Abstract
The epidermal growth factor receptor (EGFr) is considered a major target for treatment of colorectal cancer (CRC). We found a mean EGFr content significantly lower but more activated in colonic neoplastic tissue than in paired normal mucosa. Phosphorylated (pY1068) EGFr detection in CRC may be a better tool than EGFr detection to select patients for targeted therapies.
Keywords: EGFr, phosphorylated EGFr, colorectal cancer, targeted therapy
Epidermal growth factor receptor (EGFr) plays a pivotal role in regulating epithelial proliferation, differentiation and survival. Aberrant regulation of EGFr signalling has been implicated in the development and progression of several different solid tumours (Rubin Grandis et al, 1996; Rusch et al, 1997; Goldstein and Armin, 2001). Colorectal cancer (CRC) is considered a tumour showing EGFr overexpression, but EGFr expression ranges between 25 and 75% (Salomon et al, 1995; Goldstein and Armin, 2001). The discrepancy in this range could be due to several factors. The first is related to EGFr detection. The most popular method of EGFr determination is immunohistochemistry (IHC) that per se does not provide for reliable quantitative analysis, and standardised techniques and scoring systems are lacking (Dei Tos and Ellis, 2005). The second factor is related to possible nonuniform EGFr expression within the tumour area (Goldstein and Armin, 2001). In addition, most studies are confined to neoplastic tissue without normalisation to the corresponding normal mucosa. Nevertheless, some IHC studies measuring EGFr expression both in neoplastic tissue and paired normal colonic mucosa reported a similar EGFr content in the two compartments (Moorghen et al, 1990; Maurer et al, 1998). These factors could be responsible for the lack of comparable results in literature and the lack of correlation between EGFr expression and the clinical activity of EGFr inhibitors in humans (Cunningham et al, 2004; Chung et al, 2005).
The aim of the present study was to shed more light on EGFr expression in CRC, evaluating total and activated (pY1068) EGFr and mRNA content on neoplastic tissue and paired normal mucosa using two quantitative techniques (ELISA and real-time PCR).
MATERIALS AND METHODS
Patients and tissues
Thirty-nine patients (21 men and 18 women) surgically treated for sporadic CRC were enrolled in the study. The clinical and pathological parameters are summarised in Table 1. Tissue samples were collected from the primary tumour and from mucosa with a roughly normal appearance more than 25 cm from the lesion. Neoplastic tissue was quickly frozen in liquid nitrogen and stored at −80°C until use. Normal mucosa was split into two blocks, one frozen and stored immediately and the other processed for histological diagnosis to exclude pathological lesions.
Table 1. Demographic and pathological characteristics of the CRC patients.
|
Patients
|
||
|---|---|---|
| Characteristic | No. | % |
| Age (years) | ||
| Mean | 69.2±1.5 | |
| Range | 46–84 | |
| Sex | ||
| Female | 18 | 46.2 |
| Male | 21 | 53.8 |
| Lesion site | ||
| Right colon | 15 | 38.5 |
| Left colon | 24 | 61.5 |
| Tumour diameter (mm) | ||
| Mean | 47.4±2.5 | |
| Range | 24–100 | |
| Histological grading | ||
| Poorly differentiated | 6 | 15.4 |
| Moderately differentiated | 31 | 79.5 |
| Well differentiated | 2 | 5.1 |
| Pathological staging | ||
| Stage II | 18 | 46.2 |
| Stage III | 19 | 48.7 |
| Stage IV | 2 | 5.1 |
CRC=colorectal cancer.
Protein extraction and ELISA quantification of total and activated (pY1068) EGFr
Frozen tissues were homogenised using lysis buffer (50 mM Tris pH 7.4, 150 mM NaCl, 2 mM MgCl2, 1% Triton X-100, 10% glycerol, 2 mM EGTA, 1 mM DTT) containing protease inhibitors (10 mg ml−1 aprotinin and leupeptin, 5 mg ml−1 pepstatin, 1 mM PMSF) and phosphatase inhibitors (50 mM NaF, 10 mM Na4P2O7, 1 mM Na3VO4, 3 mM H2O2). Homogenates were centrifuged at 13 000 g for 15 min at 4°C, and supernatants were stored at −80°C until analysis.
The concentration of total and pY1068 EGFr was assessed using ELISA kits purchased from Biosource International Inc. (Camarillo, CA, USA). Protein lysates from A431 and SW620 cell lines were used as positive and negative controls, respectively, to verify the specificity of the EGFr ELISA assays.
Relative activated (pY1068) EGFr was defined as pY1068/total EGFr.
RNA extraction and real-time PCR quantification of EGFr
Total RNA was isolated using TRIzol Reagent (Invitrogen Life Technologies, Carlsbad, CA, USA) and reverse transcribed using Superscript II (Invitrogen Life Technologies) with oligo-dT primers, according to the manufacturer's guidelines.
Gene-specific primers and TaqMan probes (Table 2) were designed with the Beacon Designer 2.00 Software (Premier Biosoft International, Palo Alto, CA, USA) and real-time PCR was performed using an iCycler apparatus (Bio-Rad Laboratories, Hercules, CA, USA). The cycle numbers were recorded when the accumulated PCR products crossed an arbitrary threshold (CT or threshold cycle) and CT values were used to calculate the expression levels of EGFr relative to the internal reference β-actin.
Table 2. Primers and Taqman probes.
| Gene | GenBank Accession No. | Forward primer (5′–3′) | Reverse primer (5′–3′) | Taqman probe (5′–3′) |
|---|---|---|---|---|
| EGFr | NM_005228 | TTCCTCCCAGTGCCTGAAT | GGGCTGGACAGTGTTGAGAT | CGCCCAGCAGAGACCCACACTACC |
| β-Actin | NM_001101 | CGGCCAGGTCATCACCATTG | TGGAGTTGAAGGTAGTTTCGTGG | TGCCACAGGACTCCATGCCCAGG |
EGFr=epidermal growth factor receptor.
Statistical analysis
Statistical calculations were performed using StatView 5.0 statistical software (SAS Institute Inc., Cary NC, USA). For all analyses, a P-value of less than 0.05 was considered significant. Values were given as mean±s.e.
The paired t-test was used to detect differences in total and relative activated (pY1068) EGFr and mRNA mean values between normal and neoplastic tissue. Associations between these variables were assessed by the Spearman rank test and regression analysis was performed. The relationship with clinicopathologic parameters was explored using the unpaired t-test.
RESULTS
Evaluation of total and activated (pY1068) EGFr by ELISA
Total and activated (pY1068) EGFr levels were determined in 39 paired samples. Mean total EGFr protein content was significantly higher in normal mucosa than in neoplastic tissue ((260.8±20.3) vs (120.5±14.7) fmol EGFr mg−1 of total protein) (Figure 1A). According to Spearman's rank test, total EGFr expression levels showed an association between normal mucosa and the respective neoplastic tissue (R=0.49; P=0.004). This relationship was visualised using scatterplot graphic analysis (Figure 1C). Mean relative activated (pY1068) EGFr content was significantly higher in neoplastic tissue than in normal mucosa ((1.103±0.387) vs (0.129±0.019) U fmol−1 EGFr).
Figure 1.
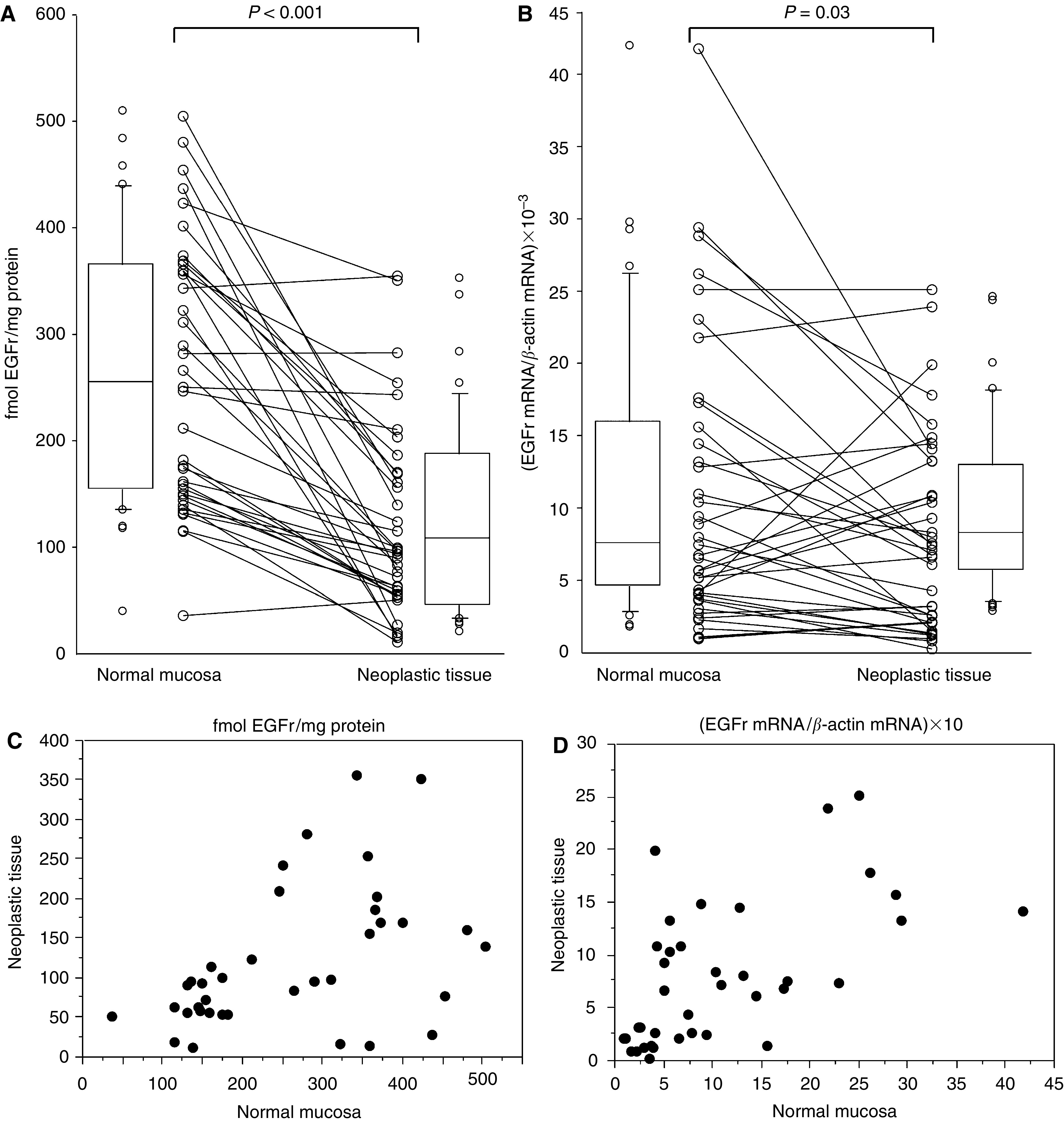
EGFr content in normal mucosa and in neoplastic tissue. Paired protein (A) and mRNA (B) samples are connected by lines. Box-plot graphic analyses are also shown. Scatterplot graphic analysis for EGFr protein (C) and mRNA (D) content are reported. Each dot represents EGFr protein or mRNA content in normal mucosa and neoplastic tissue of the same patient.
Evaluation of EGFr mRNA expression by real-time PCR
EGFr mRNA content was determined in 39 paired samples. Mean EGFr mRNA content was significantly higher in normal mucosa than in neoplastic tissue ((10.7±1.6) × 10−3 vs (7.8±1.1) × 10−3) (Figure 1B). According to Spearman's rank test, EGFr mRNA expression showed an association between normal mucosa and the respective neoplastic tissue (R=0.65; P<0.0001). This relationship was visualised using scatterplot graphic analysis (Figure 1D). Regression analysis was also performed (P<0.0001).
Correlation with clinicopathologic parameters
No association was found between total or relative activated (pY1068) EGFr or mRNA content in neoplastic tissue and normal mucosa and sex, tumour location, histological grading and stage.
DISCUSSION
We studied total and activated (pY1068) EGFr and mRNA content in neoplastic tissue and paired normal mucosa samples from 39 CRC patients using two quantitative techniques. Three main results emerged from the study. Firstly, both EGFr protein and mRNA content varied widely in both neoplastic tissue and normal mucosa in our CRC patients, in agreement with IHC studies (Salomon et al, 1995; Goldstein and Armin, 2001). Secondly, EGFr expression in the apparently normal colorectal mucosa of our CRC patients supports the idea that EGFr expression may not be exclusive to CRC. In fact, normalising EGFr protein content in neoplastic tissue vs normal mucosa did not disclose EGFr overexpression. In addition, an association was found for EGFr protein or mRNA content in neoplastic tissue and normal mucosa from the same patient. Thirdly, in neoplastic tissue EGFr is more activated than in paired normal mucosa.
These results have certain biological and clinical implications. The fact that the mean EGFr content is higher in normal mucosa than in neoplastic tissue, both for protein and mRNA determination, does not exclude a role for EGFr in the carcinogenesis of CRC. Epidermal growth factor receptor signalling in the maintenance of carcinomas during intestinal tumorigenesis has been found in animal experiments (Roberts et al, 2002). In our study, the inverse relationship between EGFr expression and activity, demonstrated so far in CRC cell lines (Keese et al, 2005), supports the hypothesis that activated EGFr has a role in CRC.
In conclusion, CRC does not invariably overexpress EGFr and, most importantly, the EGFr content is frequently lower but more activated in cancer tissue than in paired normal mucosa. Epidermal growth factor receptor activity may be considered a better indicator than EGFr content when selecting expected responders to targeted therapy. This would, in part, explain the modest results observed in clinical practice when specific antibodies (i.e. Cetuximab) are combined with chemotherapy for CRC patients with IHC-positive tumors (Cunningham et al, 2004; Chung et al, 2005). The activity of specific monoclonal antibodies on apparently normal colorectal mucosa overexpressing EGFr, and the crosstalking of different biological pathways leading to cancer growth should be topics for preclinical research. Some studies currently in progress on these issues are expected to yield more data for a more correct clinical use of the so-called targeted therapies (Pantaleo et al, 2006).
Acknowledgments
This work was supported by a grant from Fondazione Cassa di Risparmio in Bologna-Italy. This work was partially presented on November 2005 at AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics. We thank Dr Massimiliano Bonafé and Dr Pasquale Chieco for their valid statistical support.
References
- Chung KI, Shia J, Kemeny NE, Shah M, Schwartz GK, Tse A, Hamilton E, Pan D, Schrag D, Schwartz L, Klimstra DS, Fridman D, Kelsen DP, Saltz LB (2005) Cetuximab shows activity in colorectal cancer patients with tumors that do not express the epidermal growth factor receptor by immunohistochemistry. J Clin Oncol 23: 1803–1810 [DOI] [PubMed] [Google Scholar]
- Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, Bets D, Mueser M, Harstrick A, Verslype C, Chau I, Van Cutsem E (2004) Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 351: 337–345 [DOI] [PubMed] [Google Scholar]
- Dei Tos AP, Ellis I (2005) Assessing epidermal growth factor receptor expression in tumours: what is the value of current test methods? Eur J Cancer 41: 1383–1392 [DOI] [PubMed] [Google Scholar]
- Goldstein NS, Armin M (2001) Epidermal growth factor receptor immunohistochemical reactivity in patients with American Joint Committee on Cancer Stage IV colon adenocarcinoma: implications for a standardized scoring system. Cancer 92: 1331–1346 [DOI] [PubMed] [Google Scholar]
- Keese M, Magdeburg RJ, Herzog T, Hasenberg T, Offterdinger M, Pepperkok R, Sturm JW, Bastiaens PI (2005) Imaging epidermal growth factor receptor phosphorylation in human colorectal cancer cells and human tissues. J Biol Chem 280: 27826–27831 [DOI] [PubMed] [Google Scholar]
- Maurer CA, Friess H, Kretschmann B, Zimmermann A, Stauffer A, Baer HU, Korc M, Bucheler MW (1998) Increased expression of erbB3 in colorectal cancer is associated with concomitant increase in the level of erbB2. Hum Pathol 29: 771–777 [DOI] [PubMed] [Google Scholar]
- Moorghen M, Ince P, Finney KJ, Watson AJ, Harris AL (1990) Epidermal growth factor receptors in colorectal carcinoma. Anticancer Res 10: 605–611 [PubMed] [Google Scholar]
- Pantaleo MA, Palassini E, Labianca R, Biasco G (2006) Targeted therapy in colorectal cancer: do we know enough? Dig Liver Dis 38: 71–77 [DOI] [PubMed] [Google Scholar]
- Roberts RB, Min L, Washington MK, Olsen SJ, Settle SH, Coffey RF, Threadgill DW (2002) Importance of epidermal growth factor receptor signaling in establishment of adenomas and maintenance of carcinomas during intestinal tumorigenesis. Proc Natl Acad Sci USA 99: 1521–1526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin Grandis J, Melhem MF, Barnes EL, Tweardy DJ (1996) Quantitative immunohistochemical analysis of transforming growth factor-alpha and epidermal growth factor receptor in patients with squamous cell carcinoma of the head and neck. Cancer 78: 1284–1292 [DOI] [PubMed] [Google Scholar]
- Rusch V, Klimstra D, Venkatraman E, Pisters PW, Langenfeld J, Dmitrovsky E (1997) Overexpression of the epidermal growth factor receptor and its ligand transforming growth factor alpha is frequent in resectable non-small cell lung cancer but does not predict tumor progression. Clin Cancer Res 3: 515–522 [PubMed] [Google Scholar]
- Salomon DS, Brandt R, Ciardiello F, Normanno N (1995) Epidermal growth factor-related peptides and their receptors in human malignancies. Crit Rev Oncol Hematol 19: 183–232 [DOI] [PubMed] [Google Scholar]


