Abstract
Aim
To determine if atypical antipsychotic agents reduce the rehospitalization rates of patients with newly diagnosed or chronic schizophrenia in comparison with typical antipsychotic drugs.
Methods
From January 1, 2003, to December 31, 2004, we retrospectively compared two-year rehospitalization rates of 135 patients with newly diagnosed schizophrenia and 398 patients with chronic schizophrenia (62% and 65% men, respectively), who were initially discharged from Vrapče Psychiatric Hospital, Zagreb, with the prescription of atypical (olanzapine, risperidone or clozapine) or typical (haloperidol or fluphenazine) antipsychotic treatment between January 1, 2002 and December 31, 2002. Time-to-readmission was determined with Kaplan-Meier formula for survival analysis.
Results
In the two-year follow-up, 52 (39%) newly diagnosed patients and 197 (47%) patients with chronic schizophrenia were rehospitalized. No significant differences in time-to-rehospitalization were observed with respect to the type of medications in patients with newly diagnosed schizophrenia (P = 0.378) or patients with chronic schizophrenia (P = 0.531).
Conclusions
Rehospitalization rates of patients who were prescribed atypical antipsychotic drugs were similar to those of patients who were prescribed typical antipsychotic drugs for both the group with the first psychotic episode and group with chronic schizophrenia.
Although antipsychotic agents have been in use for the treatment of schizophrenia for over 50 years, the individual patient outcome is still far from satisfactory. In most patients, schizophrenia has a chronic course characterized by frequent relapses, ie, exacerbation of psychotic symptoms and the need for rehospitalization (1-3).
Relapse prevention seems to be crucial for a beneficial long-term outcome. Successive relapses have a negative impact on duration of illness and the level of remission, causing higher degree of disability and refractoriness to treatment (4). Relapse could be defined as worsening of psychotic symptoms and behavior that puts the patients or their environment at risk of serious damage or even death. Although not ideal, the time between two hospitalizations is the most frequently used measure of relapse rate (5-8).
Antipsychotic drugs can prevent relapse in individuals with schizophrenia. Relapse prevention strongly depends on patient compliance, which may be reduced due to unpleasant side effects of antipsychotic drugs (9). Typical antipsychotic drugs often cause extrapyramidal side effects, such as dystonic reactions, akathisia, and persistent pseudoparkinsonism. Atypical antipsychotic medications, on the other hand, often lead to weight gain, glucose intolerance, hyperlipidemia, serious hematological disturbances, prolongation of QT interval, and stroke in older patients (10,11).
Previous research has shown that atypical antipsychotic drugs directly reduce the rate of rehospitalization (12-17). Given that hospitalization costs make a large part of the overall cost of schizophrenia treatment (18), reduction in hospitalization rates would considerably decrease the overall costs of the treatment (19).
As new antipsychotic agents enter the market, it is important to compare their benefits with those of typical antipsychotic medications (20-22). In Croatia, all typical antipsychotic drugs and clozapine had become available before 1995. Risperidone became available in 1994 and olanzapine in 1996. A preliminary analysis performed for our in-house needs showed that the number of hospitalized schizophrenic patients in our hospital has decreased by 8.4% since the introduction of atypical antipsychotic drugs in 1995. Several studies have shown lower rehospitalization rates of patients with schizophrenia who take atypical antipsychotic drugs (12-17). On the other hand, Patel et al (23) found lower rehospitalization rates of patients who received typical antipsychotic drugs. Other studies found no differences in rehospitalization rates between patients prescribed atypical and typical antipsychotic drugs (5,7). However, in most of these studies the patients were not followed-up for more than a year and the effects of antipsychotic drugs on rehospitalization rates after the first year of treatment were not investigated.
The aim of our study was to determine if atypical antipsychotic agents, ie, olanzapine, risperidone, or clozapine, reduce the rehospitalization rates of patients with newly diagnosed or chronic schizophrenia in comparison with typical antipsychotic drugs, ie, haloperidol or fluphenazine.
Patients and methods
Design and setting
From January 1, 2003 to December 31, 2004 we retrospectively determined rehospitalization rate in patients with schizophrenia who were discharged from Vrapče Psychiatric Hospital, Zagreb, in 2002.
Patient data were collected from Vrapče Psychiatric Hospital database of medical records. The hospital serves a greater part of the city of Zagreb and the surrounding area, as well as other parts of the country. It admits around 7000 patients a year and has a complete patient database. To identify the patients who were possibly rehospitalized over the two-year follow-up period in health care institutions other than Vrapče Psychiatric Hospital, we searched the National Register for Psychoses. The Register is maintained by the Croatian National Institute of Public Health and contains records of all hospital admissions of patients with psychotic disorders to any health care institution with mental health service in Croatia.
Patients
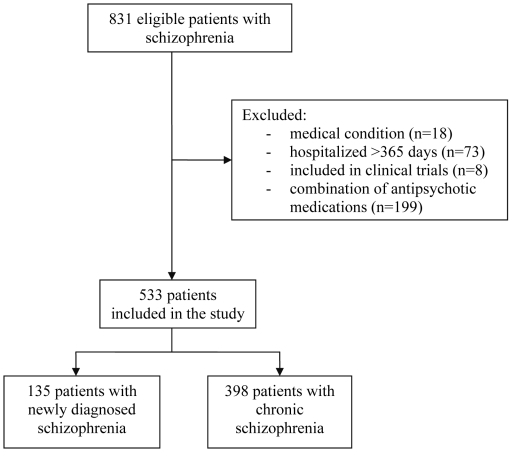
To be included in the study, patients had to be between 18 and 65 years old, discharged from the hospital between January 1 and December 31, 2002, with the diagnosis of schizophrenia (newly diagnosed or chronic) and prescribed atypical (olanzapine, risperidone or clozapine) or typical (haloperidol or fluphenazine) antipsychotic treatment. In our study we divided new and chronic schizophrenic patients. Diagnosis of schizophrenia was established by licensed psychiatrists according to international classification manuals, International Classification of Diseases – version 10 and Diagnostic and Diagnostic and Statistical Manual of Mental Disorders – 4th edition (24,25). In our research we did not separate the patients according to subtype of schizophrenia. Antipsychotic medication was prescribed by psychiatrists on the ward according to clinical presentation of patients. Of 831 patients who met these criteria, we excluded those who were transferred to another hospital due to a general medical condition (n = 18), those who were hospitalized for more than 365 days (n = 73), and those included in randomized controlled trials (n = 8). We also excluded the patients who were taking a combination of antipsychotic drugs (n = 199). The remaining 533 patients (192 women and 341 men) were included in the analysis and divided in two groups, one consisting of 135 patients with newly diagnosed schizophrenia and the other consisting of 398 patients with chronic schizophrenia (Figure 1).
Figure 1.
Flow diagram of patients with schizophrenia discharged from Vrapče Psychiatric Hospital between January 1 and December 31, 2002.
Data collection
Data on sex, age, age at illness onset, duration of hospitalization in 2002, number of previous hospitalizations, and antipsychotic dose at discharge were collected from the hospital medical records. Time-to-rehospitalization was measured as the time from the initial discharge in 2002 to the admittance to either our hospital or some other psychiatric facility during the 2003-2004 follow-up period. Data on rehospitalization of patients admitted to some psychiatric institution other than Vrapče Psychiatric Hospital during the study period were obtained from the National Register of Psychoses.
All patients included in the study were prescribed medical treatment after being discharged from the hospital and were not provided any additional special care or therapy. Rehospitalizations of these patient were followed up for 2 years, ie, from January 1, 2003 to December 31, 2004.
The Ethical Committee of the hospital approved the conduct of the study, in accordance with the 1964 Helsinki declaration.
Statistical analysis
Standard descriptive statistics was used to describe the demographic and clinical characteristics of the patients. Frequency tables were calculated for categorical variables. Since continuous data were not normally distributed, medians with interquartile ranges were calculated for age, age at illness onset, number of hospitalizations, duration of hospitalization, time to rehospitalization, and the dose of antipsychotic medication. Differences in proportion of men and women between the study groups were compared with the Mantel-Haenszel test χ2 test. Differences in continuous variables between the study groups were assessed with the Man-Whitney U test or Kruskal-Wallis Anova, as appropriate. To measure the time to readmission, we used the survival analysis. Survival curves were estimated by the product-limit (Kaplan-Meier) formula. The significance of differences between groups was measured by the multiple-sample test (multiple groups) and the Cox F-Test (two groups). Cox regression model was used to evaluate the impact of age, number of hospitalizations, and the duration of the previous hospitalization on survival curves. All statistical tests were two-tailed, and P<0.05 was considered significant. All tabulations and statistical analysis were performed with Statistica, version 5.5 for Windows (StatSoft Inc. Tulsa, OK, USA).
Results
In the group patients with newly diagnosed schizophrenia, 72 were on typical and 63 were on atypical antipsychotic medications. In this group, 22% of patients were taking haloperidol, 31% fluphenazine, 19% risperidone, 19% olanzapine, and 10% clozapine (Table 1). Different treatment subgroups significantly differed in their age, age at the onset of schizophrenia, and duration of hospitalization. Younger patients were more often treated with atypical antipsychotic medications, ie, olanzapine or risperidone, than older patients, (Table 1). Patients with earlier onset of schizophrenia were significantly more often prescribed risperidone than fluphenazine. The duration of hospitalization was longest in patients taking olanzapine and shortest in the patients taking fluphenazine (Table 1).
Table 1.
Demographic and clinical characteristics of patients with newly diagnosed schizophrenia discharged from Vrapče Psychiatric Hospital, Zagreb, in 2002
| Characteristics | Total (n = 135) | Treatment groups of antipsychotic drugs |
P* | ||||
|---|---|---|---|---|---|---|---|
| typical |
atypical |
||||||
| haloperidol (n = 30) | fluphenazine (n = 42) | risperidone (n = 25) | olanzapine (n = 25) | clozapine (n = 13) | |||
| No. (%) of men | 82 (61.0) | 19 (63.0) | 26 (62.0) | 16 (64.0) | 11 (44.0) | 10 (77.0) | 0.330 |
| Age (years; median, IQ)† | 31 (23-43) | 36.5 (22-37) | 38 (27-47) | 24 (20-32) | 27 (22-39) | 33 (27-46) | 0.014‡ |
| Age at illness onset (years; median, IQ) | 27 (22-36) | 28 (22-37) | 32.5 (24-41) | 23 (20-28) | 26 (21-34) | 26 (22-29) | 0.007‡ |
| Duration of hospitalization (days; median, IQ) | 33 (18.5-58.5) | 30 (14-60) | 25 (11-39) | 33 (26-60) | 46.5 (27-70) | 40 (29-58) | 0.015‡ |
| Time to rehospitalization (days; median, IQ) | 775 (333-936) | 735 (242-936) | 805 (661-995) | 768 (524-936) | 825 (352-878) | 762 (71-804) | 0.378‡ |
| Dose (mg/d) | 13,5 (6-20) | 7.5 (5-15) | 4 (4-6) | 10 (10-15) | 250 (200-300) | - | |
*Mantel-Haenszel test χ2 test.
†IQ – interquartile (25%-75%) range.
‡Man-Whitney U test.
In the group of patients with chronic schizophrenia, 33% were taking haloperidol, 25% fluphenazine, 17% risperidone, 10% olanzapine, and 15% clozapine (Table 2). In this group, there were significantly more men than women. The patients taking typical antipsychotic medications, ie, haloperidol or fluphenazine, were significantly older than patients taking other antipsychotic drugs. No significant difference was found between the treatment subgroups in the age of onset of schizophrenia or the number of previous hospitalizations (Table 2). The duration of hospitalization was longest for the patients taking olanzapine, and the shortest for the patients taking clozapine.
Table 2.
Demographic and clinical characteristics of patients with chronic schizophrenia discharged from Vrapče Psychiatric Hospital, Zagreb, in 2002
| Characteristics | Total (n = 398) | Treatment groups of antipsychotic drugs | P | ||||
|---|---|---|---|---|---|---|---|
| typical | atypical | ||||||
| haloperidol (n = 130) | fluphenazine (n = 101) | risperidone (n = 67) | olanzapine (n = 40) | clozapine (n = 60) | |||
| No. (%) of men | 259 (65.0) | 101 (78.0) | 58 (57.0) | 43 (64.0) | 21 (53.0) | 36 (60.0) | 0.004* |
| Age (years; median, IQ)† | 42 (35-49) | 44 (38-50) | 44 (38-51) | 38 (30-45) | 36 (28.5-44.0) | 40 (33.5-47.5) | <0.001‡ |
| Age at illness onset (years; median, IQ) | 27 (24-33) | 27 (24-34) | 28 (24-32) | 30 (22-34) | 28 (23.5-32) | 26 (23.5-31) | 0.688‡ |
| No. of hospitalizations (median, IQ) | 6 (3-10) | 6 (3-10) | 7 (3-11) | 5 (3-7) | 4.5 (3-8) | 6 (4-10) | 0.103‡ |
| Duration of hospitalization (days; median, IQ) | 43 (23-69) | 46 (26-80) | 36 (21-59) | 38.5 (17-54) | 59.5 (43.5-96.5) | 35 (24.0-68.5) | 0.001‡ |
| Time to rehospitalization (days; median, IQ) | 410 (147-820) | 485.5 (2-1083) | 334 (157-820) | 594 (194-794) | 424 (16-1083) | 456.5 (116.0-843.5) | 0.531‡ |
| Dose (mg/d; median, IQ) | 20 (15-30) | 7.5 (5-15) | 4 (3-6) | 15 (10.0-17.5) | 200 (150-300) | - | |
*M-L χ2 test.
†IQ – interquartile (25%-75%) range.
‡Man-Whitney U test.
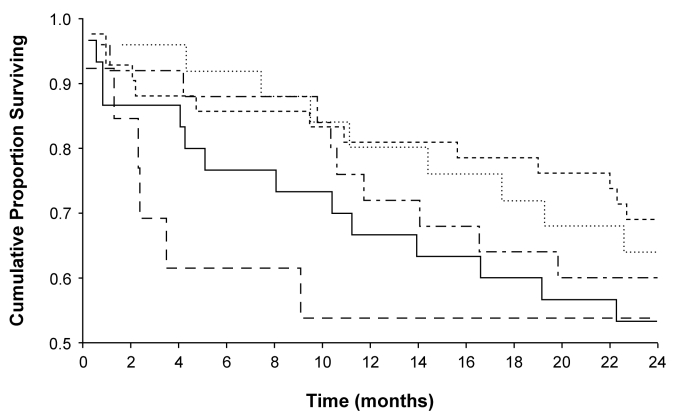
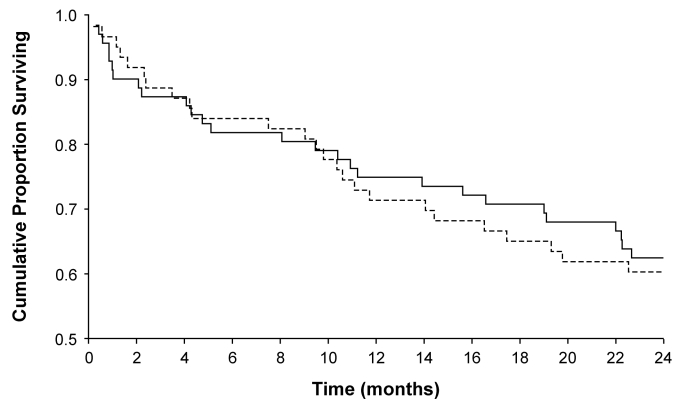
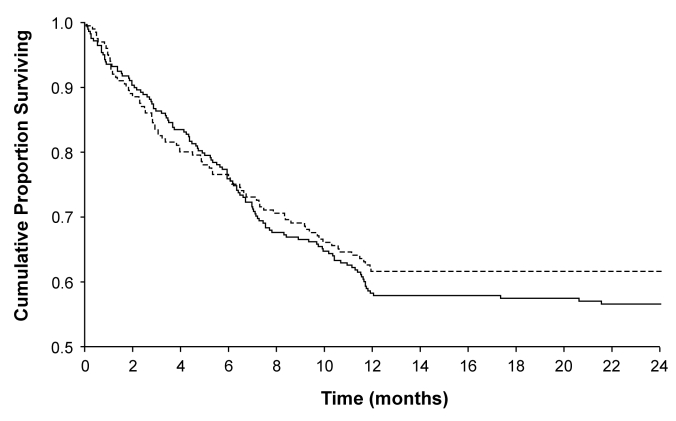
Of 135 patients who were newly diagnosed with schizophrenia, 36 (27%) were rehospitalized in the first year and 52 (39%) in the second year of follow-up. There were 27 of 72 patients taking typical antipsychotic medications and 25 of 63 patients taking atypical antipsychotic medications who were rehospitalized in the two-year period. Of these 52 patients, 14 were taking haloperidol, 13 fluphenazine, 9 risperidone, 10 olanzapine, and 6 clozapine. The patients on clozapine were rehospitalized more often than other groups during the first year of follow-up, but after two years no significant difference in the rehospitalization rate was found among different treatment groups of patients newly diagnosed with schizophrenia (Figure 2). During the first year of follow-up, patients on atypical antipsychotic medications were rehospitalized less often than patients on typical antipsychotic medications, but during the second year of follow-up, this difference disappeared (Figure 3). The longest period between discharge and first rehospitalization was found in the patients taking olanzapine, and the shortest in the patients taking haloperidol, but the difference between them was not significant (Table 1).
Figure 2.
Time to rehospitalization of patients with newly diagnosed schizophrenia who were discharged on typical antipsychotic drugs fluphenazine (dashed line) or haloperidol (full line), or atypical antipsychotic drugs risperidone (dotted line), olanzapine (short-/long-dashed line), or clozapine (long-dashed line).
Figure 3.
Time to rehospitalization of patients with newly diagnosed schizophrenia discharged on typical (full line) or atypical antipsychotic medications (dashed line).
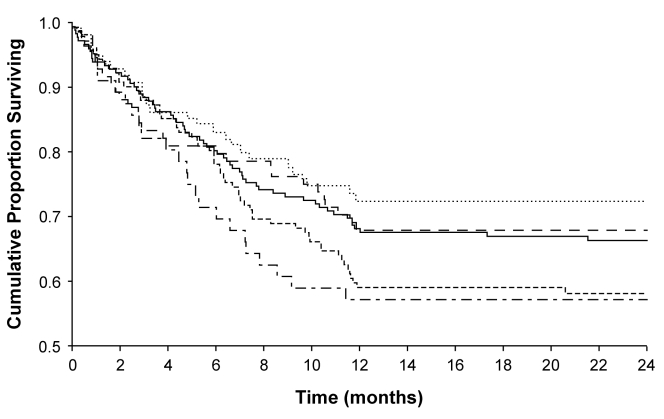
Of 389 patients with chronic schizophrenia, 193 (48%) were rehospitalized during the first year of follow-up. By the end of the second year of follow-up, the number of rehospitalized patients increased only by 4. Of 197 (49%) patients rehospitalized during the follow-up, 61 (31%) were taking haloperidol, 59 (31%) fluphenazine, 26 (13%) risperidone, 24 (12%) olanzapine, and 27 (14%) clozapine. The proportion of rehospitalized patients in each treatment group was not significantly different during the first year of follow-up and there were no changes in the rehospitalization rate in the second year of follow-up (Figure 4). By the end of the two-year follow-up period, 120 (61%) patients taking typical antipsychotic drugs (haloperidol or fluphenazine) and 77 (39%) patients taking atypical antipsychotics (risperidone, olanzapine or clozapine) were rehospitalized (Figure 5). Among the patients with chronic schizophrenia, the longest period to first rehospitalization was found in patients on risperidone and the shortest in patients on fluphenazine, but again the difference was not significant (Table 2).
Figure 4.
Time to rehospitalization of patients with chronic schizophrenia who were discharged on typical antipsychotic drugs fluphenazine (dashed line) or haloperidol (full line), or atypical antipsychotic drugs risperidone (dotted line), olanzapine (short-/long-dashed line), or clozapine (long-dashed line).
Figure 5.
Time to rehospitalization of patients with chronic schizophrenia who were discharged on typical antipsychotic medications (full line) or atypical antipsychotic medications (dashed line).
Discussion
We found no differences in the two-year rehospitalization rates between the patients who were taking atypical or typical antipsychotic agents either in the group with newly diagnosed or in the group with chronic schizophrenia. No differences were found between the treatment groups of newly diagnosed schizophrenic patients in any of the demographic and clinical characteristics, except for duration of hospitalization, which was longest in the patients taking atypical antipsychotic olanzapine. In our clinical practice, the first acute psychotic episode is initially treated with a typical antipsychotic drug and later on replaced by a new atypical antipsychotic drug, such as olanzapine. Thus, there is a possibility that patients on olanzapine were first administered typical antipsychotic drugs, which prolonged the duration of hospitalization. The duration of hospitalization was also significantly longer in chronically ill schizophrenic patients taking olanzapine than in those taking other antipsychotic drugs.
In most studies investigating rehospitalization rates of schizophrenic patients on different antipsychotic drugs, the follow-up period did not last longer than a year (5,7,15,17,23). In our opinion, one-year follow-up may not be long enough to show a possible long-term reduction in rehospitalization rates. A follow-up period of at least two years may be necessary to clearly demonstrate the impact of atypical and typical antipsychotic drugs on rehospitalization rates (26).
We did not find any significant difference in the rehospitalization rates between different treatment groups of patients newly diagnosed with schizophrenia, but we noticed that patients on clozapine were rehospitalized more often than other treatment groups during the first year of follow-up. Clozapine, according to the clinical guidelines (27), is not the medication of choice for the first psychotic episode. However, clozapine was administered to some of our patients with newly diagnosed schizophrenia, most probably due to refractoriness to treatment. These patients were also rehospitalized more often probably due to more severe symptoms.
In our study, atypical antipsychotic drugs were significantly superior to typical antipsychotic medications in the first year of follow-up with respect to rehospitalization rate, but this difference disappeared during the second year of follow-up period. This finding is contrary to the results obtained by Patel et al (23), who found typical antipsychotic medications to be superior to atypical ones over the first year of follow-up with respect to rehospitalization rate. However, they did not analyze patients with newly diagnosed shizophrenia separately from patients with chronic schizophrenia.
In patients with chronic schizophrenia in our study, two-thirds were men. Most men with chronic schizophrenia were on haloperidol; the youngest patients were on olanzapine. This is in line with the trend in our clinical practice that expensive atypical antipsychotic drugs are more often prescribed to younger patients, whereas cheaper antipsychotic drugs, such as haloperidol, are more often prescribed to older patients and men. The duration of hospitalization was longest for chronically ill patients on olanzapine and shortest for patients on clozapine. Clozapine was the medication of choice for chronic and refractory cases of schizophrenia, so these patients probably achieved remission sooner and were therefore discharged earlier from the hospital. There is a possibility that they were on clozapine even before hospitalization, but were hospitalized because they stopped taking the medication, received the same treatment, and achieved remission sooner, with earlier discharge from the hospital.
All treatment groups of patients with chronic schizophrenia reached the plateau after one year of follow-up, and the number of rehospitalized patients in each treatment group did not change significantly over the second year of follow-up. More precisely, 48% of patients with chronic schizophrenia were rehospitalized by the end of the first year of follow-up and 49% by the end of the second year. Most patients who were not rehospitalized during the first year of follow-up were not rehospitalized during the second year of follow-up either. Although the possible reasons for rehospitalization during the first year of follow-up remain to be determined, we may speculate that they include poor compliance, inadequate choice of drug, side effects, comorbidity (eg, addiction), and lack of family support. We noticed that, after the first 8 months, the number of rehospitalized patients taking clozapine did not change until the end of the two-year follow-up. In clinical practice, 6-8 months is an optimal period to see if clozapine is an effective therapy (27-29).
We did not find significant differences in the rehospitalization rates of patients taking atypical or typical antipsychotic drugs over the two-year follow-up, which is in accordance with the findings reported by Lin et al (7) and Rabinowitz et al (17).
The novel aspect of our study is that patients with newly diagnosed schizophrenia were analyzed separately from patients with chronic schizophrenia. Previous studies analyzed either patients diagnosed with schizophrenia all together or only those with either newly diagnosed or chronic schizophrenia. We believe that the patients with the first psychotic decompensation and patients with multiple psychotic decompensations respond differently to treatment and that their time to rehospitalization differs. Our finding that the proportion of patients with chronic schizophrenia rehospitalized during the first year was the same as the proportion rehospitalized during the second year of follow-up is in accordance with previous studies (17,30). On the other hand, fewer patients with newly diagnosed than with chronic schizophrenia were rehospitalized in the first and the second year of follow-up in our study, which implies a better prognosis and longer remission, ie, time to rehospitalization. The first year rehospitalization rate of patients with newly diagnosed schizophrenia was lower than that reported by Strasser et al (5).
Our study has several limitations. The first limitation is inherent to the retrospective study design, ie, the patients were not randomly assigned to the treatments. Second, the comparison involved clozapine, which is a drug reserved for the treatment of refractory schizophrenia. Third, discharge from the hospital does not necessarily imply that the patient continued to take the prescribed drug in the outpatient setting. And fourthly, we did not evaluate the duration of treatment with antipsychotic drugs before discharge from the hospital. However, we had access to outpatient prescription records for most of the patients and, given the sample size and relatively high degree of completeness of data, we may consider our conclusions reliable.
In conclusion, we observed no significant differences in time-to-rehospitalization between different treatment groups during the two-year follow-up either in patients with newly diagnosed or chronic schizophrenia. The rehospitalization rates with atypical antipsychotic drugs were similar to those with typical antipsychotic drugs for both the patients with newly diagnosed schizophrenia and patients with chronic schizophrenia, which indicates that the beneficial properties of modern atypical antipsychotic drugs have less favorable effects on rehospitalization rates than expected.
Future research should focus on other factors possibly associated with rehospitalization and choice of antipsychotic therapy, such as clinical presentation at baseline and intensity of illness, type of symptoms, presence of comorbidity, treatment adherence, history of previous trauma, and reasons for readmission.
Acknowledgment
The authors did not receive any financial support from commercial sources for the conduct of this study.
References
- 1.Craig TJ, Fennig S, Tanenberg-Karant M, Bromet EJ. Rapid versus delayed readmission in first-admission psychosis: quality indicators for managed care? Ann Clin Psychiatry. 2000;12:233–8. doi: 10.1023/A:1009038627449. [DOI] [PubMed] [Google Scholar]
- 2.Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209–23. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- 3.Ascher-Svanum H, Zhu B, Faries D, Landbloom R, Swartz M, Swanson J. Time to discontinuation of atypical versus typical antipsychotics in the naturalistic treatment of schizophrenia. BMC Psychiatry. 2006;6:8. doi: 10.1186/1471-244X-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muller P, Nerenz H, Schaefer E. The risk of rehospitalisation during therapy with atypical and typical neuroleptics – a contribution to differential indication. Psychiatr Prax. 2002;29:388–91. doi: 10.1055/s-2002-34655. [in German] [DOI] [PubMed] [Google Scholar]
- 5.Strasser O, Schmauss M, Messer T. Rehospitalization rates of newly diagnosed schizophrenic patients on atypical neuroleptic medication. Psychiatr Prax. 2004;31(Suppl 1):S38–40. doi: 10.1055/s-2004-828501. [in German] [DOI] [PubMed] [Google Scholar]
- 6.Dossenbach M, Arango-Davila C, Silva Ibarra H, Landa E, Aguilar J, Caro O, et al. Response and relapse in patients with schizophrenia treated with olanzapine, risperidone, quetiapine, or haloperidol: 12-month follow-up of the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) study. J Clin Psychiatry. 2005;66:1021–30. doi: 10.4088/jcp.v66n0810. [DOI] [PubMed] [Google Scholar]
- 7.Lin CH, Lin SC, Chen MC, Wang SY. Comparison of time to rehospitalization among schizophrenic patients discharged on typical antipsychotics, clozapine or risperidone. J Chin Med Assoc. 2006;69:264–9. doi: 10.1016/S1726-4901(09)70254-0. [DOI] [PubMed] [Google Scholar]
- 8.Moore DB, Kelly DL, Sherr JD, Love RC, Conley RR. Rehospitalization rates for depot antipsychotics and pharmacoeconomic implications: comparison with risperidone. Am J Health Syst Pharm. 1998;55(24) Suppl 4:S17–9. doi: 10.1093/ajhp/55.suppl_4.S17. [DOI] [PubMed] [Google Scholar]
- 9.Novak-Grubic V, Tavcar R. Treatment compliance in first-episode schizophrenia. Psychiatr Serv. 1999;50:970–1. doi: 10.1176/ps.50.7.970. [DOI] [PubMed] [Google Scholar]
- 10.Remington G, Chong SA. Conventional versus novel antipsychotics: changing concepts and clinical implications. J Psychiatry Neurosci. 1999;24:431–41. [PMC free article] [PubMed] [Google Scholar]
- 11.Herceg M. Analysis of hospital use of psychopharmaceuticals in Vrapče Psychiatric Hospital over a 4-year period [in Croatian]. Master’s thesis. Zagreb: Zagreb University School of Medicine; 2003. [Google Scholar]
- 12.Essock SM, Hargreaves WA, Covell NH, Goethe J. Clozapine's effectiveness for patients in state hospitals: results from a randomized trial. Psychopharmacol Bull. 1996;32:683–97. [PubMed] [Google Scholar]
- 13.Dellva MA, Tran P, Tollefson GD, Wentley AL, Beasley CM., Jr Standard olanzapine versus placebo and ineffective-dose olanzapine in the maintenance treatment of schizophrenia. Psychiatr Serv. 1997;48:1571–7. doi: 10.1176/ps.48.12.1571. [DOI] [PubMed] [Google Scholar]
- 14.Tran PV, Dellva MA, Tollefson GD, Wentley AL, Beasley CM., Jr Oral olanzapine versus oral haloperidol in the maintenance treatment of schizophrenia and related psychoses. Br J Psychiatry. 1998;172:499–505. doi: 10.1192/bjp.172.6.499. [DOI] [PubMed] [Google Scholar]
- 15.Conley RR, Love RC, Kelly DL, Bartko JJ. Rehospitalization rates of patients recently discharged on a regimen of risperidone or clozapine. Am J Psychiatry. 1999;156:863–8. doi: 10.1176/ajp.156.6.863. [DOI] [PubMed] [Google Scholar]
- 16.Revicki DA. Pharmacoeconomic studies of atypical antipsychotic drugs for the treatment of schizophrenia. Schizophr Res. 1999;35(Suppl):S101–9. doi: 10.1016/S0920-9964(98)00168-6. [DOI] [PubMed] [Google Scholar]
- 17.Rabinowitz J, Lichtenberg P, Kaplan Z, Mark M, Nahon D, Davidson M. Rehospitalization rates of chronically ill schizophrenic patients discharged on a regimen of risperidone, olanzapine, or conventional antipsychotics. Am J Psychiatry. 2001;158:266–9. doi: 10.1176/appi.ajp.158.2.266. [DOI] [PubMed] [Google Scholar]
- 18.Rice DP, Miller LS. The economic burden of schizophrenia: conceptual and methodological issues, and cost estimates. In: Moscarelli M, Rupp A, Sartorius N, editors. Handbook of mental health economics and health policy. Vol. 1. Schizophrenia. Chichester: John Wiley and Sons; 1996; p. 321-34. [Google Scholar]
- 19.Mojtabai R, Lavelle J, Gibson PJ, Bromet EJ. Atypical antipsychotics in first admission schizophrenia: medication continuation and outcomes. Schizophr Bull. 2003;29:519–30. doi: 10.1093/oxfordjournals.schbul.a007024. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton SH, Revicki DA, Edgell ET, Genduso LA, Tollefson G. Clinical and economic outcomes of olanzapine compared with haloperidol for schizophrenia. Results from a randomised clinical trial. Pharmacoeconomics. 1999;15:469–80. doi: 10.2165/00019053-199915050-00005. [DOI] [PubMed] [Google Scholar]
- 21.Marder SR, Glynn SM, Wirshing WC, Wirshing DA, Ross D, Widmark C, et al. Maintenance treatment of schizophrenia with risperidone or haloperidol: 2-year outcomes. Am J Psychiatry. 2003;160:1405–12. doi: 10.1176/appi.ajp.160.8.1405. [DOI] [PubMed] [Google Scholar]
- 22.Jukic V, Baric V, Culav-Sumic J, Herceg M, Majdancic Z, Werft-Cop M. The impact of novel antipsychotic drugs on quality of life among people suffering from schizophrenia. Coll Antropol. 2003;27(Suppl 1):119–24. [PubMed] [Google Scholar]
- 23.Patel NC, Dorson PG, Edwards N, Mendelson S, Crismon ML. One-year rehospitalization rates of patients discharged on atypical versus conventional antipsychotics. Psychiatr Serv. 2002;53:891–3. doi: 10.1176/appi.ps.53.7.891. [DOI] [PubMed] [Google Scholar]
- 24.International classification of diseases and related health problems, 10th revision. Geneva: World Health Organization: 1992. [Google Scholar]
- 25.Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): American Psychiatric Association; 1994. [Google Scholar]
- 26.Honigfeld G, Patin J. A two-year clinical and economic follow-up of patients on clozapine. Hosp Community Psychiatry. 1990;41:882–5. doi: 10.1176/ps.41.8.882. [DOI] [PubMed] [Google Scholar]
- 27.Wahlbeck K, Cheine M, Essali A, Adams C. Evidence of clozapine's effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry. 1999;156:990–9. doi: 10.1176/ajp.156.7.990. [DOI] [PubMed] [Google Scholar]
- 28.Chakos M, Lieberman J, Hoffman E, Bradford D, Sheitman B. Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: a review and meta-analysis of randomized trials. Am J Psychiatry. 2001;158:518–26. doi: 10.1176/appi.ajp.158.4.518. [DOI] [PubMed] [Google Scholar]
- 29.Lindstrom LH. A retrospective study on the long-term efficacy of clozapine in 96 schizophrenic and schizoaffective patients during a 13-year period. Psychopharmacology (Berl) 1989;99(Suppl):S84–6. doi: 10.1007/BF00442567. [DOI] [PubMed] [Google Scholar]
- 30.Weiden P, Aquila R, Standard J. Atypical antipsychotic drugs and long-term outcome in schizophrenia. J Clin Psychiatry. 1996;57(Suppl 11):53–60. [PubMed] [Google Scholar]