Abstract
Background
Hyperglycemia is common among diabetic inpatients, and has been linked to adverse outcomes. However, antihyperglycemic treatment is seldom intensified in noncritical care patients, and the relationship between intensification frequency and glucose control is poorly understood. We evaluated the relationship between treatment intensification and changes in blood glucose in hospitalized diabetic patients.
Design
We retrospectively analyzed 3,613 hospitalized diabetic patients who were admitted to the hospital between January 2003 and August 2004, were not hospitalized in an ICU, were not prescribed IV insulin or total parenteral nutrition (TPN), had a length of stay of at least 3 days, and had at least one point-of-care blood glucose measurement. A linear model was used to assess the relationship between intensification of antihyperglycemic medications and the average daily change in point-of-care glucose measurements.
Results
Hyperglycemia (>180 mg/dL) was documented at least once for 82.5% of patient admissions. Antihyperglycemic treatment was intensified for 22.0% of days with hyperglycemia. Intensifications of scheduled and sliding scale insulin, but not oral medications, were associated with a 11.1 mg/dL (p < 0.0001) and 12.2 mg/dL (p < 0.0001) reduction in the average daily glucose, respectively. Hypoglycemia (<50 mg/dL) was documented on 2.2% of days after antihyperglycemic treatment intensification.
Conclusion
In this cohort, lack of treatment intensification in response to inpatient hyperglycemia was common. Antihyperglycemic treatment intensification was strongly associated with decrease in average daily glucose, while hypoglycemia was uncommon. This suggests that increasing the frequency of treatment intensifications could lead to improved glycemic control in inpatients with diabetes.
KEY WORDS: treatment intensification, hyperglycemia, hypoglycemia, diabetes mellitus, blood glucose, insulin
INTRODUCTION
Diabetes mellitus is a commonly encountered comorbid condition among hospitalized patients. In recent years, approximately 5 million hospitalizations annually were associated with diabetes, and 18% of all hospitalized adults had a secondary diagnosis of diabetes.1,2 Inpatient hyperglycemia has been associated with a number of adverse outcomes, such as increased length of stay, increased risk of infection, poor wound healing, decreased ability to live independently after discharge, and increased mortality.3–7
A number of evaluations within the intensive care environment have shown that aggressive treatment of hyperglycemia improves outcomes. These studies found lower infection rates,8,9 improved short-term mortality9,10 with intensive treatment, and accelerated discharge from the intensive care unit (ICU).11,12 Outside of the intensive care units, antihyperglycemic treatment of hospitalized patients is seldom intensified.13,14
A number of studies have linked treatment intensification to improved glycemic control in outpatient settings.15–17 However, it is not known how much effect such intensification has on hyperglycemia in the inpatient setting. Therefore, a retrospective study was conducted to evaluate the relationship between antihyperglycemic treatment intensification and blood glucose control in hospitalized diabetic patients.
RESEARCH DESIGN AND METHODS
Study Patients and Settings
The participants were patients with a diagnosis of diabetes who were admitted to a 734-bed teaching hospital between January 2003 and August 2004, which included 9,285 of 32,264 total hospitalizations (excluding pregnant women and newborns) during the study period. Diabetic patient hospitalizations were identified using a previously validated free text parsing algorithm called Diabetes Identification Through Textual element Occurrences (DITTO), which combines analysis of the text of outpatient physician notes with billing and laboratory data.18 When compared with manual record review, the algorithm had a sensitivity of 96.2% and a specificity of 98.0%.
A total of 3,613 diabetic patient hospitalizations were evaluated after the following exclusion criteria were applied: no documented point-of-care glucose (POCBG) testing results (3,824), admission to an ICU or received intravenous insulin (799), received total parenteral nutrition (TPN; 37), had a length of stay less than 3 days (989), or did not have any computerized medication order entry (CPOE) records available (23). Partners HealthCare System institutional review board granted expedited approval of this study and waived the need for informed consent.
Data Collection
Patient demographics, admission and discharge dates, laboratory data, discharge summaries, and outpatient physician notes were obtained from the Research Partners Data Registry (RPDR), a large data warehouse that serves as a central clinical data repository for participating hospitals and clinics within the Partners HealthCare System. CPOE data were obtained from the hospital inpatient electronic health record. POCBG data were obtained from the QC Manager system™ (Abbott Laboratories, Abbott Park, IL).
The inpatient CPOE data were semiformatted free text, and a series of Perl programs were written within ActiveState Komodo (Version 3.5, Vancouver, Canada) using regular expressions19 to parse discrete information from the data. All of the information was then linked by the patient’s unique hospital identifier and allocated to a specific hospitalization based on admission and discharge dates.
Measurements
The primary outcome was the average daily change in POCBG during a patient’s hospitalization. It was calculated as the slope of the line fitted through the mean daily POCBG levels over the entire hospital stay using the least squares method. The mean daily POCBG was used to normalize for variable numbers of glucose measurements per day as well as diurnal fluctuations for a given patient within the same hospital day. The secondary outcome was the incidence of hypoglycemia (defined as a single glucose level ≤50 mg/dL) the day after any treatment intensification.
Treatment intensification was defined as an increase in the total daily dose of any antihyperglycemic medication, which included either the initiation of a new medication or an increase in the dose of an existing medication. Treatment intensification was determined from CPOE data, excluding admission orders. Separate analyses were conducted for intensification of subcutaneous sliding scale insulin (SS), oral diabetic medications (PO), and scheduled subcutaneous insulin (SC). Discontinuations of medications or decreases in medication doses were not analyzed. Treatment intensification was linked to an episode of hyperglycemia when the medication order was written by the end of the day after the day the hyperglycemia was recorded. Hypoglycemia was linked to an episode of treatment intensification when it occurred by the end of the day after the intensification order was written.
Treatment intensification rates by medication category (PO, SC, and SS) were calculated for each patient hospitalization as the ratio of (1) the number of anti-hyperglycemic treatment intensifications associated with an episode of hyperglycemia to (2) the total number of days when hyperglycemia was observed, as shown in the following equation:
 |
For example, if a patient had 4 days of hyperglycemia in a hospital stay of 6 days, and received 1 day of SS intensification after a day of hyperglycemia, the SS intensification rate would be 0.25 (1/4) and the PO and SC intensification rates would be 0 (0/4).
Temporal relationships between meals and glucose measurements were not available in the dataset, and all POCBG measurements were conservatively assumed to be postprandial for the purpose of this evaluation. Recent reviews and American Diabetes Association (ADA) consensus statements have recommended using 180 mg/dL as the postprandial blood glucose target for hospitalized patients with diabetes. We therefore defined blood glucose levels ≥180 mg/dL as elevated in this evaluation.9,20
Glucocorticoid and antibiotic use was defined as any CPOE order present during a patient’s hospitalization for a medication in that class. Antibiotics were categorized by antibacterial, antifungal, and antiviral mechanisms of action. Patients were considered to have used glucocorticoids or antibiotics if these agents were ordered at any time during the hospitalization. Dosage as well as number of days the medication was administered were not included in the models.
Statistical Analysis
Evaluation of the effect treatment intensification had on the daily change in glucose was performed by multivariable linear regression analysis adjusting for patient age, gender, race, insurance, length of stay, the use of oral or intravenous steroids, and the use of an antibiotic. A mixed model with random effects was used to adjust for clustering within individual patients (when the same patient was admitted to the hospital more than once during the study period) and Diagnosis-related groups (DRG) codes. To correct for multiple hypothesis testing when evaluating the effect of scheduled insulin, sliding scale insulin, and oral antihyperglycemic medication intensification rates on blood glucose, p < 0.015 was used as the threshold for statistical significance based on the Bonferroni correction. Intensifications of multiple antihyperglycemic medication categories on the same day were analyzed separately. Six hundred thirty-three patients were lacking bedside glucose measurements on at least 2 separate hospital days (required for the calculation of a slope) or had no hyperglycemic episodes, and were excluded from this analysis. All statistical analyses were performed with SAS (Version 9.1, Cary, NC).
RESULTS
Three thousand six hundred and thirteen patient hospitalizations met the criteria for analysis, and a summary of demographic and clinical characteristics for these patients is shown in Table 1. On average, patients had a length of stay of 5.8 days, and POCBG measurements were taken 3.6 times per patient per day. Among those monitored, inpatient hyperglycemia was present at least once in 2,980 (82.5%) of hospitalizations. Table 1 includes the proportion of patient hospitalizations taking antihyperglycemic medications by category and combination of categories. Aggregating combination therapies, a total of 3,034 (84.0%) patient hospitalizations utilized sliding scale orders, 1,250 (34.6%) utilized scheduled insulin orders, and 1,240 (34.3%) utilized oral antihyperglycemic orders. Incidence of each category of therapy employed for each day of hospitalization is shown in Figure 1, and the discrepancy between the aggregate use and maximal daily use is caused by staggered medication starting and stopping dates.
Table 1.
Clinical and Demographic Characteristics
| Characteristic | Value |
|---|---|
| Mean age (years)* | 64.1 (14.9) |
| Mean length of stay (days)* | 5.8 (5.8) |
| Mean Bedside Glucose (mg/dL)* | 172.0 (76.2) |
| Mean POCBG Measurements (per patient per day)* | 3.6 (1.1) |
| Total Patient Hospitalizations | 100.0 (3613) |
| Female† | 51.7 (1867) |
| Race † | |
| White | 59.3 (2143) |
| African American | 21.5 (776) |
| Hispanic | 10.4 (377) |
| Other/Unknown | 8.8 (317) |
| Insurance† | |
| Medicare | 55.2 (1993) |
| Medicaid | 14.6 (527) |
| Commercial | 29.6 (1069) |
| Self-Pay | 0.6 (24) |
| Anti-Hyperglycemic Use (By Category)† | |
| All Categories (SS, SC, and PO) | 5.3 (190) |
| SS and SC | 25.0 (904) |
| SS and PO | 25.1 (908) |
| SC and PO | 0.8 (30) |
| SS Only | 28.6 (1032) |
| SC Only | 3.5 (126) |
| PO Only | 3.1 (112) |
| Admission Service† | |
| Medical | 62.1 (2244) |
| Surgical | 36.3 (1310) |
| Unknown | 1.6 (59) |
| Most Common Admission DRGs †: | |
| 127 (Heart failure shock) | 5.95 (215) |
| 89 (Simple pneumonia adult with complications) | 2.46 (89) |
| 209 (Major joint limb reattachment procedures of lower extremity) | 2.32 (84) |
| 144 (Other circulatory system diagnoses with complications) | 2.19 (79) |
| 296 (Nutritional miscellaneous metabolic disorders age >17 with complications) | 2.08 (75) |
POCBG=point-of-care blood glucose, SS=sliding scale insulin, SC=scheduled subcutaneous insulin, and PO=oral anti-hyperglycemic agents.
*Values are means with standard deviations.
†Values are means with percentages and total counts.
Figure 1.
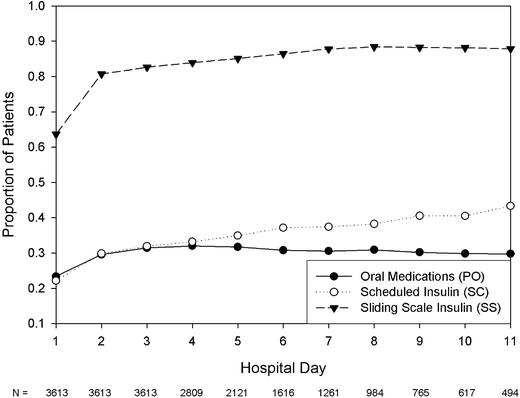
Proportion of patients receiving each category of anti-hyperglycemic medications by the day of hospitalization.
Some form of antihyperglycemic therapy intensification was ordered in 1,314 hospitalizations. Overall, antihyperglycemic treatment intensifications occurred after only 2,944 of 13,360 (22.0%) hospital days with hyperglycemia, and multiple categories of intensification were ordered together in 446 (3.3%) days. Among these, the most commonly ordered intensifications were scheduled insulin (1606 [12.0%]), followed by sliding scale insulin (937 [7.0%]), and oral medications (881 [6.6%]). Unadjusted effects of intensification on average daily blood glucose are shown in Figure 2. A summary of these characteristics is shown in Table 2.
Figure 2.
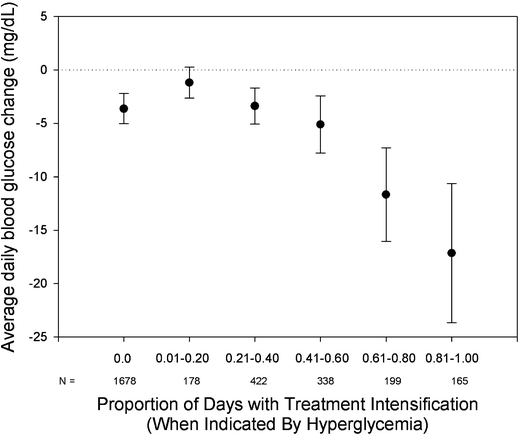
Unadjusted average daily blood glucose change in proportional categories of treatment intensification. N=number of patient hospitalizations in that category.
Table 2.
Characteristics of Patient Glycemic Control
| Characteristic | Percent (%), Number (N) |
|---|---|
| Total Hospital Days | 100.0 (24,653) |
| Hyperglycemia Present | 54.2 (13,360) |
| Hypoglycemia Present | 1.8 (434) |
| Total Hyperglycemic Days | 100.0 (13360) |
| Any Treatment Intensification | 22.0 (2944) |
| Scheduled Insulin Intensification | 12.0 (1606) |
| Sliding Scale Insulin Intensification | 7.0 (937) |
| Oral Medication Intensification | 6.6 (881) |
Patients had 1 or more episodes of hypoglycemia on 1.8% (434/24,653) of all hospitalized days. Hypoglycemia was encountered in 2.2% (53/2,374) of hyperglycemic patients the day after intensification of any therapy, and in 2.1% (309/15,053) without any intensification. The comparison of event rates with and without intensification was performed excluding the day of admission.
Two thousand nine hundred and eighty of 3,613 (82.5%) patient hospitalizations had at least 2 days of recorded POCBG measurements, and experienced at least 1 day of hyperglycemia during the hospitalization. Results of the effects of each category of intensification on the outcome after adjusting for patient age, gender, race, length of stay, insurance, DRG code, and the use of glucocorticoids or antibiotics are shown in Table 3. Increase in the rate of intensification of sliding scale insulin from 0% to 100% was associated with a 12.2 mg/dL average daily reduction in bedside glucose (p < 0.0001), whereas a similar increase in the rate of intensification of scheduled subcutaneous insulin was associated with an 11.1 mg/dL average daily reduction in the bedside glucose (p < 0.0001). Intensification of oral diabetic agents was not associated with a significant reduction in daily bedside glucose.
Table 3.
Average Daily Change in Glucose for Each Category of Intensification Adjusted for Age, Gender, Race, Length of Stay, Glucocorticoid Use, and Antibiotic Use
| Intensification Type | Slope (mg/dL/day) | Standard Error (mg/dL/day) | p |
|---|---|---|---|
| Scheduled Insulin | −11.1 | 2.34 | <.0001 |
| Sliding Scale Insulin | −12.2 | 2.47 | <.0001 |
| Oral Medication | −5.5 | 2.58 | .032 |
P < .015 was considered significant based on the Bonferroni correction.
CONCLUSIONS
In this large observational single institutional sample, treatment intensification occurred in less than 1/4 of days when hyperglycemia occurred. There was a strong association between the frequency of both scheduled and sliding scale insulin intensification and the magnitude of decline in mean daily blood glucose. These findings are consistent with studies in outpatient settings which demonstrate that (1) treatment intensification is infrequent and (2) low frequency of treatment intensification is associated with reduced achievement of glycemic goals.
Although tight glycemic control has been shown to improve outcomes in some critically ill patients, it is unknown whether intensive glycemic control has benefits outside of an ICU environment. No randomized, controlled, interventional trials have been conducted to assess this. Such trials would be logistically difficult for multiple reasons, including the lack of available protocols for antihyperglycemic treatments with strategies besides intravenous insulin. These results, which show a direct relationship between the frequency of insulin intensification and the magnitude of blood glucose reductions, suggest a potential strategy for the reduction of hyperglycemia in a non-ICU general inpatient ward setting, where intravenous insulin typically is not used.
These findings are consistent with prior evaluations supporting the utility of scheduled insulin intensifications.14 Although there is general agreement in the literature that the sliding scale method is not very effective,9,14,21–24 this study found that intensification of sliding scale insulin also was associated with a significant decrease in blood glucose levels.25 No association between intensification of oral diabetic agents and reduction of hyperglycemia was found. Fear of hypoglycemia is a commonly cited concern for frequent insulin intensification among hospitalized patients.26 In this study, the incidence of hypoglycemia was similar with or without intensification.
In the outpatient treatment of diabetes, numerous factors impede the successful treatment of hyperglycemia, including access to care, patient adherence, and availability of home glucose data.16,27,28 Many of these factors are absent in the inpatient setting, and therefore effective process of care, including timely treatment intensification, acquires prominence among determinants of glycemic outcomes. However, there are also potential obstacles to intensification that exist only in the inpatient setting, such as a change in the patient’s clinical status, rapidly decreasing glucocorticoid dose, or anticipation of discharge, that must also be addressed. In our study, similar to previous reports,13 rates of treatment intensification continue to be low.
This evaluation has a number of strengths. Because of the availability of electronic data in our local institution, we were able to evaluate several thousand ethnically and socioeconomically diverse patients. Unlike most of the previously published reports on outcomes of treatment of inpatient hyperglycemia, which focused on patients treated in the intensive care unit, our study analyzed treatment of hyperglycemia in the general ward, where most of the diabetic patients are hospitalized.
It should also be noted that there was a small but significant unadjusted decline in mean daily blood glucose among the patients who never received an intensification of therapy (Fig. 2). This could be caused by a transient elevation in blood glucose in the acute setting that later spontaneously improved with the resolution of illness. Inability to account for the changes in the patient’s clinical status is therefore a potential limitation of this study.9 However, in the fully adjusted model, this trend should result in a conservative estimate of the effect that intensification had on the change in the blood glucose.
There are several limitations to this study. Only inpatient glucose and medication data for patients were available. Thus, outpatient glycemic control before admission could not be determined, and comparison between outpatient and inpatient antihyperglycemic medication regiments (both pre- and posthospitalization) could not be performed. In a retrospective observational analysis, the inability to capture and incorporate all of the potential factors affecting the outcome of interest can introduce bias in the analysis. In addition, missing data can create bias in the results. Also, all medication intensifications were measured from the CPOE data because medication administration records were only available on paper. While these are generally accurate in terms of dosing, more variability exists regarding the time of administration. The study attempted to minimize this by evaluating dose changes by days, and allowing both the same day and the next day to count as a successful intensification after a hyperglycemic episode. In addition, while glucocorticoid administration was included in the model for adjustment, hyperglycemia among patients can be dose-dependent, and glucocorticoid dosage was not included in the model. Patients who stayed in the hospital less than 3 days were excluded from the study and therefore the study findings are not applicable to this population. The generalizability of the results is also limited by single institutional evaluation.
In summary, this study demonstrates an association between the frequency of both scheduled and sliding scale insulin intensification and the magnitude of decline in the mean daily blood glucose in diabetic patients hospitalized on the general ward. Further studies are needed to establish whether decrease in blood glucose levels leads to improvements in the clinical outcomes in this patient population.
Acknowledgments
This study was supported by grants from the Diabetes Trust Foundation (to AT), Diabetes Action Research and Education Foundation (to AT), and T15-LM-07092 from the National Library of Medicine (to MEM). The authors would like to thank Jennifer Rogala for her assistance extracting the CPOE orders from the inpatient medical record, and Shawn Murphy and the staff of the Laboratory of Computer Science (LCS) for the use of the RPDR.
Conflicts of Interest Statement None disclosed.
Footnotes
Conference Abstract: American Diabetic Association 2007
Contributor Information
Michael E. Matheny, Phone: +1-615-3274751, FAX: +1-615-3275381, Email: michael.matheny@vanderbilt.edu.
Alexander Turchin, Email: aturchin@partners.org.
References
- 1.Agency for Healthcare Research and Quality. HCUPnet, Healthcare Cost and Utilization Project. Rockville, MD; 2005.
- 2.Brunkhorst FM, Kuhnt E, Engel C, et al. Intensive insulin therapy in patients with severe sepsis and septic shock is associated with an increased rate of hypoglycemia—results from a randomized multicenter study (VISEP). Infection 2005;33:19–20.
- 3.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 2002;87:978–82. [DOI] [PubMed]
- 4.Pomposelli JJ, Baxter JK, 3rd, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. JPEN J Parenter Enteral Nutr 1998;22:77–81. [DOI] [PubMed]
- 5.Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 2000;355:773–8. [DOI] [PubMed]
- 6.Bolk J, van der Ploeg T, Cornel JH, Arnold AE, Sepers J, Umans VA. Impaired glucose metabolism predicts mortality after a myocardial infarction. Int J Cardiol 2001;79:207–14. [DOI] [PubMed]
- 7.Pulsinelli WA, Levy DE, Sigsbee B, Scherer P, Plum F. Increased damage after ischemic stroke in patients with hyperglycemia with or without established diabetes mellitus. Am J Med 1983;74:540–4. [DOI] [PubMed]
- 8.Golden SH, Peart-Vigilance C, Kao WH, Brancati FL. Perioperative glycemic control and the risk of infectious complications in a cohort of adults with diabetes. Diabetes Care 1999;22:1408–14. [DOI] [PubMed]
- 9.Garber AJ, Moghissi ES, Bransome ED, Jr. et al. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract 2004;10:77–82. [DOI] [PubMed]
- 10.van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001;345:1359–67. [DOI] [PubMed]
- 11.Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006;354:449–61. [DOI] [PubMed]
- 12.Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc 2004;79:992–1000. [DOI] [PubMed]
- 13.Knecht LA, Gauthier SM, Castro JC, et al. Diabetes care in the hospital: is there clinical inertia? J Hosp Med 2006;1:151–60. [DOI] [PubMed]
- 14.Queale WS, Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus. Arch Intern Med 1997;157:545–52. [DOI] [PubMed]
- 15.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med 2001;135:825–34. [DOI] [PubMed]
- 16.Berlowitz DR, Ash AS, Glickman M, et al. Developing a quality measure for clinical inertia in diabetes care. Health Serv Res 2005;40:1836–53. [DOI] [PMC free article] [PubMed]
- 17.Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes (IPCAAD) 8. Arch Intern Med 2006;166:507–13. [DOI] [PubMed]
- 18.Turchin A, Kohane IS, Pendergrass ML. Identification of patients with diabetes from the text of physician notes in the electronic medical record. Diabetes Care 2005;28:1794–5. [DOI] [PubMed]
- 19.Friedl JEF. Mastering Regular Expressions. Second edn. Cambridge, MA: O’Reilly and Associates; 2002.
- 20.Inzucchi SE. Clinical practice. Management of hyperglycemia in the hospital setting. N Engl J Med 2006;355:1903–11. [DOI] [PubMed]
- 21.Lorber DL. Sliding scale insulin. Diabetes Care 2001;24:2011–2. [DOI] [PubMed]
- 22.Genuth S. The automatic (regular insulin) sliding scale or 2, 4, 6, 8-call H.O. Clin Diabetes 1994;12:40–2.
- 23.Dickerson LM, Ye X, Sack JL, Hueston WJ. Glycemic control in medical inpatients with type 2 diabetes mellitus receiving sliding scale insulin regimens versus routine diabetes medications: a multicenter randomized controlled trial. Ann Fam Med 2003;1:29–35. [DOI] [PMC free article] [PubMed]
- 24.Golightly LK, Jones MA, Hamamura DH, Stolpman NM, McDermott MT. Management of diabetes mellitus in hospitalized patients: efficiency and effectiveness of sliding-scale insulin therapy. Pharmacotherapy 2006;26:1421–32. [DOI] [PubMed]
- 25.Bode BW, Braithwaite SS, Steed RD, Davidson PC. Intravenous insulin infusion therapy: indications, methods, and transition to subcutaneous insulin therapy. Endocr Pract 2004;10 Suppl 2:71–80. [DOI] [PubMed]
- 26.Murata GH, Hoffman RM, Shah JH, Wendel CS, Duckworth WC. A probabilistic model for predicting hypoglycemia in type 2 diabetes mellitus: the Diabetes Outcomes in Veterans Study (DOVES). Arch Intern Med 2004;164:1445–50. [DOI] [PubMed]
- 27.Wexler DJ, Meigs JB, Cagliero E, Nathan DM, Grant RW. Prevalence of hyper- and hypoglycemia among inpatients with diabetes: a national survey of 44 U.S. hospitals. Diabetes Care 2007;30:367–9. [DOI] [PubMed]
- 28.O’Connor PJ. Improving diabetes care by combating clinical inertia. Health Serv Res 2005;40:1854. [DOI] [PMC free article] [PubMed]


