [Google Scholar]
- van Teijlingen E., McCaffery P. The profession of midwife in The Netherlands. Midwifery. 1987 Dec;3(4):178–186. doi: 10.1016/s0266-6138(87)80038-4. [DOI] [PubMed] [Google Scholar]


