Abstract
Diagnostic errors are poorly understood despite being a frequent cause of medical errors. Recent efforts have aimed to advance the "basic science" of diagnostic error prevention by tracing errors to their most basic origins. Although a refined theory of diagnostic error prevention will take years to formulate, we focus on communication breakdown, a major contributor to diagnostic errors and an increasingly recognized preventable factor in medical mishaps. We describe a comprehensive framework that integrates the potential sources of communication breakdowns within the diagnostic process and identifies vulnerable steps in the diagnostic process where various types of communication breakdowns can precipitate error. We then discuss potential information technology-based interventions that may have efficacy in preventing one or more forms of these breakdowns. These possible intervention strategies include using new technologies to enhance communication between health providers and health systems, improve patient involvement, and facilitate management of information in the medical record.
KEY WORDS: diagnostic errors, patient safety, communication, information technology
THE PROBLEM OF DIAGNOSTIC ERRORS
Diagnostic errors are a frequent cause of medical errors in the United States. Large risk-management database studies have shown that out of all liability claims, those related to diagnoses are the most frequent and expensive (about 40% of all malpractice payments in 2003, with an average payment of approximately $300,000 per claim1). One such study analyzed 49,345 malpractice claims between 1985 and 2000 and found over one-third of the claims to be caused by diagnostic error.2 Although the true prevalence of diagnostic error is unknown, 1 in 6 subjects interviewed in a National Patient Safety Foundation poll claimed to have personally experienced diagnostic error.3 Such errors also appear to be burdensome in the training environment.4–6
Diagnostic errors are defined as those in which diagnosis was unintentionally delayed (sufficient information was available earlier), wrong (another diagnosis was made before the correct one), or missed (no diagnosis was ever made), as judged from the eventual appreciation of more definitive information.7 Examples include failure to use an indicated diagnostic test, misinterpretation of test results, and failure to act on abnormal results.8 Although diagnostic errors may occur when signs of a disease are atypical or absent, diagnostic errors are often attributed to cognitive (e.g., faulty clinical reasoning) and/or systems-related factors (e.g., inefficient processes and poor communication7,9–21). Despite the importance of diagnostic errors, relatively little is known about their causes and prevention.22 Thus, a comprehensive approach to understanding diagnostic errors is needed to guide the development of future interventions to prevent the occurrence of these errors.
Little is known about the precise cognitive processes that physicians use to confirm and reject their diagnostic hypotheses,20 and diagnostic difficulties persist despite practitioner experience and advances in diagnostic tests.23,24 Although a refined cognitive theory of diagnostic decision making will require years of development, in the near term communication processes are a more feasible target for improving the timeliness and accuracy of diagnoses. Communication breakdowns are an increasingly recognized preventable factor in medical mishaps, and emerging data suggest a high prevalence of communication breakdowns among physicians, patients, and important members of the health care team who assist with the diagnostic process.21,25–32 For example, in a study of abnormal mammograms, over a third of the women studied did not receive appropriate follow-up.30 In another study, 68% of specialists reported not receiving any information from the primary care physician before the referral visit, and 25% of primary care physicians reported that they still had not received any information from specialists 4 weeks after referral visits.28 Thus, addressing preventable communication breakdowns by using resources such as information technology offers a viable and timely opportunity to improve the diagnostic quality.
THE ANATOMY OF COMMUNICATION BREAKDOWNS IN DIAGNOSIS
Diagnostic Steps
According to Kuhn, the process of making a diagnosis involves 3 sequential, overlapping steps: data gathering, data integration, and verification of diagnosis.23 Data gathering occurs when critical diagnostic information is collected during a physician–patient encounter primarily through history-taking, physical examination, and review of medical records;23 hence, any information gathered before formulating one’s thoughts or analyzing a patient’s condition to formulate a diagnosis could be thought as data gathering.
The second step of the diagnostic process is data integration, a cognitive process involving physician judgment and expertise.23 Inadequate data collection would lead to errors in clinical reasoning and therefore in data integration as well. The third diagnostic step, diagnosis verification, entails the confirmation or rejection of diagnostic hypotheses by obtaining further data such as laboratory tests, imaging, or pathology specimens.23 Thus, all 3 of the above steps, but particularly data gathering and diagnosis verification, rely on good communication and may be targeted for interventions to improve the process of making a correct diagnosis.
Communication Breakdowns in the Diagnostic Process
For the purpose of this article, we define 2 forms of communication that are relevant to the data gathering and verification steps of the diagnostic process: interpersonal communication and informational communication.33 Interpersonal communication is the verbal exchange of information between 2 individuals (e.g., physicians, patients, nurses, etc.). Informational communication, conversely, entails the processing and management of data such as notes in a chart, written instructions, laboratory values, imaging reports, or any aspect of data retrieved with an electronic chart system.
In addition to identifying the diagnostic steps that are vulnerable to communication breakdowns (data gathering and diagnosis verification), and the types of communication involved (interpersonal or informational), we can further analyze the sources of diagnostic errors by examining the point at which errors occur in the chain of communication. In this paper, it is worthwhile to consider the goals of communication in the health care setting: often communication is not only intended to transfer information, but also to generate a response from the recipient of the information, such as taking an action and acknowledging receipt of the information.34 In our recent work on informational communication related to diagnosis verification, we have validated a 3-point taxonomy of communication breakdowns proposed by Weinger in which communication errors are classified as breakdowns in message transmission, message reception, and message acknowledgement.35 Breakdowns in message transmission include failure to transmit essential information for making a diagnosis, delayed transmission of this information, or transmitted information that is wrong, ambiguous, or incomplete. Breakdowns in message reception occur when the recipient does not perceive the information, when the perception is incorrect, or when the recipient fails to act on the message. Breakdowns in message acknowledgement include failures to acknowledge receipt or understanding of the received message or failure to state when appropriate action has been taken. Although message acknowledgement is not strictly necessary for data synthesis and follow-up action in all cases, acknowledgement facilitates concordance among parties and typically implies that some action will follow. Thus, an acknowledgement breakdown can still lead to a poor outcome because the sender may not be able to verify whether the message was received and the action took place.
A FRAMEWORK TO UNDERSTAND AND REDUCE COMMUNICATION BREAKDOWNS
The 2 steps of the diagnostic process (data gathering and diagnosis verification) are the starting points of the flowchart shown in Figure 1, a three-level framework that ties these steps to the communication process. Using interpersonal or informational communication, messages are transmitted to, received by, and acknowledged by the physician during both the data gathering and diagnosis verification steps (see Fig. 1). Hence, our model includes twelve possible types of communication errors (see Table 1; henceforth we will refer to Examples 1–12 from this table). This framework posits that many diagnostic errors can be traced to 1 or more communication errors during data gathering and diagnosis verification. It serves as a conceptual foundation for designing future interventions to prevent communication breakdowns. Complex interventions can be developed and tested at multiple checkpoints along this framework.
Fig. 1.
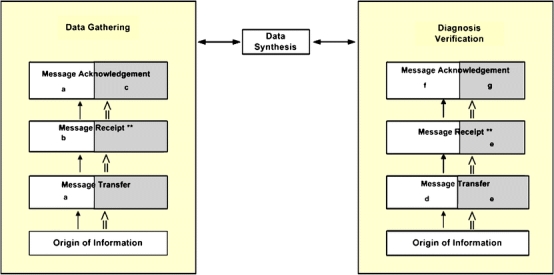
A Framework Integrating the Diagnostic Process with Communication Breakdowns. **Message reception can lead directly to data synthesis (and hence action) without message acknowledgement in some cases.  Interpersonal communication,
Interpersonal communication,  Informational communication,
Informational communication,  Interpersonal communication,
Interpersonal communication,  Informational communication. a. Collaborative goal-setting using an Information Technology platform (Example 1 from table), b. Use of personal health records (Example 2), c. Using electronic progress notes requiring co-signatures of physician (Example 5), d. Electronic Medical Record generated report transmitted to pager or mobile phone of referring physician (Example 7), e. Use of alerts for abnormal test results (Example 10), f. Electronic Medical Record generated reminders to patient and physician (Example 3), g. Using software to track unacknowledged alerts (Example 12)
Informational communication. a. Collaborative goal-setting using an Information Technology platform (Example 1 from table), b. Use of personal health records (Example 2), c. Using electronic progress notes requiring co-signatures of physician (Example 5), d. Electronic Medical Record generated report transmitted to pager or mobile phone of referring physician (Example 7), e. Use of alerts for abnormal test results (Example 10), f. Electronic Medical Record generated reminders to patient and physician (Example 3), g. Using software to track unacknowledged alerts (Example 12)
Table 1.
Types and Examples of Communication Breakdowns that Can Lead to Diagnostic Errors
| Examples of communication breakdowns that may result in data gathering-related diagnostic errors |
|---|
| 1. Interpersonal transmission errors: A patient does not inform her physician about a new growth in her breast. |
| 2. Interpersonal reception errors: The patient informs his physician about a change in his mole, but the physician gets distracted by an interruption and fails to perform a complete history and exam. |
| 3. Interpersonal acknowledgment errors: The physician informs the patient to return to the clinic after an urgent x-ray, but does not verify that the patient understood. Patient gets lost to follow-up leading to delayed diagnosis. |
| 4. Informational transmission errors: A patient calls the nurse 2 days after a physician visit with continued symptoms of fever and chills; information is recorded appropriately but is lost before it reaches the physician. |
| 5. Informational reception errors: Information about a patient’s continued symptoms is placed in the physician’s message inbox but not dated; physician misunderstands and believes that the note was from 2 days ago. |
| 6. Informational acknowledgment errors: A physician reads an email from a nurse about a recent change in a patient’s mole, but does not inform the nurse what to do next. The patient believes that the physician is not too concerned and does not seek care. |
| Examples of communication breakdowns that may result in diagnosis verification related diagnostic errors |
|---|
| 7. Interpersonal transmission errors: A radiologist fails to inform the referring physician about free air noted on a patient’s abdominal x-ray. |
| 8. Interpersonal reception errors: The laboratory calls the on-call physician on a weekend to inform her about the abnormal test results, but the covering physician informs the wrong primary physician. The patient’s physician never receives the abnormal test result. |
| 9. Interpersonal acknowledgment errors: The laboratory calls the on-call physician at night about a critical test result, but the physician is only partially awake; no action is taken. |
| 10. Informational transmission errors: An abnormal radiology report of a potential malignancy is not sent to the primary care physician. |
| 11. Informational reception errors: An electronic notification of the abnormal radiology report is sent to the physician via the electronic medical record, but the physician either does not read the alert transmitting the test result or fails to take action on it. |
| 12. Informational acknowledgment errors: Physician does not electronically acknowledge the receipt of transmitted abnormal test results. No further action is taken and the results are lost to follow-up. |
DEFINING THE ROLE OF INFORMATION TECHNOLOGY IN REDUCING COMMUNICATION BREAKDOWNS THAT RESULT IN DIAGNOSTIC ERRORS
To improve communication and patient safety, the Institute of Medicine has called for redesigning and error-proofing health care delivery systems.36 One method for achieving this goal is to develop electronic information systems for the delivery of health care data.36,37 Using information technology (IT) and adopting electronic medical records (EMR) can significantly improve the quality of information transfer38,39 and reduce failures in several of the pathways we have described. Although we believe that IT-related interventions have tremendous potential in reducing communication breakdowns that lead to diagnostic errors, other innovative communication strategies have also been proposed. For example, the Situation-Background-Assessment-Recommendation (SBAR) technique implemented widely at health systems such as Kaiser Permanente standardizes communication and reduces breakdowns related to data gathering.40 Another intervention known as “read-back verification” requires the clinician to repeat the information back to the person who transmitted it, completing the loop of reception and acknowledgement in a verifiable manner.41 This technique could be useful to prevent the communication breakdown in Example 9.
IT-based interventions alone, however, cannot assure improvements in communication. For instance, computerized information systems themselves can lead to unintended errors including those that involve communication processes.25,34,42 Studies including our own have reported communication breakdowns among providers even in systems that use advanced IT.25 Thus, achieving high standards of patient safety through the use of IT also entails system redesign to include formal policies and procedures regarding the use of IT.43–47 To improve the design of any IT-based system, the IOM proposes the application of engineering concepts and methods, especially in the area of human factors.36,37 Systems that use IT must first be tested on their usability, which represents the effectiveness, efficiency, and satisfaction with which specific users can achieve a specific task by using the system. Efforts must also be targeted to train future physicians to adopt and use IT appropriately for diagnostic purposes.
SPECIFIC TECHNIQUES TO ENHANCE COMMUNICATION
Improving Communication Breakdowns Related to Data Gathering by Physicians
Data gathering problems may be the most common reasons for diagnostic errors, at least among trainees.4 Clearly, the training curriculum needs to further emphasize traditional history and physical examination to our future physicians, who tend to over-rely on expensive and unnecessary diagnostic tests.48 However, there are also several ways in which IT could play an important role in data gathering (Fig. 1) by practicing physicians, e.g.:
An EMR can reduce the problem of missing clinical information that is frequently encountered in paper-based records.49
Patients can use personal health records (PHRs; secure electronic repositories of health information50) to generate their own medical histories before their visits and integrate selected information with the physician’s EMR at their discretion.51 In Example 2, an interpersonal reception problem could be averted if the melanoma complaint were integrated with the physician’s EMR through the patient’s PHR.
EMRs can provide effective decision support, clinical reminders, and other diagnostic aids so that the diagnostic workup can be automatically prompted based on complaints and findings.
Provider-to-provider communication through electronic progress notes could reduce communication breakdowns between health providers as in Examples 4 and 5.
EMR linkages can make available a “distributed” electronic health record to several providers across multiple health care systems and thereby centralize patient information to facilitate diagnosis.
Improving Communication Breakdowns in the Diagnosis Verification Process
Alerting for Diagnostic Test Result Management Several EMRs use a notification system (for instance, the VA’s View Alert system) that immediately alerts clinicians about clinically significant events such as abnormal test results. Electronic “alerts” have been shown to improve critical lab results communication in the inpatient setting, and they show promise in improving the safety of outpatient test result follow-up.45,52,53 Electronic alerting could help prevent the communication breakdown in Example 10, where the abnormal report would be sent to the provider’s EMR screen automatically. However, what about Examples 11 and 12, when providers fail to take action or acknowledge the alert or simply ignore alerts because they receive too many? Customizing EMR screens to receive only critical alerts and using special alert management software to track them can avoid such problems. For instance, the VA’s View Alert system tracks acknowledgement of abnormal test results, and results that go unacknowledged receive a higher degree of oversight to reduce the chance that the report would be lost in the system (e.g., Example 12).25 In addition, “smart monitors” could reduce the total number of alerts by filtering information through algorithms so that providers are alerted only when immediate action is necessary.54
Direct Reporting of Test Results Providers may report test results directly to their patients through secure electronic mail, web-based portals, and other methods. Although direct reporting to patients may prevent loss of follow-up, physicians currently tend to favor direct reporting only when test results are normal, have less diagnostic severity, or have less potential for emotional impact.55 This evolving concept is likely to gain strength in the future.
Reinforcing Critical Result Transmission by More Than One Method To complement the transmission of results through EMRs, pagers and other wireless data devices could be used to communicate abnormal test results requiring immediate attention.56 Additional use of data mining, a technique used to search electronic repositories, can identify exceptions automatically. For example, automated programs can review all lab results over a given time period and alert clinicians to abnormal results that have not received appropriate follow up (e.g., positive fecal occult blood tests not followed up by a colonoscopy).
Tracking Consultations Consultations can be tracked from the moment the physician makes the electronic referral so that providers can identify patients who are not given an appointment or fail to show up for referral visits. The EMR can also be programmed to generate an urgent report to the referring physician by text messaging, which would have averted the communication breakdown in Example 7.
Using Electronic Mail to Supplement Communication Related to the Medical Encounter
Secure email can be an adjunct to interpersonal communication and facilitates both data gathering and diagnosis verification. Email also has potential to enhance patient–physician interaction, particularly when face-to-face communication is limited,57 and provides opportunities to improve the efficiency of clinical time use.58,59 Although overall patient desire to communicate with their physicians electronically is high,60 adoption by physicians is generally low61–63 and several barriers exist.64
Using IT to Strengthen Data Gathering-Related Communication with Patients
One prominent strategy to reduce diagnostic errors is shared decision making in the diagnostic process. Although patients employ many ingenious methods to engage clinicians, such as using notepads and tape recorders,65 many of these processes are prone to the same errors that contribute to communication breakdowns. Standardized physician–patient communication software that is integrated with an EMR and a PHR could lead to better communication outcomes. Collaborative goal-setting is one promising intervention for reducing transmission and acknowledgement breakdowns in interpersonal communication.66 If integrated with an IT platform, goal-setting may enhance patients’ perceptions of risks pertaining to diagnostic tests, expectations regarding the significance of posttest results, and self-efficacy with the diagnostic process. This type of intervention could reduce delays in diagnosis and treatment resulting from communication breakdowns as in Example 1, especially among high-risk patients.
Websites of government agencies and large national organizations including the Agency for Healthcare Research and Quality (AHRQ) and the American Association of Retired Persons (AARP) offer patients information about how to get the most out of a doctor visit. Dissemination of these techniques using IT as a medium could enhance patient understanding of risks and expectations regarding diagnostic procedures and prompt them to discuss important information in future visits.
Overcoming Communication Problems Related to Patient Follow-up and Monitoring
EMRs can track patient appointments for tests and consultations and hence can facilitate interpersonal communication during diagnosis verification. For instance, in Example 3 the interpersonal acknowledgement problem could be overcome using an EMR-generated reminder letter to the patient followed by a reminder notification to the physician. PHRs can also be used to provide patient reminders for tests and appointments.
Interactive communication between patients using IT is another avenue for reducing diagnostic errors. The internet has become a natural experiment for uncontrolled and unstructured peer communication regarding medical diagnoses. In a recent study, the internet proved to be a remarkably effective and accurate mechanism for enhancing peer communication.67 Other studies testing a telephone-based peer support communication tool for chronic heart failure and diabetes care are currently underway. These studies use an interactive voice response tool to enhance self-care and improve the diagnosis of disease decompensation.68,69 Closer monitoring of patients with increased health care needs in their homes via devices and applications connected to an electronic network can also facilitate earlier diagnosis when problems arise.
CONCLUSIONS
Focusing interventions on diagnostic steps that are prone to communication breakdowns could achieve a significant reduction in diagnostic errors. We present a novel and comprehensive framework for understanding the complexity of communication breakdowns that lead to diagnostic errors. This framework can inform the design and testing of IT-based interventions to improve the effectiveness of communication. Multidisciplinary IT-based strategies that integrate the science of physician–patient communication and health informatics can offer a pragmatic approach to reduce diagnostic errors in health care.
Acknowledgments
We acknowledge Dr. Richard Street, PhD, Head, Department of Communication, Texas A&M University and Chief, Health Decision-Making and Communication Program at the Houston Center for Quality of Care and Utilization Studies, for his thoughtful insights about an earlier version of this manuscript, and Annie Bradford for her assistance with technical writing.
Conflict of Interest None disclosed.
Funding This work was supported by Grant Number K23CA125585 from the National Cancer Institute to Dr. Singh.Dr. Naik is supported by the National Institute of Aging (NIH K23AG027144).Dr. Petersen was a Robert Wood Johnson Foundation Generalist Physician Faculty Scholar (grant number 045444) at the time this work was completed and is a recipient of the American Heart Association Established Investigator Award (grant number 0540043N).This article is the result of work supported with resources and the use of facilities at the Houston Center for Quality of Care & Utilization Studies, The Center of Inquiry to Improve Outpatient Safety through Effective Electronic Communication and Michael E. DeBakey Veterans Affairs Medical Center.The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health, or the Department of Veterans Affairs.None of the funding sources had any role in the preparation, review, or approval of the manuscript.
Reference
- 1.Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood). 2005;Suppl Web Exclusives:W5. [DOI] [PubMed]
- 2.Phillips RL Jr, Bartholomew LA, Dovey SM, Fryer GE Jr, Miyoshi TJ, Green LA. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13:121–6. [DOI] [PMC free article] [PubMed]
- 3.Golodner L. How the public perceives patient safety. Newsletter of the National Safety Foundation. 2004;1997:1–6.
- 4.Singh H, Thomas EJ, Khan M, Petersen LA. Identifying diagnostic errors in primary care using an electronic screening algorithm. Arch Intern Med. 2007;167(3):302–8. [DOI] [PubMed]
- 5.Singh H, Thomas EJ, Petersen LA, Studdert DM. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007 Oct 22;167(19):2030–6. [DOI] [PubMed]
- 6.Wu AW, Folkman S, McPhee SJ, Lo B. Do house officers learn from their mistakes? JAMA. 1991;265:2089–94. [DOI] [PubMed]
- 7.Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165:1493–9. [DOI] [PubMed]
- 8.Agency for Healthcare Research and Quality. Medical Errors: The Scope of the Problem. Fact Sheet, Publication No AHRQ 00-P037. 2005. Available at http://www.ahrq.gov/qual/errback.htm. Accessed 7-11-2007.
- 9.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145:488–96. [DOI] [PubMed]
- 10.Croskerry P. Diagnostic failure: a cognitive and affective approach. AHRQ . 2005. Available at Available at: http://www.ahrq.gov/downloads/pub/advances/vol2/Croskerry.pdf. Accessed 7-2-2007. [PubMed]
- 11.Elstein AS. Heuristics and biases: selected errors in clinical reasoning. Acad Med. 1999;74:791–4. [DOI] [PubMed]
- 12.Hodder RJ, Ballal M, Selvachandran SN, Cade D. Variations in the evaluation of colorectal cancer risk. Colorectal Dis. 2005;7:254–62. [DOI] [PubMed]
- 13.Kahneman D, Slovic P, Tversky A. Judgment Under Uncertainty: Heuristics and Biases. Cambridge UK: Cambridge University Press; 1982.
- 14.Klein G. Sources of Power: How People Make Decisions. Cambridge, Massachusetts: The MIT Press; 1998.
- 15.McDonald CJ. Medical heuristics: the silent adjudicators of clinical practice. Ann Intern Med. 1996;124:56–62. [DOI] [PubMed]
- 16.Tanenbaum SJ. What physicians know. N Engl J Med. 1993;329:1268–71. [DOI] [PubMed]
- 17.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–8. [DOI] [PubMed]
- 18.Voytovich AE, Rippey RM, Suffredini A. Premature conclusions in diagnostic reasoning. J Med Educ. 1985;60:302–7. [DOI] [PubMed]
- 19.Kassirer JP, Kopelman RI. Cognitive errors in diagnosis: instantiation, classification, and consequences. Am J Med. 1989;86:433–41. [DOI] [PubMed]
- 20.Sox HC, Blatt MA, Higgins MC, Marton KI. Medical Decision Making. Stoneham, MA: Butterworth-Heinemann; 1988.
- 21.Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med. 2005;142:352–8. [DOI] [PubMed]
- 22.Singh H, Petersen LA, Thomas EJ. Understanding diagnostic errors in medicine: a lesson from aviation. Qual Saf Health Care. 2006;15:159–64. [DOI] [PMC free article] [PubMed]
- 23.Kuhn GJ. Diagnostic errors. Acad Emerg Med. 2002;9:740–50. [DOI] [PubMed]
- 24.Friedman CP, Gatti GG, Franz TM, et al. Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. J Gen Intern Med. 2005;20:334–9. [DOI] [PMC free article] [PubMed]
- 25.Singh H, Arora HS, Vij MS, Rao R, Khan M, Petersen LA. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459–66. [DOI] [PMC free article] [PubMed]
- 26.Boohaker EA, Ward RE, Uman JE, McCarthy BD. Patient notification and follow-up of abnormal test results. A physician survey. Arch Intern Med. 1996;156:327–31. [DOI] [PubMed]
- 27.Brenner RJ, Bartholomew L. Communication errors in radiology: a liability cost analysis. J Am Coll Radiol. 2005;2:428–31. [DOI] [PubMed]
- 28.Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15:626–31. [DOI] [PMC free article] [PubMed]
- 29.Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72. [DOI] [PubMed]
- 30.Poon EG, Haas JS, Louise PA, Gandhi TK, Burdick E, Bates DW, Brennan TA. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004;19:316–23. [DOI] [PMC free article] [PubMed]
- 31.Schiff GD. Introduction: communicating critical test results. Jt Comm J Qual Patient Saf. 2005;31:63–5. [DOI] [PubMed]
- 32.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79:186–94. [DOI] [PubMed]
- 33.Woolf SH, Kuzel AJ, Dovey SM, Phillips RL Jr. A string of mistakes: the importance of cascade analysis in describing, counting, and preventing medical errors. Ann Fam Med. 2004;2:317–26. [DOI] [PMC free article] [PubMed]
- 34.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;11:104–12. [DOI] [PMC free article] [PubMed]
- 35.Weinger MB, Blike G. Intubation Mishap. Agency for Health Care Research and Quality Web M & M Rounds. 2003.
- 36.Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, D.C.: National Academy Press; 1999.
- 37.Institute of Medicine of the National Academies. Patient Safety: Achieving a New Standard for Care. Washington, D.C.: National Academy Press; 2004. [PubMed]
- 38.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348:2526–34. [DOI] [PubMed]
- 39.Petersen LA, Orav EJ, Teich JM, O’Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24:77–87. [DOI] [PubMed]
- 40.Kaiser Permanente of Colorado. SBAR Technique for Communication: A Situational Briefing Model. The Institute for Healthcare Improvement . 2006. Available at http://www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm. Accessed 7-2-2007.
- 41.Barenfanger J, Sautter RL, Lang DL, Collins SM, Hacek DM, Peterson LR. Improving patient safety by repeating (Read-Back) telephone reports of critical information. Am J Clin Pathol. 2004;121:801–3. [DOI] [PubMed]
- 42.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13:547–56. [DOI] [PMC free article] [PubMed]
- 43.Brantley SD, Brantley RD. Reporting significant unexpected findings: the emergence of information technology solutions. J Am Coll Radiol. 2005;2:304–7. [DOI] [PubMed]
- 44.Brenner RJ. To err is human, to correct divine: the emergence of technology-based communication systems. J Am Coll Radiol. 2006;3:340–5. [DOI] [PubMed]
- 45.Kuperman GJ, Teich JM, Tanasijevic MJ, et al. Improving response to critical laboratory results with automation: results of a randomized controlled trial. J Am Med Inform Assoc. 1999;6:512–22. [DOI] [PMC free article] [PubMed]
- 46.Poon EG, Wang SJ, Gandhi TK, Bates DW, Kuperman GJ. Design and implementation of a comprehensive outpatient Results Manager. J Biomed Inform. 2003;36:80–91. [DOI] [PubMed]
- 47.Berlin L. Using an automated coding and review process to communicate critical radiologic findings: one way to skin a cat. AJR Am J Roentgenol. 2005;185:840–3. [DOI] [PubMed]
- 48.Bordage G. Why did I miss the diagnosis? Some cognitive explanations and educational implications. Acad Med. 1999;74:S138–43. [DOI] [PubMed]
- 49.Smith PC, Raya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA. 2005;293:565–71. [DOI] [PubMed]
- 50.Gearon CJ. Perspectives on the Future of Personal Health Records. Health Records . 2007. 7-17-2007. Available at http://www.chcf.org/documents/chronicdisease/PHRPerspectives.pdf. Accessed 7-12-2007.
- 51.Medical Net Systems, Inc. Medical Net Systems EMR PHR Integration and Other Advance Features; Executive Summary. Medical Net Systems, Inc. 2007. Available at http://www.medicalnetsystems.com/index/EMR_PHR_Integration. Accessed 7-12-2007.
- 52.Rind DM, Safran C, Phillips RS, et al. Effect of computer-based alerts on the treatment and outcomes of hospitalized patients. Arch Intern Med. 1994;154:1511–7. [DOI] [PubMed]
- 53.Choksi V, Marn C, Piotrowski M, Bell Y, Carlos R. Illustrating the root cause analysis process: creation of safety net with a semi-automated process for notification of critical findings in diagnostic imaging. J Am Coll Radiol. 2005;2:768–76. [DOI] [PubMed]
- 54.Wahls T, Haugen T, Cowell K, Becker B. Assessing diagnostic test result managment in a VA health care network. Fed Pract. 2006;23:23–42.
- 55.Sung S, Forman-Hoffman V, Wilson MC, Cram P. Direct reporting of laboratory test results to patients by mail to enhance patient safety. J Gen Intern Med. 2006;21:1075–8. [DOI] [PMC free article] [PubMed]
- 56.Poon EG, Kuperman GJ, Fiskio J, Bates DW. Real-time notification of laboratory data requested by users through alphanumeric pagers. J Am Med Inform Assoc. 2002;9:217–22. [DOI] [PMC free article] [PubMed]
- 57.Weiner M, Biondich P. The influence of information technology on patient–physician relationships. J Gen Intern Med. 2006;21(Suppl 1):S35–9. [DOI] [PMC free article] [PubMed]
- 58.Leong SL, Gingrich D, Lewis PR, Mauger DT, George JH. Enhancing doctor–patient communication using email: a pilot study. J Am Board Fam Pract. 2005;18:180–8. [DOI] [PubMed]
- 59.Mandl KD, Kohane IS, Brandt AM. Electronic patient–physician communication: problems and promise. Ann Intern Med. 1998;129:495–500. [DOI] [PubMed]
- 60.Sittig DF, King S, Hazlehurst BL. A survey of patient–provider e-mail communication: what do patients think? International Journal of Medical Informatics. 2001;61:71–80. [DOI] [PubMed]
- 61.Baker LP, Wagner THP, Singer SM, Bundorf MK. Use of the internet and e-mail for health care information: results from a national survey. (Article). JAMA. 2003;289:2400–6. [DOI] [PubMed]
- 62.Brooks GR, Menachemi N. Physicians’ use of email with patients: factors influencing electronic communication and adherence to best practices. J Med Internet Res. 2006;8:e2. [DOI] [PMC free article] [PubMed]
- 63.Moyer CA, Stern DT, Dobias KS, Cox DT, Katz SJ. Bridging the electronic divide: patient and provider perspectives on e-mail communication in primary care. Am J Manag Care. 2002;8:427–33. [PubMed]
- 64.Slack WV. A 67-year-old man who e-mails his physician. JAMA. 2004;292:2255–61. [DOI] [PubMed]
- 65.Naik AD, Schulman-Green D, McCorkle R, Bradley EH, Bogardus ST. Will older persons and their clinicians use a shared decision-making instrument? J Gen Intern Med. 2005;20:640–3. [DOI] [PMC free article] [PubMed]
- 66.Schulman-Green DJ, Naik AD, Bradley EH, McCorkle R, Bogardus ST. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Educ Couns. 2006;63:145–51. [DOI] [PMC free article] [PubMed]
- 67.Esquivel A, Meric-Bernstam F, Bernstam EV. Accuracy and self correction of information received from an internet breast cancer list: content analysis. BMJ. 2006;332:939–42. [DOI] [PMC free article] [PubMed]
- 68.Heisler M, Piette JD. "I help you, and you help me": facilitated telephone peer support among patients with diabetes. Diabetes Educ. 2005;31:869–79. [DOI] [PubMed]
- 69.Heisler M, Halasyamani L, Resnicow K, et al. “I am not alone”: the feasibility and acceptability of interactive voice response-facilitated telephone peer support among older adults with heart failure. Congest Heart Fail. 2007;13:149–57. [DOI] [PubMed]


