Abstract
BACKGROUND
A new pay-for-performance scheme for primary care physicians was introduced in England in 2004 as part of an initiative to link the quality of primary care with physician pay.
OBJECTIVE
To investigate the association between the quality of primary care and rates of hospital admissions for coronary heart disease.
DESIGN
Ecological cross-sectional study using data from the Quality and Outcomes Framework for family practice, hospital admissions, and census data.
PARTICIPANTS
All 303 primary care trusts in England, covering approximately 50 million people.
MEASUREMENTS
Rates of elective and unplanned hospital admissions for coronary heart disease and rates of coronary angioplasty and coronary artery bypass grafting were regressed against quality-of-care measures from the Quality and Outcomes Framework, area socioeconomic scores, and disease prevalence.
RESULTS
Correlations between prevalence, area socioeconomic scores, and admission rates were generally weak. The strongest relations were seen between area socioeconomic scores and elective and unplanned hospital admissions and revascularization procedures among the age group 45–74 years. Among those aged 75 years and over, the only positive association observed was between area socioeconomic scores and unplanned hospital admissions.
CONCLUSIONS
The lack of an association between quality scores and admission rates suggests that improving the quality of primary care may not reduce demands on the hospital sector and that other factors are much better predictors of hospitalization for coronary heart disease.
KEY WORDS: primary care, quality of care, hospital admissions, coronary heart disease
INTRODUCTION
Although many people with chronic diseases can be managed successfully in primary care, hospital admission rates for complications of chronic conditions such as coronary heart disease (CHD) continue to rise in many countries.1 Controlling this rise in admission rates for chronic diseases is of high priority for health care systems. Work from the United States suggests that hospital admission rates for ambulatory sensitive conditions, such as cardiovascular disorders, may be indicative of the quality of chronic disease management in primary care, with better care being associated with lower admission rates for these conditions.2,3
In recent years, several initiatives have aimed to improve the quality of chronic disease management in England’s National Health Service.4,5 A key driver of policy has been the belief that care provided in ambulatory settings is more accessible and acceptable to patients and that quality improvement in primary care services will reduce the demand for specialist hospital services. Among these recent initiatives was a new national contract6 for family practitioners in which a significant proportion of physician income would be determined by performance against a Quality and Outcomes Framework (QOF). The framework contains a number of evidence-based measures of chronic disease management7 and has been described as the world’s boldest attempt yet to improve the quality of primary care and to link quality with pay.8 Previous interventional studies in primary care have shown that achievement of the clinical interventions and targets in QOF can reduce morbidity and mortality from chronic diseases.
We wanted to determine whether there was any association between the quality of primary care as measured by the new framework and age–gender-adjusted hospital admission or revascularization procedure rates for CHD for all 303 primary care trusts in England, adjusting for disease prevalence and socioeconomic deprivation. The link between deprivation and admission rates is well established, but the link between the quality of care and admissions is not.
Primary care trusts are the statutory bodies responsible for purchasing specialist services and for delivering primary health care services to local areas in England. They are also the administrative authority for family practitioners and typically cover a population of 150,000–300,000 people. Because the numbers of hospitalizations at family practice level were too small to give robust results, analyses were performed at primary care trust level.
METHODS
Hospital Episode Statistics Data
The Hospital Episode Statistics database contains records of all inpatient and day case care provided by National Health Service hospitals in England. The data are recorded as finished consultant episodes, which are defined as the period during which an admitted patient is under the care of a particular consultant within a hospital provider. These were linked into admissions, with transfers to another hospital trust also linked so that they were not counted as separate admissions.
Diagnoses were coded using the International Classification of Disease (ICD) version 10, and procedures were coded using the Office for Population Censuses and Surveys version 4.2 classification (OPCS4). All admissions were selected where the primary diagnosis was CHD (ICD I20-125), divided into unplanned and elective. We used hospital admissions data for inpatients aged 45 years or over for the financial year April 2004 to March 2005 [adding the area socioeconomic status score data (as described below) via the patient’s postcode]. Admissions for revascularization procedures were defined as those in which OPCS4 codes K49–K50 (coronary angioplasty) or K40–K46 (coronary artery bypass graft) appeared in any procedure field.
Quality and Outcomes Framework Data
We obtained QOF data from the Department of Health’s Health and Social Care Information Centre web site for all 303 primary care trusts in England for the financial year April 2004 to March 2005.9 The framework was introduced in April 2004 and then contained 146 performance indicators. There were 12 CHD indicators, which accounted for 101 of the total 1,050 points available to each practice (Appendix). For each practice, data were downloaded on the total number of patients registered and the total QOF points that were achieved by domain and by individual indicator. We also analyzed separately points for the 2 CHD indicators most closely linked with health outcome: “CHD6” (percentage of CHD patients whose last blood pressure reading was 150/90 or less) and “CHD8” [percentage of CHD patients whose last cholesterol level was 5 mmol/l (193 mg/dl) or less]. Practice figures were summed to primary care trust level.
Prevalence Data
We obtained the number of CHD patients recorded on the family practice register on March 2005 from the same Department of Health web site to calculate crude disease prevalences of CHD for each practice and primary care trust. No breakdown by age or gender was available.
Population Data
We obtained mid-2003 population estimates by 5-year age band and gender of residents by primary care trust in England from the Office for National Statistics.
Measure of Area Socioeconomic Status
We obtained the Index of Multiple Deprivation 2004 data at super-output area level (these areas cover an average of about 1,500 residents) for England from the Department of Transport, Local Government and the Regions.10 The Index of Multiple Deprivation 2004 includes 37 indicators under 7 domains: income deprivation; employment deprivation; health deprivation and disability; education, skills, and training deprivation; living environment deprivation; barriers to housing and services; and crime. Each area is assigned a score, with high scores implying high levels of deprivation. Index of Multiple Deprivation data were available for 8,457 practices (total practices = 8,576) by linking the practice postcode to a super-output area. The score for each primary care trust was taken to be the average of its practice-level scores.
Statistical Analysis
At primary care trust level, the QOF scores are proportional to the number of practices and the number of registered patients. For each primary care trust, we transformed the score using the following formula:
 |
We calculated directly standardized rates that were expressed as admissions per 100,000 population using the total England population as the standard, adjusting for age and gender. We plotted prevalence and area socioeconomic status scores against the directly standardized rates for elective and unplanned CHD admissions and for coronary angioplasty and coronary artery bypass grafting. When a negative relation between prevalence and revascularizations was observed, we plotted the raw unplanned admission rates against the raw revascularization rates by 5-year age band. The relation between area-level socioeconomic status scores has been shown to vary with age, with less influence among the elderly.11 We therefore analyzed data by 2 age groups: 45–74 years and 75 years and over. We calculated standardized admission ratios using the indirect method, as the direct method can be sensitive to small numbers in the age–gender strata. We excluded patients under 45 years of age because CHD is rare in this group.12
There were 8,576 family practices in England with QOF data. Three practice codes were obsolete. Prevalence estimates were available for 8,486 practices. Of these practices, socioeconomic scores were available for 8,457; the practice postcode did not map to a super-output area for the others. A further 15 were excluded because of zero QOF scores for CHD, indicating missing data. There were, however, some low non-zero scores (the minimum total score was 6) but there was no obvious cut-off level in the distribution of scores that might suggest missing data for some indicators, and we therefore analyzed all practices with total non-zero scores. This left 8,442 practices for aggregation.
We used regression (linear for directly standardized rates and log-linear for standardized admission ratios) for elective and unplanned CHD admissions, and for each type of revascularization procedure against mean deprivation score, the prevalence of CHD and QOFPPP. All 3 predictors were entered at once, after first plotting each one against the outcome and calculating Pearson correlation coefficients.
A second analysis split the admissions into “first” admissions for CHD and “subsequent” admissions for CHD. In our data set, there is no field indicating whether the current admission is the patient’s first or otherwise for any condition. As a proxy, a CHD admission for each patient was defined as being their “first” if they had not had 1 in the previous 3 years; other CHD admissions in 2004/2005 were therefore defined as “subsequent.” As the quality indicators relate to secondary prevention measures, i.e., improving the profile of risk factors such as blood pressure in patients who already have CHD, one might argue that only a relation between quality scores and subsequent admissions might be seen. The regressions were therefore repeated for each age group using directly standardized rates of these “subsequent” admissions for electives and unplanned admissions separately.
We focus throughout on primary care trust level results primarily because of the small numbers of admissions at family practice level. To check whether our ecological analysis missed any relation between framework points and admissions, we also calculated standardized admission ratios for each practice (the direct method would yield rates that are too unstable). These were entered in a log-linear model as for the primary care trusts, with framework scores per practice divided by the total list size and multiplied by 1,000. SPSS was used for all analyses.
RESULTS
The characteristics of the 303 English primary care trusts varied widely (Table 1). Performance in the QOF was generally good, with an overall median score per primary care trust of 973 (maximum possible score 1,050) and a score of 100 for the CHD domain (maximum possible score 101 points). Because of considerable variations in the list size, QOFPPP varied much more between primary care trusts.
Table 1.
Baseline Characteristics of Primary Care Trusts in England
| Mean (SD) | Min | Max | Median | IQR | |
|---|---|---|---|---|---|
| Primary care trust characteristics (N = 303) | |||||
| Resident population (mid-2003 estimate) | 164,561 | 64,863 | 369,731 | 155,606 | 115,427–206,503 |
| Percent people aged 45–74 years | 32.8 (4.2) | 19.1 | 42.1 | 33.4 | 30.8–35.6 |
| Percent people aged 75+ | 7.8 (1.8) | 3.7 | 15.4 | 7.5 | 6.7–8.5 |
| IMD | 23.8 (12.0) | 4.6 | 62.9 | 21.6 | 14.5–32.0 |
| Percent practices in most deprived IMD quintile | 24.6 (26.6) | 0.0 | 97.1 | 15.4 | 0.0–44.1 |
| Number of general practices | 27.9 (14.5) | 8 | 81 | 24 | 17–34 |
| Practice list size | 173,773 | 70,003 | 389,319 | 158,779 | 118,134–215,920 |
| QOF points per practice (8,442 practices) | |||||
| Total coronary heart disease points | 96.8 (8.3) | 6.0 | 101.0 | 100.4 | 96.4–101.0 |
| Points for blood pressure ≤150/90 | 18.8 (1.2) | 0 | 19 | 19 | 19–19 |
| Points for cholesterol ≤5 mmol/l | 15.3 (2.4) | 0 | 16 | 16 | 16–16 |
| Total primary care trust level coronary heart disease QOF points divided by number of practices | 97.4 (2.7) | 86.7 | 101.0 | 98.3 | 95.7–99.5 |
SD = standard deviation, IQR = interquartile range, IMD = index of multiple deprivation, QOF = Quality and Outcomes Framework
Table 2 summarizes the directly age- and gender-standardized rates for CHD admissions and revascularization procedures. There was wide variation between primary care trusts: prevalence varied 4-fold, unplanned directly standardized rates more than 6-fold for ages 45–74 years and more than 5-fold for ages 75 years and over, and elective directly standardized rates more than 6-fold for ages 45–74 years and more than 10-fold for ages 75 years and over.
Table 2.
Summary of Prevalence and Number of Hospital Admissions for Coronary Heart Disease and Coronary Angioplasty and Coronary Artery Bypass Grafting for 303 Primary Care Trusts (N = 8,442 General Practices), by Age
| Mean (SD) | Min | Max | Median | IQR | |
|---|---|---|---|---|---|
| CHD register count | 6,231.4 (2,481) | 2,091 | 16,424 | 5,810 | 4,438–7,606 |
| Prevalence of CHD | 3.7% (0.1%) | 1.4% | 5.9% | 3.8% | 3.1%–4.3% |
| Elective CHD admissions | |||||
| 45–74 years | 135.9 (62.6) | 20 | 414 | 125 | 86–169 |
| 75+ years | 28.7 (16.3) | 4 | 106 | 27 | 16–36 |
| DSR 45–74 years | 256.7 (77.8) | 83.9 | 535.6 | 249.8 | 200.7–299.8 |
| DSR 75+ years | 230.4 (98.1) | 49.6 | 527.2 | 225.8 | 157.7–293.8 |
| Unplanned CHD admissions | |||||
| 45–74 years | 301.9 (133.2) | 77 | 853 | 281 | 199–372 |
| 75+ years | 215.6 (94.3) | 52 | 628 | 195 | 143–267 |
| DSR 45–74 years | 576.3 (191.6) | 256.7 | 1,734.3 | 540.6 | 445.6–651.7 |
| DSR 75+ years | 1,743.8 (421.1) | 859.4 | 4,525.5 | 1,663.2 | 1,453.7–2,018.4 |
| Coronary angioplasty | |||||
| 45–74 years | 118.6 (58.2) | 22 | 373 | 110 | 78–145 |
| 75+ years | 23.6 (16.2) | 0 | 97 | 20 | 12–32 |
| DSR 45–74 years | 225.4 (81.7) | 68.2 | 635.8 | 214.7 | 168.1–263.8 |
| DSR 75+ years | 190.8 (111.2) | 0 | 594.3 | 167.3 | 107.4–255.9 |
| Coronary artery bypass graft | |||||
| 45–74 years | 56.4 (26.1) | 15 | 139 | 51 | 36–73 |
| 75+ years | 13.5 (7.6) | 0 | 46 | 12 | 8–18 |
| DSR 45–74 years | 106.7 (33.1) | 39.7 | 212.6 | 102.9 | 82.5–124.4 |
| DSR 75+ years | 108.2 (47.3) | 0 | 266.9 | 102.6 | 76.6–137.6 |
SD = standard deviation, IQR = interquartile range, CHD = coronary heart disease, DSR = directly standardized rate per 100,000 population
We found that revascularization rates for people aged 75 years and over (and particularly those aged 80 years and over) were lower than their level of unplanned CHD admissions predicted. Figure 1 shows the large increase in unplanned directly standardized admission rates from the youngest to the oldest age group, which was not accompanied by a similar rise in directly standardized rates for either coronary angioplasty or coronary artery bypass graft. There was only a weak association between QOF score and deprivation.
Figure 1.

Mean rates of elective and unplanned hospital admissions for coronary heart disease and mean rates of hospital admissions for coronary angioplasty (PTCA) and coronary artery bypass grafting (CABG) by age
Table 3 shows the correlation coefficients between mean area socioeconomic status score, CHD prevalence, and hospital admissions by age group. Most correlations were weak, but they were often statistically significant. The strongest relations were seen between area socioeconomic status and elective and unplanned hospital admissions and revascularization procedures among those aged 45–74 years. Among people aged 75 years and over, the only positive association observed was between area socioeconomic status and unplanned hospital admissions.
Table 3.
Correlations between Mean Area Socioeconomic Status Score (Index of Multiple Deprivation), Coronary Heart Disease (CHD) Prevalence and Rates of Hospital Admission for CHD and for Coronary Angioplasty and Coronary Artery Bypass Grafting and Quality and Outcomes Framework Points per Practice per 1,000 Population, By Age
| Correlation coefficient (p value if not <0.001) | ||||||
|---|---|---|---|---|---|---|
| Prevalence | DSR unplanned CHD hospital admissions | DSR elective CHD hospital admissions | DSR CABG | DSR coronary angioplasty | QOF points per practice per 1,000 population | |
| Ages 45–74 | ||||||
| IMD | +0.27 | +0.74 | +0.45 | +0.45 | +0.35 | +0.10 (p = 0.10) |
| Prevalence | – | +0.15 (p = 0.012) | +0.09 (p = 0.14) | +0.22 | −0.25 | +0.33 |
| DSR unplanned CHD hospital admission | – | +0.45 | +0.45 | +0.37 | −0.12 (p = 0.045) | |
| DSR elective CHD hospital admission | – | +0.65 | +0.66 | −0.12 (p = 0.032) | ||
| DSR CABG | – | +0.35 | −0.02 (p = 0.74) | |||
| DSR coronary angioplasty | – | −0.22 | ||||
| QOF points per practice per 1,000 population | – | |||||
| Ages 75+ | ||||||
| IMD | +0.27 | +0.46 | −0.11 (p = 0.064) | −0.11 (p = 0.062) | −0.10 (p = 0.082) | +0.10 (p = 0.10) |
| Prevalence | – | +0.39 | −0.22 | −0.09 (p = 0.13) | −0.43 | +0.33 |
| DSR unplanned CHD hospital admission | – | −0.16 (p = 0.005) | +0.02 (p = 0.69) | −0.26 | 0.04 (p = 0.45) | |
| DSR elective CHD hospital admission | – | +0.66 | +0.69 | −0.04 (p = 0.47) | ||
| DSR CABG | – | +0.35 | −0.02 (p = 0.73) | |||
| DSR coronary angioplasty | – | −0.15 (p = 0.012) | ||||
DSR = directly standardized rate per 100,000 population, CHD = coronary heart disease, CABG = coronary artery bypass grafting, IMD = index of multiple deprivation, QOF = Quality and Outcomes Framework
For overall prevalence, the only notable association was a negative one for coronary angioplasty for people aged 75 and over. As expected, elective directly standardized rates correlated more closely with procedural directly standardized rates, as elective admissions for CHD will often be for a revascularization procedure. QOFPPP showed a moderate positive correlation with overall disease prevalence but weak correlations with the other variables, including deprivation. There was a marginally significant association between QOFPPP and unplanned CHD admission rates (correlation coefficient = −0.12, p = 0.045, Fig. 2).
Figure 2.
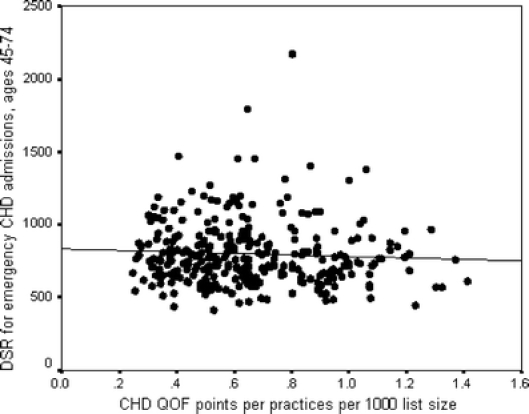
Relation between Quality and Outcomes Framework (QOF) points for coronary heart disease (CHD) per practice per 1,000 population and directly standardized rates (DSR) for unplanned admissions for ages 45–74
Regression Results
In the regression analyses, there was a significant positive relation between mean area socioeconomic status and the 4 directly standardized rates (p < 0.001 for each model and age group). Area socioeconomic status was the most important of the 3 predictors in explaining the variation in directly standardized rates.
For ages 45–74 years, QOFPPP showed nonsignificant relations with all 4 directly standardized rates and indirectly standardized admission ratios (p > 0.2). Results were the same for the blood pressure and cholesterol indicators. The association between overall prevalence and the directly standardized rates was not significant for unplanned (p = 0.47) or elective CHD (p = 0.99). A 1% increase in disease prevalence was associated with 4.3 more coronary artery bypass grafts per 100,000 population (95% CI 0.2 to 8.4, p = 0.04) and 31.3 fewer coronary angioplasties per 100,000 population (95% CI 21.5 to 41.2, p < 0.001).
For ages 75 years and over, QOFPPP showed nonsignificant relations with all 4 directly standardized rates and indirectly standardized admission ratios (p > 0.7). Again, results were the same for the blood pressure and cholesterol indicators. A 1% increase in CHD prevalence was associated with an extra 133.6 unplanned CHD admissions per 100,000 population (95% CI 84 to 183.2, p < 0.001) and 23.3 fewer elective CHD admissions per 100,000 population (95% CI 9.9 to 36.6, p = 0.001), 3.3 fewer coronary artery bypass grafts per 100,000 population (95% CI 9.8 fewer to 3.3 extra, p = 0.33), and 53.6 fewer coronary angioplasties (95% CI 39.8 to 67.4, p < 0.001).
Regression results for the “subsequent” admissions showed very similar results to the previous analyses that included all CHD admissions: QOFPPP showed nonsignificant relations with all the directly standardized rates examined (p > 0.7). Practice-level regression results showed very similar patterns to primary care trust level analyses for the relations between admissions and both deprivation and prevalence. Although quality and outcome framework scores per 1,000 list patients sometimes showed statistically significant associations with standardized admission ratios, the size of the associations was clinically unimportant. For example, the largest effect was for coronary artery bypass grafts in patients aged 75 and over, for whom an increase of 100 points per 1,000 list patients was associated with only 0.3 fewer procedures; an increase in 100 points would be very large, given that the mean framework score per 1,000 list patients is only 23.3 with an interquartile range of 11.5 to 30.1.
DISCUSSION
Summary of Main Findings
We found no significant association between the quality of CHD care, as measured by the QOF, and rates of elective or unplanned hospital admission for CHD by primary care trust in England. This suggests that high-quality primary care may not necessarily lead to lower rates of hospital admissions. Population factors such as prevalence and area socioeconomic status may be more important determinants of hospital admission rates than quality of care.
We also found that lower socioeconomic status was positively associated with hospital admission rates for CHD, particularly for those aged 45–74 years, and explains more of the variation observed amongst primary care trusts than either the overall prevalence for CHD or QOF scores for CHD.
Strengths and Limitations of the Study
A key strength of this study is the large size of the population covered (50 million). Moreover, the structure of primary care in England offers some unique opportunities for examining factors associated with the quality of care. Almost all the English population is registered with a family practitioner, who is responsible for providing primary care services and arranging referrals for specialist care (all of which are free at the point of delivery). This means that family practitioners have well-defined denominator populations, which in turn allows for more accurate calculations of disease prevalence and treatment rates.13
Among the limitations of the study are the assumptions inherent with QOF data. The first key assumption is that a high QOF score is indicative of good-quality primary care. There was relatively little variation between Primary Care Trusts in quality scores for CHD. This may be because the framework itself has been successful in reducing the previously documented variations in CHD management in primary care. Conversely, it may be because the total CHD score is relatively poor at discriminating good- from poor-quality care. We sought to address this potential limitation by conducting separate analyses for intermediate clinical outcome indicators (blood pressure and cholesterol) that have good predictive values for CHD and hospital admissions.14 The pattern of results for these intermediate outcome scores was the same as for the total framework scores.
Second, we measured associations between the quality of primary care and hospital admissions over the same 12-month period. The assumption here is that the quality scores relate not just to 2004 but also reflect historical variations in quality, and therefore, there may be enough lag time to see an association with admission rates. If, however, the family practitioner contract resulted in better care and reduced variations in quality, in addition to a number of previous improvement initiatives, then it might be too early to see changes in admission rates that are because of improved care owing to the new contract. We repeated the analysis using admissions for the following year, 2005/2006, and found the same pattern of results.
Third, only rates for subsequent rather than all admissions for CHD might be expected to correlate with scores for secondary prevention, although the finding that quality scores also showed nonsignificant relations with the revascularization rates suggests that we have not missed a possible association. Analysis of “subsequent” admissions showed very similar results to those obtained using all admissions, although our definition of “subsequent” was imperfect (data not shown).
Fourth, people with CHD who are not identified or coded by the practice are excluded from the data set. However, payments to family practices under the new contract are weighted by disease prevalence, thereby giving a financial incentive for full recording of patients with CHD. Patients can also be “exception coded,” and thus excluded from the denominator for some of the indicator scores, and initial analysis suggests that, although this is not extensive, it is a predictor of high levels of achievement.15 Other limitations include the lack of prevalence estimates broken down by either age or gender. It was also not possible to tell whether the admitted patients had high or low indicator scores because the scores were only available at aggregate level for family practices. Finally, the financial incentives associated with achieving high quality and outcomes score may encourage general practices to manipulate data, for example, by recording a patient’s blood pressure as being lower than it actually is. This “gaming” will be difficult to detect, despite annual inspection of practices and the severe penalties incurred for making fraudulent claims.
Comparisons with Previous Research
Because QOF data have only become available relatively recently, few studies are available against which to directly compare our findings. Our findings do, however, reinforce the associations seen in previous studies between deprivation and hospital admission rates, especially with unplanned admission rates.16,17
Implications for Future Research and Clinical Practice
Unplanned admissions for CHD will include some acute events that will occur regardless of the quality of primary care, but we might expect to avoid some unplanned admissions with primary prevention and early diagnosis and management in primary care. If the principal goal of the new family practitioner contract was to establish disease registers in primary care and to begin to control disease risk factors, then we may not see health improvement (and corresponding reduction in unplanned admissions) over this short space of time.
Nevertheless, the lack of an association between quality scores and admission rates is an important finding. It suggests that improving the quality of primary care by itself may not reduce admissions for potentially ambulatory care sensitive disorders such as coronary heart disorders. Furthermore, in England, hospital admission rates for disorders such as CHD may not reflect the accessibility, continuity, or quality of primary care services. This is in contrast to the conclusions of some previous U.S. studies.18,19
Conclusions
We found relatively weak associations between the quality of primary care services for CHD in primary care and hospital admission rates for this disorder in England, and even these became nonsignificant after adjusting for disease prevalence and area socioeconomic status. This suggests that higher-quality primary care services, which clearly have other benefits to patients, may not necessarily lead to lower hospital admission rates or lower spending on hospital care. This finding has important implications for health policy in the UK and elsewhere.
Conflict of Interest
The Dr Foster Unit (but not the rest of the department of primary care and social medicine) is funded by a grant from Dr Foster Ltd (an independent health service research organization).
We have Section 60 approval from the Security and Confidentiality Advisory Group to hold confidential data and analyze them for research purposes. We also have approval from St Mary’s Local Research Ethics Committee.
AB, SG and AM conceived the study. AB performed all analyses. All authors wrote the manuscript. AB is the guarantor for the study.
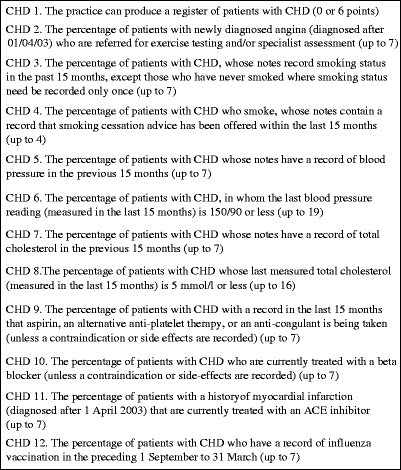
Appendix
Appendix Box 1. Quality and Outcomes Framework Indicators for CHD Management in 2004–2005 with Number of Points Available in Parentheses
References
- 1.Hensher M, Edwards N, Stokes R. International trends in the provision and utilisation of hospital care. Br Med J. 1999;319:845–8. [DOI] [PMC free article] [PubMed]
- 2.Zhan C, Miller MR, Wong H, Meyer GS. The effects of HMO penetration on preventable hospitalizations. Health Serv Res. 2004;39(2):345–61. [DOI] [PMC free article] [PubMed]
- 3.Basu J, Friedman B, Burstin H. Primary care, HMO enrollment, and hospitalization for ambulatory care sensitive conditions: a new approach. Med Care 2002;40(12):1260–9. [DOI] [PubMed]
- 4.Department of Health. Supporting people with long term conditions. London: Department of Health; 2005. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyandGuidance/DH_4100252 (accessed March 2007).
- 5.Wilson T, Buck D, Ham C. Rising to the challenge: will the NHS support people with long term conditions? Br Med J. 2005;330:657–61. [DOI] [PMC free article] [PubMed]
- 6.British Medical Association. The new general medical services contract. http://www.bma.org.uk/ap.nsf/content/investinggp (accessed May 2007)
- 7.Shekelle P. New contract for general practitioners. Br Med J. 2003;326:457–8. [DOI] [PMC free article] [PubMed]
- 8.Ashworth M, Armstrong D. The relationship between general practice characteristics and quality of care: a national survey of quality indicators used in the UK Quality and Outcomes Framework, 2004–5. BMC Fam Pract. 2006;7.1:68. [DOI] [PMC free article] [PubMed]
- 9.Information Centre for Health and Social Care. Quality and outcomes framework 2004/5. http://www.ic.nhs.uk/services/qof/data/gptables (accessed May 2007).
- 10.Office of the Deputy Prime Minister. Indices of deprivation 2004. http://www.communities.gov.uk/archived/publications/communities/indicesdeprivation (accessed March 2007).
- 11.Carstairs V. Deprivation indices: their interpretation and use in relation to health. J Epidemiol Community Health. 1995;49(Suppl 2):S3–8. [DOI] [PMC free article] [PubMed]
- 12.Ryan R, Majeed A. Prevalence of ischaemic heart disease and its management with statins and aspirin in general practice in England and Wales, 1994–1998. Health Stat Q. 2001;12:34–9.
- 13.Gnani S, Majeed A. A user’s guide to data collected in primary care in England. Eastern Region Public Health Observatory, Cambridge, 2006. http://www.erpho.org.uk/viewResource.aspx?id=12899 (accessed February 2007).
- 14.Department of Health. Quality and outcomes framework. Guidance—updated August 2004. http://www.dh.gov.uk/assetRoot/04/08/86/93/04088693.pdf (accessed February 2007).
- 15.Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis E, Hiroeh U et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355(4):375–84. [DOI] [PubMed]
- 16.Duffy R, Neville R, Staines H. Variance in practice emergency medical admission rates: can it be explained? Br J Gen Pract. 2002;52(474):14–7. [PMC free article] [PubMed]
- 17.Majeed A, Bardsley M, Morgan D, O’Sullivan C, Bindman AB. Cross sectional study of primary care groups in London: association of measures of socioeconomic and health status with hospital admission rates. Br Med J. 2000;321(7268):1057–60. [DOI] [PMC free article] [PubMed]
- 18.Gill JM, Mainous AG III. The role of provider continuity in preventing hospitalizations. Arch Fam Med 1998;7:352–7. [DOI] [PubMed]
- 19.Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, Billings J, Stewart A. Preventable hospitalizations and access to health care. JAMA 1995;274:305–11. [DOI] [PubMed]


