Abstract
Epithelial cell adhesion molecule (Ep-CAM; CD326) is used as a target by many immunotherapeutic approaches, but little data are available about Ep-CAM expression in major human malignancies with respect to level, frequency, tumour stage, grade, histologic tumour type and impact on survival. We analysed by immunohistochemical staining tissue microarrays with 4046 primary human carcinoma samples from colon, stomach, prostate and lung cancers for both frequency and intensity of Ep-CAM expression under highly standardised conditions. A total of 3360 samples were analysable. High-level Ep-CAM expression was observed in 97.7% (n=1186) of colon, 90.7% of gastric (n=473), and 87.2% of prostate cancers (n=414), and in 63.9% of lung cancers (n=1287). No detectable Ep-CAM staining was found with only 0.4% of colon, 2.5% of gastric, 1.9% of prostate cancers, and 13.5% of lung cancers. The only significant correlation of Ep-CAM expression with tumour grading was observed in colon cancer where high-level Ep-CAM expression on grade 3 tumours was down to 92.1% (P<0.0001). Adenosquamous and squamous carcinomas of the lung had a lower percentage of high-level Ep-CAM expression compared to adenocarcinomas with 35.4 and 53.6%, respectively, and with 45.5 and 17.3% of tumours being Ep-CAM negative. With the exception of moderately differentiated colon carcinoma, where patients not expressing Ep-CAM on their tumours showed an inferior survival (P=0.0014), correlation of Ep-CAM expression with survival did not reach statistical significance for any of the other cancer indications and subgroups. In conclusion, the data strongly support the notion that Ep-CAM is a prime target for immunotherapies in major human malignancies. This is because the most common human cancers show (i) a low frequency of Ep-CAM-negative tumours, (ii) a high frequency of Ep-CAM expression on cells of a given tumour, and (iii) for most cancers, an insignificant influence of tumour staging, grading and histology on Ep-CAM expression.
Keywords: Ep-CAM, colon cancer, stomach cancer, prostate cancer, lung cancer, monoclonal antibody
Epithelial cell adhesion molecule (Ep-CAM)is a type I transmembrane glycoprotein of Mr 40 000 Da, expressed in most normal epithelial tissues on the basolateral surface. While no expression is seen on squamous epithelia and hepatocytes, it is detected on colon, gastric, prostatic and lung epithelium (Moldenhauer et al, 1987). Epithelial cell adhesion molecule is thought to function as a homotypic intercellular adhesion molecule (Litvinov et al, 1994). Its role in epithelial cell adhesion is dynamic and interconnected with E-cadherin (Litvinov et al, 1997). By upregulation of Ep-CAM, E-cadherin-mediated cell adhesion diminishes and the Ep-CAM mediated adhesion becomes predominant. During organogenesis in mice, Ep-CAM exhibits features of a morpho-regulatory molecule, which, for instance, is involved in the development of human pancreatic islets (Cirulli et al, 1998).
Epithelial cell adhesion molecule was discovered as one of the first tumour-associated antigens by immunising mice with human colon cancer cells followed by analysis of tumour-specific monoclonal antibodies (Herlyn et al, 1979; Sears et al, 1982). Epithelial cell adhesion molecule was then found to be expressed at a high level and frequency not only on colon cancer tissues but on most human adenocarcinomas (Went et al, 2004) as well as on squamous cell carcinomas (Quak et al, 1990). In the case of breast and ovarian cancers, Ep-CAM mRNA was found to be more than 100-fold overexpressed relative to normal epithelial tissues (Kim et al, 2003; Osta et al, 2004).
Overexpression of Ep-CAM is linked to differentiation and cell proliferation (Jordinson et al, 1999), although the molecular mechanism is still poorly understood. In vitro, its overexpression has been shown to be directly linked to stimulation of the cell cycle and proliferation by upregulating c-myc and cyclin A/E (Munz et al, 2004). In breast cancer cells, inhibition of Ep-CAM expression by small inhibitory RNA diminishes cell proliferation, migration and invasiveness of cells (Osta et al, 2004). Epithelial cell adhesion molecule gene expression appears to be negatively regulated by TNF-alpha through activation of NF-kappaB (Gires et al, 2001). Upon cell cycle arrest by various chemotherapeutics, Ep-CAM surface expression is enhanced (Flieger et al, 2001; Thurmond et al, 2003). As Ep-CAM is involved in adhesion, differentiation and cell proliferation, an influence of Ep-CAM expression on survival of cancer patients can be expected. In breast and gall bladder cancer, patients with high Ep-CAM-expressing primary tumours indeed showed a decreased survival (Gastl et al, 2000; Spizzo et al, 2002; Spizzo et al, 2004; Varga et al, 2004). In clear cell renal cell carcinoma, Ep-CAM expression is infrequent, but patients with Ep-CAM overexpressing tumours show a trend to better survival (Kim et al, 2004; Seligson et al, 2004; Went et al, 2005). A similar correlation was reported for gastric cancers (Songun et al, 2005). Very little information is currently available with regard to the correlation of Ep-CAM expression with survival and tumour staging for colon and lung cancers, while more recent studies have explored larger sample numbers of gastric (Songun et al, 2005) and prostate cancers (Poczatek et al, 1999; Zellweger et al, 2005) for Ep-CAM expression.
Due to its frequent and high-level expression, Ep-CAM was selected as target antigen for a multitude of immunotherapeutic approaches (Balzar et al, 1999). These include murine and human monoclonal antibodies, antibody conjugates with bacterial toxins and chemotherapeutics, and vaccines. Currently, a number of Ep-CAM-specific immunotherapies are in phase I and II clinical trials. These are anti-Ep-CAM antibodies ING-1 (de Bono et al, 2004), adecatumumab (Naundorf et al, 2002; Prang et al, 2005), and edrecolomab (Himmler et al, 2003), as well as an immunotoxin (Zimmermann et al, 1997; Di Paolo et al, 2003). It is therefore very important to understand which human cancers are amenable to Ep-CAM-specific immunotherapy based on Ep-CAM expression with respect to intensity, frequency and disease stage. Likewise, it is interesting to investigate a correlation of Ep-CAM expression with survival prognosis in patients.
The aim of the present retrospective study was to investigate the frequency and intensity of Ep-CAM expression in four major human cancers by the use of tissue microarrays. This technology allows for a simultaneous comparison of immunohistochemical staining patterns and intensities across a large panel of tumour samples. Variability due to fixation and staining procedures are reduced to a minimum, while comparability is maximised. Epithelial cell adhesion molecule expression results were correlated for the first time with clinico-pathological parameters in colon and lung cancers, while results from a large panel of gastric and prostate cancer samples are being compared to published data. Our results show that colon, gastric and prostate cancers as well as adenocarcinoma of the lung are promising indications for treatment with Ep-CAM-specific immunotherapies. Their frequencies of high-level Ep-CAM expression >80% may even obviate the need for prescreening of patients.
MATERIALS AND METHODS
Array composition
Primary tumours of colon, stomach, lung and prostate were included in this study. Formalin-fixed and paraffin-embedded tissue probes were retrieved from the archives of the Institute for Pathology of the University Hospital Basel (Switzerland), the City Hospital Triemli in Zürich (Switzerland) and the Departments of Pathology of the University of Freiburg (Germany) and the Shiraz University (Iran). Retrieval of tissue and clinical data was performed according to the regulations of the local institutional review board and data safety laws. The grade of the tumours was obtained by a review of each case by a specialised pathologist. A total of 1407 colon cancers (1261 adenocarcinomas NOS, five medullary carcinomas, 119 mucinous carcinomas, five signet ring carcinomas, four other types), 559 stomach, 1527 lung (367 adenocarcinomas (AC), 13 adenosquamous carcinomas, 82 bronchioloalveolar carcinomas, 258 large cell carcinomas, 63 neuroendocrine carcinomas, 744 squamous cell carcinomas (SCC)) and 553 prostate carcinomas were then arrayed as described before (Bubendorf et al, 2001). Briefly, tissue cylinders with a diameter of 0.6 mm were punched from representative tumour areas of each donor tissue block and brought into a recipient paraffin block. Multiple 4 μm sections of the resulting tissue microarray block were cut and mounted to an adhesive-coated slide system.
Clinical data
All relevant patient data were anonymised. Sex, age and stage according to the WHO/UICC 1997 were recorded in subsets of gastric, colon, lung and prostate cancers. In prostate cancers, the Gleason score was available. Grade was also known in colon and lung cancers. Additionally, the survival time was recorded in tumours from the colon, lung and prostate, but not stomach. Overall survival (OS) was calculated from the date of diagnosis until death from any cause or date of last contact for living patients. The cause of death was recorded in a subset of patients to calculate the tumour-specific survival.
Immunohistochemistry
Standard indirect staining procedures were used for immunohistochemistry (ABC-Elite-Kit, Vector Laboratories, Burlingame, CA, USA). After heat-induced pretreatment (water bath, 30 min, 99°C in target retrieval solution buffer (DAKO code S1699, DAKO, Glostrup, Denmark)) for antigen retrieval, a mouse monoclonal anti-Ep-CAM-antibody (ESA, clone VU-1D9, Novocastra, Newcastle upon Tyne, UK) was applied for 2 h at a dilution of 1 : 50 at 37°C. The slides were then incubated with the secondary, biotinylated antibody. Osmium-enhanced diaminobenzidine was used as the chromogen. Counterstaining was carried out with Harris' haematoxylin. Only fresh cut slides were stained simultaneously to minimise the influence of slide ageing and maximise repeatability and reproducibility of the experiment. For negative controls, the primary antibody was omitted, as positive controls the internal normal tissues with known EpCam positivity were used. For each sample, staining intensity (0, faint to moderate, intense) and percentage of positive tumour cells was estimated. A case was considered strongly positive if the antibody detected >70% positive cells, otherwise weakly positive, or negative if no cells were stained. Staining intensity was recorded, but not used for correlation with clinical findings, as it can vary depending on the manner of tissue fixation. Cytoplasmic staining alone was considered as nonspecific as Ep-CAM is localised on the cell membrane. These cases were excluded from analysis. The slides were all evaluated in one day by one experienced pathologist (GS) to minimise inter- and intraobserver variability of the results.
Statistics
The software used for statistical analysis was statview 5.0 (SAS Institute Inc., NC, USA) The Fisher's exact test and the χ2 test were used to compare Ep-CAM expression and clinical and morphological tumour characteristics. For survival analysis, patients with Ep-CAM weakly to moderately positive and negative tumours were grouped together to emphasise on Ep-CAM overexpressing tumours. Survival curves were plotted according to Kaplan–Meier. The univariate association between individual clinical features and overall survival (OS) was determined with the log-rank test. Factors independently associated with OS were identified in a multivariate analysis by the Cox proportional hazards regression model. The limit of significance for all analyses was defined as a P-value <0.05; two-sided tests were used in all calculations.
RESULTS
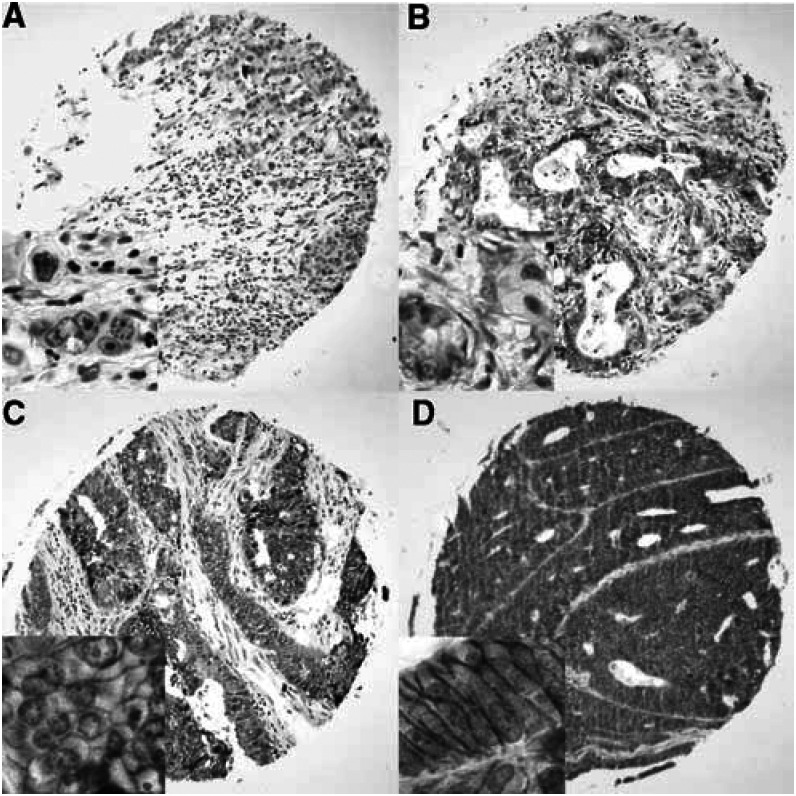
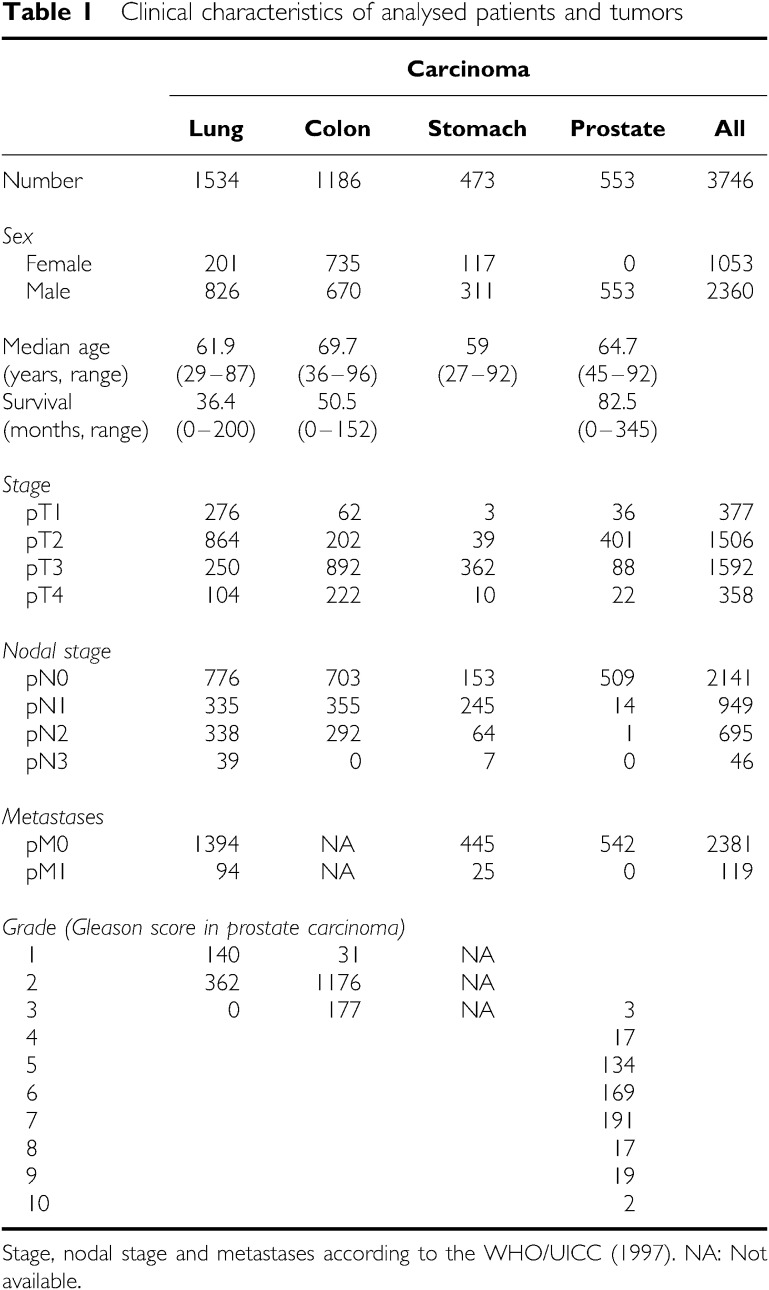
Clinical information was available for 3746 tumours (Table 1), whereas Ep-CAM staining results from tissue microarrays were obtained for 3360 tumour samples. A total of 686 tumour samples (17%) on microarrays could not be analysed due to issues of sample quality. Figure 1 shows examples for different intensities of Ep-CAM-specific immunohistochemical staining of tissue microarray samples from four colon cancer patients.
Table 1. Clinical characteristics of analysed patients and tumors.
|
Carcinoma
|
|||||
|---|---|---|---|---|---|
| Lung | Colon | Stomach | Prostate | All | |
| Number | 1534 | 1186 | 473 | 553 | 3746 |
| Sex | |||||
| Female | 201 | 735 | 117 | 0 | 1053 |
| Male | 826 | 670 | 311 | 553 | 2360 |
| Median age | 61.9 | 69.7 | 59 | 64.7 | |
| (years, range) | (29–87) | (36–96) | (27–92) | (45–92) | |
| Survival | 36.4 | 50.5 | 82.5 | ||
| (months, range) | (0–200) | (0–152) | (0–345) | ||
| Stage | |||||
| pT1 | 276 | 62 | 3 | 36 | 377 |
| pT2 | 864 | 202 | 39 | 401 | 1506 |
| pT3 | 250 | 892 | 362 | 88 | 1592 |
| pT4 | 104 | 222 | 10 | 22 | 358 |
| Nodal stage | |||||
| pN0 | 776 | 703 | 153 | 509 | 2141 |
| pN1 | 335 | 355 | 245 | 14 | 949 |
| pN2 | 338 | 292 | 64 | 1 | 695 |
| pN3 | 39 | 0 | 7 | 0 | 46 |
| Metastases | |||||
| pM0 | 1394 | NA | 445 | 542 | 2381 |
| pM1 | 94 | NA | 25 | 0 | 119 |
| Grade (Gleason score in prostate carcinoma) | |||||
| 1 | 140 | 31 | NA | ||
| 2 | 362 | 1176 | NA | ||
| 3 | 0 | 177 | NA | 3 | |
| 4 | 17 | ||||
| 5 | 134 | ||||
| 6 | 169 | ||||
| 7 | 191 | ||||
| 8 | 17 | ||||
| 9 | 19 | ||||
| 10 | 2 | ||||
Stage, nodal stage and metastases according to the WHO/UICC (1997).
NA: Not available.
Figure 1.
Examples of Ep-CAM staining of four human colon carcinoma samples from a tissue microarray. (A) Sample with no Ep-CAM staining. Samples with weak (B), moderate (C) or intense (D) Ep-CAM staining. Note that in (B) and (C) the staining intensity and quantity of positive tumour cells are different. Inlets showing detailed view of the membrane localised staining product.
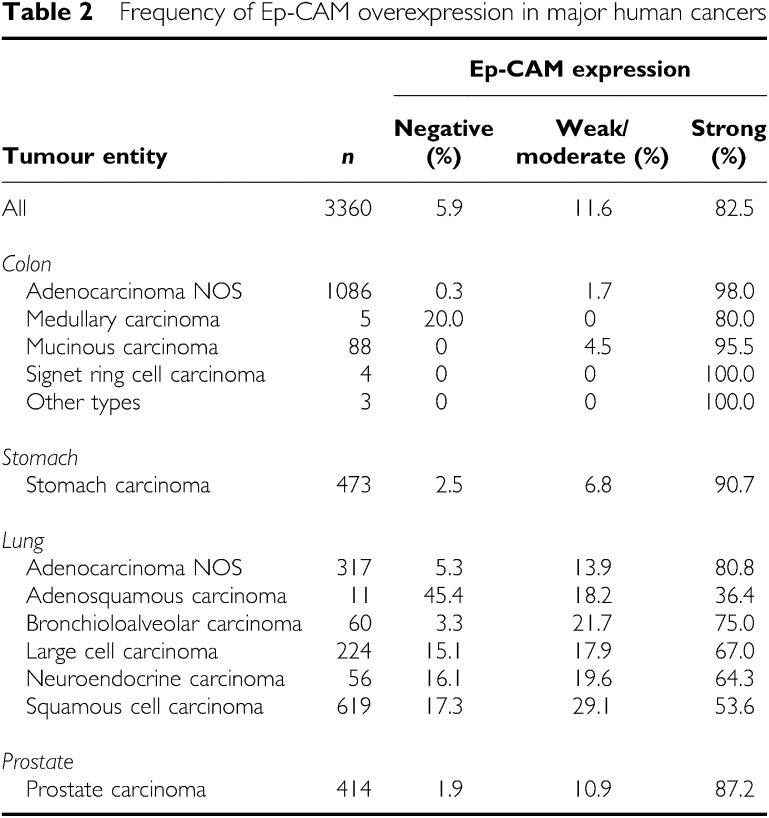
In all four tumour entities, staining was predominantly membranous but cytoplasmic staining could also be seen in cases with an intense staining. In total, 74.1% of the 3360 tumours showed a high-level Ep-CAM staining. In total, 85.1% of samples showed a staining in >70% of tumour cells. Of note, 92.2% (2118 of 2297 cases) of tumours with an Ep-CAM-positive cell fraction >70% had at the same time the highest staining intensity score, indicating a marked coincidence of high-level staining intensity with a high fraction of positive tumour cells. As intensity is typically subdued to variations following tissue fixation and most notably staining procedures, the equal high staining intensity in the majority of cases well reflects the highly optimised staining procedure, whereas the high percentage of positive cases indicates an excellent preservation of the investigated antigen in the samples selected for construction of microarrays. This obviously led to an almost binary data set in which only 11.6% of the 3360 tumour samples showed a positive tumour cell fraction of less than 70%, and on average 19.6% a weak to moderate staining intensity. The observed ‘black or white’ pattern was further emphasised by the scoring system, correlating only strongly positive tumours with survival data. On average, Ep-CAM expression was completely absent from only 5.9% of tumours (198 cases) based on immunohistochemical analysis. An overview of staining results across all tumour samples is shown in Table 2.
Table 2. Frequency of Ep-CAM overexpression in major human cancers.
|
Ep-CAM expression
|
||||
|---|---|---|---|---|
| Tumour entity | n | Negative (%) | Weak/ moderate (%) | Strong (%) |
| All | 3360 | 5.9 | 11.6 | 82.5 |
| Colon | ||||
| Adenocarcinoma NOS | 1086 | 0.3 | 1.7 | 98.0 |
| Medullary carcinoma | 5 | 20.0 | 0 | 80.0 |
| Mucinous carcinoma | 88 | 0 | 4.5 | 95.5 |
| Signet ring cell carcinoma | 4 | 0 | 0 | 100.0 |
| Other types | 3 | 0 | 0 | 100.0 |
| Stomach | ||||
| Stomach carcinoma | 473 | 2.5 | 6.8 | 90.7 |
| Lung | ||||
| Adenocarcinoma NOS | 317 | 5.3 | 13.9 | 80.8 |
| Adenosquamous carcinoma | 11 | 45.4 | 18.2 | 36.4 |
| Bronchioloalveolar carcinoma | 60 | 3.3 | 21.7 | 75.0 |
| Large cell carcinoma | 224 | 15.1 | 17.9 | 67.0 |
| Neuroendocrine carcinoma | 56 | 16.1 | 19.6 | 64.3 |
| Squamous cell carcinoma | 619 | 17.3 | 29.1 | 53.6 |
| Prostate | ||||
| Prostate carcinoma | 414 | 1.9 | 10.9 | 87.2 |
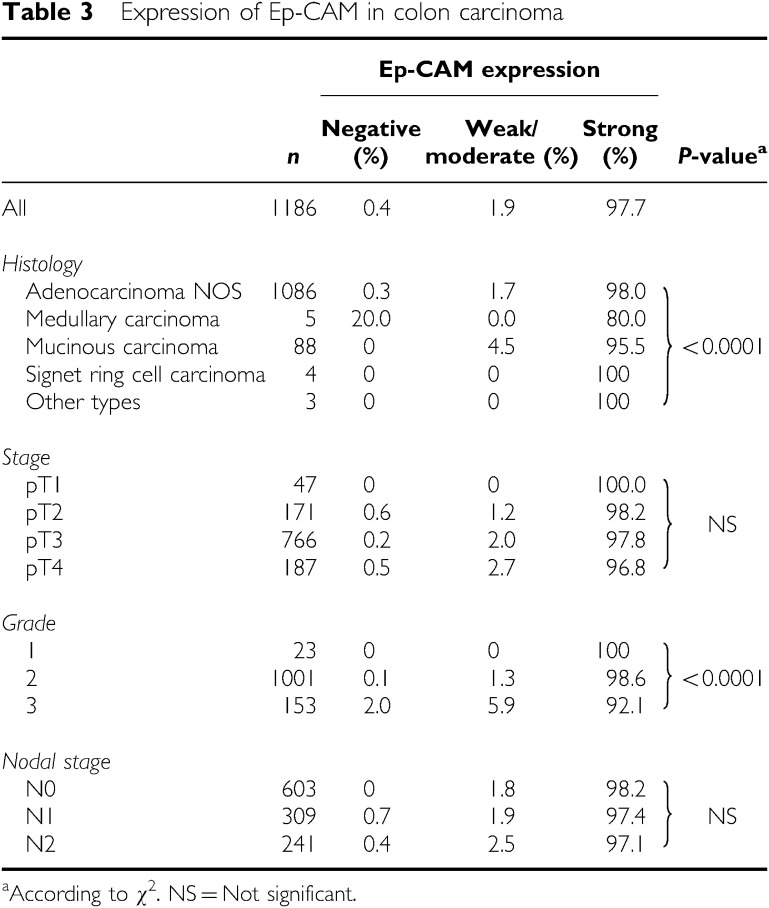
Epithelial cell adhesion molecule expression in colon cancer
In the colon cancer microarray (Table 3), samples from 1186 patients were analysable. Most of the cases showed an intense staining signal in the vast majority of tumour cells. Only seven tumours (0.6%) showed a faint staining intensity, whereas 1152 tumours (97.1%) showed a strong staining intensity. In total, 97.7% of cases (n=1159) showed Ep-CAM expression in more than 70% of tumour cells.
Table 3. Expression of Ep-CAM in colon carcinoma.
Highly differentiated colon cancers expressed Ep-CAM significantly more frequently and strongly than the other colon cancers (P<0.0001). However, the low differentiated colon cancers of grade 3 were still strongly positive for Ep-CAM in 92.1% of cases.
In an univariate survival analysis, the lymph node status (pN0 vs pN+, P<0.0001), vascular invasion (P<0.0001) and postoperative chemotherapy (P<0.0001) were significant regarding tumour-specific survival. Because Ep-CAM expression and tumour grade showed a significant association, the different grades were analysed separately. Patients with Ep-CAM negative, moderately differentiated colon cancers (Grade 2) showed a significantly inferior tumour-specific survival (OR 5.421, 95% CI 1.685–17.442, P=0.0014, n=284), whereas in the other subgroups patients with strongly Ep-CAM expressing tumours showed no such trend towards a better survival. This association in the G2 colon carcinomas remained significant in a multivariate analysis including Ep-CAM expression (OR 11.175, 95% CI 3.327–37.534, P<0.0001), the lymph node status (OR 3.169, 95% CI 1.768–5.680, P=0.0001), vascular invasion (OR 2.408, 95% CI 1.345–4.309, P=0.0031), whereas postoperative chemotherapy (OR 0.772, 95% CI 0.421–1.413, P=0.4006) showed no statistical significance.
EPITHELIAL CELL ADHESION MOLECULE EXPRESSION IN STOMACH CANCER
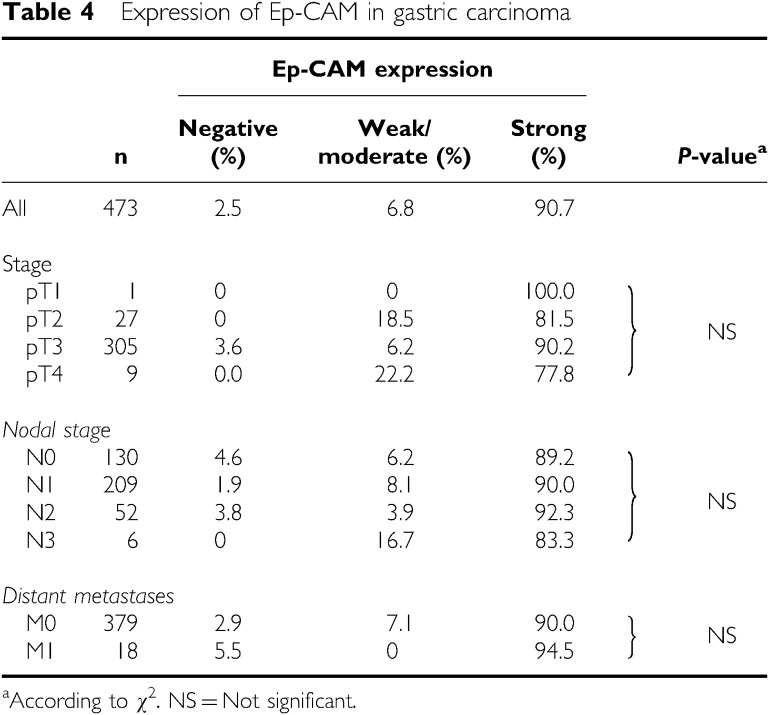
On the stomach cancer microarray (Table 4), 473 cases were analyzable. In total, 90.7% of the tumours (n=429) expressed Ep-CAM on >70% of cells and 85.8% of the cases (n=406) showed the highest level of staining intensity. Epithelial cell adhesion molecule frequency was lowest in pT4 tumours (77.8%), while all other subgroups showed Ep-CAM expression in more than 80% of tumours. No significant correlation of Ep-CAM expression between primary tumour, nodal or metastasised stage was found. In this group of patients, no data on patient survival were available for correlation with Ep-CAM expression.
Table 4. Expression of Ep-CAM in gastric carcinoma.
Epithelial cell adhesion molecule expression in prostate cancer
In the prostate cancer microarray, 414 cases were analyzable (Table 5). Of these, 361 cases (87.2%) showed a strong Ep-CAM expression. Epithelial cell adhesion molecule expression and stage or grade according to Gleason did not correlate. In univariate survival analysis, there was the expected significant correlation between Gleason score and survival in (P<0.0001). However, there was no correlation of Gleason score or survival with Ep-CAM expression.
Table 5. Expression of Ep-CAM in prostate carcinoma.
Epithelial cell adhesion molecule expression in lung cancers
In the lung cancer array, 1287 cases were analyzable (Table 6). On average, 64% of cases (n=823) showed a high Ep-CAM expression score. An intense staining signal was detected in 51% of cases (n=660). Squamous cell (53.6%, n=332), neuroendocrine (64.3%, n=36) and large cell carcinomas (67%, n=150) were expressing Ep-CAM less frequently at a high level than adenocarcinomas (80.8%, n=256) (P<0.0001). There was no association of stage or grade and Ep-CAM expression in any of the histological subgroups.
Table 6. Expression of Ep-CAM in lung carcinoma.
In univariate survival analysis, the expected significant correlation between tumour stage and survival was observed (P<0.0001). Because the different histological subgroups showed varying Ep-CAM expression, they were analysed separately. No definite correlations were found regarding Ep-CAM expression, grade and survival in any of the histological entities, although sample bias cannot be completely excluded as our tumour collective did not contain poorly differentiated tumours. There was a trend toward a longer survival in patients with adenocarcinomas, large cell and bronchioloalveolar carcinomas and strong Ep-CAM expression. This trend was inversed in SCC.
DISCUSSION
This is the largest analysis of Ep-CAM expression in major human malignancies performed to date. It employed a highly reproducible and standardised high-throughput array technology, which allows comparison of staining intensity and frequency for a large set of tissue samples. Comparability of IHC data within and across studies is frequently hampered by the use of distinct fixation, staining and antibody detection protocols. In addition, different antibodies are used in the literature to stain a particular target antigen. In the present analysis, all these parameters were kept constant. The use of high sample numbers, one of the main advantages of array technology, resulted in reaching statistically meaningful conclusions. With lung, colon, prostate and gastric cancers, we have selected four of the most frequent cancers in the industrialised world. Epithelial cell adhesion molecule expression in breast cancer has been previously published for more than 1700 patient samples (Gastl et al, 2000; Spizzo et al, 2002; Spizzo et al, 2004).
In primary tumours of colon, lung, prostate and stomach, Ep-CAM was on average significantly expressed in 94.1% of 3360 cases. In our analysis, Ep-CAM expression showed a tendency to be binary with the larger group consisting of tumours with high staining intensity on a major fraction of tumour cells, and a much smaller group expressing Ep-CAM only at weak or moderate levels, or not all. In well and poorly differentiated colon cancers, and lung and prostate cancer, no obvious correlation of Ep-CAM expression with survival, tumour stage or grade was observed. Gastric cancer could not be analysed for a correlation of Ep-CAM expression with survival because no patient survival data were available for this indication. Previous studies investigated the influence of Ep-CAM expression on survival in a number of other carcinoma. Epithelial cell adhesion molecule upregulation was an independent marker for poor survival in lymph node positive breast cancers (Spizzo et al, 2004), and gall bladder cancers (Varga et al, 2004). In contrast, improved survival was found associated with Ep-CAM upregulation in clear cell renal cell carcinoma (Kim et al, 2004; Seligson et al, 2004; Went et al, 2005), and gastric cancers (Songun et al, 2005). Here, we observed that survival of patients in the subgroup of moderately differentiated colon cancers also showed a significant positive correlation with Ep-CAM expression. Consistent with previous reports, we could not find an influence of Ep-CAM expression on patients' survival outcome in lung and prostate cancers (Poczatek et al, 1999; Piyathilake et al, 2000).
How can the effect of Ep-CAM overexpression on survival be so different depending on cancer indication, and for subgroups within a given indication? The emerging functional importance of Ep-CAM for tumour cells would be more consistent with the phenotype of breast and gall bladder cancers, where Ep-CAM overexpression is an independent predictor of poor survival (Spizzo et al, 2004; Varga et al, 2004). Overexpressed Ep-CAM was shown to provide a potent growth stimulus to tumour cells enabling proliferation (Munz et al, 2004), and led to an increased invasiveness and migration of tumour cells presumably due to E-cadherin antagonism (Litvinov et al, 1997; Osta et al, 2004). It is likely that Ep-CAM exerts the same functions in cells of primary tumours and metastases, which would well explain why Ep-CAM shows high-level and largely uniform expression on tumour cells of most patients with adenocarcinoma of lung, prostate, breast, colon, and gastric cancer. In many of these cancers, the fraction of Ep-CAM-negative tumours is very small. For instance, in the present study, only four out of 1186 colon cancer samples were Ep-CAM-negative. In breast cancer, the analytical situation was better because approximately 10% of tumours are Ep-CAM negative (Spizzo et al, 2004). Hence, despite very large sample numbers, it may be still difficult to accrue large enough sample populations for statistical comparison of Ep-CAM-negative with positive tumours. As a consequence, studies have to rely on comparing different expression levels of Ep-CAM, the accuracy of which is limited by the semiquantitative nature of immunohistochemical staining procedures.
A hallmark of tumour cells is de-differentiation, which typically goes along with the loss of expression of differentiation markers (Kiemer et al, 2001; Peinado et al, 2004). Epithelial cell adhesion molecule is an epithelial differentiation marker, which is frequently expressed on normal epithelial cells (Winter et al, 2003). Loss of Ep-CAM expression is therefore a likely consequence of tumour cell de-differentiation, as for instance is seen for the epithelial differentiation antigen E-cadherin (Sulzer et al, 1998). On the other hand, overexpression or maintenance of Ep-CAM expression on tumour cells relative to normal epithelia may then be an indication that its presence confers a benefit to tumour cells. The level of Ep-CAM expression on tumour cells will then reflect a balance of reduced expression due to de-differentiation and over- or maintained expression as a consequence of positive selection of a certain growth phenotype. The survival difference between patient populations with high and low Ep-CAM-expressing tumours should therefore be seen in light of an antagonism between de-differentiation and positive selection.
While both high and low Ep-CAM-expressing tumours may still benefit from growth-stimulatory and metastatic properties of Ep-CAM, the population of low and no Ep-CAM expressors may have undergone further de-differentiation events to a level were reduced expression or loss of Ep-CAM has been compensated for by overexpression of other growth-promoting proteins. Examples are growth factor receptors like HER-2 and EGFR, which in contrast to Ep-CAM, are upregulated as a consequence of gene amplification events (Simon et al, 2003; Al-Kuraya et al, 2004). Future studies are needed to explore whether reduced Ep-CAM expression or its loss is linked to a concomitant overexpression of other proteins with oncogenic potential. If this functional compensation is specific for tumour type, it could explain why Ep-CAM expression has such distinct effects on survival prognosis over different indications.
Its high-level, frequent and homogenous expression on human adenocarcinoma make Ep-CAM an ideal target for antibody-based immunotherapeutic approaches. Epithelial cell adhesion molecule is currently targeted by two principally different approaches in cancer therapy: passive and active immunotherapy. The first antibody used in passive immunotherapy was edrecolomab, a murine IgG2a antibody targeting Ep-CAM (Sears et al, 1984; Riethmuller et al, 1994). The therapeutic effect of this antibody administered alone or in combination with chemotherapy or GM-CSF (Mellstedt et al, 2000) was not conclusive, but it showed a very benign safety profile (Fields et al, 2002; Punt et al, 2002; Hartung et al, 2005). To reduce immunogenicity and enhance antibody-dependant cytotoxicity, complement dependant cytotoxicity and serum half-life, humanised antibodies ING-1 (de Bono et al, 2004), 3622W94 (Abdullah et al, 1999; Martin et al, 1999) and fully human IgG1 antibody MT201 (adecatumumab) (Naundorf et al, 2002; Brischwein et al, 2005) were developed. All showed much higher in vitro cytotoxic activity than edrecolomab, but the two high-affinity antibodies ING-1 and 3622W94 turned out to be much less tolerable than edrecolomab due to induction of acute pancreatitis. Conjugation of the Ep-CAM-specific murine monoclonal antibody 323/A3 human with beta-glucuronidase is a prodrug approach designed to locally augment the anti-tumour effect of doxorubicin (Houba et al, 2001). A fusion protein between a single-chain antibody and a bacterial toxin is currently being tested for local treatment of head and neck tumours in a phase I trial (Quenneville et al, 2005), and has shown extraordinary antitumour activity and potency in a xenograft model (Di Paolo et al, 2003). Epithelial cell adhesion molecule was also selected as target for bi- and trispecific antibody therapies. Three T-cell activating, single-chain bispecific antibodies were shown to potently eradicate established and disseminated tumours in immunodeficient and -competent mouse models (Peters et al, 2004; Brischwein et al, 2005; Schlereth et al, 2005a, 2005b), and a related bispecific antibody called E3Bi demonstrated high in-vitro cytotoxicity (Ren-Heidenreich et al, 2004). The trifunctional antibody catumaxomab (anti-Ep-CAM × anti-CD3) has been safely administered in a phase I/II study to patients suffering from malignant ascites (Stroehlein et al, 2005). Bispecific antibodies that link adenovirus to Ep-CAM are experimentally used in combination with recombinant adenoviral vectors for cancer gene therapy (Haisma et al, 1999), and adenoviral vectors expressing virus with an anti-Ep-CAM surface protein were also constructed (Oosterhoff et al, 2005).
One active immunotherapy approach is using IGN101 (formulated edrecolomab) for induction of anti-Ep-CAM anti-idiotypic antibodies (Zaloudik et al, 2002). This vaccination was shown to be safe, reduce Ep-CAM positive tumour cells in circulation and prolong survival of patients with metastatic rectal cancer (Himmler et al, 2005). Current experimental approaches are using the Ep-CAM promoter to control the expression of therapeutic genes (Gires et al, 2004), and short interfering RNA for the silencing of Ep-CAM expression, which resulted in a 35–80% decrease in proliferation of breast cancer cell lines (Osta et al, 2004). Lastly, the Ep-CAM protein is being used as a vaccine to elicit by various approaches the induction of specific T and B cell responses (Mosolits et al, 2004, 2005; Neidhart et al, 2004).
The emerging results from Ep-CAM-targeting immunotherapies show a wide utility of the target antigen. Although Ep-CAM is also expressed on normal epithelia, a lower expression there compared to tumour cells (Kim et al, 2004; Osta et al, 2004) and a possible sequestration of Ep-CAM between epithelial cells (McLaughlin et al, 2001) appears to open a therapeutic window. This is supported by the benign safety profile of certain Ep-CAM targeted therapies such as edrecolomab, adecatumumab and vaccination approaches with the autoantigen. In indications showing a strong correlation between Ep-CAM overexpression and poor survival prognosis, selective ablation of Ep-CAM positive cells by the above therapeutic approaches may translate into a survival benefit. In indications with a neutral or positive effect of Ep-CAM overexpression on survival, the high proportion of Ep-CAM positive cells in tumours may still be efficacious in particular if the targeted immunotherapy is combined with chemotherapeutics, and if used in adjuvant settings as are characterised by low tumour load.
References
- Abdullah N, Greenman J, Pimenidou A, Topping KP, Monson JR (1999) The role of monocytes and natural killer cells in mediating antibody-dependent lysis of colorectal tumour cells. Cancer Immunol Immunother 48: 517–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraya K, Schraml P, Torhorst J, Tapia C, Zaharieva B, Novotny H, Spichtin H, Maurer R, Mirlacher M, Kochli O, Zuber M, Dieterich H, Mross F, Wilber K, Simon R, Sauter G (2004) Prognostic relevance of gene amplifications and coamplifications in breast cancer. Cancer Res 64: 8534–8540 [DOI] [PubMed] [Google Scholar]
- Balzar M, Winter MJ, de Boer CJ, Litvinov SV (1999) The biology of the 17-1A antigen (Ep-CAM). J Mol Med 77: 699–712 [DOI] [PubMed] [Google Scholar]
- Brischwein K, Schlereth B, Guller B, Steiger C, Wolf A, Lutterbuese R, Offner S, Locher M, Urbig T, Raum T, Kleindienst P, Wimberger P, Kimmig R, Fichtner I, Kufer P, Hofmeister R, da Silva AJ, Baeuerle PA (2005) MT110: a novel bispecific single-chain antibody construct with high efficacy in eradicating established tumors. Mol Immunol; Epub ahead of print [DOI] [PubMed]
- Bubendorf L, Nocito A, Moch H, Sauter G (2001) Tissue microarray (TMA) technology: miniaturized pathology archives for high-throughput in situ studies. J Pathol 195: 72–79 [DOI] [PubMed] [Google Scholar]
- Cirulli V, Crisa L, Beattie GM, Mally MI, Lopez AD, Fannon A, Ptasznik A, Inverardi L, Ricordi C, Deerinck T, Ellisman M, Reisfeld RA, Hayek A (1998) KSA antigen Ep-CAM mediates cell–cell adhesion of pancreatic epithelial cells: morphoregulatory roles in pancreatic islet development. J Cell Biol 140: 1519–1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bono JS, Tolcher AW, Forero A, Vanhove GF, Takimoto C, Bauer RJ, Hammond LA, Patnaik A, White ML, Shen S, Khazaeli MB, Rowinsky EK, LoBuglio AF (2004) ING-1, a monoclonal antibody targeting Ep-CAM in patients with advanced adenocarcinomas. Clin Cancer Res 10: 7555–7565 [DOI] [PubMed] [Google Scholar]
- Di Paolo C, Willuda J, Kubetzko S, Lauffer I, Tschudi D, Waibel R, Pluckthun A, Stahel RA, Zangemeister-Wittke U (2003) A recombinant immunotoxin derived from a humanized epithelial cell adhesion molecule-specific single-chain antibody fragment has potent and selective antitumor activity. Clin Cancer Res 9: 2837–2848 [PubMed] [Google Scholar]
- Fields AF, Keller AM, Schwartzberg L, Bernard S, Pazdur R, Kardinal C, Cohen A, Schultz J, Eisenberg P, Barber L, Edmundson S, Wisse P (2002) Edrecolomab (17-1A antibody) (EDR) in combination with 5-fluorouracil (FU) based chemotherapy in the adjuvant treatment of stage III colon cancer: results of a randomised North American Phase III Study. J Clin Oncol 20: A508 [Google Scholar]
- Flieger D, Hoff AS, Sauerbruch T, Schmidt-Wolf IG (2001) Influence of cytokines, monoclonal antibodies and chemotherapeutic drugs on epithelial cell adhesion molecule (EpCAM) and LewisY antigen expression. Clin Exp Immunol 123: 9–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gastl G, Spizzo G, Obrist P, Dunser M, Mikuz G (2000) Ep-CAM overexpression in breast cancer as a predictor of survival. Lancet 356: 1981–1982 [DOI] [PubMed] [Google Scholar]
- Gires O, Kieu C, Fix P, Schmitt B, Munz M, Wollenberg B, Zeidler R (2001) Tumor necrosis factor alpha negatively regulates the expression of the carcinoma-associated antigen epithelial cell adhesion molecule. Cancer 92: 620–628 [DOI] [PubMed] [Google Scholar]
- Gires O, Pockl S, Chapman RD, Munz M (2004) Targeted gene expression using a 1.1 kilobase promoter fragment of the tumour-associated antigen EpCAM. Anticancer Res 24: 3715–3721 [PubMed] [Google Scholar]
- Haisma HJ, Pinedo HM, Rijswijk A, der Meulen-Muileman I, Sosnowski BA, Ying W, Beusechem VW, Tillman BW, Gerritsen WR, Curiel DT (1999) Tumor-specific gene transfer via an adenoviral vector targeted to the pan-carcinoma antigen EpCAM. Gene Therapy 6: 1469–1474 [DOI] [PubMed] [Google Scholar]
- Hartung G, Hofheinz RD, Dencausse Y, Sturm J, Kopp-Schneider A, Dietrich G, Fackler-Schwalbe I, Bornbusch D, Gonnermann M, Wojatschek C, Lindemann W, Eschenburg H, Jost K, Edler L, Hochhaus A, Queisser W (2005) Adjuvant therapy with edrecolomab vs observation in stage II colon cancer: a multicenter randomized phase III study. Onkologie 28: 347–350 [DOI] [PubMed] [Google Scholar]
- Herlyn M, Steplewski Z, Herlyn D, Koprowski H (1979) Colorectal carcinoma-specific antigen: detection by means of monoclonal antibodies. Proc Natl Acad Sci USA 76: 1438–1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmler G, Loibner H, Schuster M, Janzek E, Stranner S, Samonigg H (2003) Murine monoclonal antibody 17-1A used as vaccine antigen (IGN101): direct induction of anti-EpCAM antibodies by vaccination of cancer patients. Proc Am Soc Clin Oncol 22: A732 [Google Scholar]
- Himmler G, Settaf A, Groiss F, Eller N, Salzberg M, Kundi M, Eckert H, Loibner H, Samonigg H (2005) A randomized placebo-controlled phase-II-study with the cancer vaccine IGN101 in patients with epithelial cancers. J Clin Oncol 23: A2555 [Google Scholar]
- Houba PH, Boven E, van der Meulen-Muileman IH, Leenders RG, Scheeren JW, Pinedo HM, Haisma HJ (2001) Pronounced antitumor efficacy of doxorubicin when given as the prodrug DOX-GA3 in combination with a monoclonal antibody beta-glucuronidase conjugate. Int J Cancer 91: 550–554 [DOI] [PubMed] [Google Scholar]
- Jordinson M, El-Hariry I, Calnan D, Calam J, Pignatelli M (1999) Vicia faba agglutinin, the lectin present in broad beans, stimulates differentiation of undifferentiated colon cancer cells. Gut 44: 709–714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiemer AK, Takeuchi K, Quinlan MP (2001) Identification of genes involoved in epithelial-mesenchymal transition and tumor progression. Oncogene 20: 6679–6688 [DOI] [PubMed] [Google Scholar]
- Kim HL, Seligson D, Liu X, Janzen N, Bui MH, Yu H, Shi T, Figlin RA, Horvath S, Belldegrun AS (2004) Using protein expressions to predict survival in clear cell renal carcinoma. Clin Cancer Res 10: 5464–5471 [DOI] [PubMed] [Google Scholar]
- Kim JH, Herlyn D, Wong KK, Park DC, Schorge JO, Lu KH, Skates SJ, Cramer DW, Berkowitz RS, Mok SC (2003) Identification of epithelial cell adhesion molecule autoantibody in patients with ovarian cancer. Clin Cancer Res 9: 4782–4791 [PubMed] [Google Scholar]
- Litvinov SV, Balzar M, Winter MJ, Bakker HA, Briaire-de Bruijn IH, Prins F, Fleuren GJ, Warnaar SO (1997) Epithelial cell adhesion molecule (Ep-CAM) modulates cell–cell interactions mediated by classic cadherins. J Cell Biol 139: 1337–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litvinov SV, Velders MP, Bakker HA, Fleuren GJ, Warnaar SO (1994) Ep-CAM: a human epithelial antigen is a homophilic cell–cell adhesion molecule. J Cell Biol 125: 437–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin IG, Cutts SG, Birbeck K, Gray S, Quirke P (1999) Expression of the 17-1A antigen in gastric and gastro-oesophageal junction adenocarcinomas: a potential immunotherapeutic target? J Clin Pathol 52: 701–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin PM, Harmsen MC, Dokter WH, Kroesen BJ, van der Molen H, Brinker MG, Hollema H, Ruiters MH, Buys CH, de Leij LF (2001) The epithelial glycoprotein 2 (EGP-2) promoter-driven epithelial-specific expression of EGP-2 in transgenic mice: a new model to study carcinoma-directed immunotherapy. Cancer Res 61: 4105–4111 [PubMed] [Google Scholar]
- Mellstedt H, Fagerberg J, Frodin JE, Hjelm-Skog AL, Liljefors M, Markovic K, Mosolits S, Ragnhammar P (2000) Ga733/EpCAM as a target for passive and active specific immunotherapy in patients with colorectal carcinoma. Ann NY Acad Sci 910: 254–261 [DOI] [PubMed] [Google Scholar]
- Moldenhauer G, Momburg F, Moller P, Schwartz R, Hammerling GJ (1987) Epithelium-specific surface glycoprotein of Mr 34,000 is a widely distributed human carcinoma marker. Br J Cancer 56: 714–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosolits S, Markovic K, Fagerberg J, Frodin JE, Rezvany MR, Kiaii S, Mellstedt H, Jeddi-Tehrani M (2005) T-cell receptor BV gene usage in colorectal carcinoma patients immunised with recombinant Ep-CAM protein or anti-idiotypic antibody. Cancer Immunol Immunother 54: 557–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosolits S, Markovic K, Frodin JE, Virving L, Magnusson CG, Steinitz M, Fagerberg J, Mellstedt H (2004) Vaccination with Ep-CAM protein or anti-idiotypic antibody induces Th1-biased response against MHC class I- and II-restricted Ep-CAM epitopes in colorectal carcinoma patients. Clin Cancer Res 10: 5391–5402 [DOI] [PubMed] [Google Scholar]
- Munz M, Kieu C, Mack B, Schmitt B, Zeidler R, Gires O (2004) The carcinoma-associated antigen EpCAM upregulates c-myc and induces cell proliferation. Oncogene 23: 5748–5758 [DOI] [PubMed] [Google Scholar]
- Naundorf S, Preithner S, Mayer P, Lippold S, Wolf A, Hanakam F, Fichtner I, Kufer P, Raum T, Riethmuller G, Baeuerle PA, Dreier T (2002) In vitro and in vivo activity of MT201, a fully human monoclonal antibody for pancarcinoma treatment. Int J Cancer 100: 101–110 [DOI] [PubMed] [Google Scholar]
- Neidhart J, Allen KO, Barlow DL, Carpenter M, Shaw DR, Triozzi PL, Conry RM (2004) Immunization of colorectal cancer patients with recombinant baculovirus-derived KSA (Ep-CAM) formulated with monophosphoryl lipid A in liposomal emulsion, with and without granulocyte-macrophage colony-stimulating factor. Vaccine 22: 773–780 [DOI] [PubMed] [Google Scholar]
- Oosterhoff D, Overmeer RM, de Graaf M, van der Meulen IH, Giaccone G, van Beusechem VW, Haisma HJ, Pinedo HM, Gerritsen WR (2005) Adenoviral vector-mediated expression of a gene encoding secreted, EpCAM-targeted carboxylesterase-2 sensitises colon cancer spheroids to CPT-11. Br J Cancer 92: 882–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osta WA, Chen Y, Mikhitarian K, Mitas M, Salem M, Hannun YA, Cole DJ, Gillanders WE (2004) EpCAM is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Res 64: 5818–5824 [DOI] [PubMed] [Google Scholar]
- Peinado H, Portillo F, Cano A (2004) Transcritional regulation of cadherins during development and carcinomgenesis. Int J Dev Biol 48: 365–375 [DOI] [PubMed] [Google Scholar]
- Peters M, Dasilva A, Weckermann D, Oberneder R, Ebner B, Kirchinger P, Fetter A, Köhne-Volland R, Baeuerle PPG (2004) Phase I study of the novel fully human monoclonal antibody MT201, directed against epithelial cellular adhesion molecule (Ep-CAM), in patients with hormone-refractory prostate cancer (HRPC). J Clin Oncol 22: A2600 [Google Scholar]
- Piyathilake CJ, Frost AR, Weiss H, Manne U, Heimburger DC, Grizzle WE (2000) The expression of Ep-CAM (17-1A) in squamous cell cancers of the lung. Hum Pathol 31: 482–487 [DOI] [PubMed] [Google Scholar]
- Poczatek RB, Myers RB, Manne U, Oelschlager DK, Weiss HL, Bostwick DG, Grizzle WE (1999) Ep-Cam levels in prostatic adenocarcinoma and prostatic intraepithelial neoplasia. J Urol 162: 1462–1466 [PubMed] [Google Scholar]
- Prang N, Preithner S, Brischwein K, Goster P, Woppel A, Muller J, Steiger C, Peters M, Baeuerle PA, da Silva AJ (2005) Cellular and complement-dependent cytotoxicity of Ep-CAM-specific monoclonal antibody MT201 against breast cancer cell lines. Br J Cancer 92: 342–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punt CJ, Nagy A, Douillard JY, Figer A, Skovsgaard T, Monson J, Barone C, Fountzilas G, Riess H, Moylan E, Jones D, Dethling J, Colman J, Coward L, MacGregor S (2002) Edrecolomab alone or in combination with fluorouracil and folinic acid in the adjuvant treatment of stage III colon cancer: a randomised study. Lancet 360: 671–677 [DOI] [PubMed] [Google Scholar]
- Quak JJ, Van Dongen G, Brakkee JG, Hayashida DJ, Balm AJ, Snow GB, Meijer CJ (1990) Production of a monoclonal antibody (K 931) to a squamous cell carcinoma associated antigen identified as the 17-1A antigen. Hybridoma 9: 377–387 [DOI] [PubMed] [Google Scholar]
- Quenneville J, Fitsialos D, Rasamoelisolo M, Cross M, Glover N, MacDonald G (2005) A phase I open-label study to evaluate safety, tolerability and pharmacokinetic (PK) profile of VB4-845, an anti-EpCAM immunotoxin, in subjects with SCCHN. J Clin Oncol 23: A5539 [Google Scholar]
- Ren-Heidenreich L, Davol PA, Kouttab NM, Elfenbein GJ, Lum LG (2004) Redirected T-cell cytotoxicity to epithelial cell adhesion molecule-overexpressing adenocarcinomas by a novel recombinant antibody, E3Bi, in vitro and in an animal model. Cancer 100: 1095–1103 [DOI] [PubMed] [Google Scholar]
- Riethmuller G, Gruber R, Schneider-Gädicke E, Schlimok G, Witte J, Raab R, Pichlmayer R, Pichlmaier H, Schmiegel W, Buggisch P, Höffken K, Hirche H, German Cancer Aid 17-1A Study Group (1994) Randomised trial of monoclonal antibody for adjuvant therapy of resected Dukes' C colorectal carcinoma. German Cancer Aid 17-1A Study Group. Lancet 343: 1177–1183 [DOI] [PubMed] [Google Scholar]
- Schlereth B, Fichtner I, Lorenczewski G, Kleindienst P, Brischwein K, da Silva A, Kufer P, Lutterbuese R, Junghahn I, Kasimir-Bauer S, Wimberger P, Kimmig R, Baeuerle PA (2005a) Eradication of tumors from a human colon cancer cell line and from ovarian cancer metastases in immunodeficient mice by a single-chain Ep-CAM-/CD3-bispecific antibody construct. Cancer Res 65: 2882–2889 [DOI] [PubMed] [Google Scholar]
- Schlereth B, Kleindienst P, Fichtner I, Lorenczewski G, Brischwein K, Lippold S, Silva AD, Locher M, Kischel R, Lutterbuse R, Kufer P, Baeuerle PA (2005b) Potent inhibition of local and disseminated tumor growth in immunocompetent mouse models by a bispecific antibody construct specific for Murine CD3. Cancer Immunol Immunother 27: 1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears HF, Herlyn D, Herlyn M, Steplewski Z, Grotzinger P, Koprowski H (1982) Ex vivo perfusion of human colon with monoclonal anticolorectal cancer antibodies. Cancer 49: 1231–1235 [DOI] [PubMed] [Google Scholar]
- Sears HF, Herlyn D, Steplewski Z, Koprowski H (1984) Effects of monoclonal antibody immunotherapy on patients with gastrointestinal adenocarcinoma. J Biol Response Mod 3: 138–150 [PubMed] [Google Scholar]
- Seligson DB, Pantuck AJ, Liu X, Huang Y, Horvath S, Bui MH, Han KR, Correa AJ, Eeva M, Tze S, Belldegrun AS, Figlin RA (2004) Epithelial cell adhesion molecule (KSA) expression: pathobiology and its role as an independent predictor of survival in renal cell carcinoma. Clin Cancer Res 10: 2659–2669 [DOI] [PubMed] [Google Scholar]
- Simon R, Atefy R, Wagner U, Forster T, Fijan A, Bruderer J, Wilber K, Mihatsch MJ, Gasser T, Sauter G (2003) HER-2 and TOP2A coamplification in urinary bladder cancer. Int J Cancer 107: 764–772 [DOI] [PubMed] [Google Scholar]
- Songun I, Litvinov SV, van de Velde CJ, Pals ST, Hermans J, van Krieken JH (2005) Loss of Ep-CAM (CO17-1A) expression predicts survival in patients with gastric cancer. Br J Cancer 92: 1767–1772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spizzo G, Obrist P, Ensinger C, Theurl I, Dunser M, Ramoni A, Gunsilius E, Eibl G, Mikuz G, Gastl G (2002) Prognostic significance of Ep-CAM and Her-2/neu overexpression in invasive breast cancer. Int J Cancer 98: 883–888 [DOI] [PubMed] [Google Scholar]
- Spizzo G, Went P, Dirnhofer S, Obrist P, Simon R, Spichtin H, Maurer R, Metzger U, von Castelberg B, Bart R, Stopatschinskaya S, Kochli OR, Haas P, Mross F, Zuber M, Dietrich H, Bischoff S, Mirlacher M, Sauter G, Gastl G (2004) High Ep-CAM expression is associated with poor prognosis in node-positive breast cancer. Breast Cancer Res Treat 86: 207–213 [DOI] [PubMed] [Google Scholar]
- Stroehlein MA, Lordick F, Ruettinger D, Gruetzner U, Menzel H, Bartelheim K, Jaeger M, Lindhofer H, Jauch K, Peschel C, Heiss MM (2005) Treatment of peritoneal carcinomatosis due to GI-tract cancer by intraperitoneal application of the trifunctional antibody catumaxomab (anti-EpcAM x anti-CD3): results of a phase I/II trial. J Clin Oncol 23: A2529 [Google Scholar]
- Sulzer M, Leers M, van NJ, Bollen E, Theunissen P (1998) Reduced E-cadherin expression is associated with increased lymph node metastasis and unfavorable prognosis in non-small cell lung cancer. Am J Respir Crit Care Med 157: 1319–1323 [DOI] [PubMed] [Google Scholar]
- Thurmond LM, Stimmel JB, Ingram AC, Ryan CH, Murray DM, Eberwein DJ, Witherspoon SM, Knick VC (2003) Adenocarcinoma cells exposed in vitro to Navelbine or Taxol increase Ep-CAM expression through a novel mechanism. Cancer Immunol Immunother 52: 429–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga M, Obrist P, Schneeberger S, Muhlmann G, Felgel-Farnholz C, Fong D, Zitt M, Brunhuber T, Schafer G, Gastl G, Spizzo G (2004) Overexpression of epithelial cell adhesion molecule antigen in gallbladder carcinoma is an independent marker for poor survival. Clin Cancer Res 10: 3131–3136 [DOI] [PubMed] [Google Scholar]
- Went P, Dirnhofer S, Salvisberg T, Amin MB, Lim SD, Diener PA, Moch H (2005) Expression of epithelial cell adhesion molecule (EpCam) in renal epithelial tumors. Am J Surg Pathol 29: 83–88 [DOI] [PubMed] [Google Scholar]
- Went PT, Lugli A, Meier S, Bundi M, Mirlacher M, Sauter G, Dirnhofer S (2004) Frequent EpCam protein expression in human carcinomas. Hum Pathol 35: 122–128 [DOI] [PubMed] [Google Scholar]
- Winter MJ, Nagtegaal ID, van Krieken JH, Litvinov SV (2003) The epithelial cell adhesion molecule (Ep-CAM) as a morphoregulatory molecule is a tool in surgical pathology. Am J Pathol 163: 2139–2148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaloudik J, Li W, Jacob L, Kieny MP, Somasundaram R, Acres B, Song H, Zhang T, Li J, Herlyn D (2002) Inhibition of tumor growth by recombinant vaccinia virus expressing GA733/CO17-1A/EpCAM/KSA/KS1-4 antigen in mice. Cancer Gene Ther 9: 382–389 [DOI] [PubMed] [Google Scholar]
- Zellweger T, Ninck C, Bloch M, Mirlacher M, Koivisto PA, Helin H, Mihatsch M, Gasser T, Bubendorf L (2005) Expression patterns of potential therapeutic targets in prostate cancer. Int J Cancer 113: 619–628 [DOI] [PubMed] [Google Scholar]
- Zimmermann S, Wels W, Froesch BA, Gerstmayer B, Stahel RA, Zangemeister-Wittke U (1997) A novel immunotoxin recognising the epithelial glycoprotein-2 has potent antitumoural activity on chemotherapy-resistant lung cancer. Cancer Immunol Immunother 44: 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]