Abstract
Uracil–Tegafur (UFT), an oral fluorinated pyrimidine chemotherapeutic agent, has been used for adjuvant chemotherapy in curatively resected colorectal cancer patients. Past trials and meta-analyses indicate that it is somewhat effective in extending survival of patients with rectal cancer. The objective of this study was to perform a reappraisal of randomised clinical trials conducted in this field. We designed an individual patient-based meta-analysis of relevant clinical trials to examine the benefit of UFT for curatively resected rectal cancer in terms of overall survival (OS), disease-free survival (DFS), and local relapse-free survival (LRFS). We analysed individual patient data of five adjuvant therapy randomised clinical trials for rectal cancer, which met the predetermined inclusion criteria. These five trials had a combined total of 2091 patients, UFT as adjuvant chemotherapy compared to surgery-alone, 5-year follow-up, intention-to-treat-based analytic strategy, and similar endpoints (OS and DFS). In a pooled analysis, UFT had significant advantage over surgery-alone in terms of both OS (hazard ratio, 0.82; 95% confidence interval (CI), 0.70–0.97; P=0.02) and DFS (hazard ratio, 0.73; 95%CI, 0.63–0.84; P<0.0001). This individual patient-based meta-analysis demonstrated that oral UFT significantly improves both OS and DFS in patients with curatively resected rectal cancer.
Keywords: rectal cancer, UFT, adjuvant chemotherapy, randomised clinical trials, individual patient data meta-analysis
Colorectal cancer accounts for 10–15% of all cancers and is the second leading cause of cancer deaths in developed countries (Pisani et al, 1993). In Japan alone, nearly 56 000 new cases are diagnosed and this disease causes 36 000 deaths every year (Statistics and information department, Ministry of Health and Welfare, 1996). Surgical treatment is the primary management of colorectal cancers, with 75–80% of the patients being operable at the time of diagnosis (Boring et al, 1991; Vernaba et al, 1994). However, even if a curative resection is performed, those patients with regional lymph node involvement (Dukes' C, Stage III) have a 40–50% 5-year survival rate.
Recently, in the field of Stage III colon cancer treatment, adjuvant chemotherapy by 5-fluorouracil (5-FU)/levamisole was proved to be superior to surgery-alone therapy, and then various 5-FU/leucovorin (LV) regimens were confirmed to be effective from the results of numerous large-scale randomised trials and from the pooled analysis of clinical trials (Wolmark et al, 1993; International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators, 1995; O'Connell et al, 1997). In 2004, results from the Multicenter International Study of Oxaliplatin/5-FU/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) trial demonstrated that combination chemotherapy with 5-FU/LV (de Gramont regimen) plus oxaliplatin was significantly superior to 5-FU/LV alone (André et al, 2004). With regard to adjuvant chemotherapy for colon cancer, therefore, solid evidence has been accumulated from relevant clinical trials, and steady evolution of the new treatment modalities has been achieved.
However, the situation is still uncertain focusing on adjuvant therapy for rectal cancer. Despite apparently curative surgery, rectal cancer recurs in more than 55% of the patients, including local recurrence rates of 25% (Vernaba et al, 1994). Despite the recommendation of the consensus conference by the National Institute of Health (NIH consensus conference, 1990) that concluded that adjuvant radiotherapy and chemotherapy should be given to all patients with locally advanced rectal cancer, recent findings by a large-scale randomised trial and meta-analysis have failed to prove significant benefit of radiotherapy for survival (Fisher et al, 1988; Vernaba et al, 1994). In this regard, the quest for an effective adjuvant treatment with a robust advantage on the outcome of resected rectal cancer remain an important task for gastrointestinal oncologists.
In Japan, mesorectal excision is standard surgical procedure. Radiotherapy is not routinely performed as adjuvant therapy.
In Japan, adjuvant therapy after resection of colorectal cancer was developed primarily using oral fluorinated pyrimidines (O-FPs). A meta-analysis of three old trials (Sakamoto et al, 1999) and a more sophisticated analysis of four recent pivotal randomised trials (Sakamoto et al, 2004) demonstrated a statistically significant benefit of O-FPs on the outcome of colorectal cancers over surgery alone. However, the survival benefit shown in that meta-analysis was more pronounced in colon cancers. The risk reduction in terms of rectal cancer was only 8% and the result of those previous meta-analyses that analysed various types of oral fluorinated pyrimidine clinical trials was not sufficient to show a significant effect on survival.
Uracil–tegafur (UFT) is one of the O-FPs. In colon cancer, the majority of recurrences occurred in the liver, whereas in rectal cancer many recurrences occurred in the lung and locally in addition to the liver. Treatment effect may thus differ between colon cancer and rectal cancer. As the previous meta-analysis, two trials of UFT in patients with rectal cancer have been reported. The present study focused on rectal cancer, which lacked a clear-cut survival benefit in our previous meta-analysis. Unlike oral fluoropyrimidines such as carmofur and capecitabine, the formulation of UFT includes a dihydropyrimidine dehydrogenase inhibitor (Diasio, 1999), designed to enhance the bioavailability of FU. This combination of uracil and tegafur was shown, in an animal tumour system, to increase the anti-tumour activity compared with tegafur alone (Ooi et al, 2001). UFT also produced an enhanced intratumoural concentration of fluorinated pyrimidine, 5–10 times greater than that achieved with Tegafur alone (Fukunaga et al, 1987). Preclinical studies established that the optimal molar ratio of uracil to Tegafur is 4 : 1, which resulted in the highest 5-FU tumour: blood and tumour: normal tissue partition coefficients (Kawaguchi et al, 1980). UFT has now been clinically tested for lung cancer (Kato et al, 2004), breast cancer (Noguchi et al, 2005), and for gastric cancer (Kinoshita et al, 2005) in an adjuvant setting in Japan. Recently, UFT has also been tested in Western countries, regarding its efficacy for both advanced and curatively resected colon cancer (Carmichael et al, 2002; Douillard et al, 2002; Lembersky et al, 2006).
Here, we present an individual patient data meta-analysis of five centrally randomised trials recently performed in Japan to compare rectal cancer patients treated with UFT, with the surgery-alone control group. This meta-analysis includes data from more than 2000 patients and therefore provides a more reliable assessment of the effect of UFT on the survival, disease-free survival (DFS), and local relapse-free survival (LRFS) of the patients with rectal cancer than is available from any of the individual studies.
PATIENTS AND METHODS
Selection of trials
Trials that randomly assigned patients to either long-term (12 months) administration of UFT or surgery-alone treatment after curative resection of rectal cancer were eligible for meta-analysis. The randomisation technique used in these trials was the centralised randomisation that precluded the possibility of prior knowledge of the treatment to be allocated.
Five relevant trials identified as Japanese Foundation for Multidisciplinary Treatment of Cancer (JFMC) 7-1 (Kodaira et al, 1998), JFMC15-1, JFMC15-2 (Watanabe et al, 2004), Tokai Adjuvant Chemotherapy Study Group for Colorectal Cancer (TAC–CR) (Kato et al, 2002), and National Surgical Adjuvant Study of Colorectal Cancer (NSAS-CC) (Akasu et al, 2006) were included in the meta-analysis involving a total of 2091 patients. In trials JFMC7-1, JFMC15-1, and JFMC 15-2, patients who were randomly assigned to the experimental group received intravenous mitomycin C (6 mg m−2) at 1 week and once monthly for 6 months. In the JFMC15-1 and 15-2 trials, patients who were randomly assigned to the experimental group additionally received an induction course of intravenous 5-FU (250 mg daily−1) during 7 postoperative days (Table 1).
Table 1. Details of the randomized controlled trials included in the individual patient data meta-analysis.
| Category | JFMC7-1 | JFMC15-1 | JFMC15-2 | TAC-CR | NSAS-CC | Total |
|---|---|---|---|---|---|---|
| Additional chemotherapy | Mitomycin C | Mitomycin C+FU IV | Mitomycin C+FU IV | None | None | — |
| Radiotherapy | None | None | None | None | None | — |
| UFT dose/day | 400 mg | 400 mg | 400 mg | 400 mg | 600 mga | — |
| Period | 12 months | 12 months | 12 months | 24 months | 12 months | — |
| Dates of accrual | 1986–1988 | 1989 | 1990 | 1991–1994 | 1996–2001 | — |
| No. of patients | 834 | 447 | 391 | 143 | 276 | — |
| Duration of accrual, months | 35 | 24 | 24 | 36 | 54 | — |
| Sex, No. of patients (male–female ratio) | ||||||
| Male | 521 (62.4%) | 260 (58.1%) | 244 (62.4%) | 93 (65.0%) | 167 (60.5%) | 1285 (61.4%) |
| Female | 313 (37.6%) | 187 (41.9%) | 147 (37.6%) | 50 (35.0%) | 109 (39.5%) | 806 (38.9%) |
| Duke's stage, No. of patients | ||||||
| A | 135 | 67 | 62 | 12 | 0 | 276 |
| B | 326 | 175 | 139 | 53 | 0 | 693 |
| C | 373 | 205 | 189 | 78 | 276 | 1121 |
| Median age | 57 | 60 | 59 | 62 | 58 | 58 |
| Upper age limit, years | 70 | 75 | 75 | 75 | 75 | — |
JFMC=Japanese Foundation for Multidisciplinary Treatment of Cancer; NSAS-CC=National Surgical Adjuvant Study of Colorectal Cancer; TAC–CR=Tokai Adjuvant Chemotherapy for Colorectal Cancer; UFT=Uracil–Tegafur.
400 mg m−2 day−1 for 5 days every 7 days.
Protocol and data collection for the meta-analysis
In December 2003, a protocol for the meta-analysis, describing the study rationale, statistical methods, and guidelines for publication, was distributed to the principal investigators of the five trials. Investigators were asked to provide individual data for every randomised patient, whether eligible or not, assessable or not, and properly followed up or not. Items requested for every patient were as follows: patient identification, date of surgery, eligibility, allocated treatment by random assignment, age, sex, primary tumour site, Dukes' stage, induction chemotherapy, dates of recurrence, death, or last visit. Disease-free survival was calculated from the date of surgery to the date of recurrence, second primary cancer or death, whichever occurred first. Survival was calculated from the date of surgery to the date of death, regardless of the cause of death. Local relapse-free survival was calculated from the date of surgery to the date of local recurrence. Data from patients with only distant recurrence and those who were died without recurrence were censored. Patients enrolled in these trials had been followed up for 5–7 years. Toxicity data were not collected, because detailed analysis of side effects can be found in the published reports of the individual trials (Kodaira et al, 1998; Kato et al, 2002; Watanabe et al, 2004; Akasu et al, 2006).
All investigators and the Clinical Trial Committee of all the trials agreed to join in the meta-analysis. Individual patient data were received by the independent secretariat by February 2004 and October 2006.
Pretreatment patient characteristics
All 2091 patients had curatively resected rectal cancer without evidence of distant metastasis by diagnostic imaging criteria or by macroscopic examination of the abdominal organs during surgery. Patients with severe postoperative complications were excluded from all trials, as were patients with any previous chemotherapy or radiotherapy or with a synchronous or metachronous second cancer. Median patient age was 61 years at the time of random assignment. The male/female ratio was approximately 3 : 2. Performance status was less than 2 on the Japan Clinical Oncology Group scale for all patients.
Statistical analysis
The method used for the meta-analysis and the format for the presentation of the results have been described in detail elsewhere (Advanced Colorectal Cancer Meta-Analysis Project, 1992). All analyses were based on individual patient data. Treatment effects on DFS, LRFS, and survival were first estimated within each trial and then combined using classical meta-analytic methods (Colorectal Cancer Collaborative Group, 2001). Treatment effects were displayed as hazard ratios. These ratios were estimated by univariate Cox's proportional model as relative risks of having an event in the UFT group as compared with having the same event in the surgery-alone control group. A ratio less than unity indicates benefit from UFT, and this benefit is statistically significant when the 95% confidence interval (CI) of the ratio does not include unity. The overall effect of treatment was assessed through a χ12 d.f. and the heterogeneity between five trials through a χ42 d.f. (Colorectal Cancer Collaborative Group, 2001). Additional analyses were carried out to determine which of the following prognostic features, if any, were predictive of the treatment effect: Dukes' stage (A vs B vs C), sex (male vs female), and age (three groups of increasing age). Tests for interaction were applied to detect departures from the homogeneity of treatment effects. Multivariate analyses were performed with the use of the Cox proportional hazards regression model for DFS, LRFS, and survival to assess the robustness of the observed effects to adjustments for important covariates and the magnitude of interaction between treatment effect and covariate (Advanced Colorectal Cancer Meta-Analysis Project, 1992). All P-values resulted from use of two-sided statistical tests. The significance level was set at 5% for all tests.
RESULTS
Survival
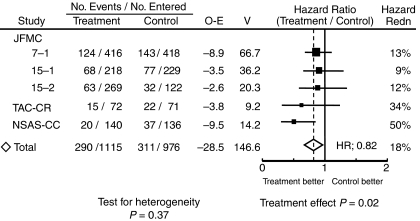
Survival hazard ratios for all the trials are presented in Figure 1. The overall hazard ratio was 0.82 (95% CI, 0.70–0.97; P=0.02) with no significant heterogeneity between the treatment effects in different trials (χ42 for heterogeneity=4.31; P=0.37). UFT showed significant effect on survival of curatively resected rectal cancers with a 5-year survival benefit of approximately 5%.
Figure 1.
Survival hazard ratios by individual trial (Abbreviations: O/N=observed number of events/number of patients; O–E=Observed minus Expected number of events; V=variance of (O–E); Hazard Redn=hazard reduction; SE=standard error of hazard reduction).
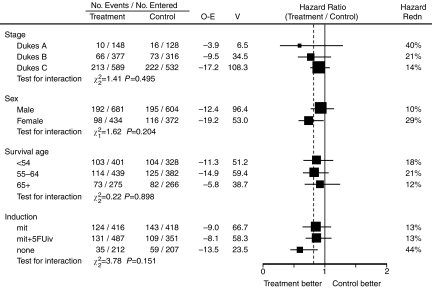
Figure 2 shows the breakdown of the survival hazard ratio stratified by various patient characteristics. There was a slight trend toward larger treatment benefits in earlier Dukes' stages (Hazard ratio; Dukes' A=0.60, Dukes' B=0.79, Dukes' C=0.86) but heterogeneity tests did not show any significant difference (χ22=1.41; P=0.495). There was no statistically significant difference in sex (χ12 for interaction=1.62; P=0.204) or age (χ22 for interaction=0.22; P=0.898).
Figure 2.
Survival hazard ratios by patient and treatment characteristics (Abbreviations as in Figure 1).
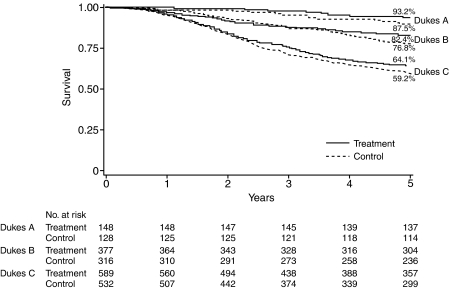
Figure 3 shows survival curves by treatment and disease stage. These curves confirm the hazard ratio analysis shown in Figure 2 and point to favourable effects of UFT in all Dukes' stages.
Figure 3.
Survival curves by tumour stage and by treatment.
Disease-free survival
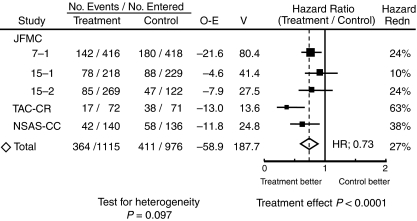
Disease-free survival hazard ratios are presented in Figure 4 for all the trials. These figure show a somewhat larger effect of treatment on DFS than on survival, with an overall DFS ratio of 0.73 (95%CI, 0.63–0.84; P<0.0001) with a 5-year DFS benefit of 9.7%, but demonstrating some heterogeneity among the treatment effects in different trials (χ42 for heterogeneity=7.85; P=0.097). Additionally, random effect model assuming the variation between trials was applied. The results of the random effect model still revealed highly significant differences owing to the relatively high effect in TAC–CR and NSAS-CC trials.
Figure 4.
Disease-free survival hazard ratios by individual trial (Abbreviations as in Figure 1).
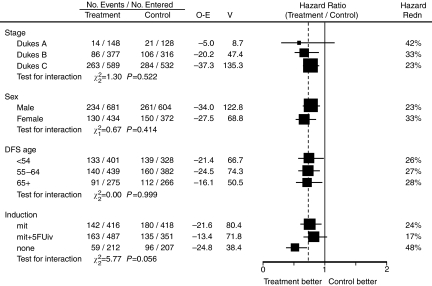
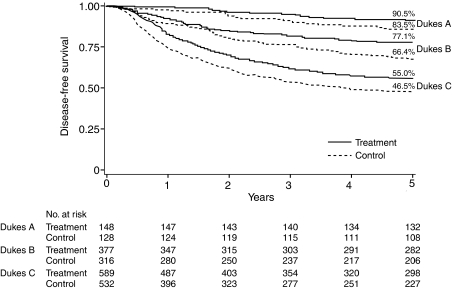
Figure 5 lists the DFS hazard ratios by various patient and treatment characteristics.
Figure 5.
Disease-free survival hazard ratios by patient and treatment characteristics (Abbreviations as in Figure 1).
Figure 6 shows DFS curves by treatment and disease stage. These curves again point to benefits of UFT in Dukes' A, B and C stages. Roughly identical effect extended across all Dukes' stages: the DFS benefits at 5 years in terms of risk reduction were 0.42, 0.33, 0.23.
Figure 6.
Disease-free survival curves by tumour stage and by treatment.
Local relapse free survival
The overall hazard ratio was 0.68 (95%CI, 0.53–0.87; P=0.0026), and demonstrating some heterogeneity among the treatment effects in different trials (χ42 for heterogeneity=8.82; P=0.0658). UFT also showed significant effect on LRFS of curatively resected rectal cancers.
DISCUSSION
Extensive preclinical and clinical research led to the optimisation of 5-FU administration, with 5-FU bolus in combination with LV as standard therapy both in metastatic disease (Advanced Colorectal Cancer Meta-Analysis Project, 1992) and after curative resection of Stage III (Dukes' C) colon cancer (International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators, 1995; O'Connell et al, 1997; Wolmark et al, 1999). However, the toxicity of bolus 5-FU/LV regimen, especially the risk of haematologic toxicity and mucositis, could not have been negligible.
Continuous-infusion 5-FU modulated by LV, utilised mostly in European countries, showed somewhat better efficacy and definitely better tolerance than bolus 5-FU in advanced diseases (de Gramont et al, 1997; Meta-Analysis Group In Cancer, 1998a, 1998b; Schmoll et al, 2000). In the adjuvant setting, one of the continuous regimens (LV5-FU2) was shown to have low toxicity than the bolus regimen, but no difference was shown in terms of survival (André et al, 2003). Recently, combination of continuous 5-FU/LV and oxaliplatin (FOLFOX 4) was demonstrated to have significant effect on DFS, and is now considered as the standard adjuvant regimen for colon cancer in the Western world.
The recent development of O-FPs has therefore opened new perspectives. Oral fluorinated pyrimidines may mimic continuous regimens without its technical inconvenience and deterring patients' quality of life. In patients with advanced colorectal cancer, the efficacy of UFT (typical and most prescribed O-FP) plus oral LV (Carmichael et al, 2002; Douillard et al, 2002) or of capecitabine alone (Hoff et al, 2001; Van Cutsem et al, 2001) seems comparable in terms of the efficacy with significantly less significant severe haematologic toxicities and/or stomatitis. The risk of severe hand-foot syndrome is lower in UFT than with capecitabine, but the risk of severe diarrhoea and other gastrointestinal symptoms is higher in UFT and in UFT/oral LV treatment for Western patients.
In Japan, UFT have been administered for many years especially for patients with curatively resected colorectal cancers. For some unknown reason, severe gastrointestinal toxicities are much less frequent in Japanese patients, and patients usually prefer oral chemotherapy especially in an adjuvant setting (Borner et al, 2002).
Furthermore, with regard to rectal cancer, it is a difficult objective for a clinical trial to accrue enough patients, compared to colon cancer, and despite the fact that several attempts of determining a standard adjuvant treatment for rectal cancer, almost no clinical trial has succeeded in showing a relevant survival benefit of adjuvant treatment, except one with preoperative radiotherapy (Swedish Rectal Cancer Trial, 1997).
In this context, several Japanese groups conducted randomised clinical trials comparing UFT with surgery alone for curatively resected rectal cancers. Five such trials were identified after a meticulous search, and are included in the present meta-analysis. This meta-analysis was restricted to trials that had been randomised centrally and from which no patient had been excluded for any reason. It represents the largest series of properly randomly assigned patients receiving the single oral adjuvant O-FP agent, that is, UFT, for rectal cancer comparing with patients receiving no therapy after curative tumour resection.
This meta-analysis found a statistically significant benefit of UFT with regard to overall survival (OS) (hazard ratio=0.82; P=0.02) as well as DFS (hazard ratio=0.73; P<0.0001), and LRFS (hazard ratio=0.68; P=0.0026). As can seen by comparing the data in Figures 1 and 4, the data from the NSAS-CC and TAC–CR study show benefits that are, apparently, larger than the others. As shown in Table 1, the dosage and duration of treatment with UFT in the NSAS-CC and TAC–CR trials differed from those in the other three trials; the dose intensity of UFT was higher in the former two trials. Several studies have reported that a high-dose intensity of UFT improves survival in patients given postoperative adjuvant chemotherapy for gastric cancer (Sugimachi et al, 1997; Danno et al, 2001). The higher dose intensity of UFT in the NSAS-CC and TAC–CR trials may have influenced the outcomes.
Most of the Japanese rectal cancer patients did not receive pre- or postoperative radiotherapy in any of the trials. Although radiotherapy has been considered one of the standard adjuvant treatments in the Western countries, significant survival benefit has not been shown with reproducibility (Wolmark et al, 2000; Colorectal Cancer Collaborative Group, 2001). The ostensible advantage of adjuvant radiotherapy is to decrease local recurrence of rectal cancers. As compared with postoperative chemoradiotherapy, preoperative chemoradiotherapy does not improve OS, but inhibits local recurrence and reduces toxicity (Sauer et al, 2004). In our study, however, LRFS was also significantly better in the UFT group compared to surgery alone group. As far as our results are concerned, UFT might also be useful in preventing local recurrence in Japanese patients who usually do not receive radiotherapy in an adjuvant setting.
Also, there is still a debate whether adjuvant chemotherapy for early stage rectal cancer is feasible (Buyse and Piedbois, 2001). In terms of numbers needed to treat, these benefits imply that approximately 20 patients need to be treated for one more patient to survive 5 years, and approximately 10 to be treated for one fewer patient to suffer a cancer recurrence within 5 years, regardless of disease stage. Our results show that the therapy is beneficial in Stage II patients not only Stage III patients with nodal involvement (Mamounas et al, 1999; Gray et al, 2004). As for early stage disease, further investigations are needed to assess potential benefits of treatment because events were infrequent and hazard ratios were small.
Regardless of the disease stage and patient background characteristics, there is a need for further trials involving UFT and new agents that are effective in advanced disease, such as irinotecan, oxaliplatin, and monoclonal antibodies.
Acknowledgments
This work is supported in part, by non-profit organization Epidemiological & Clinical Research Information Network (ECRIN), Kyoto University EBM Collaborating Center, and grant-in aid from Japanese Society for Cancer of the Colon and Rectum, from Japanese Society for Strategies of Cancer Therapy, and from Osaka Cancer Foundation. The authors are indebted to Professor J Patrick Barron of the International Medical Communications Center of Tokyo Medical University for his review of this article.
Footnotes
Previous presentation: The 41st annual meeting of American Society of Clinical Oncology, Orlando (Proc Am Soc Clin Oncol 2005; 23: 253s)
References
- Advanced Colorectal Cancer Meta-Analysis Project (1992) Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: evidence in terms of response rate. J Clin Oncol 10: 896–903 [DOI] [PubMed] [Google Scholar]
- Akasu T, Moriya Y, Ohashi Y, Yoshida S, Shirao K, Kodaira S, NSAS-CC Group (2006) Adjuvant chemotherapy with uracil-tegafur for pathological stage III rectal cancer after mesorectal excision with selective lateral pelvic lymphadenectomy: a multicenter randomized controlled trial. Jpn J Clin Oncol 36: 237–244 [DOI] [PubMed] [Google Scholar]
- André T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, Topham C, Zaninelli M, Clingan P, Bridgewater J, Tabah-Fisch I, de Gramont A (2004) Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) Investigators. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350: 2343–2351 [DOI] [PubMed] [Google Scholar]
- André T, Colin P, Louvet C, Gamelin E, Bouche O, Achille E, Colbert N, Boaziz C, Piedbois P, Tubiana-Mathieu N, Boutan-Laroze A, Flesch M, Buyse M, de Gramont A (2003) Bi-monthly regimen of 5-fluorouracil and leucovorin (LV5FU2) as adjuvant therapy in stage II and III colon cancer: 4-year results of a randomised trial. J Clin Oncol 21: 2896–2903 [DOI] [PubMed] [Google Scholar]
- Boring CC, Squires TS, Tong T (1991) Cancer statistics. CA Cancer J Clin 41: 19–51 [DOI] [PubMed] [Google Scholar]
- Borner MM, Schoffski P, de Wit R, Caponigro F, Comella G, Sulkes A, Greim G, Peters GJ, van der Born K, Wanders J, de Boer RF, Martin C, Fumoleau P (2002) Patient preference and pharmacokinetics of oral modulated UFT vs intravenous fluorouracil leucovorin: a randomised crossover trial in advanced colorectal cancer. Eur J Cancer 38: 349–358 [DOI] [PubMed] [Google Scholar]
- Buyse M, Piedbois P (2001) Should Dukes' B patients receive adjuvant chemotherapy? A statistical perspective. Seminars Oncol 28(Suppl 1): 20–24 [DOI] [PubMed] [Google Scholar]
- Carmichael J, Popiela T, Radstone D, Falk S, Borner M, Oza A, Skovsgaard T, Munier S, Martin C (2002) Randomized comparative study of tegafur/uracil and oral leucovorin vs parenteral fluorouracil and leucovorin in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 20: 3617–3627 [DOI] [PubMed] [Google Scholar]
- Colorectal Cancer Collaborative Group (2001) Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients form 22 randomised trials. Lancet 358: 1291–1304 [DOI] [PubMed] [Google Scholar]
- Danno M, Shiroto H, Kunii Y, Ishibiki K, Yamamura Y, Sakamoto Y, Tamura Y, Kunitomo K, Kumashiro R (2001) Study on the intensity of MMC and UFT in postoperative adjuvant chemotherapy for gastric cancer-study report of JFMTC Study No. 10. Jpn J Cancer Chemother 28: 195–203 [PubMed] [Google Scholar]
- de Gramont A, Bosset JF, Milan C, Rougier P, Bouche O, Etienne PL, Morvan F, Louvet C, Guillot T, Francois E, Bedenne L (1997) Randomized trial comparing monthly low-dose leucovorin and fluorouracil bolus with bimonthly high-dose leucovorin and fluorouracil bolus plus continuous infusion for advanced colorectal cancer. J Clin Oncol 15: 808–815 [DOI] [PubMed] [Google Scholar]
- Diasio RB (1999) Clinical implications of dihydropyrimidine dehydrogenase inhibition. Oncology 13: 17–21 [PubMed] [Google Scholar]
- Douillard JY, Hoff PM, Skillings JR, Eisenberg P, Davidson N, Harper P, Vincent MD, Lembersky BC, Thompson S, Maniero A, Benner SE (2002) Multicenter phase III study of uracil/tegafur and oral leucovorin vs fluorouracil and leucovorin in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 20: 3605–3616 [DOI] [PubMed] [Google Scholar]
- Fisher B, Wolmark N, Rockette H, Redmond C, Deutsch M, Wickerham DL, Fisher ER, Caplan R, Jones J, Lerner H, Gordon P, Feldman M, Cruz A, Legault-Poisson S, Wexler M, Lawrence W, Robidoux A, Other NSABP Investigators (1988) Postoperative adjuvant chemotherapy or radiation therapy for rectal cancer: results from NSABP protocol R-01. J Natl Cancer Inst 80: 21–29 [DOI] [PubMed] [Google Scholar]
- Fukunaga H, Katsumi M, Aoki Y, Oka S, Konishi R, Yukawa H, Kawaguchi T, Tamaki Y, Takifuji K (1987) 5-FU concentration in tumor tissue and the antitumor effect in patients with gastric cancer after oral administration of UFT. Jpn J Cancer Chemother 14: 2735–2739 (in Japanese) [PubMed] [Google Scholar]
- Gray RG, Barnwell J, Hills R, McConkey C, Williams N, Kerr D, for the QUASAR Collaborative Group (2004) QUASAR: A randomized study of adjuvant chemotherapy (CT) vs observation including 3238 colorectal cancer patients. Proc Am Soc Clin Oncol 23: 246 (abstr 3501) [Google Scholar]
- Hoff PM, Ansari R, Batist G, Cox J, Kocha W, Kuperminc M, Maroun J, Walde D, Weaver C, Harrison E, Burger HU, Osterwalder B, Wong AO, Wong R (2001) Comparison of oral capecitabine vs intravenous fluorouracil plus leucovorin as first-line treatment in 605 patients with metastatic colorectal cancer: results of a randomized phase III study. J Clin Oncol 19: 2282–2292 [DOI] [PubMed] [Google Scholar]
- International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators (1995) Efficacy of adjuvant fluorouracil and folinic acid in colon cancer. Lancet 345: 939–944 [PubMed] [Google Scholar]
- Kato H, Ichinose Y, Ohta M, Hata E, Tsubota N, Tada H, Watanabe Y, Wada H, Tsuboi M, Hamajima N, Ohta M, Japan Lung Cancer Research Group on Postsurgical Adjuvant Chemotherapy (2004) A randomized trial of adjuvant chemotherapy with uracil-tegafur for adenocarcinoma of the lung. N Engl J Med 350: 1713–1721 [DOI] [PubMed] [Google Scholar]
- Kato T, Ohashi Y, Nakazato H, Koike S, Saji S, Suzuki H, Takagi H, Nimura Y, Hasumi A, Baba S, Manabe T, Maruta M, Miura K, Yamaguchi A (2002) Efficacy of oral UFT as adjuvant chemotherapy to curative resection of colorectal cancer: multicenter prospective randomized trial. Langenbecks Arch Surg 386: 575–581 [DOI] [PubMed] [Google Scholar]
- Kawaguchi Y, Nagayama S, Masuda H, Yasuda A (1980) Studies on the metabolism of 1-(2-tetrahydrofuryl)-5-fluorouracil and uracil co-administered orally to tumor- bearing rats. Gann 71: 889–899 [PubMed] [Google Scholar]
- Kinoshita T, Nakajima T, Ohashi Y, National Surgical Adjuvant Study Group of Gastric Cancer (2005) Survival benefit of adjuvant chemotherapy with Uracil-tegafur (UFT) for serosa negative advanced gastric cancer (AGC): Results of a randomized trial by National Surgical Adjuvant Study of Gastric Cancer. Proc Am Soc Clin Oncol 23S: 313s (abstr 4021) [Google Scholar]
- Kodaira S, Kikuchi K, Yasutomi M, Takahashi T, Hojo K, Kato T, Tominaga T, Kunii Y (1998) Postoperative adjuvant chemotherapy with mitomycin C and UFT for curatively resected rectal cancer. Results from the Cooperative Project No. 7 Group of the Japanese Foundation for Multidisciplinary Treatment of Cancer. Int J Clin Oncol 3: 357–364 [Google Scholar]
- Lembersky BC, Wieand HS, Petrelli NJ, O'Connell MJ, Colangelo LH, Smith RE, Seay TE, Giguere JK, Marshall ME, Jacobs AD, Colman LK, Soran A, Yothers G, Wolmark N (2006) Oral uracil and tegafur plus leucovorin compared with intravenous fluorouracil and leucovorin in stage II and III carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project Protocol C-06. J Clin Oncol 24: 2059–2064 [DOI] [PubMed] [Google Scholar]
- Mamounas E, Wieand S, Wolmark N, Bear HD, Atkins JN, Song K, Jones J, Rockette H (1999) Comparative efficacy of adjuvant chemotherapy in patients with Dukes' B vs Dukes' C colon cancer: results from four National Surgical Adjuvant Breast and Bowel Project adjuvant studies (C-01, C-02, C-03, and C-04). J Clin Oncol 17: 1349–1355 [DOI] [PubMed] [Google Scholar]
- Meta-Analysis Group In Cancer (1998a) Toxicity of 5-fluorouracil in patients with advanced colorectal cancer: effect of administration schedule and prognostic factors. J Clin Oncol 16: 1–6 [DOI] [PubMed] [Google Scholar]
- Meta-Analysis Group In Cancer (1998b) Efficacy of intravenous continuous infusion of fluorouracil compared with bolus administration in advanced colorectal cancer. J Clin Oncol 16: 301–308 [DOI] [PubMed] [Google Scholar]
- NIH Consensus Conference (1990) Adjuvant therapy for patients with colon and rectal cancer. JAMA 264: 1444–1450 [PubMed] [Google Scholar]
- Noguchi S, Koyama H, Uchino J, Abe R, Miura S, Sugimachi K, Akazawa K, Abe O (2005) Postoperative adjuvant therapy with tamoxifen, tegafur plus uracil, or both in women with node-negative breast cancer: a pooled analysis of six randomized controlled trials. J Clin Oncol 23: 2172–2184 [DOI] [PubMed] [Google Scholar]
- O'Connell MJ, Mailliard JA, Kahn MJ, Macdonald JS, Haller DG, Mayer RJ, Wieand HS (1997) Controlled trial of fluorouracil and low-dose leucovorin given for 6 months as postoperative adjuvant therapy for colon cancer. J Clin Oncol 15: 246–250 [DOI] [PubMed] [Google Scholar]
- Ooi A, Ohkubo T, Higashigawa M, Kawasaki H, Kakito H, Kagawa Y, Kojima M, Sakurai M (2001) Plasma, intestine and tumor levels of 5-fluorouracil in mice bearing L1210 ascites tumor following oral administration of 5-fluorouracil, UFT (mixed compound of tegafur and uracil), carmofur and 5′-deoxy-5-fluorouridine. Biol Pharm Bull 24: 1329–1331 [DOI] [PubMed] [Google Scholar]
- Pisani P, Parkin DM, Ferlay J (1993) Estimates of the worldwide mortality from eighteen major cancers in 1985. Implications for prevention and projections of future burden. Int J Cancer 55: 891–903 [DOI] [PubMed] [Google Scholar]
- Sakamoto J, Hamada C, Kodaira S, Nakazato H, Ohashi Y (1999) Adjuvant therapy with oral fluoropyrimidines as main chemotherapeutic agents after curative resection for colorectal cancer: Individual patient data meta-analysis of randomized trials. Jpn J Clin Oncol 29: 78–86 [DOI] [PubMed] [Google Scholar]
- Sakamoto J, Ohashi Y, Hamada C, Buyse M, Burzykowski T, Piedbois P (2004) Meta-Analysis Group of the Japanese Society for Cancer of the Colon and Recum; Meta-Analysis Group in Cancer. Efficacy of oral adjuvant therapy after resection of colorectal cancer: 5-year results from three randomized trials. J Clin Oncol 22: 484–492 [DOI] [PubMed] [Google Scholar]
- Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidgerger H, Raab R, German Rectal Cancer Study Group (2004) Preoperative vs postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351: 1731–1740 [DOI] [PubMed] [Google Scholar]
- Schmoll HJ, Köhne CH, Lorenz M, Schöffski P, Voigtmann R, Bokemeyer C, Lutz MP, Kleeberg U, Ridwelski K, Souchon R, El-Sarafi M, Weiss U, Couvreur ML, Baron B, Wils JA (2000) Weekly 24 h infusion of high-dose (HD) 5-fluorouracil (5-FU24 h) with or without folinic acid (FA) vs bolus 5-FU/FA (NCCTG/Mayo) in advanced colorectal cancer (CRC): a randomized phase III study of the EORTC GITCCG and the AIO. Proc Am Soc Clin Oncol 19: 241a (abstr 935) [Google Scholar]
- Statistics and information department, Ministry of Health and Welfare (1996) Deaths and death rates by sex and causes of death: Japan 1995 and 1994. In: Vital Stastics of Japan, vol 1, p 465. Health and Welfare Statistics Association: Tokyo [Google Scholar]
- Sugimachi K, Maehara Y, Ogawa M, Kakegawa T, Tomita M (1997) Dose intensity of uracil and tegafur in postoperative chemotherapy for patients with poorly differentiated gastric cancer. Cancer Chemother Pharmacol 40: 233–238 [DOI] [PubMed] [Google Scholar]
- Swedish Rectal Cancer Trial (1997) Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med 336: 980–987 [DOI] [PubMed] [Google Scholar]
- Van Cutsem E, Twelves C, Cassidy J, Allman D, Bajetta E, Boyer M, Bugat R, Findlay M, Frings S, Jahn M, McKendrick J, Osterwalder B, Perez-Manga G, Rosso R, Rougier P, Schmiegel WH, Seitz JF, Thompson P, Vieitez JM, Weitzel C, Harper P (2001) Oral capecitabine compared with with intravenous 5-fluorouracil plus leucovorin (Mayo Clinic regimen) in patients with metastatic colorectal cancer: results of a large phase III study. J Clin Oncol 19: 4097–4106 [DOI] [PubMed] [Google Scholar]
- Vernaba AM, Longo WE, Virgo KS, Coplin MA, Wade TP, Johnson FE (1994) Current follow up statistics after resection of colorectal cancer. Dis Colon Rectum 37: 573–583 [DOI] [PubMed] [Google Scholar]
- Watanabe M, Nishida O, Kunii Y, Kodaira S, Takahashi T, Tominaga T, Hojyo K, Kato T, Niimoto M, Kunitomo K, Isomoto H, Ohashi Y, Yasutomi M (2004) Randomized controlled trial of the efficacy of adjuvant immunochemotherapy and adjuvant chemotherapy for colorectal cancer, using different combinations of the intracutaneous streptococcal preparation OK-432 and the oral pyrimidines 1-hexylcarbamoyl-5-fluorouracil and uracil/tegafur. Int J Clin Oncol 9: 98–106 [DOI] [PubMed] [Google Scholar]
- Wolmark N, Rockette H, Fisher B, Wickerham DL, Redmond C, Fisher ER, Jones J, Mamounas EP, L Ore L, Petrelli NJ (1993) The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project Protocol C-03. J Clin Oncol 11: 1879–1887 [DOI] [PubMed] [Google Scholar]
- Wolmark N, Rockette H, Mamounas E, Jones J, Wieand S, Wickerham DL, Bear HD, Atkins JN, Dimitrov NV, Glass AG, Fisher ER, Fisher B (1999) Clinical trial to assess the relative efficacy of fluorouracil and leucovolin, fluorouracil and levamisole, and fluorouracil, leucovorin, and levamisole in patients with Dukes'B and C carcinoma of the colon : Results from national surgical adjuvant breast and bowel project C-04. J Clin Oncol 17: 3553–3559 [DOI] [PubMed] [Google Scholar]
- Wolmark N, Wieand HS, Hyams DM, Colangelo L, Dimitrov NV, Romond EH, Wexler M, Prager D, Cruz Jr AB, Gordon PH, Petrelli NJ, Deutsch M, Mamounas E, Wickerham DL, Fisher ER, Rockette H, Fisher B (2000) Randomized trial of postoperative adjuvant chemotherapy with or without radiotherapy for carcinoma of rectum: National Surgical Adjuvant Breast and Bowel Project Protocol R-02. J Natl Cancer Inst 92: 388–396 [DOI] [PubMed] [Google Scholar]