Abstract
Background
Discrimination toward gay and lesbian patients by health care providers has been documented. No study has determined if patient behavior would change when seeing a gay/lesbian provider.
Objective
The objective of the study was to examine whether a provider’s sexual orientation would affect the choice of provider, practice, or preference for a chaperone during genital exams.
Design
The design of the study was an anonymous, cross-sectional survey.
Participants
The participants were a random national sample of persons 18 years or older residing in the USA able to read English.
Measurements
The measurements were self-reported perceptions and chaperone preference based on provider gender and sexual orientation.
Results
The response rate was 32% (n = 502). Many respondents indicated they would change providers upon finding out their provider was gay/lesbian (30.4%) or change practices if gay/lesbian providers were employed there (35.4%). Female respondents preferred chaperones most with heterosexual male providers (adjusted odds ratio [OR] 1.50, 95% confidence interval [CI] = 1.15 to 1.95) followed by homosexual male (OR 1.17, 95% CI = 0.93 to 1.47), lesbian (reference), and heterosexual female providers (OR 0.63, 95% CI = 0.51 to 0.77). Male respondents showed an increased preference for chaperones with gay/lesbian providers of either gender (OR 1.52, 95%, CI = 1.22 to 1.90, for gay male provider, [reference] for lesbian provider) than with either heterosexual male (OR 0.36, 95% CI = 0.26 to 0.52) or heterosexual female providers (OR 0.39, 95% CI = 0.29 to 0.54).
Conclusions
Patients may change providers, practices, or desire for chaperone based on a provider’s gender and sexual orientation. Although the low response rate may limit generalizability, these findings have the potential to impact aspects of practice structure including chaperone use and provider–patient relationships.
KEY WORDS: Patient–provider relationship, gay/lesbian, disclosure, practice of medicine
BACKGROUND
Discrimination toward gay and lesbian (gay/lesbian) patients by health care providers has been well documented. In 1 study, 27% of gay/lesbian patients reported interactions with a prejudiced physician, 2% reported an openly hostile physician, and 21% felt their provider was not supportive of their gay/lesbian orientation.1 Other studies have reported that 20–30% of physicians surveyed are homophobic.2,3 However, very little work has been done to examine whether the reverse holds true—whether patients would discriminate against gay/lesbian providers.
Only 1 published study to date has documented discrimination against gay/lesbian providers.4 The 2 most common reasons cited were fear of incompetence and worries about feeling “uncomfortable” having a gay/lesbian provider.
No study yet has determined if patient behavior would change when seeing an “out” gay/lesbian provider (that is, a gay/lesbian provider who is has publicly revealed his or her sexual orientation) or how patient characteristics affect these perspectives. Using a nationally representative sample, we examined whether respondents felt their provider’s gender or sexual orientation was important and whether a provider’s sexual orientation would affect their choice of provider, practice, or preference for a chaperone during genital exams.
METHODS
Survey Development
A survey was developed and pilot tested with a nationwide random sample of 100 individuals 18 years of age or older. Based on pilot results, the survey instrument was modified. Survey responses were based on a 5-point Likert scale (strongly disagree, somewhat disagree, neither agree nor disagree, somewhat agree, strongly agree).
We designed the survey to assess patient preferences and possible behavioral changes if the patient was to become aware that his/her health care provider was gay/lesbian. Specifically, we focused on clinically important outcomes such as changing providers, changing practices, or discomfort in discussing important personal issues with their provider. In addition, the survey assessed whether knowledge of the provider’s sexual orientation would change patients’ preferences regarding chaperones during genital (breast, pap/pelvic, rectal/prostate) exams and whether patients believe that providers should reveal their sexual orientation to their patients.
The study was approved by the Colorado Multiple Institutional Review Board.
Survey Administration
This was a cross-sectional, mailed, self-administered survey. We distributed our survey via mail to 1,600 individuals randomly selected from the List Company, a national marketing database. Study subjects had to be able to read English and have a mailing address. All participants were at least 18 years of age.
The Dillman “Tailored Design Method” was used to maximize the response rate.5 This method includes a total of up to 5 contacts to each selected recipient of the survey. The first contact was an “advance letter” that alerted the recipient that the survey will be arriving in the next few days and the importance of their participation. The second contact was a cover letter with the survey, including a stamped envelope for returning the survey. A few days later, the third contact was sent—a postcard reminding the recipient to return the survey. The fourth and fifth contacts were remailings of the survey packet, with a revised cover letter, a new copy of the questionnaire, and a return envelope.
Statistical Analysis
Data analysis was performed using SPSS version 14 (Chicago, IL) and SAS version 9.13 (Cary, NC). Dependent variables were dichotomized based on clinical relevance (strongly agree and somewhat agree versus neutral, strongly disagree, and somewhat disagree). Dichotomization was based on the premise that those who strongly and somewhat agree are more likely to make a true change in behavior compared to those that are neutral or disagree. A Chi-squared test was used to explore the association between respondents’ feelings about provider sexual orientation and behavior change. Also using Chi-square tests, a preliminary analysis was conducted with the dependent variables and demographic (predictor) variables to identify potential predictors to enter into a regression model. Independent variables associated with dependent variables at a level of P < .20 were entered into a forward logistic regression analysis with the dependent variable.
To capture whether respondents would change their preferences for a chaperone during genital exams based on the 4 possible combinations of provider gender and sexual orientation, a repeated-measures analysis was conducted using the generalized estimating equations (GEE) method. Respondent demographic variables were entered into a logistic regression model to identify significant predictor variables of chaperone change. Additionally, to test our hypothesis that respondent preference for chaperone would change based on provider gender and sexual orientation, we used the GEE method with interaction terms. The interaction among respondent gender, provider gender, and provider sexual orientation for chaperone preference was investigated by first stratifying by respondent gender and then estimating a two-way interaction between provider gender and sexual orientation in each subgroup.
RESULTS
The overall response rate was 32%. Of 1,600 surveys mailed, 32 were unusable (deceased or invalid) addresses, and 502 completed surveys were received. Table 1 shows characteristics of the respondents. Data about nonrespondents were not available.
Table 1.
Respondent Characteristics
| Demographics | Value* |
|---|---|
| Mean age (SD), year | 55.9 (15.6) |
| Gender | |
| Male | 292 (59.3) |
| Sexual orientation | |
| Heterosexual | 473 (96.3) |
| Race | |
| White/Caucasian | 427 (87.7) |
| Black | 31 (6.4) |
| Asian/Pacific Islander | 13 (2.7) |
| Native American | 3 (0.6) |
| Other | 13 (2.7) |
| Ethnicity | |
| Non-Hispanic | 471 (95.5) |
| Education | |
| High school or less | 111 (22.6) |
| Some college | 166 (33.7) |
| College graduate | 112 (22.8) |
| Postgraduate | 103 (20.9) |
| Religion | |
| Catholic/Christian | 137 (28.2) |
| Christian | 262 (53.9) |
| Jewish | 9 (1.9) |
| Muslim | 0 (0.0) |
| Atheist/Agnostic | 32 (6.6) |
| Other | 46 (9.5) |
| Religious service attendance (past year) | |
| None | 103 (20.9) |
| Once or a few times | 119 (24.2) |
| Once a month | 66 (13.4) |
| Once a week | 150 (30.5) |
| Several times a week | 54 (11.0) |
| Region of country | |
| Northeast | 101 (20.8) |
| Mid-Atlantic | 27 (5.6) |
| South | 119 (24.5) |
| Midwest | 131 (27.0) |
| Southwest | 39 (8.0) |
| West | 69 (14.2) |
| Type of town/city | |
| Urban | 115 (23.3) |
| Suburban | 239 (48.5) |
| Rural | 139 (28.2) |
| Political belief system | |
| Extremely/Very liberal | 36 (7.7) |
| Liberal | 182 (38.7) |
| Conservative | 195 (41.5) |
| Extremely/Very conservative | 57 (12.1) |
| Affiliated with military (active, retired, reserve, spouse/partner) | 57 (11.7) |
| Current provider sexual orientation | |
| Openly gay/lesbian | 2 (0.4) |
| Assume gay/lesbian | 0 (0.0) |
| Assume heterosexual | 232 (46.9) |
| Openly heterosexual | 101 (20.4) |
| Do not know | 137 (27.7) |
| Do not have provider | 23 (4.6) |
| Ever gay/lesbian PCP | |
| Yes | 20 (4.0) |
| No | 151 (30.3) |
| Do not know | 328 (65.7) |
SD Standard deviation
*All values are N (%) unless otherwise noted. Numbers in each category may not add up to 502 because of missing data points.
Frequency data for respondents who reported “somewhat agree or strongly agree” to the survey questions are listed in Table 2. Thirty percent of respondents reported that they would change providers if they found out their health care provider was gay/lesbian (39.2% strongly disagree, 11.6% somewhat disagree, 18.8% neutral, 11.8% somewhat agree, 18.6% strongly agree), and 35.4% would change practices if their practice employed an openly gay/lesbian health care provider (34.0% strongly disagree, 10.1% somewhat disagree, 20.5% neutral, 15.5% somewhat agree, 19.9% strongly agree).
Table 2.
Percentage of Respondents who Reported “Somewhat/strongly Agree” to the Following Survey Items
| Item | N (%) |
|---|---|
| Important my health care provider is same gender as me | 111 (22.1) |
| Important my health care provider is same sexual orientation as me | 172 (34.5) |
| My health care provider’s gender is important to me | 125 (25.2) |
| My health care provider’s sexual orientation is important to me | 166 (34.1) |
| Providers should tell patients about their sexual orientation | 76 (15.4) |
| Patients should be informed if their provider is gay/lesbian | 124 (25.1) |
| The sexual orientation of my health care provider is private | 342 (69.7) |
| More comfortable discussing issues related to personal relationships with provider of same sexual orientation | 214 (43.0) |
| More comfortable discussing issues related to sexual functioning with provider of same sexual orientation | 251 (50.5) |
| If I found out my health care provider were gay/lesbian, I would change providers | 149 (30.4) |
| If a clinic employed openly gay/lesbian health care providers, I would change to a different practice | 176 (35.4) |
| Prefer chaperone for all genital exams | 184 (37.3) |
| Prefer chaperone if provider heterosexual male | 191 (38.7) |
| Prefer chaperone if provider gay male | 251 (51.2) |
| Prefer chaperone if provider heterosexual female | 158 (32.2) |
| Prefer chaperone if provider lesbian | 220 (45.0) |
Using Chi-squared tests, individuals who reported that the sexual orientation of their provider was important were more likely to anticipate changing either providers (P < .001) or practices (P < .001). There was also an association between those indicating they should be informed of their provider’s sexual orientation and those who would change both provider and practice (P < .001).
Potential predictors of whether respondents would change providers if they found out their health care provider were gay/lesbian include male gender (P < .001), lower education (P = .014), religion (P = .071), more frequent attendance of religious services (P = .002), and military affiliation (P = .016). These same variables, with the addition of white race (P = 0.026), emerged as potential predictors of those intending to change practices. Age, ethnicity, region of country, type of town, political belief, previous gay/lesbian provider, or current provider sexual orientation were not potential predictors of change in either provider or practice (data not shown). In the logistic regression model, gender, education, and attendance of religious services were significant predictors of respondents wanting to change providers and practices (Table 3). Men and respondents with less than postgraduate education were more likely to indicate that they would change providers and practices. Respondents who attended religious services once per month or less were less likely to change providers or practices.
Table 3.
Summary of Logistic Regression Predicting Respondents who would Change Provider and Practices*
| Would change providers (n = 477) | Would change practices (n = 484) | |
|---|---|---|
| Variable | OR (95% CI) | OR (95% CI) |
| Gender | ||
| Male | 2.97 (1.88 to 4.69) | 2.60 (1.69 to 4.01) |
| Female | Reference | Reference |
| Education | ||
| High school grad or less | 3.09 (1.63 to 5.86) | 5.16 (2.72 to 9.78) |
| Some college | 1.31 (0.72 to 2.40) | 1.65 (0.90 to 3.01) |
| College grad | 1.68 (0.89 to 3.17) | 2.96 (1.58 to 5.55) |
| Postgraduate education | Reference | Reference |
| Religious service attendance (past year) | ||
| None | 0.33 (0.16 to 0.71) | 0.21 (0.10 to 0.45) |
| Once or a few times | 0.38 (0.19 to 0.79) | 0.40 (0.20 to 0.80) |
| Once a month | 0.27 (0.12 to 0.63) | 0.31 (0.14 to 0.70) |
| Once a week | 0.68 (0.35 to 1.35) | 0.60 (0.31 to 1.18) |
| Several times a week | Reference | Reference |
OR Odds ratio, CI confidence interval
*Variables retained in the model are displayed.
Significant predictors of chaperone preference included provider orientation, respondent and provider gender, respondent education level, religion, geographic region, and previous history of gay/lesbian provider in the main-effects GEE model (Table 4).
Table 4.
GEE Results: Variables Predicting Respondents Wanting a Chaperone during Genital Exams
| Variable | Adjusted OR (95% CI) |
|---|---|
| Provider orientation | |
| Heterosexual | 0.53 (0.45 to 0.62) |
| Gay/Lesbian | Reference |
| Respondent gender | |
| Male | 0.24 (0.17 to 0.35) |
| Female | Reference |
| Provider gender | |
| Male | 1.45 (1.27 to 1.66) |
| Female | Reference |
| Education | |
| High school grad or less | 3.57 (1.99 to 6.41) |
| Some college | 2.35 (1.40 to 3.96) |
| College grad | 1.05 (0.60 to 1.83) |
| Post graduate education | Reference |
| Religion | |
| Christian/Catholic | 2.51 (1.50 to 4.23) |
| Other | Reference |
| Region of country | |
| Northeast | 1.39 (0.83 to 2.35) |
| Mid-Atlantic | 2.47 (1.14 to 5.37) |
| South | 1.98 (1.24 to 3.18) |
| Southwest | 1.90 (0.93 to 3.87) |
| West | 1.47 (0.86 to 2.52) |
| Midwest | Reference |
| Ever had a gay/lesbian provider | |
| Yes | 1.15 (0.52 to 2.57) |
| No | 2.11 (1.46 to 3.04) |
| Do not know | Reference |
Based on GEE modeling with interactions, female and male respondents showed different patterns of chaperone preference based on provider gender and sexual orientation (Fig. 1a and b). The interaction of provider gender and sexual orientation with each respondent gender was statistically significant (female P < .0001, male P = .01). Female respondents expressed a preference for chaperones most frequently with heterosexual male providers (odds ratio [OR] 1.50, 95% confidence interval [CI] = 1.15 to 1.95) followed by homosexual male providers (OR 1.17, 95% CI = 0.93 to 1.47), lesbian providers (reference category), and heterosexual female providers (OR 0.63, 95% CI = 0.51 to 0.77; Fig. 1a). Male respondents showed a greater preference for chaperones with gay/lesbian providers of either gender (OR 1.52, 95% CI = 1.22 to 1.90 for gay male provider, 1.0 [reference category] for lesbian provider) than with either heterosexual male providers (OR 0.36, 95% CI = 0.26 to 0.52) or heterosexual female providers (OR 0.39, 95% CI = 0.29 to 0.54; Fig. 1b).
Figure 1.
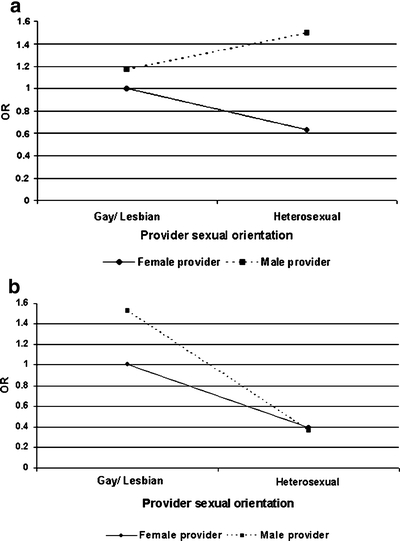
a Effect of hypothetical provider sexual orientation by gender on chaperone preference for female respondents. b Effect of hypothetical provider sexual orientation by gender on chaperone preference for male respondents.
DISCUSSION
This is the first national study to document patient behaviors with regard to their provider’s sexual orientation. Whereas close to 70% of respondents felt that a provider’s sexual orientation was private and not to be shared, one third indicated they would change providers if they found out their provider was gay/lesbian, and one third would change practices if they found out an openly gay/lesbian provider was employed by the practice. Only male gender, less education, and more attendance at religious services emerged as predictors of respondents’ intended behavior.
Our study did not examine why patients would leave a gay/lesbian provider, but we propose that sexual orientation concordance is a potential explanation. It has previously been well documented that gender and race concordance increases satisfaction in physician and patient pairs.6,7 Some proposed that race concordance, in particular, increases the “participatory style” of the physician–patient interaction.7 Adapting this theory, a perceived need for sexual orientation concordance may help explain why respondents would intend to change physicians. This theory may be supported by the data from Table 2 where half of the respondents stated they would feel more comfortable discussing sexual functioning and relationship issues with providers with the same sexual orientation. Among gay/lesbian patients, sexual orientation concordance may be preferable, with two thirds who had previously experienced prejudice in the health care environment desiring a homosexual provider.1
Whereas sexual orientation concordance may explain why respondents would change providers, it is less applicable when discerning why a respondent would leave a practice that employed gay/lesbian providers (more so than changing providers). This apparent paradox may be explained by the more personal relationship with one’s provider as opposed to the practice.
Respondents were more likely to prefer a chaperone for genital exams if the provider were gay/lesbian, with the notable exception that female respondents preferred chaperones more for heterosexual versus homosexual male providers. The reasons for gender and sexual orientation interaction of chaperone preference are unclear. Women more often preferred chaperones with male providers than with female providers, regardless of the provider sexual orientation. Previous surveys of female patients have shown a strong preference for chaperones during sensitive examinations by a male physician.8,9 One possible explanation for their preferences could be fears of sexual advances by the provider. However, the study by Druzin et al.4 only found 5% of respondents reporting “fear of being thought of sexually” and 10% reporting “fear of being sexually harassed” as reasons for discriminating against gay/lesbian providers. In addition, this theory does not explain the differences in chaperone preference by male respondents. Their chaperone preferences may be partially explained by suggestions in the literature that men have more discriminatory attitudes toward homosexuals than women.10 Although there have been suggestions to universally offer chaperones for intimate examinations, no national standard exists, and each state medical board sets its own standards.11 Accordingly, several studies have shown that chaperone use is extremely variable and ranges from 16 to 53%.12–14 Therefore, factors that increase patients’ preference for chaperones may have a significant impact on policy as well as clinical practice.
Only 1 other study has looked at patient discrimination against gay/lesbian providers.4 It found that 11.8% of respondents would refuse to see a gay/lesbian physician—the most common reasons being concerns about provider competence and feeling “uncomfortable.” In 1994, a national survey of gay/lesbian physicians found that 67% felt “many physicians would jeopardize their practices if their colleagues learned they are lesbian, gay, or bisexual,” and 73% felt “many physicians would jeopardize their practices if their patients learned they are lesbian, gay, or bisexual.”15 Our study appears to support this fear that knowledge of a provider’s sexual orientation could jeopardize the practice.
Whereas this study presents novel findings, some limitations exist. The 32% response rate might lead to response bias as there are more male respondents and more educated respondents than would be expected in the general population based on the 2000 Census Bureau data.16 In addition, responses may be subject to social acceptability bias. However, there is the possibility that responses to survey questions are not constrained by social acceptability in the same way that real-life situations may be, thus making our data more reflective of true desired behaviors by respondents.
Although our 3.7% response rate of self-identified homosexual or bisexual individuals may seem low, it matches estimates based on recent population estimates.17 Respondents may have had a “stronger” opinion than nonrespondents leading to more polarized responses. However, this response rate is higher than a prior study, with a similar design method on an equally sensitive topic, which was only able to achieve a 22% response rate.18 Although our response rate suggests our sample’s results may not be generalizable to the entire US population, our sample does provide important preliminary findings on a topic that has been understudied. In addition, respondent reactions to a hypothetical provider may differ from their reaction to their established provider because attitudes do not always reflect actual behavior.19
There are approximately 116,000 to 347,000 gay/lesbian providers in the USA. Therefore, the preferences we have identified in this study may impact numerous patients, providers, clinical practices, and the intersections between these groups. Presumably, most patients are not explicitly asking providers about their sexual orientation, but many ask providers about their personal lives—family, children, activities—such that they indirectly ascertain provider sexual orientation. This can place gay/lesbian providers in an awkward position. While they might like to remain honest with their patients, doing so could jeopardize both the patient–physician relationship and the practice. Gay/lesbian providers may have to choose between honesty, dishonesty, or “vaguery” (not being dishonest but not full disclosure).
Our findings accentuate the dilemma of providing outreach to medically underserved populations, such as gay/lesbian patients, while maintaining a viable clinical practice. It has been previously suggested that health care plans should provide patients with the opportunity to find gay-/lesbian- friendly physicians.20 This could be done by creating directories of culturally competent providers who are aware and trained in gay/lesbian issues so gay/lesbian patients would have a way of identifying supportive providers. Because a portion of these providers will be gay/lesbian themselves, this poses a potential dilemma as they may face discrimination from both colleagues and patients as reported above. There have also been calls for providers to be “out” in the hopes of increasing access to health care for gay/lesbian patients and to act as role models for gay/lesbian medical students and residents.21,22 Our data show that providers may jeopardize their practices if they choose to become advocates. Gay/lesbian providers who wish to be “out” for the reasons listed above need to understand the risks involved when acting as role models.
An additional clinical implication of this study is the desire for chaperones in 37% of the respondents. This could have enormous administrative implications in terms of time, cost, and staffing. Clearly, no uniform protocol can take into account every potential patient–physician interaction and preference, but this may be an important determinant of patient comfort and satisfaction.
This dilemma of disclosure leads to many more questions around the patient–provider relationship, the many roles providers play in their careers, and the clinical practice of medicine. More research is needed to explore why some respondents would consider changing their provider and practice based on provider sexual orientation and how these issues can be addressed at the individual, clinic, and system levels. Further understanding of the gender- and sexual orientation–specific chaperone preferences should be explored. In addition, new methods of improving access to competent care for gay/lesbian patients, addressing patient chaperone preferences, and matching sexual orientation concordance for all who desire it need to be researched and developed.
Acknowledgments
Financial support for this study was provided by a University of Colorado at Denver and Health Sciences Center, Division of General Internal Medicine Small Grant awarded to Rita Lee, M.D. The authors would like to acknowledge the statistical assistance of Sung-joon Min, Ph.D., Assistant Professor, Division of Health Care Policy and Research and Colorado Health Outcomes Program, University of Colorado at Denver and Health Sciences Center (UCDHSC), and the guidance of Jean S. Kutner, MD, MSPH, Associate Professor and Division Head, General Internal Medicine, UCDHSC, and John F. Steiner, MD, MPH, Professor and Director, Colorado Health Outcomes Program, UCDHSC. Thanks to Sung-Joon Min, Jean Kutner, and John Steiner.
Conflict of Interest None disclosed
Footnotes
Presented in Poster format at Society of General Internal Medicine meeting in Toronto, Canada, on April 25, 2007. Presented in Workshop format at Gay Lesbian Medical Association meeting in San Juan, Puerto Rico on September 28, 2007.
References
- 1.Dardick L, Grady KE. Openness between gay persons and health professionals. Ann Int Med. 1980;931115–9. [DOI] [PubMed]
- 2.Mathews WC, Booth MW, Turner JD, Kessler L. Physicians’ attitudes toward homosexuality—survey of a California county medical society. West J Med. 1986;144:106–10. [PMC free article] [PubMed]
- 3.Prichard JG, Dial LK, Holloway RL, Mosley M, Bale RM, Kaplowitz HJ. Attitudes of family medicine residents toward homosexuality. J Fam Pract. 1988;27:637–9. [PubMed]
- 4.Druzin P, Schrier I, Yacowar M, Rossignol M. Discrimination against gay, lesbian, and bisexual family physicians by patients. CMAJ. 1998;158:593–7. [PMC free article] [PubMed]
- 5.Dillman DA. Mail and Internet Surveys: The Tailored Design Method, 2nd Ed. New York: Wiley; 2000.
- 6.Chen FM, Fryer GE, Phillips RL, Wilson E, Pathman DE. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005;3(2):138–43. [DOI] [PMC free article] [PubMed]
- 7.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe N, Nelson C, Ford DE. Race, gender, and partnership in the patient–physician relationship. JAMA. 1999;282(6):583–9. [DOI] [PubMed]
- 8.Patton DD, Bodtke S, Horner RD. Patient perceptions of the need for chaperones during pelvic exams. Fam Med. 1990;22(3):215–8. [PubMed]
- 9.Penn MA, Bourguet CC. Patients’ attitudes regarding chaperones during physical examinations. J Fam Pract. 1992;35(6):639–43. [PubMed]
- 10.LaMar L, Kite M. Sex differences in attitudes toward gay men and lesbians: a multidimensional perspective. J Sex Research. 1998;35(2):189–96.
- 11.Stagno SJ, Forster H, Belinson J. Medical and osteopathic boards’ positions on chaperones during gynecologic examinations. Obstet Gynecol. 1999;94:352–4. [DOI] [PubMed]
- 12.Speelman A, Savage J, Verburgh M. Use of chaperones by general practitioners. BMJ. 1993;307:986–7. [DOI] [PMC free article] [PubMed]
- 13.Price DH, Tracy CS, Upshur REG. Chaperone use during intimate examinations in primary care: postal survey of family physicians. BMC Fam Pract. 2005;6:52. [DOI] [PMC free article] [PubMed]
- 14.Ehrenthal DB, Farber NJ, Collier VU, Aboff BM. Chaperone use by residents during pelvic, breast, testicular, and rectal exams. J Gen Intern Med. 2000;15(8):573–6. [DOI] [PMC free article] [PubMed]
- 15.Schatz B, O’Hanlan KA. Anti-gay Discrimination in Medicine: Results of a National Survey of Lesbian, Gay, And Bisexual Physicians. San Francisco, CA: Gay and Lesbian Medical Association; 1994.
- 16.US Census Bureau. State and County QuickFacts; 2007. Available at: http://quickfacts.census.gov/qfd/states/00000.html, retrieved on February 21, 2007.
- 17.Black D, Gates G, Sanders S, Taylor L. Demographics of the gay and lesbian population in the United States: evidence from available systematic data sources. Demography. 2000;37(2):139–54. [DOI] [PubMed]
- 18.Senn CY, Verberg N, Desmarais S, Wood E. Sampling the reluctant participant: a random-sample response-rate study of men and sexual coercion. J Applied Soc Psych. 2000;30(1):96–105. [DOI]
- 19.Aizen I, Fishbein M. Understanding the Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980.
- 20.Klitzman RL, Greenberg JD. Patterns of communication between gay and lesbian patients and their health care providers. J Homosex. 2002;42(4):65–75. [DOI] [PubMed]
- 21.Risdon C, Cook D, Willms D. Gay and lesbian physicians in training: a qualitative study. CMAJ. 2000;162(3):331–4. [PMC free article] [PubMed]
- 22.Townsend MH, Wallick MM, Cambre KM. Support services for homosexual students at US medical schools. Acad Med. 1991;66(6):361–3. [DOI] [PubMed]


