Abstract
Chemokine (C-C motif) ligand-2 (CCL2) is a chemoattractant and activator of macrophages and is a key determinant of the macrophage infiltrate into tumours. We demonstrate here that CCL2 is expressed in normal human ovarian surface epithelium (HOSE) cells and is silenced in most ovarian cancer cell lines, and silenced or downregulated in the majority of primary ovarian adenocarcinomas. Analysis of the CCL2 locus at 17q11.2–q12 showed loss of heterozygosity (LOH) in 70% of primary tumours, and this was significantly more common in tumours of advanced stage or grade. However, we did not detect any mutations in the CCL2 coding sequence in 94 primary ovarian adenocarcinomas. These data support the hypothesis that CCL2 may play a role in the pathobiology of ovarian cancers, but additional studies will be required to evaluate this possibility.
Keywords: ovarian adenocarcinoma, CCL2, MCP-1, 5-aza-2′-deoxycytidine, SSCP, in situ hybridisation
Ovarian cancer is the leading cause of death from gynaecological neoplasias, and the sixth most common cancer among women worldwide (Parkin et al, 1999). The lack of symptoms during the early stages of the disease results in the majority of women presenting with advanced tumours that do not respond well to treatment. Consequently, the overall 5-year survival rate is only 30%. Most ovarian cancers, the adenocarcinomas, arise as a consequence of the accumulation of genetic or epigenetic inactivation of tumour suppressor genes and activation of oncogenes in the ovarian surface epithelium (OSE) (reviewed in Aunoble et al, 2000; Liu and Ganesan, 2002). Ovarian neoplasms occur in benign, low malignant potential (LMP) and malignant forms although the relationship between these forms is not clear, nor are the genetic and biological events that underlie the initiation and progression of ovarian adenocarcinomas.
Ovarian tumours may contain a significant number of infiltrating host leukocytes, and in the case of ovarian cancers, these are predominantly macrophages and T cells (Merogi et al, 1997; Negus et al, 1997). The likely stimulus for the presence of these leukocytes is the local production of chemokines. Chemokines are a family of small, secreted, proinflamatory cytokines with chemotactic activity against leukocytes (Oppenheim et al, 1991). In particular, chemokine (C-C motif) ligand 2 (CCL2, previously known as monocyte chemotactic protein-1, MCP-1), which is a potent chemoattractant for macrophages (Sica et al, 1990), and also T cells (Taub et al, 1995), has been found to be expressed in ovarian tumours (Negus et al, 1995; Burke et al, 1996) and appears to be an important determinant of the leukocyte infiltrate into tumours (Zacchariae et al, 1990; Rollins, 1991; Bottazzi et al, 1992; Negus et al, 1997; Zhang et al, 1997).
However, the role of these tumour-associated leukocytes remains unclear (Mantovani et al, 1992; Mantovani, 1994; O'Sullivan and Lewis, 1994). It is known that they can mount an immune response against malignant cells and kill them (Parmiani et al, 1990; Rollins and Sunday, 1991; Colombo et al, 1992; Peoples et al, 1995; Goedegebuure et al, 1997) and, indeed, the presence of intratumoural T cells in ovarian cancer patients has been shown to be significantly associated with increased progression-free and overall survival (Zhang et al, 2003). On the other hand, macrophages can produce factors that help tumour growth and/or vascularisation through paracrine loops (Malik and Balkwill, 1991; Mantovani et al, 1992). The particular role of these cells in a given case depends on factors such as the activation state of the macrophages and the intrinsic properties of the tumour cell, and is known as the macrophage balance (Mantovani, 1994).
Using cDNA array screening of normal OSE cells and ovarian cancer cell lines, we previously identified CCL2 as a gene whose expression is downregulated or lost in ovarian cancer cell lines (Arnold et al, 2001a). In this report, we describe the characterisation of CCL2 expression in a larger panel of ovarian cancer cell lines and primary tumours and mutation analysis of the CCL2 gene in primary ovarian adenocarcinomas.
MATERIALS AND METHODS
Cell lines, OSE cultures and primary tumours
Human ovarian surface epithelial cell lines (HOSE) 17.1 and 1.1, immortalised with a replication-defective retroviral construct expressing human papillomavirus oncogenes (Tsao et al, 1995), were maintained in a medium composed of 1 : 1 M199 : MCDB105 with 10% FCS. The HEY (Buick et al, 1985) and OVCAR4, OVCAR5 and OVCAR8 (kind gift from Dr E Marshall, Auckland Cancer Society) and OVHS-1 (kind gift of Dr N Ahmed, Royal Women's Hospital, Melbourne) ovarian cancer cell lines were maintained in MEM alpha medium with 10% FCS. OAW 42 (Wilson, 1984), OAW 28+53 (Wilson et al, 1987), PEO1 and PEO4 (Wolf et al, 1987), PEO14 (Langdon et al, 1988), JAM (Ward et al, 1987), SKOV3 (Fogh and Trempe, 1975), COLO316 (Woods et al, 1979), CAOV3 (Wong et al, 1999), OVCAR-3 (Hamilton et al, 1983), A2780 (established by Dr S Aaronson, National Cancer Institute), CI80135 and 27/87 (established by T Hurst, Obstetrics and Gynecology, Royal Brisbane Hospital) were all maintained in RPMI 1640 with 10% FCS. OVCA420, OVCA432, OVCA433 and DOV13 (kind gifts from Dr S Mok, Laboratory of Gynecologic Oncology, Brigham and Women's hospital, Boston, MA, USA) were maintained in a mixture of 1 : 1 MCDB105 and M199 with 10% FCS.
Cells were harvested for RNA at about 80% confluence. The cell lines OAW42, PEO1, PEO4, PEO14, JAM, SKOV3 and COLO316 were derived from serous tumours, and 27/87 was from an endometrioid tumour. The histological origin of the remaining cell lines is not available.
Uncultured HOSE cells were obtained by scraping stromal cells away from epithelial sheets. Their distinctive cellular morphology was used to confirm that the cells were epithelial. RNA was extracted directly from these peeled epithelial cells without culturing.
Ovarian adenocarcinomas were obtained from 97 patients undergoing surgery. There were 68 serous tumours, 13 endometrioid tumours, nine mucinous tumours, five clear-cell tumours and two tumours of mixed histology. The series included one benign and 10 LMP tumours as well as 86 malignant tumours. All patients were staged at laparotomy, in accordance with the recommendations of the International Federation of Gynaecology and Obstetrics (FIGO). Of the LMP tumours, five were FIGO stage 1 and four were stage 3 (one was of unknown stage) and of the malignant tumours, seven were FIGO stage 1, five stage 2, 66 stage 3 and eight stage 4. Constitutional DNA was available in all cases from peripheral blood.
Isolation of DNA and RNA
Tumour tissue was dissected free from necrotic and connective tissue, and mechanically dispersed prior to collagenase treatment (0.1 mg ml−1 in Hanks balanced salt solution). Erythrocytes and necrotic cells were removed with ficoll-paque, and genomic DNA was extracted by the salting-out method as described elsewhere (Miller et al, 1988). Total RNA was extracted from fresh primary tumours and subconfluent cultured cell lines using Tri-reagent (Sigma, Castle Hill, NSW), following the manufacturers' instructions. PolyA+ RNA was prepared from total RNA using Dynabeads (Dynal, Carlton South, Vic), according to the recommended protocol.
Northern blot analysis
RNA was denatured and electrophoresed on a formaldehyde–agarose gel and transferred onto a nylon membrane by capillary blotting overnight according to standard protocols (Sambrook and Russell, 2001). The RNA was then fixed to the membrane by UV irradiation. Probes were prepared from RT–PCR products by random priming and hybridisation was carried out for 2 h in ExpressHyb solution (Clontech, Palo Alto, CA, USA) at 65°C and then the membrane was subjected to standard washing procedures and autoradiography.
Semiquantitative RT–PCR
cDNA synthesis was carried out with the Superscript II reverse transcriptase on 1 μg of total RNA primed with random hexamers. RT–PCR was performed with primers for both CCL2 and β-actin in a multiplex reaction in a total volume of 20 μl incorporating 33P-labelled dATP using standard PCR cycling conditions with annealing at 60°C. The reaction was stopped and 5 μl of product removed at cycles 24, 28, 32 and 36 to ensure linear amplification and the products were run on a denaturing acrylamide gel prior to autoradiography. The primer sequences for both CCL2 (CTAAGCTTCCAGCATGAAAGTCTCTGG and GTGAGTGTTCAAGTCTTCG) and β-actin (CGTGACATTAAGGAGAAGCTGTGC and CTCAGGAGGAGCAATGATCTTGAT) spanned at least one intron to ensure quantitation was assessed only on amplified cDNA.
mRNA in situ hybridisation (ISH)
The CCL2 full-length cDNA was subcloned into pGEM-T vector (Promega, Annandale, NSW). Digoxigenin-labelled riboprobes for sense and antisense orientations were produced by in vitro transcription with SP6 and T7 RNA polymerases (Roche, Mannheim, Germany) as previously described (Ramm et al, 1998) and then subjected to alkaline hydrolysis. Sections were deparaffinised with xylene, rehydrated in an alcohol gradient and subjected to hydrochloric acid (0.2 mol l−1), as previously described (Rex and Scotting, 1994). Sections were permeabilised with 20 μg ml−1 proteinase K for 15 min at 37°C and fixed in 4% paraformaldehyde for 20 min at room temperature. Prehybridisation (4 × SSC/50% (v v−1) formamide) was performed at 42°C for 4 h followed by hybridisation for 18 h at 42°C with digoxigenin-labelled riboprobe at a concentration of 1 μg ml−1 in a solution of 40% (v v−1) formamide, 10% (w v−1) dextran sulphate, 1 × Denhardt's solution, 4 × SSC, 10 mM DTT and 1 mg ml−1 yeast tRNA.
Sections were washed to remove unbound probe and then incubated with alkaline phosphatase-conjugated antidigoxigenin polyclonal sera (1 : 100) (Roche, Mannheim, Germany) at room temperature for 2 h. Unbound antibody was removed by washing, followed by visualisation with nitroblue tetrazolium chloride/5-bromo-4-chloro-3-indolyl phosphate (Roche, Mannheim, Germany) in the dark at room temperature for 18 h. Unbound complex was removed by washing and sections were counterstained with eosin. Sections were visualised with a Nikon Eclipse E800 microscope and photographed with a Nikon DXM1200F digital camera.
Loss of heterozygosity (LOH) analyses
Loss of heterozygosity was assessed at 17q11.2–q12 with the D17S1293 and D17S933 microsatellite markers, which are located 0.02 Mb proximal and 0.61 Mb distal to CCL2 at 32.73 Mb (www.ncbi.nlm.nih.gov/). PCR amplification was carried out for 35 cycles in the presence of 33P-labelled dATP and PCR products were analysed on a denaturing polyacrylamide gel. Loss of heterozygosity was scored conservatively as a clear reduction in the intensity of one allele (>70%) by two independent observers, one of whom was blind with respect to the sample identity.
Single-strand conformation polymorphism analysis
Primers were designed to intronic regions to amplify each of the three coding exons of the human CCL2 gene. A total of 94 primary ovarian tumours obtained prior to chemotherapy were screened and constitutional DNA from blood was available for all. DNA samples were amplified in the presence of 33P-labelled dATP using standard PCR cycling conditions with annealing at 60°C, denatured at 95°C for 5 min and then electrophoresed on 0.5 × MDE (FMC Biotech, Rockland, Maine) gel overnight at room temperature.
The primers used for SSCP and product sizes were: exon 1 CAATAAGAGGCAGAGACAGCAGCCAG and GTTAAAGCAAGACTGTGGGTACCACG (273 bp); exon 2 GCTCTTTCTCTTCTCCTGCCTGC and GAGGCTTGTCCCTTGCTCCACAAGG (300 bp); exon 3 CCTCCTAGTCTCCATGGCAGCTCGC and ACAGGGTGTCTGGGGAAAGCTAGG (253 bp). PCR products amplified from these primers span all coding exons of the CCL2 gene and include sequences 72 bp upstream of the start codon, 44 bp downstream of the stop codon and at least 40 bp of flanking intronic sequences exclusive of the primers.
5-aza-2′-deoxycytidine treatment of ovarian adenocarcinoma cell lines
Cell lines were plated at 20–30% confluence and treated 24 h later (day 0) with 0, 0.5 or 2.0 μM 5-aza-2′-deoxycytidine. Fresh media containing the same concentration of 5-aza-2′-deoxycytidine was added on day 2 and cells were harvested for RNA extraction on day 5.
RESULTS
CCL2 expression analysis in ovarian adenocarcinoma cell lines
We previously conducted a screen for genes aberrantly expressed in three ovarian adenocarcinoma cell lines compared to an immortalised HOSE using a human cDNA array containing 588 known genes (Arnold et al, 2001a). This showed that expression of CCL2 is greatly reduced in ovarian cancer cell lines. This finding was confirmed using semiquantitative RT–PCR analysis which showed that CCL2 was expressed in both of the HOSE cell lines tested, while three out of four ovarian cancer cell lines did not express and one out of four had reduced levels of expression (Arnold et al, 2001a).
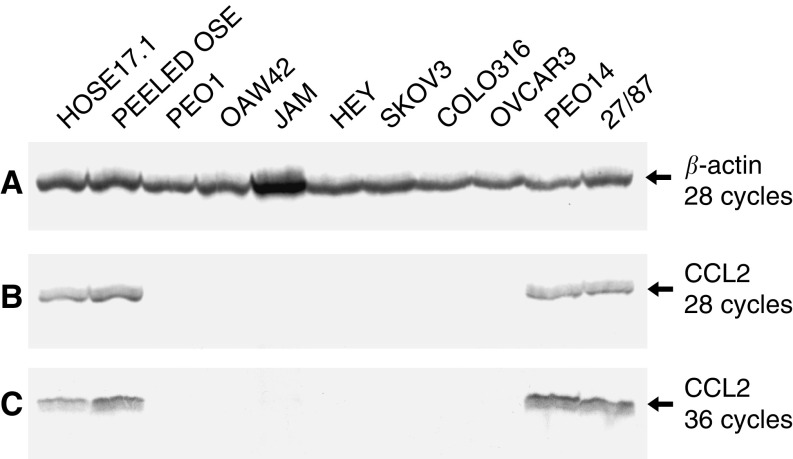
To further extend these results, semiquantitative RT–PCR was repeated to include peeled (uncultured) normal OSE cells as well as the HOSE17.1 cell line and a broader panel of ovarian cancer cell lines. Expression of CCL2 was detected at similar levels in the HOSE17.1 cell line, the uncultured normal OSE cells, and the PEO14 and 27/87 ovarian cancer cell lines (Figure 1A, B). No CCL2 expression was detected in the remaining seven ovarian adenocarcinoma cell lines, even after 36 rounds of PCR amplification (Figure 1C).
Figure 1.
Analysis of CCL2 expression in immortalised HOSE cells, peeled (uncultured) OSE cells and ovarian adenocarcinoma cell lines by RT–PCR. Multiplex PCR was carried out for CCL2 and β-actin on cDNA, run on a polyacrylamide gel, and exposed to film. (A) PCR products for β-actin after 28 cycles of amplification. (B) PCR products for CCL2 after 28 cycles of amplification. (C) PCR products for CCL2 after 36 cycles of amplification.
The expression of CCL2 mRNA was next examined in a larger panel of HOSE and ovarian cancer cell lines by Northern blot analysis (Figure 2). Strong expression was detected in the HOSE17.1 and HOSE1.1 cell lines, while much weaker expression was found in the PEO14 and 27/87 cell lines. No expression was detected in the remaining 16 ovarian adenocarcinoma cell lines.
Figure 2.
Analysis of CCL2 expression in HOSE and ovarian adenocarcinoma cell lines by Northern blotting. Each lane represents 2 μg of polyA+ RNA. (A) Hybridisation with the CCL2 probe. (B) Hybridisation with the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) probe.
CCL2 expression analysis in primary ovarian adenocarcinomas
Having demonstrated that CCL2 is strongly expressed in cultured and uncultured HOSE cells, and that expression is lost or reduced in the vast majority of ovarian cancer cell lines, we next investigated its expression in primary ovarian tumours. Northern blot analysis of the HOSE17.1 cell line and 13 primary adenocarcinomas revealed greatly reduced levels of expression in two primary tumours (35 out of 90 and 33 out of 91) compared to the HOSE17.1 cells, while no expression was detected in the remaining 11 primary tumours (Figure 3).
Figure 3.
Analysis of CCL2 expression in ovarian primary adenocarcinomas by Northern blotting. Lane 1, HOSE17.1 cell line; lanes 2–9, ovarian serous adenocarcinomas; lanes 10–13 ovarian endometrioid adenocarcinomas; lane 14 mucinous ovarian adenocarcinoma. Each lane represents 5 μg of total RNA. (A) Hybridisation with the CCL2 probe. (B) Hybridisation with the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) probe.
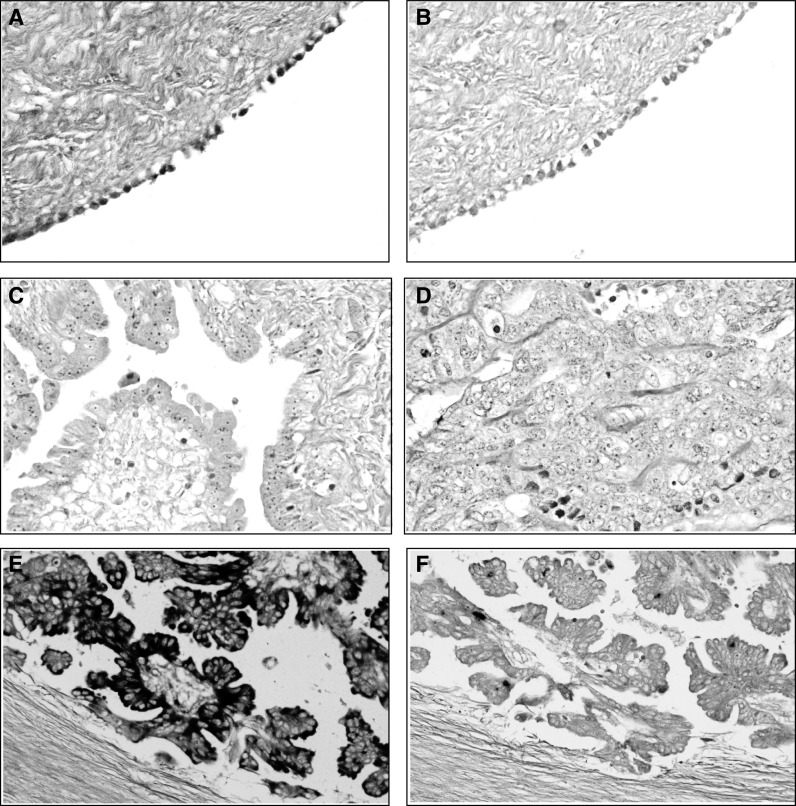
To further investigate the extent and localisation of CCL2 expression in primary ovarian tumours, we used mRNA ISH to analyse two normal ovaries and 13 primary adenocarcinomas. This series included nine adenocarcinomas that we had previously investigated by Northern blot. A pathologist (MC) scored the percent of expressing cells into categories. No CCL2 expression was detected in the stroma of any of the tumours. Four tumours expressed CCL2 in 0–5% of epithelial cells, six tumours expressed CCL2 in 6–25% of epithelial cells, while only three tumours expressed CCL2 in greater than 25% of the epithelial cells. In the normal ovaries, CCL2 expression was detected in 60–80% of the surface epithelial cells and also epithelial cells lining invaginations and inclusion cysts. Representative photomicrographs of CCL2 staining in a normal ovary and three tumours are shown in Figure 4.
Figure 4.
In situ hybridisation of CCL2 in ovarian tumours and normal ovaries. Normal ovary hybridised with (A) antisense CCL2 probe (× 40) and (B) sense control probe (× 40) showing staining in the majority of surface epithelial cells. Ovarian adenocarcinomas hybridised with antisense CCL2 probe (C, D, E) or sense control probe (F). Tumours 97/93 (C, × 40) and 99/93 (D, × 40) show very little staining for CCL2. Ovarian adenocarcinoma 52/92 hybridised with (E) antisense CCL2 probe (× 40) and (F) sense control probe (× 20). The majority of 52/92 tumour cells in this field show CCL2 expression.
There were nine tumours, which were analysed by both ISH and Northern blot. Of the seven tumours in which expression was not detected by Northern blot, six had less than 25% epithelial cells expressing, while one (61 out of 93) had 26–50%, and of the two which did show expression on the Northern blot, one tumour was scored as having 50–75% expression while the other was scored as 6–25%. The lack of correlation between these two methods in tumour 61 out of 93 is probably due to tumour heterogeneity, since the sections used for ISH were not adjacent to the tissue used to isolate RNA.
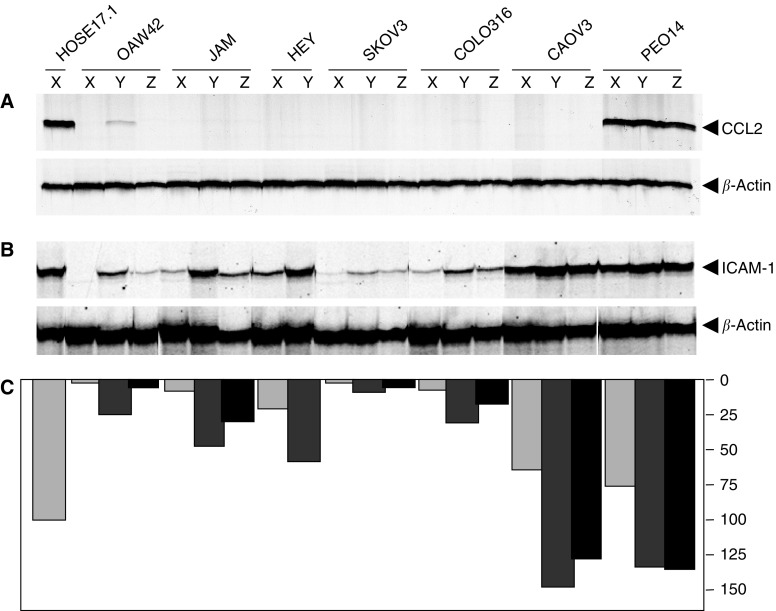
5-azacytidine treatment of cell lines
To test whether the silencing of CCL2 expression in the ovarian cancer cell lines is related to hyper-methylation of CpG dinucleotides, we treated cell lines with 0, 0.5 or 2.0 μM of the methyltransferase inhibitor 5-azacytidine. RNA was extracted from the cultures after 5 days and the level of expression of CCL2 was examined by semiquantitative RT–PCR (Figure 5). Consistent with previous results, the untreated controls showed no CCL2 expression in the OAW42, JAM, HEY, SKOV3, COLO316 or CAOV3 cell lines, while strong expression was observed in the PEO14 cells. There was a slight induction of CCL2 expression in the OAW42 cell line treated with 0.5 μM 5-azacytidine, but no induction of expression in any of the other six cell lines (Figure 5A). Previous analysis of the same RNA samples for ICAM-1 expression (Arnold et al, 2001b) showed induction of ICAM-1 in cell lines treated with 5-azacytidine, demonstrating that the 5-azacytidine treatment was successful (Figure 5B, C).
Figure 5.
Analysis of CCL2 expression in ovarian cancer cell lines following treatment with 5-azacytidine. Cell lines were treated with 0 (X), 0.5 (Y) or 2.0 (Z) μM 5-azacytidine and RNA harvested 5 days later. (A) Multiplex PCR carried out with primers for β-actin and CCL2 for 28 cycles. (B) Multiplex PCR carried out with primers for β-actin and ICAM-1 as previously described (Arnold et al, 2001b). (C) Quantitation of intensity of bands for ICAM-1 normalised to β-actin.
Loss of heterozygosity analysis at 17q11.2–q12
Loss of heterozygosity analysis was carried out on 41 ovarian adenocarcinomas with the D17S1293 and D17S933 microsatellite markers, which are located 0.02 Mb proximal and 0.61 Mb distal to CCL2 at 32.73 Mb (www.ncbi.nlm.nih.gov/). Loss of heterozygosity was detected in 19 out of 27 (70%) informative cases for D17S1293 and 19 out of 26 (73%) informative cases for D17S933. Overall, LOH was detected in at least one marker in 22 out of 32 (69%) of informative cases. The LOH was significantly more common in Stage 3–4 tumours than Stage 1–2 tumours (P=0.03, Fisher's exact test), and tended to occur in tumours of advanced grade (P=0.058, Mantel–Haenszel χ2 test for trend). Of the informative tumours that did not express CCL2 by Northern blot, six had LOH and one had no loss, while one tumour that did express CCL2 also had LOH. Similarly, of the informative tumours that had 0–25% cells positive for CCL2 by ISH, four had LOH and two had no loss, while there were two tumours with greater than 26% of cells positive that both had LOH.
Mutation analysis of the CCL2 gene
Single-strand conformation polymorphism (SSCP) analysis was carried out on all three exons of the CCL2 gene, including sequences 72 bp upstream of the start codon and 44 bp downstream of the stop codon and at least 40 bp of flanking intronic sequences surrounding each exon. There were no aberrant bands detected in the PCR of any exon of CCL2 in the panel of 94 primary ovarian adenocarcinomas tested.
DISCUSSION
We first detected CCL2 as a gene whose expression is downregulated in ovarian adenocarcinoma cell lines relative to OSE cells by cDNA array (Arnold et al, 2001a). Further analysis of CCL2 expression presented here confirms that it is strongly expressed in peeled (uncultured) normal HOSE cells and immortalised cell lines derived from OSE cells. Expression is silenced in most ovarian cancer cell lines and silenced or downregulated in the majority of ovarian primary adenocarcinomas. This suggests that a selective advantage may result from downregulation of CCL2 expression, consistent with a role of CCL2 in the pathobiology of ovarian cancer.
A previous study of CCL2 expression in seven ovarian cancer cell lines by RT–PCR and ELISA, found the highest levels in PEO14 and HL60, with lower levels in OVCAR3, PEO1 and PEO4 and barely detectable expression in SKOV3 and PEA2 cells (Negus et al, 1995). This is consistent with our results in which we also found high levels of CCL2 mRNA in PEO14 and no expression in most other cell lines. In primary tumours, mRNA ISH showed expression of CCL2 in an average of 1.4% of cells in 23 out of 26 primary ovarian tumours, and ELISA detected CCL2 protein in ascites from ovarian cancer patients with a mean level of 4.28 ng ml−1 (Negus et al, 1995). This is also consistent with our Northern blot results, although we detected higher levels of expression than Negus et al by ISH. The same study did not detect CCL2 mRNA in the normal ovarian mesothelium (OSE), which was examined in only one case. In contrast, we have demonstrated strong expression in both cultured immortalised and uncultured OSE cells by RT–PCR, Northern blotting and ISH. This is an important new finding and demonstrates that CCL2 expression is silenced or downregulated in the majority of ovarian cell lines and primary tumours.
Expression of CCL2 has also been found to be decreased in prostate adenocarcinoma compared to benign prostate hyperplasia (Mazzucchelli et al, 1996) and cervical carcinomas compared to normal or hyperplastic squamous epithelium (Riethdorf et al, 1998; Kleine-Lowinski et al, 1999). In contrast, CCL2 expression has been found to be increased in malignant glioma (Kuratsu et al, 1993; Takeshima et al, 1994), primary and metastatic melanoma (Graves et al, 1992) and glioblastomas and astrocytomas (Desbaillets et al, 1994) compared to corresponding normal tissues. CCL2 expression has also been found to be increased in paclitaxel resistant cell lines and in the serum of ovarian cancer patients following paclitaxel treatment (Duan et al, 1999; Penson et al, 2000). However, rather than being associated with paclitaxel resistance, it is postulated that the increased CCL2 expression may simply reflect stress in the host (Penson et al, 2000).
To investigate the mechanism of downregulation of expression of CCL2, we treated a panel of ovarian cancer cell lines with the methyltransferase inhibitor 5-azacytidine. This resulted in a small increase in expression levels in only the OAW42 cell line, while there was no induction of expression in the other six. This suggests that hypermethylation of CpG islands near the CCL2 gene is not the major cause of the silencing of expression. Indeed, a search of the CCL2 genomic region from 7 kb upstream of the start codon to 2.5 kb downstream of the stop codon (GenBank Accession Number Y18933) using Cpgplot (www.angis.org.au) did not detect any CpG islands, which further supports our findings.
We next investigated whether genetic changes may be responsible for the downregulation of CCL2 expression. There was no evidence of any mutations in the CCL2 gene in 94 primary ovarian adenocarcinomas, demonstrating that CCL2 is not inactivated by somatic mutations, nor is downregulation of its expression the result of mutation in the coding or adjacent flanking sequences. There are five single-nucleotide polymorphisms reported within the CCL2 locus (http://www.ncbi.nih.gov/SNP/); however, only two of these were within the region screened for mutations and each of these had minor allele frequencies of less than 0.5% so it is not surprising that these were not detected within the 94 ovarian cancer samples we screened.
An overall LOH frequency of 69% was detected at the CCL2 locus at 17q11.2–q12, but there was no association with loss of CCL2 expression. Loss of heterozygosity on chromosome 17 frequently involves the whole chromosome (Shelling et al, 1995), but minimal regions of loss have been detected at 17p13, 17q12.2, 17q21 and 17q25.1–qter (Liu and Ganesan, 2002). Our finding of high rates of LOH at 17q11.2–q12 places this region among the most frequently deleted regions in ovarian cancer (Shelling et al, 1995; Liu and Ganesan, 2002). The fact that this LOH is significantly more common in late stage than early stage tumours, indicates that it is associated with progression rather than initiation. Further analysis of 17q is required to refine the minimal region of deletion at 17q11.2–q12 and to determine whether CCL2 is the target of this loss.
Transfection with human CCL2 has been reported to suppress the in vivo growth and tumorigenicity of CHO cells (Rollins and Sunday, 1991) and melanoma cells (Bottazzi et al, 1992), and the fusion of tumorigenic HeLa cells, which do not express CCL2, with normal fibroblasts, resulted in CCL2 expressing somatic hybrids unable to form tumours in nude mice (Rosl et al, 1994). In contrast, no effect on tumour growth was found for human or murine CCL2 transfected into colon adenocarcinoma cells (Hirose et al, 1995). We transfected the HEY and OVCAR8 ovarian cancer cell lines with CCL2 cloned into pcDNA3.1, but were unable to develop stable clones with comparable levels of expression to the HOSE cells, and so were unable or to interpret the consequences of in vitro or in vivo assays (data not shown).
The consequences of the introduction of CCL2 into biologically early, nontumorigenic melanoma cells were found to depend on the level of CCL2 secretion (Nesbit et al, 2001). Low level secretion was found to stimulate tumour growth through angiogenesis mediated by monocyte activation, whereas high levels of CCL2 attracted large numbers of monocytes/macrophages and rapid tumour destruction (Nesbit et al, 2001). Thus, it appears that the levels of CCL2 may determine the biological effect. The reduced levels of CCL2 found in ovarian cancers may be promoting tumour growth through various growth factors produced by monocytes attracted to the tumour, in addition to evading the destructive response of the host macrophages and T cells. This concept requires more investigation in ovarian cancer and other neoplasias.
Acknowledgments
This work was supported by grants from the National Health and Medical Research Council of Australia (NHMRC #981331 to GC-T and NHMRC #290220 to GAR).
References
- Arnold JM, Mok SC, Purdie D, Chenevix-Trench G (2001a) Decreased expression of the Id3 gene at 1p36.1 in ovarian adenocarcinomas. Br J Cancer 84: 1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold JM, Cummings M, Purdie D, Chenevix-Trench G (2001b) Reduced expression of intercellular adhesion molecule-1 in ovarian adenocarcinomas. Br J Cancer 85: 1351–1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aunoble B, Sanches R, Didier E, Bignon Y (2000) Major oncogenes and tumour suppressor genes involved in epithelial ovarian cancer (review). Int J Oncol 16: 567–576 [DOI] [PubMed] [Google Scholar]
- Bottazzi B, Walter S, Govoni D, Colotta F, Mantovani A (1992) Monocyte chemotactic cytokine gene transfer modulates macrophage infiltration, growth and susceptibility to IL-2 therapy of a murine melanoma. J Immunol 148: 1280–1285 [PubMed] [Google Scholar]
- Buick RN, Pullano R, Trent JM (1985) Comparative proterties of five human ovarian adenocarcinoma cell lines. Cancer Res 45: 3668–3676 [PubMed] [Google Scholar]
- Burke F, Relf M, Negus R, Balkwill F (1996) A cytokine profile of normal and malignant ovary. Cytokine 8: 578–585 [DOI] [PubMed] [Google Scholar]
- Colombo MP, Modesti A, Parmiani G, Forni G (1992) Local cytokine availability elicits tumor rejection and systemic immunity through granulocyte-T-lymphocyte cross-talk. Cancer Res 52: 4853–4857 [PubMed] [Google Scholar]
- Desbaillets I, Tada M, de Tribolet N, Diserens AC, Hamou MF, Van Meir EG (1994) Human astrocytomas and glioblastomas express monocyte chemoattractant protein-1 (MCP-1) in vivo and in vitro. Int J Cancer 58: 240–247 [DOI] [PubMed] [Google Scholar]
- Duan Z, Feller AJ, Penson RT, Chabner BA, Seiden MV (1999) Discovery of differentially expressed genes associated with paclitaxel resistance using cDNA array technology: analysis of interleukin (IL) 6, IL-8 and monocyte chemotactic protein 1 in the paclitaxel-resistant phenotype. Clin Cancer Res 5: 3445–3453 [PubMed] [Google Scholar]
- Fogh J, Trempe G (1975) New human cell lines. In Human tumour cells in vitro Fogh J (ed) pp 155–159. New York: Plenum [Google Scholar]
- Goedegebuure PS, Douville CC, Doherty JM, Linehan DC, Lee K-Y, Ganguly EK, Eberlein TJ (1997) Simultaneous production of T helper-1-like cytokines and cytolytic activity by tumor-specific T cells in ovarian and breast cancer. Cell Immunol 175: 150–156 [DOI] [PubMed] [Google Scholar]
- Graves DT, Barnhill R, Galanopoulos T, Antoniades HN (1992) Expression of monocyte chemotactic protein-1 in human melanoma in vivo. Am J Pathol 140: 9–14 [PMC free article] [PubMed] [Google Scholar]
- Hamilton TC, Young RC, McKoy WM, Grotzinger KR, Green JA, Chu EW, Whang-Peng J, Rogan AM, Green WR, Ozols RF (1983) Characterization of a human ovarian carcinoma cell line (NIH:OVCAR-3) with androgen and estrogen receptors. Cancer Res 43: 5379–5389 [PubMed] [Google Scholar]
- Hirose K, Hakozaki M, Nyunoya Y, Kobayashi Y, Matsushita K, Takenouchi T, Mikata A, Mukaida N, Matsushima K (1995) Chemokine gene transfection into tumour cells reduced tumorigenicity in nude mice in association with neutrophilic infiltration. Br J Cancer 72: 708–714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleine-Lowinski K, Gillitzer R, Kuhne-Heid R, Rosl F (1999) Monocyte-chemo-attractant-protein-1 (MCP-1) gene expression in cervical intra-epithelial neoplasias and cervical carcinomas. Int J Cancer 82: 6–11 [DOI] [PubMed] [Google Scholar]
- Kuratsu J, Yoshizato K, Yoshimura T, Leonard EJ, Takeshima H, Ushio Y (1993) Quantitative study of monocyte chemoattractant protein-1 (MCP-1) in cerebrospinal fluid and cyst fluid from patients with malignant glioma. J Natl Cancer Inst 85: 1836–1839 [DOI] [PubMed] [Google Scholar]
- Langdon SP, Lawrie SS, Hay FG, Hawkes MM, McDonald A, Hayward IP, Schol DJ, Hilgers J, Leonard RCF, Smyth JF (1988) Characterization and properties of nine human ovarian adenocarcinoma cell lines. Cancer Res 48: 6166–6172 [PubMed] [Google Scholar]
- Liu Y, Ganesan TS (2002) Tumour suppressor genes in sporadic epithelial ovarian cancer. Reproduction 123: 341–353 [DOI] [PubMed] [Google Scholar]
- Malik S, Balkwill F (1991) Epithelial ovarian cancer: a cyotkine propelled disease? Br J Cancer 64: 617–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A (1994) Biology of disease. Tumor-associated macrophages in neoplastic progression: a paradigm for the in vivo function of chemokines. Lab Invest 71: 5–16 [PubMed] [Google Scholar]
- Mantovani A, Bottazzi B, Colotta F, Sozzani S, Ruco L (1992) The origin and function of tumor-associated macrophages. Immunol Today 13: 265–270 [DOI] [PubMed] [Google Scholar]
- Mazzucchelli L, Loetscher P, Kappeler A, Uguccioni M, Baggiolini M, Laissue JA, Mueller C (1996) Monocyte chemoattractant protein-1 gene expression in prostate hyperplasia and prostate adenocarcinoma. Am J Pathol 149: 501–509 [PMC free article] [PubMed] [Google Scholar]
- Merogi AI, Marrogi AI, Ramesh R, Robinson WR, Fermin CD, Freeman SM (1997) Tumor-host interaction: analysis of cytokines, growth factors, and tumor-infiltrating lymphocytes in ovarian carcinomas. Hum Pathol 28: 321–331 [DOI] [PubMed] [Google Scholar]
- Miller SA, Dykes DD, Polesky HF (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16: 1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negus RP, Stamp GW, Relf MG, Burke F, Malik ST, Bernasconi S, Allavena P, Sozzani S, Mantovani A, Balkwill FR (1995) The detection and localization of monocyte chemoattractant protein-1 (MCP-1) in human ovarian cancer. J Clin Invest 95: 2391–2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negus RPM, Stamp GWH, Hadley J, Balkwill FR (1997) Quantitative assessment of the leukocyte infiltrate in ovarian cancer and its relationship to the expression of C-C chemokines. Am J Pathol 150: 1723–1734 [PMC free article] [PubMed] [Google Scholar]
- Nesbit M, Schaider H, Miller TH, Herlyn M (2001) Low-level monocyte chemoattractant protein-1 stimulation of monocytes leads to tumour formation in non-tumorigenic melanoma cells. J Immunol 166: 6483–6490 [DOI] [PubMed] [Google Scholar]
- Oppenheim JJ, Zachariae COC, Mukaida N, Matsushima K (1991) Properties of the novel proinflamatory supergene ‘intercrine’ cytokine family. Annu Rev Immunol 9: 617–648 [DOI] [PubMed] [Google Scholar]
- O'Sullivan C, Lewis CE (1994) Tumor-associated leukocytes: friends or foes in breast carcinoma. J Pathol 172: 229–235 [DOI] [PubMed] [Google Scholar]
- Parkin DM, Pisani P, Ferlay J (1999) Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer 80: 827–841 [DOI] [PubMed] [Google Scholar]
- Parmiani G, Anichini A, Fossati GJ (1990) Cellular immune response against autologous human malignant melanoma: are in vitro studies providing a framework for a more effective immunotherapy? J Natl Cancer Inst 82: 361–370 [DOI] [PubMed] [Google Scholar]
- Penson RT, Kronishi K, Duan Z, Feller AJ, Stark P, Cook P, Duskat LR, Fuller AF, Goodman AK, Nikruh N, MacNeill KM, Matulonis UA, Preffers FI, Seiden MV (2000) Cytokines IL-1β, IL-2, IL-6, IL-8, MCP-1, GM-CSF and TNFα in patients with epithelial ovarian cancer and their relationship to treatment with paclitaxel. Int J Gynecol Cancer 10: 33–41 [DOI] [PubMed] [Google Scholar]
- Peoples GE, Davey MP, Goedegebuure PS, Schoof DD, Eberlein TJ (1995) T cell receptor V beta 2 and V beta 6 mediate tumor-specific cytotoxicity by tumor-infiltrating lymphocytes in ovarian cancer. J Immunol 151: 5472–5480 [PubMed] [Google Scholar]
- Ramm GA, Nair VG, Bridle KR, Shepherd RW, Crawford DHG (1998) Contribution of hepatic parenchymal and nonparenchymal cells to hepatic fibrogenesis in biliary atresia. Am J Pathol 153: 527–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rex M, Scotting PJ (1994) Simultaneous detection of RNA and protein in tissue sections by nonradioactive in situ hybridization followed by immunohistochemistry. Biochemica 3: 24–26 [Google Scholar]
- Riethdorf S, Riethdorf L, Richter N, Loning T (1998) Expression of the MCP-1 gene and the HPV 16 E6/E7 oncogenes in squamous cell carcinomas of the cervix uteri and metastasis. Pathobiology 66: 260–267 [DOI] [PubMed] [Google Scholar]
- Rollins BJ (1991) JE/MCP-1: an early-response gene encodes a monocyte-specific cytokine. Cancer Cells 3: 517–524 [PubMed] [Google Scholar]
- Rollins BJ, Sunday ME (1991) Suppression of tumor formation in vivo by expression of the JE gene in malignant cells. Mol Cell Biol 11: 3125–3131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosl F, Lengert M, Albrecht J, Kleine K, Zawatzky R, Schraven B, Zur Hausen H (1994) Differential regulation of the JE gene encoding the monocyte chemoattractant protein (MCP-1) in cervical carcinoma cells and derived hytbrids. J Virol 68: 2142–2150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sambrook J, Russell DW (2001) Molecular Cloning: A Laboratory Manual 3rd edn New York: Cold Spring Harbour Laboratory Press [Google Scholar]
- Shelling AN, Cooke IE, Ganesan TS (1995) The genetic analysis of ovarian cancer. Br J Cancer 72: 521–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica A, Wang JM, Colotta F, Dejana S, Mantovani A, Oppenheim JJ, Larsen CG, Zachariae CO, Matsushima K (1990) Monocyte chemotactic and activating factor gene expression induced in endothelial cells by IL-1 and tumor necrosis factor. J Immunol 144: 3034–3038 [PubMed] [Google Scholar]
- Takeshima H, Kuratsu J, Takeya M, Yoshimura T, Ushio Y (1994) Expression and localization of messenger RNA and protein for monocyte chemoattractant protein-1 in human malignant glioma. J Neurosurg 80: 1056–1062 [DOI] [PubMed] [Google Scholar]
- Taub DD, Proost P, Murphy WJ, Anver M, Longo DJ, van Damme J, Oppenheim JJ (1995) Monocyte chemotactic protein-1 (MCP-1), -2 and -3 are chemotactic for human T lymphocytes. J Clin Invest 95: 1370–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsao S-W, Mok SC, Fey EG, Fletcher JA, Wan TSK, Chew E-C, Muto MG, Knapp RC, Berkowitz RS (1995) Characterization of human ovarian surface epithelial cells immortalized by human papilloma viral oncogenes (HPV-E6E7 ORFs). Exp Cell Res 218: 499–507 [DOI] [PubMed] [Google Scholar]
- Ward BG, Wallace K, Shepherd JH, Balkwill FR (1987) Intraperitoneal xenografts of human epithelial ovarian cancer in nude mice. Cancer Res 47: 2662–2667 [PubMed] [Google Scholar]
- Wilson AP (1984) Characterization of a cell line derived from the ascites of a patient with papillary serous cystadenocarcinoma of the ovary. J Natl Cancer Inst 72: 513–520 [PubMed] [Google Scholar]
- Wilson AP, Ford CHJ, Newman CE, Howell A (1987) Cis-platinum and ovarian carcinoma: in vitro chemosenstitvity of cultures tumour cells from patients receiving high dose cis-platinum as first line treatment. Br J Cancer 56: 763–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf CR, Hayward IP, Lawrie SS, Buckton K, McIntyre MA, Adams DJ, Lewis AD, Scott ARR, Smyth JF (1987) Cellular heterogeneity and drug resistance in two ovarian adenocarcinoma cell lines derived from a single patient. Int J Cancer 39: 695–702 [DOI] [PubMed] [Google Scholar]
- Wong AST, Maines-Bandiear SL, Rosen B, Wheelock MJ, Johnson KR, Leung PCK, Roskelley CD, Auersperg N (1999) Constitutive and conditional cadherin expression in cultured human ovarian surface epithelium: influence of family history on ovarian cancer. Int J Cancer 81: 180–188 [DOI] [PubMed] [Google Scholar]
- Woods LK, Morgan RT, Quinn LA, Moore GE, Semple TU, Stedman KE (1979) Comparison of four new cell lines from patients with adenocarcinoma of the ovary. Cancer Res 39: 4449–4459 [PubMed] [Google Scholar]
- Zacchariae CO, Anderson AO, Thompson HL, Appella E, Mantovani A, Oppenheim JJ, Matsushima K (1990) Properties of a monocyte chemotactic and activating factor (MCAF) purified from a human fibrosarcoma cell line. J Exp Med 171: 2177–2182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty P, Massobrio M, Regnani G, Makrigiannakis A, Gray H, Schlienger K, Liebman MN, Rubin SC, Coukos G (2003) Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. New Engl J Med 348: 203–213 [DOI] [PubMed] [Google Scholar]
- Zhang L, Khayat A, Cheng H, Graves DT (1997) The pattern of monocyte recruitment in tumors is modulated by MCP-1 expression and influences the rate of tumor growth. Lab Invest 76: 579–590 [PubMed] [Google Scholar]