Abstract
Here we show that human papillomavirus (HPV) E6 and E7 oncoproteins induce hWAPL expression. In addition, small interfering RNA (siRNA) of hWAPL suppressed the growth of tumours derived from SiHa cells in nude mice. Thus, hWAPL may be one of the effective targets of uterine cervical cancer therapy.
Keywords: hWAPL, HPV, E6, E7, siRNA
Cervical cancer is unique due to its association with high-risk human papilloma virus (HPV) infection with strains such as HPV-16 and HPV-18 (zur Hausen, 1996). The high-risk-HPV oncoproteins, E6 and E7, are necessary for immortalisation and transformation of cervical keratinocytes (Munger et al, 1989). E6 binds to the wild-type p53 protein and promotes its ubiquitin-dependent degradation (Scheffner et al, 1990, 1993), and E7 binds to the retinoblastoma protein Rb and disrupts the complex between Rb and the E2F transcription factor family, which controls the expression of genes involved in cell-cycle progression (Dyson et al, 1992). Therefore, the development of anticancer therapies that target HPV E6 and E7 and/or downstream targets of HPV E6 and E7 might be a specific and effective treatment for cervical cancer. In fact, RNA interference (RNAi) of E6 and/or E7 inhibits growth of HPV-positive cancer cells (Jiang and Milner, 2002; Butz et al, 2003; Yoshinouchi et al, 2003).
Our previous study demonstrated that the novel human gene hWAPL showed the unscheduled high-level expression in cervical dysplasia and carcinoma (Oikawa et al, 2004). In addition, NIH3T3 cells overexpressing hWAPL developed into tumours upon injection into nude mice, suggesting that hWAPL plays a significant role in cervical carcinogenesis and tumour progression as an oncogene (Oikawa et al, 2004). Furthermore, siRNA of hWAPL inhibited cell growth in cervical cancer-derived cultured cells (Oikawa et al, 2004).
In this report, we reveal that HPV E6 and E7 oncoproteins affect hWAPL expression. We also show that hWAPL exhibited great potential as a novel therapeutic target molecule in the treatment of cervical cancer.
MATERIALS AND METHODS
Cell culture, retroviral vector construction and retroviral infection
SiHa, CaSki and C33A cells were grown in DMEM (Sigma Chemical Co., St Louis, MO, USA) containing 10% fetal bovine serum (FBS) at 37°C in a 5% CO2 environment. Normal human epidermal keratinocytes from adult skin (HDK1) were grown in keratinocyte serum-free medium (K-SFM; Invitrogen, Carlsbad, CA, USA).
The HPV16-E6, E7, and E6E7 genes were amplified by polymerase chain reaction (PCR) using the following primers: 5′-AAAAAGCAGGCTCCACCATGTTTCAGGACCCACAGGAGCGACCC-3′ and 5′-AGAAAGCTGGGTTACAGCTGGGTTTCTCTACGTG-3′ for E6, and 5′-AAAAAGCAGGCTCCACCATGCATGGAGATACACCTACAT-3′ and 5′-AGAAAGCTGGGTTATGGTTTCTGAGAACAGATGGGG-3′ for E7. The amplified DNA fragments were cloned into the retroviral vector, pCLXSN.
The bovine papillomavirus type 1 (BPV1) E2 segment was obtained by nested PCR from a pBPV-MII template using 5′-GGGGACAAGTTTGTACAAAAAAGCAGGCT-3′ and 5′-GGGGACCACTTTGTACAAGAAAGCTGGGT-3′ as outer primers, and 5′-AAAAAGCAGGCTCCACCATGGAGACAGCATGCGAAC-3′ and 5′-AGAAAGCTGGGTCAGAAGTCCAAGCTGGCTGTAAAG-3′ as inner primers. The BPV1 E2 segment was then cloned into a pCMSCV-based (Clontech, Palo Alto, CA, USA) retroviral vector, pCMSVpuro.
The preparation of recombinant retroviruses and the infection procedures have been previously described (Naviaux et al, 1996). HDK1 cells were infected with the prepared retroviruses, LXSN-16E6, LXSN-16E7, LXSN-16E6E7, or the control LXSN. The infected cells were selected in the presence of 50 μg ml−1 of G418. SiHa, CaSki and C33A cells were infected with either the MSCV-puro or MSCV-puroBPV1E2 viruses and selected with 1 μg ml−1 of puromycin.
Immunoblot analysis
We generated a rabbit polyclonal antibody against a synthetic peptide, amino acids 50–66 (CNFKPDIQEIPKKPKVEE) of hWAPL (termed anti-hWAPL-N). Immunoblot analyses were performed as previously described (Kiyono et al, 1997). Antibodies against hWAPL (anti-hWAPL-N), p53 (Oncogene Science, Cambridge, MA, USA, DO-1), and the anti-HPV16 E7 (ZYMED, South San Francisco, CA, USA, 8C9) were used at a dilution of 1/1000.
Animals and treatments
Guidelines for the care and use of animals were approved by the animal research centre in Tokyo Medical University. BALB/cAJc1-nu female mice (4 weeks old) were purchased from Charles River Japan, Inc. (Kanagawa, Japan). The individual mice were injected with ≈4 × 107 SiHa cells suspended in 200 μl of PBS. Upon the development of a tumour from the injected SiHa cells 1 week after injection, we injected either an active siRNA specific for hWAPL or the negative control siRNA at the indicated time points (Figures 2A and 3). The nucleotide sequences of the siRNAs were as previously described (Oikawa et al, 2004). The active siRNA specific for hWAPL corresponds to siRNA(I) in the previous study (Oikawa et al, 2004). The injection materials were generated as follows: In Figure 2, the siRNAs were synthesised by in vitro transcription using a Silencer siRNA Construction Kit (Ambion, Austin, TX, USA). One microlitre of 10 μM siRNA and 2 μl of Oligofectamine Reagent (Invitrogen Japan, Tokyo, Japan) were diluted into 89 μl and 8 μl of Opti-MEM I (Invitrogen Japan), respectively. After a 10-min incubation, the diluted reagents were combined and incubated for an additional 20 min. The siRNA-Oligofectamine mixture was then injected into the mouse at the tumour site. In Figure 3, 1 μl of 10 μM siRNA and 74 μl of 2% atelocollagen (Koken Co. Ltd, Tokyo, Japan) (Takei et al, 2004) were mixed on ice, and then the siRNA-atelocollagen mixture was injected into mouse at the tumour site.
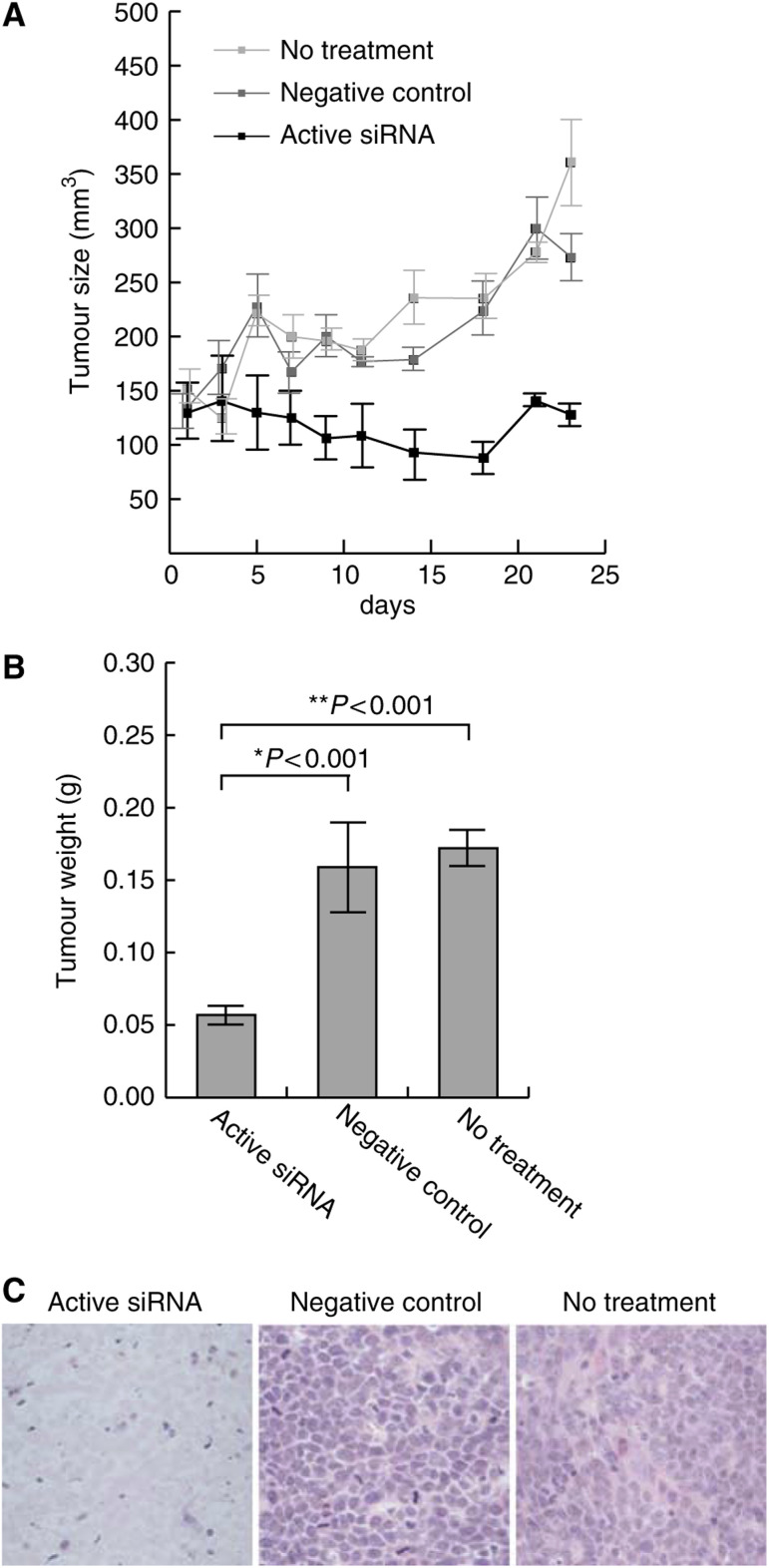
Figure 2.
An active siRNA inhibiting hWAPL expression suppressed the growth of subcutaneous tumours derived from SiHa cells inoculated into nude mice. (A) Tumour growth curves. The tumour volume (mm3) was approximated by multiplication of the major axis, the minor axis, and the height of each tumour. Each data point represents the mean of eight samples. Bars, s.e. (B) Weights of the tumours in nude mice 25 days after the first siRNA injection. Each data point represents the mean of eight samples. Bars, s.e. *P<0.001 vs negative control. **P<0.001 vs no treatment. (C) Representative histology of the subcutaneous tumours in nude mice. The excised tumours were subjected to paraffin sectioning, then stained with haematoxylin and eosin.
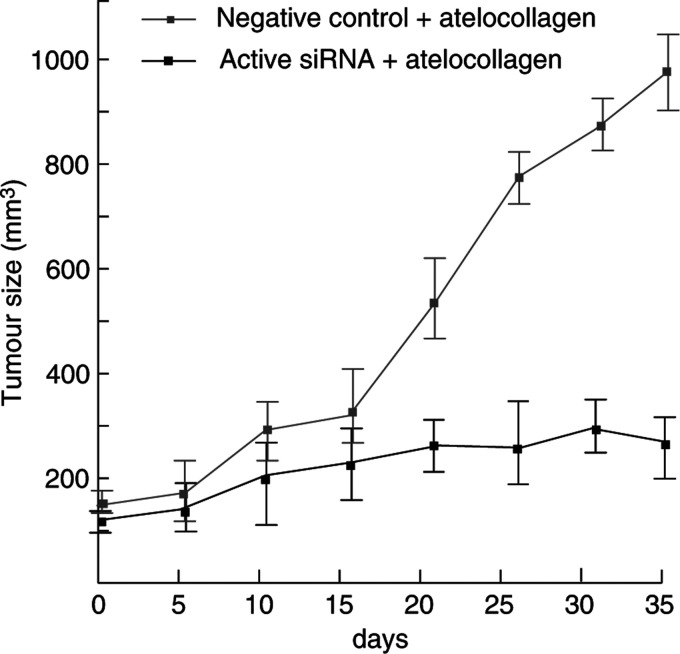
Figure 3.
Atelocollagen increases antitumour effects of hWAPL siRNA. The growth curves of subcutaneous tumours injected with active or negative control siRNA mixed with atelocollagen were shown. The tumour volume (mm3) was approximated by multiplication of the major axis, the minor axis, and the height of each tumour. Each data point represents the mean of four samples. Bars, s.e.
Statistical analysis
The data were analysed using the Student's t-test, and P<0.001 were considered to indicate significant differences.
RESULTS
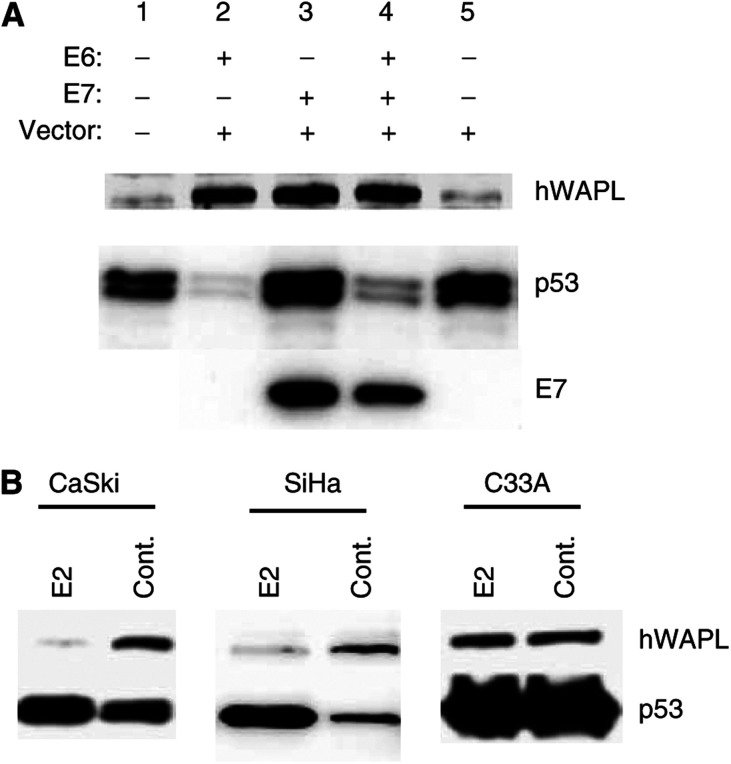
HPV oncoproteins E6 and E7 induce hWAPL
We examined whether HPV-16 E6 and E7 oncogene products influence hWAPL expression. We infected normal human epidermal keratinocytes from adult skin tissue (HDK1) with HPV-16 E6- and E7-expressing retroviruses, and observed that both HPV-16 E6 and E7 induce hWAPL expression (Figure 1A). E6 and E7 expression levels were confirmed by monitoring p53 degradation and E7 antibody staining, respectively (Figure 1A).
Figure 1.
(A) HPV-16 E6 and E7 expression induces increased expression of hWAPL. hWAPL protein was induced by HPV E6 and E7 oncoprotein expression in HDK1 cells (passage 5), as determined by Western blotting. E6 induced p53 degradation (lanes 2, E6 and 4, E6E7). A Western blot showing HPV-16 E7 protein levels is provided in the bottom panel. (B) BPV1 E2 suppressed hWAPL expression. hWAPL protein levels were reduced by exogenous BPV1 E2 expression in the HPV 16 E6- and E7-expressing cell lines, CaSki and SiHa, as determined by Western blot analysis.
To confirm that hWAPL expression is inducible by E6 and E7, we also examined whether repression of E6 and E7 expression causes hWAPL reduction in cervical cancer-derived cell lines. Because the papillomavirus E2 protein represses E6/E7 transcription by binding the HPV early promoter (Hwang et al, 1993, 1996; Dowhanick et al, 1995; Francis et al, 2000), we analyse the effect of E2 on hWAPL expression. We observed a significant reduction of hWAPL protein levels after the infection of HPV-16 E6- and E7-expressing cervical cancer cell lines, such as CaSki and SiHa, with the retrovirus encoding E2 (Figure 1B). The HPV-negative cervical cancer cell line C33A, however, did not exhibit significant changes in hWAPL protein levels after E2 retrovirus infection (Figure 1B). These results demonstrate that hWAPL can be induced by HPV E6 and E7 oncoproteins.
The mechanism of hWAPL induction by E6 and E7 has not yet been elucidated. Although both E6 and E7 contribute transformation of human keratinocytes, functions of these proteins are different. hWAPL induction by the combination of E6 and E7, however, showed similar level to that by either E6 or E7 alone (Figure 1A). Thus, hWAPL transcription may possibly respond to a particular precancerous cell states induced by E6 and/or E7. In fact, HPV-positive normal cervical tissue samples exhibited a low level of hWAPL expression (Oikawa et al, 2004), and C33A, an HPV-negative uterine cervical cancer-derived cell line, showed high hWAPL expression (Figure 1B, and data not shown), suggesting that hWAPL expression is more closely related with cervical carcinogenesis than HPV infection, as previously mentioned (Oikawa et al, 2004). Nevertheless, although HPV infection does not always induce hWAPL expression, E6 and E7 oncoproteins are still likely to be associated with hWAPL expression in cervical cancers.
hWAPL exhibits great potential as a therapeutic target
We previously observed that repression of hWAPL expression by a specific siRNA inhibited cell growth in various cervical cancer-derived cell lines such as SiHa, CaSki (Oikawa et al, 2004) and C33A (data not shown) in vitro. Thus, we next investigated the possibility that hWAPL might be a novel cancer therapeutic target molecule. We generated tumours in nude mice by subcutaneous injection of SiHa cells. At 1 week after injection of the tumour cells, we measured tumour sizes using caliper squares and then injected siRNA into the tumours on alternate days for 3 weeks (Figure 2A). The growth of tumours injected with the active siRNA specific for hWAPL was repressed in comparison with untreated tumours or tumours injected with negative control siRNA (Figure 2A, B). We observed necrosis in the tumours injected with the active siRNA (Figure 2C). In contrast, untreated or control tumours were viable (Figure 2C). We also observed similar effects of the siRNA on tumours arising from another cervical cancer-derived cell line, CaSki (data not shown). These results demonstrate that hWAPL may have potential as a therapeutic target, particularly in cervical cancer.
However, siRNA itself is rapidly degraded in tumours (Takei et al, 2004) and the durability of the effects may be insufficient for clinical application. In fact, although we injected the hWAPL siRNA into tumours on alternate days, the repression of the tumour growth was not preserved in a few cases (Figure 2A and data not shown). Recently, a new gene transfer method using atelocollagen has been established (Ochiya et al, 1999). Atelocollagen is expected to increase cellular uptake, nuclease resistance, and prolonged release of siRNAs adiministered into tumours because of its unique property that it is a liquid at 4°C and a gel at 37°C (Ochiya et al, 1999; Takei et al, 2004). Furthermore, Takei et al revealed that atelocollagen contributes the increased stability of siRNAs injected in tumours. Thus, we generated tumours in nude mice by subcutaneous injection of SiHa cells again, and then monitored the growth of the tumours injected with active siRNA or negative control siRNA mixed with atelocollagen (Figure 3). The injection was performed at only 4 time points of 0, 5th, 10th and 20th day for 35 days. As shown in Figure 3, active siRNA with atelocollagen dramatically suppressed tumour growth.
DISCUSSION
Recent findings show that the targeted inactivation of oncogenes could be a specific and effective treatment for cancer (Felsher, 2003). For uterine cervical cancer, HPV E6 and/or E7 were shown to be a strong candidate as a target for gene-specific therapy (Jiang and Milner, 2002; Butz et al, 2003; Yoshinouchi et al, 2003). However, many subtypes of high-risk HPV have been detected in cervical cancers although HPV types 16 and 18 are great majority of cervical carcinomas (Nakagawa et al, 2000). Thus, for clinical application of E6 and E7 siRNAs, various nucleotide sequences may be required for the respective types of HPV. In this study, we have demonstrated that an siRNA of hWAPL induces tumour regression in vivo. This anticancer effects by the hWAPL siRNA stands comparison with the effects of the E6 siRNA (Jiang and Milner, 2002; Butz et al, 2003; Yoshinouchi et al, 2003). Therefore, we expect that hWAPL is one of strong candidates as a target for uterine cervical cancer therapy.
Acknowledgments
This work was supported in part by Grant-in-Aid for scientific research on Priority Area(C) and Grant-in-Aid for Encouragement of Young Scientists from the Ministry of Education, Scientific, Sports and Culture, and Core Research for Evolutional Science and Technology (CREST) from Japan Science and Technology Corporation.
References
- Butz K, Ristriani T, Hengstermann A, Denk C, Scheffner M, Hoppe-Seyler F (2003) siRNA targeting of the viral E6 oncogene efficiently kills human papillomavirus-positive cancer cells. Oncogene 22: 5938–5945 [DOI] [PubMed] [Google Scholar]
- Dowhanick JJ, McBride AA, Howley PM (1995) Suppression of cellular proliferation by the papillomavirus E2 protein. J Virol 69: 7791–7799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyson N, Guida P, Munger K, Harlow E (1992) Homologous sequences in adenovirus E1A and human papillomavirus E7 proteins mediate interaction with the same set of cellular proteins. J Virol 66: 6893–6902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felsher DW (2003) Cancer revoked: oncogenes as therapeutic targets. Nat Rev Cancer 3: 375–380 [DOI] [PubMed] [Google Scholar]
- Francis DA, Schmid SI, Howley PM (2000) Repression of the integrated papillomavirus E6/E7 promoter is required for growth suppression of cervical cancer cells. J Virol 74: 2679–2686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang ES, Naeger LK, DiMaio D (1996) Activation of the endogenous p53 growth inhibitory pathway in HeLa cervical carcinoma cells by expression of the bovine papillomavirus E2 gene. Oncogene 12: 795–803 [PubMed] [Google Scholar]
- Hwang ES, Riese II DJ, Settleman J, Nilson LA, Honig J, Flynn S, DiMaio D (1993) Inhibition of cervical carcinoma cell line proliferation by the introduction of a bovine papillomavirus regulatory gene. J Virol 67: 3720–3729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang M, Milner J (2002) Selective silencing of viral gene expression in HPV-positive human cervical carcinoma cells treated with siRNA, a primer of RNA interference. Oncogene 21: 6041–6048 [DOI] [PubMed] [Google Scholar]
- Kiyono T, Hiraiwa A, Fujita M, Hayashi Y, Akiyama T, Ishibashi M (1997) Binding of high-risk human papillomavirus E6 oncoproteins to the human homologue of the Drosophila discs large tumor suppressor protein. Proc Natl Acad Sci USA 94: 11612–11616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munger K, Phelps WC, Bubb V, Howley PM, Schlegel R (1989) The E6 and E7 genes of the human papillomavirus type 16 together are necessary and sufficient for transformation of primary human keratinocytes. J Virol 63: 4417–4421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa S, Yoshikawa H, Yasugi T, Kimura M, Kawana K, Matsumoto K, Yamada M, Onda T, Taketani Y (2000) Ubiquitous presence of E6 and E7 transcripts in human papillomavirus-positive cervical carcinomas regardless of its type. J Med Virol 62: 251–258 [DOI] [PubMed] [Google Scholar]
- Naviaux RK, Costanzi E, Haas M, Verma IM (1996) The pCL vector system: rapid production of helper-free, high-titer, recombinant retroviruses. J Virol 70: 5701–5705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochiya T, Takahama Y, Nagahara S, Sumita Y, Hisada A, Itoh H, Nagai Y, Terada M (1999) New delivery system for plasmid DNA in vivo using atelocollagen as a carrier material: the Minipellet. Nat Med 5: 707–710 [DOI] [PubMed] [Google Scholar]
- Oikawa K, Ohbayashi T, Kiyono T, Nishi H, Isaka K, Umezawa A, Kuroda M, Mukai K (2004) Expression of a novel human gene, human wings apart-like (hWAPL), is associated with cervical carcinogenesis and tumor progression. Cancer Res 64: 3545–3549 [DOI] [PubMed] [Google Scholar]
- Scheffner M, Huibregtse JM, Vierstra RD, Howley PM (1993) The HPV-16 E6 and E6-AP complex functions as a ubiquitin-protein ligase in the ubiquitination of p53. Cell 75: 495–505 [DOI] [PubMed] [Google Scholar]
- Scheffner M, Werness BA, Huibregtse JM, Levine AJ, Howley PM (1990) The E6 oncoprotein encoded by human papillomavirus types 16 and 18 promotes the degradation of p53. Cell 63: 1129–1136 [DOI] [PubMed] [Google Scholar]
- Takei Y, Kadomatsu K, Yuzawa Y, Matsuo S, Muramatsu T (2004) A small interfering RNA targeting vascular endothelial growth factor as cancer therapeutics. Cancer Res 64: 3365–3370 [DOI] [PubMed] [Google Scholar]
- Yoshinouchi M, Yamada T, Kizaki M, Fen J, Koseki T, Ikeda Y, Nishihara T, Yamato K (2003) In vitro and in vivo growth suppression of human papillomavirus 16-positive cervical cancer cells by E6 siRNA. Mol Ther 8: 762–768 [DOI] [PubMed] [Google Scholar]
- zur Hausen H (1996) Papillomavirus infections – a major cause of human cancers. Biochim Biophys Acta 1288: F55–F78 [DOI] [PubMed] [Google Scholar]