Abstract
Research studies investigating the impact of childhood cumulative adversity on adult mental health have proliferated in recent years. In general, little attention has been paid to the operationalization of cumulative adversity, with most studies operationalizing this as the simple sum of the number of occurrences of distinct events experienced. In addition, the possibility that the mathematical relationship of cumulative childhood adversity to some mental health dimensions may be more complex than a basic linear association has not often been considered. This study explores these issues with 2 waves of data drawn from an economically and racially diverse sample transitioning to adulthood in Boston, USA. A diverse set of childhood adversities were reported in high school and 3 mental health outcomes--depressed mood, drug use, and antisocial behavior--were reported 2 years later during the transition to adulthood
Our results suggest that both operationalization and statistical modeling are important and interrelated and, as such, they have the potential to influence substantive interpretation of the effect of cumulative childhood adversity on adult mental health. In our data, total cumulative childhood adversity was related to depressive symptoms, drug use, and antisocial behavior in a positive curvilinear manner with incremental impact increasing as adversities accumulate, but further analysis revealed that this curvilinear effect was an artifact of the confounding of high cumulative adversity scores with the experience of more severe events. Thus, respondents with higher cumulative adversity had disproportionately poorer mental health because of the severity of the adversities they were exposed to, not the cumulative number of different types of adversities experienced. These results indicate that public health efforts targeting prevention of childhood adversities would best be aimed at the most severe adversities in order to have greatest benefit to mental health in young adulthood.
Keywords: USA, cumulative adversity, transition to adulthood, depression, drug use, antisocial behavior, adolescents, mental health
Recent research has documented the strong association between cumulative childhood adversity (CCA) and a variety of mental health outcomes including: adult major depression and depressive symptoms (Chapman, Whitfield, Felitti, Dube, Edwards, & Anda, 2004; Hammen, Henry, & Daley, 2000; Turner & Butler, 2003; Turner & Lloyd, 1995), adolescent depressive symptoms and anger/aggression (Turner, Finkelhor, & Ormrod, 2006), adolescent and adult suicide attempts (Dube, Anda, Felitti, Chapman, Williamson, & Giles, 2001), and alcohol and substance use (Dube, Anda, Felitti, Edwards, & Croft, 2002; Turner & Lloyd, 1995; Turner & Lloyd, 2003). This research has consistently demonstrated that the accumulation of childhood adversities is associated with poorer mental health in adolescence and adulthood
Many of these studies are informed by life course perspectives on the influence of stressors in childhood on the course of mental health as people age (Elder, 1998). Developmentally oriented research has largely focused on the construct of family socioeconomic disadvantage and has routinely employed the strategy of summing a number of risk factors in examining the effects of disadvantage on later mental health, academic success and behavioral adjustment (Caprara & Rutter, 1995; Sameroff, Seifer, Baldwin, & Baldwin, 1993). Conceptual and methodological advances in the study of childhood stress and trauma have resulted in attention to a broader range of threatening experiences including witnessing violence, being injured or very ill, involvement in war or disaster, among other major events that vary from study to study.
Mental health researchers have been increasingly interested in risk processes originating in childhood that jeopardize a successful transition to adulthood, which they define as skillfully navigating the pervasive normative changes involved in assuming adult roles and forging relationships outside the family of origin (Schulenberg, Sameroff, & Cicchetti, 2004). Rates of major depression and alcohol dependence are high among young people between the ages of 18 and 24 (Kessler, McGonagle, Zhao, Nelson, Hughes, Eshleman et al., 1994) and evidence implicates childhood adversities in the more severe profiles of disorder (Moffitt & Caspi, 2001). Thus, major research questions concern the role of childhood events in shaping differences among groups in their mental health and social functioning during this time of change. Practical problems abound in attempting to do so; a key one is representing the multiplicity of childhood risk variables. In this paper we focus on the young adult period and consider methodological issues in achieving a parsimonious measure of cumulative childhood adversity.
Problems of measurement and modeling impacts
Much of the research on childhood adversity and its mental health impact draws on earlier conceptualizations and approaches to measuring cumulative life events, as reflected in the extensive research that has utilized lengthy checklist assessments of recent stressful experiences. From the inception of this tradition, obvious differences in the stressfulness of different events led to consideration of weighting methods to incorporate event severity into aggregate measures of cumulative stress. (Ross & Mirowsky, 1979), for example, demonstrated that a sum score based on “effect proportional” weighting (weighting based on empirically determined effect sizes) greatly improved prediction of psychopathology compared to a simple sum, but their approach was criticized as atheoretical and sample-dependent with effects often based on very low event frequencies (Dohrenwend, 1980; Kessler, 1980). Ross and Mirowsky subsequently moderated their enthusiasm for effect proportional weighting (Mirowsky & Ross, 1980) and a consensus never developed that a specific weighting method was an unambiguous improvement over the simple sum of events. However, Turner and Wheaton have argued that variations in regression-based weighting were never sufficiently explored in the life events literature and contend that using regression weights to “roughly categorize” the general importance of individual events would reduce the bias and error variance in the estimates of the impact of cumulative adversity and minimize the impact of “suppressor events” (e.g., events that have no impact on outcomes) in such estimates (Turner & Wheaton, 1997).
Furthermore, there is some evidence that a simple sum score may mask important information about the impact of different types of events. For example, a handful of studies have aggregated conceptually similar events into separate cumulative adversity scores allowing the association with mental health outcomes to vary in statistical models (e.g., (Turner, Finkelhor, & Ormrod, 2006; Turner & Lloyd, 2003). Categorization based on adversity type did appear to result in varying strength of association between each index and mental health outcomes.
In addition to operationalization, an issue that has been relatively unexplored in the cumulative adversity literature involves model specification: using a simple sum alone as a predictor assumes linearity in the effects of cumulative adversity on mental health. This is an important issue in the life course perspective which maintains that the importance of event exposure in shaping the subsequent life course is not determined in isolation. Despite evidence for non-additivity in the effects of multiple adversities (e.g., (Anderson, Tiro, Price, Bender, & Kaslow, 2002; Kessler, Davis, & Kendler, 1997), researchers modeling the impact of cumulative adversity rarely test for non-linearity in the effects of CCA. More fine-tuned specification of this statistical relationship may provide important clues to the developmental mechanisms undergirding these effects. For example, a positive curvilinear relationship may imply a sensitization process in which the effects of adversity compound as development proceeds throughout childhood and into young adulthood. Some evidence for a curvilinear association of this type has been reported by (Hammen, Henry, & Daley, 2000)), who found that CCA increased vulnerability to depression at low levels of stress in adulthood. In contrast, a negative curvilinear relationship might imply a psychological “steeling effect,” in which exposure to prior adversities inures individuals to the impact of subsequent stressors (see (Pudrovska, Schieman, Pearlin, & Nguyen, 2005). In either case, it remains important to determine the form of relationship and whether it varies for specific mental health dimensions.
Our study, as well as most studies discussed to this point, uses a variable-centered checklist approach to life events measurement. Although this approach enables retrospective assessment of childhood adversities, it has two main weaknesses: (a) it does not provide information regarding the context in which the adversity occurred, and (b) it is more subject to recall bias than interview methods. The seminal work of Brown and associates (Brown, 1981; Brown & Harris, 1989) demonstrated the importance of adversity context obtained through interview probes towards determining which events are experienced as stressful. However, it would be problematic to conduct a contextual evaluation of severe stress experienced during childhood (either during childhood or through retrospective reports) in a community sample due to the quantity of detail surrounding the childhood events that must be obtained. Regarding the potential for recall bias, our study design may mitigate some of the weaknesses of adversity checklists. Our young adult cohort was asked during their senior year in high school to report on major events that occurred while they were growing up. At this age, lifetime experiences are sufficiently proximal and the recall period is relatively short and unambiguous. In addition, young adults are mature enough to understand and report on such events (see (Perkonigg, Kessler, Storz, & Wittchen, 2000). We will return to these issues and consider other study limitations at the close of the paper.
The purpose of this study is to explore the nature of the relationship between CCA and depressed mood, delinquency, and drug use in an economically and racially diverse sample of young adults. Specifically, we examine how our understanding of the impact of childhood adversity on later mental health is affected by the operationalization and modeling of risk exposure. Because research indicates that the effects of many childhood adversities are not disorder-specific and that effects vary by gender, we examine three significant outcomes for this age group which have a differential prevalence for young men and young women and potentially a differential exposure profile.
Method
Sample and Procedures
The data for these analyses came from the first two waves of a prospective study of childhood experiences, adolescent development, and mental health among high school students designed to investigate childhood and adolescent circumstances and events that affect the transition to adulthood. A systematic probability sample of 1,578 high school seniors from 9 public schools serving communities in the Boston Metropolitan area was selected using official rosters obtained from each school. Students were sampled proportionate to the size of the high school they were attending. A total of 1143 of these students were interviewed in the winter and spring of 1998, representing a 72% response rate. Interviews were also conducted with former students of these schools who would have been in the senior cohort but who dropped out. We learned from efforts to contact these former students that only about 2/3 of the individuals originally on our list actually met the dropout criteria described above; this yielded an estimated target sample of 260. Interviews were completed with 182 students, resulting in an estimated response rate of 70%. Thus, the total Wave 1 sample, including graduates and dropouts, is 1325.
At Wave 1, personal interviews, averaging 70 minutes in length, were conducted by trained professional interviewers from the University of Massachusetts Center for Survey Research. A total of 66 interviews were done over the phone for individuals who were not available for a personal interview. Passive parental consent was obtained from parents following a home mailing of study information including a letter from the school indicating their support. Students gave their consent for participation at the time of the interview and were given a gift of 2 movie tickets for their time.
The second wave of interviews was conducted in 2000 and involved 1093 members (83%) of the Wave 1 sample, which includes both the graduates and dropouts. An effort was made to conduct the Wave 2 interviews on the same schedule as the Wave 1 interviews to maintain a 2 year follow-up interval, These interviews were conducted over the telephone with all individuals, with verbal consent given at that time. Participants were given a check for $50 in appreciation for their time. Attrition from the sample was largely a result of an inability to trace respondents due to relocation; only 3% of graduates and 4% of dropouts who were successfully re-contacted refused to participate in the follow-up. We examined variables associated with study retention by estimating a logistic regression model that included dummy variables for race/ethnicity (with whites the omitted category), gender, dropout status, parents' highest education, family standard of living, depressed mood, and family support. Significant predictors of study attrition (all p <.001) included: being Black or Hispanic, dropout status, and having less educated parents (p<.001). Specifically, there was a 12% attrition rate among Whites, in contrast with a 31% rate among Hispanics, and from 18 to 22% among the other race/ethnic groups. The attrition rate for the dropout subsample was estimated on the basis of a projected eligibility rate of 2/3, based on the numbers of individuals who were designated as dropouts in our screenings. Therefore we report an estimated attrition rate of 30% that includes 14% refusals, and 16% non-interviews due to an inability to make contact after an average of 23 tries.
A demographic profile of the sample is presented in Table 1. As a whole the sample is quite diverse and contains large numbers of youths from disadvantaged backgrounds. Although not shown in Table 1, significant differences in SES are apparent among the three racial/ethnic categories examined in this study (identifying reference removed).
Table 1.
Demographic information at Wave 1
| n | % | n | % | ||
|---|---|---|---|---|---|
| Gender | Parents’ Education | ||||
| Male | 643 | 48% | Less than High School | 178 | 14% |
| Female | 682 | 52% | High School Graduatea | 483 | 38% |
| Age | Some College | 218 | 17% | ||
| 16–17 | 396 | 35% | College Degree | 401 | 31% |
| 18 | 559 | 49% | Family Structure | ||
| 19 | 149 | 13% | Intact Two Parent | 666 | 50% |
| 20 and above | 39 | 2% | Step-Parent | 139 | 11% |
| ESL | Single Parent | 390 | 29% | ||
| ESL | 313 | 24% | Other | 130 | 10% |
| No ESL | 101 | 76% | Race/Ethnicity | ||
| Family Income | White | 648 | 49% | ||
| Under $20,000 | 124 | 15% | Black | 279 | 21% |
| $20,000 - $30,000 | 159 | 19% | Hispanic | 145 | 11% |
| $30,000 - $45,000 | 122 | 14% | Asian | 93 | 7% |
| $45,000 - $60,000 | 169 | 20% | Multi | 71 | 5% |
| $60,000 - $80,000 | 157 | 19% | Other | 89 | 7% |
| Above $80,000 | 113 | 13% |
| Table 1b. Means, Standard Deviations, and bivariate correlations for Wave 2 mental health outcome variables | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | n | M | SD | 1 | 2 | 3 | 4 | 5 |
| 1. Depressive symptoms | 1091 | 3.6 | 1.7 | 1 | .23 | .15 | .25 | .23 |
| 2. Antisocial behavior | 1091 | 6.1 | 0.1 | --- | 1 | .42 | .21 | .17 |
| 3. Drug Use | 1018 | 4.1 | 1.2 | ---- | ---- | 1 | .19 | .16 |
| 4. CCAa | 1307 | 1.6 | 1.6 | ---- | ---- | ---- | 1 | .96 |
| 5. CCAb | 1307 | 1.4 | 1.4 | ---- | ---- | ---- | ---- | 1 |
or Voc/Other non-college income
Measures
Three dependent mental health variables were used in this analysis: depressed mood, frequency of drug use, and frequency of antisocial behavior. Depressed mood was measured with a modified 12-item version of the 20- item Center for Epidemiological Studies’ Depression (CESD) scale (Radloff, 1977). This smaller set of items was chosen on the basis of prior work (Ross & Mirowsky, 1984) and represents the 4 dimension factor structure that is seen to represent the major components of depressive symptomatology. The validity and reliability of the CES-D measure has been well established in a number of studies seeking to ascertain its psychometric properties and relationship to diagnostic assessments (Gotlib, Lewinsohn, & Seeley, 1995). The short version has excellent reliability and validity, with an internal consistency of .81 at Wave 1 and .82 at Wave 2, and had a correlation of .95 with the full version in similar data on young adults (identifying reference deleted). Antisocial behavior was assessed by asking respondents to report the number of times in the past 12 months that they had participated in 14 types of aggressive and/or illegal behavior. Prior to calculating a summary measure, frequencies of each item were truncated to 10, in order to diminish the effect of outliers. Drug use was assessed with a self-administered form, which increases validity in reporting sensitive information. We assessed frequency of (a) illegal drugs used or (b) legal drugs used without a doctor’s prescription, in larger amounts than prescribed, or for a longer period of time than prescribed. Respondents were asked how many times in the past 12 months they had used each drug, from “never” to “more than 10 times” on a five-point scale, and a summary variable was created indicating the mean frequency of use. People having missing data for the summary measures were excluded from analyses; this resulted in an effective sample size ranging between 1004 (drug use) and 1075 (depressive symptoms and antisocial behavior). Being a dropout and being male predicted missing data on the drug use summary measure. Means, standard deviations, and correlations for these three outcomes are presented in Table 1b.
Adverse childhood events
Participants answered a series of questions regarding adverse events that ever happened in his/her life and the age at first occurrence. The content and structure of these items are identical to items used in major studies (Turner, Wheaton, & Lloyd, 1995) including the National Comorbidity Survey (e.g., (Kessler, Davis, & Kendler, 1997). These included (a) Did your parents ever have a marital separation of one month or more without ever getting divorced? (b) Did your parents ever get divorced from one another? (c) Did either of your parents die? (d) Did you have a major illness or accident that required you to spend a week or more in the hospital? (e) Did you miss a year of school or have to do it over? (f) Were you ever sent away from home because you did something wrong or your parents felt they couldn’t handle you? (g) Did your father or mother not have a job for a long time when they wanted to work? (h) Did either of your parents drink or use drugs so often or so regularly that it caused problems for the family? (i) Were you ever involved in a life-threatening accident? (j) Were you ever a victim of a fire, flood, or natural disaster? (k) Have you ever witnessed someone being badly injured or killed? (l) Were you ever seriously physically attacked or assaulted? (m) Were you ever physically abused as a child? (n) Were you ever seriously neglected as a child? For each of the above questions, dummy variables were created, coded as “1” if the participant answered “yes” and age at first occurrence was 17 or younger and “0” if the participant answered “no.”
In addition, to assess sexual abuse/assault events, participants were asked if they had ever been: (o) raped (someone had sexual intercourse with you when you did not want to by threatening you or using some degree of force) (p) sexually molested (someone touched or felt your genitals when you did not want them to) and/or (q) sexually abused as a child. To prevent duplication in the reporting of sexual victimization, respondents were instructed to exclude previously reported events in answering the latter two questions (p and q). The effects of these events on the three mental health outcomes were assessed for each event individually in preliminary analyses. Because of the overlap among these items due to the way these questions were structured, and due also to the similarity in their effects on each outcome, a participant who answered “yes” to any of these outcomes, with age of first occurrence 17 or younger, was coded “1” on a single dummy variable. Participants were coded “0” on the sexual abuse/assault variable if they answered no to all three questions.
To estimate the cumulative effect of childhood trauma on mental health in emerging adulthood, two cumulative adversity variables were created. The first variable (CCAa included the sum of all the variables listed above and was used to predict depressive symptoms and drug use. The second variable (CCAb) was used to predict antisocial behavior; it was identical to the first but only events that occurred before the age of 12 were used for the following adversity items: “were you ever sent away from home because you did something wrong or your parents felt they couldn’t handle you,” “have you ever witnessed someone being badly injured or killed,” and “were you ever seriously physically attacked or assaulted.” These variables were modified because the events are confounded with involvement in activities used to define antisocial behavior. For all these events, we obtained the date(s) of first occurrence. Means and standard deviations for these cumulative adversity variables, as well as correlations with outcomes, are presented in Table 1b.
Overview of Analysis
Although there are important study limitations to which we will return at the end of the paper, the goal of the analyses was to use the strengths of our data, in terms of sample and measures, to address important and neglected issues in specifying the relationship between CCA and adult mental health. Specifically, we focus on the question of whether and how the number and severity of events are implicated in the predictive impact of event accumulation.
Analyses were performed using SPSS 15.0. In order to promote comparison across mental health outcomes, and to allow for a straightforward interpretation of the coefficients in standard deviation units, each outcome was standardized to have a mean of 0 and a standard deviation of 1. First, a baseline regression model predicting standardized mental health outcomes with demographic variables was estimated. Second, two models—linear and quadratic—were estimated using the total measure of CCA (i.e., a count of all types of adversities experienced by each respondent). Then, to assess the adequacy of the total CCA measure, adversities were categorized into three levels separately for each gender, based on their gender-specific impact on the mental health outcomes. This allows us to investigate whether the additive impact is best explained in terms of total numbers of adversities experienced, or is dependent on the severity of the event (as inferred from the impact value). Two models—linear and quadratic—were again estimated using these more fine-tuned CCA variables. Finally, the relationship between total CCA score and adversity severity was explored.
All analyses involved estimation of the effects of the adverse events reported at Wave 1 on the three mental health outcomes assessed at Wave 2. Wave 2 mental health outcomes were used to relate CCA to emotional and behavioral functioning during the transition to adulthood, and to mitigate recall bias related to the selective memory of persons in depressed affective states for lifetime stressful events (Schraedley, Turner, & Gotlib, 2002). Wave 1 outcome measures were not included as predictors in these models because we are interested in the relationship of CCA to absolute functioning at Wave 2, not to change in functioning from Wave 1 to Wave 2 (see (Allison, 1990; Kessler & Greenberg, 1981)).
Results
Total CCA
Partially standardized regression coefficients are presented in Table 2 for six models with adversities measured at Wave 1 predicting all three outcomes 2 years later. Model 1 includes controls (gender, race/ethnicity, parent’s education, and dropout status), and total cumulative adversity. Total CCA significantly predicted depressive symptoms, antisocial behavior, and drug use. In Model 2, the interaction of cumulative adversity with gender was added to the variables in Model 1. The impact of cumulative adversity on antisocial behavior and drug use was significantly greater for males than for females; no gender difference was observed for depressive symptoms. Model 2 was then reparameterized to yield separate CCA coefficients by gender to yield Model 3; in this specification CCA coefficients were positive and significantly related to all mental health outcomes for males and to depressive symptoms and drug use for females.
Table 2.
Effects of cumulative childhood adversity (CCA) on standardized mental health outcomes
| Model | Depressive Symptoms | Antisocial Behavior | Drug Use | ||||||
|---|---|---|---|---|---|---|---|---|---|
| b. | s.e. | P | b. | s.e. | P | b. | s.e. | P | |
| Model 1 | |||||||||
| CCA | 0.141* | 0.19 | 0.000 | 0.116* | 0.022 | 0.000 | 0.114* | 0.020 | 0.000 |
| Model 2 | |||||||||
| CCA | 0.131* | 0.023 | 0.000 | 0.204* | 0.024 | 0.000 | 0.151* | 0.025 | 0.000 |
| CCA* gender | 0.021 | 0.027 | 0.436 | −0.154* | 0.027 | 0.000 | −0.067* | 0.028 | 0.015 |
| Model 3 | |||||||||
| CCA for girls | 0.152* | 0.023 | 0.000 | 0.033 | 0.027 | 0.222 | 0.084* | 0.023 | 0.000 |
| CCA for boys | 0.131* | 0.023 | 0.000 | 0.201* | 0.027 | 0.000 | 0.151* | 0.025 | 0.000 |
| Model 4 | |||||||||
| CCA for girls | 0.056 | 0.047 | 0.228 | −0.098# | 0.052 | 0.061 | 0.005 | 0.047 | 0.908 |
| CCA for boys | 0.028 | 0.050 | 0.570 | 0.054 | 0.057 | 0.350 | 0.067 | 0.051 | 0.189 |
| CCA squared | 0.019* | 0.008 | 0.019 | 0.031* | 0.011 | 0.004 | 0.016# | 0.008 | 0.058 |
| Model 5 | |||||||||
| Low impact CCA for girls | −0.076 | 0.053 | 0.152 | −0.043 | 0.043 | 0.311 | −0.050 | 0.044 | 0.262 |
| Medium impact CCA for girls | 0.174* | 0.065 | 0.007 | 0.231* | 0.073 | 0.002 | 0.154* | 0.049 | 0.002 |
| High impact CCA for girls | 0.282* | 0.048 | 0.000 | 0.376* | 0.144 | 0.009 | 0.480* | 0.143 | 0.001 |
| Low impact CCA for boys | 0.034 | 0.071 | 0.636 | −0.056 | 0.049 | 0.259 | −0.015 | 0.057 | 0.794 |
| Medium impact CCA for boys | 0.138* | 0.042 | 0.001 | 0.082 | 0.084 | 0.332 | 0.109* | 0.053 | 0.039 |
| High impact CCA for boys | 0.256* | 0.081 | 0.002 | 0.519* | 0.069 | 0.000 | 0.487* | 0.092 | 0.000 |
| Model 6 | |||||||||
| Low impact CCA for girls | −0.110# | 0.063 | 0.082 | −0.090 | 0.060 | 0.133 | −0.031 | 0.056 | 0.579 |
| Medium impact CCA for girls | 0.139# | 0.074 | 0.060 | 0.172# | 0.091 | 0.057 | 0.179* | 0.068 | 0.009 |
| High impact CCA for girls | 0.231* | 0.070 | 0.001 | 0.327* | 0.150 | 0.030 | 0.520* | 0.161 | 0.001 |
| Low impact CCA for boys | −0.004 | 0.081 | 0.963 | −0.107 | 0.067 | 0.113 | 0.005 | 0.068 | 0.944 |
| Medium impact CCA for boys | 0.096 | 0.060 | 0.109 | 0.039 | 0.093 | 0.676 | 0.135# | 0.072 | 0.059 |
| High impact CCA for boys | 0.184# | 0.108 | 0.090 | 0.431* | 0.105 | 0.000 | 0.529* | 0.120 | 0.000 |
| CCA squared | 0.008 | 0.009 | 0.323 | 0.012 | 0.011 | 0.267 | −0.005 | 0.009 | 0.588 |
p < .05
All models control for gender, parent’s education, race and dropout status.
To test for an accelerating effect of cumulative adversity, we added the square of the cumulative adversity variable to Model 3 to yield Model 4. The quadratic effect of cumulative adversity significantly predicted depressive symptoms and delinquency, and it was marginally significant at the .10 alpha level in predicting drug use. An interaction of squared CCA with gender added to this model was not significant for any outcome, indicating that the quadratic effect of CCA was equivalent for both genders. On the face of it, this analysis indicates that adverse childhood experiences become increasingly damaging to young adult mental health as they accumulate over a child’s lifetime, which is consistent with the sensitization model. However, this analysis assumes that all adverse childhood events have the same impact on mental health, i.e., this approach does not take into account the possibility that individual events have differential impact on mental health outcomes.
Considering adversity impact in CCA operationalization
To determine whether the significance of the quadratic effect resulted from sensitization to adversity or from an increasing likelihood of experiencing more serious events as the number of adversities experienced increased, we needed to take into account the differing individual impacts of the adversities on mental health, separately for females and males. One approach, which we rejected, involved controlling for all other adversities in an effort to isolate the “pure” effect of each adversity. However, because of the likelihood that adversities do not occur randomly, the varying nature of events in the same category, the existence of non-assessed adversities, and possible ceiling effects on outcomes, we did not believe that it would be possible to estimate the “pure” impact of a specific type of event. We thus endeavored to estimate the relative impact of each adverse experience, by regressing each mental health outcome on each adversity separately for females and males controlling for gender, race, and parent’s education. We believe that, for each adversity, this approach captured the average mental health effect of adversities (over differing contexts) relative to other types of adversities. The adversity coefficients, which were categorized into low (≤ - .2), medium (.2 – .4), and high (≥.4) impact groups, are presented in Table 3. Three cumulative adversity variables were then created for each outcome by counting the number of adversities experienced within each impact level, separately by gender (a total of 6 CCA variables—3 for boys and 3 for girls). Regression models with demographic controls and the 6 CCA variables predicting each mental health outcome were estimated; cumulative adversity coefficients from these models are presented in Table 2 (Model 5). Within each gender, and for each mental health outcome, the standardized coefficients increase with increasing impact level. The low impact cumulative adversity variables do not even show a positive linear effect; 5/6 coefficients had negative signs and none reached statistical significance. In contrast, the medium impact sum scores were moderately associated with the 3 mental health variables, and the high impact sum scores were strongly associated with poorer mental health.
Table 3.
Impact size for individual adversities on mental health outcomes controlling for demographics
| Depressive symptoms | Delinquency | Drug use | |||||||
|---|---|---|---|---|---|---|---|---|---|
| L | M | H | L | M | H | L | M | H | |
| Hospitalized ever | ♀ | ♀♂ | ♀♂ | ||||||
| Parents separated/not divorced | ♂ | ♀ | ♀♂ | ♀♂ | |||||
| Missed/repeated grade ever | ♀ | ♂ | ♀♂ | ♀♂ | |||||
| Sent away from home ever | ♀♂ | ♀ | ♂ | ♀♂ | |||||
| Parent unemployed ever | ♀ | ♂ | ♀ | ♂ | ♀ | ♂ | |||
| Parent drink/drug problem ever | ♂ | ♀ | ♀ | ♂ | ♀♂ | ||||
| Life threatening accident | ♀ | ♂ | ♂ | ♀ | ♀♂ | ||||
| Victim of natural disaster | ♀♂ | ♀♂ | ♀ | ♂ | |||||
| Witnessed injury/death | ♀♂ | ♀♂ | ♀♂ | ||||||
| Combined sex abuse/assault | ♀♂ | ♀ | ♂ | ♀ | ♂ | ||||
| Physically assaulted | ♀♂ | ♀ | ♂ | ♀ | ♂ | ||||
| Physically abused | ♀♂ | ♀ | ♂ | ♀ | ♂ | ||||
| Seriously neglected | ♀♂ | ♀ | ♂ | ♂ | ♀ | ||||
| At least one parent died | ♂ | ♀ | ♂ | ♀ | ♂ | ♀ | |||
| Parents divorced | ♀ | ♂ | ♀ | ♂ | ♀♂ | ||||
NOTE: L = Low (≤.2), M = Medium (.2 - .4), H = High (≥.4 ) ♀= female, ♂ = male
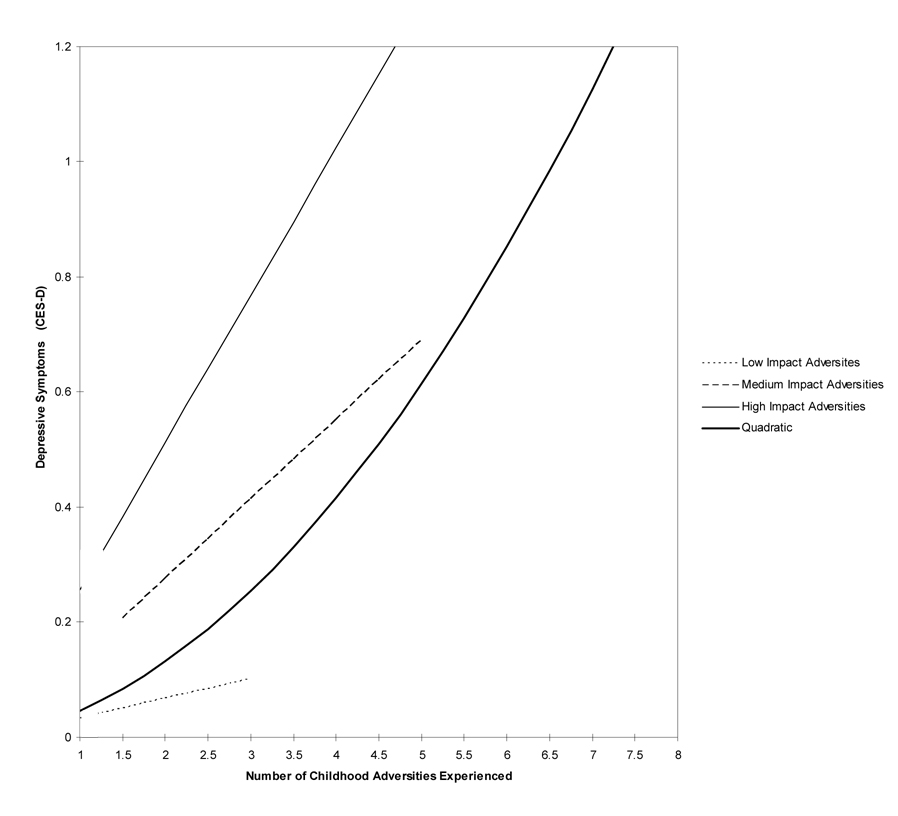
To determine whether accounting for the relative impact of adverse events actually explains the acceleration effect (i.e., the quadratic effect), a final model was estimated in which the squared cumulative adversity variable was added to Model 5 in Table 2 (Model 6). In contrast to Model 4, the quadratic effects for the CCA coefficients in Model 6 were all close to zero and did not significantly predict any mental health outcome. However, the coefficients for high impact events remained strong and statistically significant. In order to assess the influence of cases missing because of attrition or non-response, models in Table 2 were replicated using outcome variables with missing values replaced by mean imputation. Although most coefficients were somewhat attenuated, results were virtually identical in terms of the pattern and significance of CCA terms in all models. These results indicate that allowing adverse events of different impact levels to have separate slopes eliminated the quadratic effect of CCA on mental health. Figure 1 illustrates why this is the case, as the separate slopes for low, moderate, and high impact events approximate the shape of the quadratic curve.
Figure 1.
Depressed mood in males by cumulative adversity level categorized by highest impact level of adversity experienced
Note: Lines begin at mean number, and extend to upper end of frequency range, of adversities experienced for boys at the given impact level or lower.
Further confirmation that accelerating effects of cumulative adversity were due to much greater exposure to high impact events among those reporting more events is seen in Table 4, which presents the proportion of young adults experiencing a high impact event at each count level of the cumulative adversity score. These data demonstrate that the likelihood of experiencing a high impact event increases sharply as CCA increases. For example, female depressive symptoms are associated with events involving parental death, being sent away from home, or child maltreatment (such as sex abuse, physical abuse, and serious neglect) which tend to occur in the context of high cumulative adversity. Correspondingly, the likelihood of experiencing no high impact events decreased sharply as the cumulative impact score increased. This is even more notable due to the strong negative correlations (mean of -.64) between event prevalence in our sample and impact on mental health [see data in (identifying reference removed)]. Thus, high cumulative adversity is confounded with a history of experiencing severe and relatively rare adverse events, and the quadratic effect is a byproduct of the higher impact of these severe events at higher cumulative adversity levels.
Table 4.
For persons experiencing at least one event, percent of respondents with no high impact events and percent with at least one high impact event in each Cumulative Adversity Score level
| Standardized CESD impacts | Standardized Delinquency impacts | Standardized Drug Use impacts | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No High Impact events | At least 1 High impact event | No High Impact events | At least 1 High impact event | No High Impact events | At least 1 High impact event | |||||||
| n | % | N | % | n | % | n | % | n | % | n | % | |
| Event sum | Females | |||||||||||
| 1 | 145 | 59.2 | 33 | 15.4 | 170 | 43.6 | 14 | 24.6 | 175 | 42.8 | 3 | 6.0 |
| 2 | 76 | 31.0 | 62 | 29.0 | 131 | 33.6 | 16 | 28.1 | 133 | 32.5 | 5 | 10.0 |
| 3 | 19 | 7.8 | 40 | 18.7 | 44 | 11.3 | 11 | 19.3 | 55 | 13.4 | 4 | 8.0 |
| 4 | 4 | 1.6 | 38 | 17.8 | 28 | 7.2 | 9 | 15.8 | 32 | 7.8 | 10 | 20.0 |
| 5 | 1 | 0.4 | 23 | 10.7 | 16 | 4.1 | 5 | 8.8 | 10 | 2.4 | 14 | 28.0 |
| 6 | 0 | 0 | 12 | 5.6 | 1 | 0.3 | 2 | 3.5 | 3 | 0.7 | 9 | 18.0 |
| 7 | 0 | 0 | 6 | 2.8 | ---- | ---- | ---- | ---- | 1 | 0.2 | 5 | 10.0 |
| Males | ||||||||||||
| 1 | 186 | 50.4 | 5 | 5.6 | 188 | 61.0 | 20 | 15.5 | 186 | 50.3 | 5 | 5.7 |
| 2 | 114 | 30.9 | 18 | 20.2 | 92 | 29.9 | 31 | 24.0 | 114 | 30.8 | 18 | 20.5 |
| 3 | 47 | 12.7 | 19 | 21.3 | 23 | 7.5 | 32 | 24.8 | 48 | 13.0 | 18 | 20.5 |
| 4 | 16 | 4.3 | 17 | 19.1 | 3 | 1.0 | 21 | 16.3 | 16 | 4.3 | 17 | 19.3 |
| 5 | 5 | 1.4 | 7 | 7.9 | 1 | 0.3 | 16 | 12.4 | 5 | 1.4 | 7 | 8.0 |
| 6 | 0 | 0.0 | 11 | 12.4 | 1 | 0.3 | 2 | 1.6 | 0 | 0.0 | 11 | 12.5 |
| 7 | 1 | 0.3 | 9 | 10.1 | 0 | 0.0 | 6 | 4.7 | 1 | 0.3 | 9 | 10.2 |
| 8 | 0 | 0.0 | 2 | 2.2 | 0 | 0.0 | 1 | 0.8 | 0 | 0.0 | 2 | 2.3 |
| 9 | 0 | 0.0 | 1 | 1.1 | --- | --- | --- | --- | 0 | 0.0 | 1 | 1.1 |
Note: The middle 50% of the distribution is bolded.
Discussion
Research studies investigating the impact of CCA on adult mental health have proliferated in recent years. However, little attention has been paid to the effect that varying operationalization can have on study results or to the possibility that the mathematical relationship of CCA to some mental health dimensions may be more complex than a basic linear association. In our data, total CCA was related to depressive symptoms, drug use, and antisocial behavior in a quadratic manner. Without further elucidation, this higher order relationship could have been interpreted as support for a sensitization process in which the long-term impact of each additional adversity on mental health compounds as childhood adversity accumulates. However, further analysis revealed that this acceleration effect was an artifact of the confounding of high cumulative adversity scores with the experience of more severe events. Thus, respondents with higher total CCA had disproportionately poorer emotional and behavioral functioning because of both the number and severity of the adversities they were exposed to, not the cumulative number of different types of adversities experienced.
Consistent with Ross and Mirowsky’s research on stressful life events (Ross & Mirowsky, 1979), the explanatory power of CCA to predict mental health was much greater when adversities were “roughly” grouped by their severity based on estimates of impact determined on each of the mental health variables for men and women. Grouping allowed the cumulative effect to vary by impact level, our proxy measure of risk severity, and increased the efficiency of estimates. Because low-impact adversities did not present a cumulative hazard to young adult mental health, they functioned as suppressor events in the total sum score, consistent with Turner and Wheaton's (1997) expectation. Their inclusion increased the “noise” in the score and greatly watered down the influence of high-impact events. Thus, in addition to decreasing efficiency, total scores may seriously underestimate the cumulative effects of severe forms of childhood adversity, such as abuse and serious neglect.
Differential severity of each adversity included in an aggregate index is clearly an important factor to consider when constructing a cumulative adversity variable. Our research demonstrates the problems inherent in overlooking issues of differential impact and impact severity. The alternative focus on individual adversities, as seen in the work of Brown and associates, raises parallel problems to the extent that contextual data at the individual level is not used to specify severity. Previous research has established that individual adversities differ in their impact for men and women and in relation to specific mental health conditions (Horwitz, White, & Howell-White, 1996) and for different racial and ethnic groups (Turner & Lloyd, 2003); identifying reference removed). Consistent with this evidence of variable impact, we found that child maltreatment variables, including sex abuse/assault, physical assault, physical abuse and serious neglect, are high impact events for both genders for depressive symptoms, but only for boys for delinquency.
Finally, what is the substantive significance of the association between exposure to many adversities and exposure to severe adversities? Whereas many of the adversities had no net impact on mental health, it is important to keep in mind current sociological understandings of stressors as structurally (not randomly) generated (Aneshensel, Rutter, & Lachenbruch, 1991; Pearlin, 1989) and, as such, logically interrelated micro-level events within the social system. Evidence indicates that many of these kinds of adversities are more probable for low-SES youth and their families, so it is not surprising to find that severe events, such as personally violent and injurious events, appear to be embedded in a range of lesser-impact but potentially harmful exposures (e.g., having parents separate, getting injured, parental unemployment) (e.g.,(Turner & Avison, 2003; Turner & Lloyd, 1999). As noted earlier, evidence indicates that severe childhood adversities are likely to affect mental health and behavior in adolescence and the transition to adulthood (See (Gore, Aseltine, & Schilling, 2007). Whereas the experience of low-impact childhood events still allows for the preservation of social functioning and opportunities at the end of adolescence, such as pursuing higher education, severe events are more likely to further deplete psychological and social resources that are essential for this transition (Hammen, 1991; Quinton, Pickles, Maughan, & Rutter, 1993; Ronka & Pulkkinen, 1995). Thus, we believe that our findings are consistent with the broader developmental research on the transition to adulthood indicating that the effects of severe adversities compromise positive choices and development in school and relationships, in turn impacting mental health (e.g., (Macmillan & Hagan, 2004); identifying reference deleted).
Limitations and Conclusions
There are a number of limitations inherent in our data. First, as with other retrospective surveys, the assessment of childhood adversities may be subject to recall bias. We believe that our design minimized some important factors known to influence bias in that (a) we assessed childhood adversity in the early adult years when memory for childhood events should be maximized and (b) we associated childhood adversity with depressive symptoms assessed 2 years later in order to reduce the likelihood that level of depression influenced adversity memory and reporting (Schraedley, Turner, & Gotlib, 2002). However, the influence of participants’ mental health on reports of adversity occurrence may have biased our results in other ways. In addition, our assessment of childhood adversities is not exhaustive. It is possible that unmeasured adverse childhood events and/or varying aspects of the adversities (such as age at exposure) may have biased our impact estimates in unknown ways. Finally, the self-report nature of our outcomes may have resulted in under- or over-reporting of depressive, drug, and antisocial symptoms and behaviors compared to a clinical interview. Symptom assessment based on clinical interview, and more refined and complete measurements of childhood adversity, would advance the public health and clinical significance of our results. Additional studies that attempt to replicate our findings with alternative measures of both mental health outcomes and cumulative adversity are needed to thoroughly address these limitations.
Our results have implications for other studies of CCA and mental health. Our study determined that the potency of CCA as a predictive instrument is limited to its inclusion of moderate- and high-impact adversities. Our procedures for demonstrating the empirical implications of index composition are grounded in the body of research on event-weighting schemes; however, our results cannot offer conclusive advice on how to incorporate measures of event severity into cumulative indices. Rather, we hope that our results will encourage further sensitivity to the composition of cumulative indices and in interpretation of their effects.
Our research intersects with lines of research on vulnerable populations and suggests that investments in public education and other social services must be complemented with public health efforts targeting prevention of the most severe childhood adversities. Despite the evidence for considerable variation in the impact of the different adversities, the clusters of events involving violence and threat of violence, in particular, appear to have the most pervasive impact across population subgroups and in relation to various mental health and behavioral problems. From a public health perspective, the aim may not be to identify how small sets of adversities operate in relation to specific outcomes for specific groups. Instead, programs that generally support vulnerable families and communities in an effort to minimize the conditions that promote violence may have the greatest payoff.
Acknowledgments
This research is supported by grants from the National Institute of Mental Health (R01-MH55626) and from the William T. Grant Foundation. The authors gratefully acknowledge the support of Karen Bourdon, The National Institute of Mental Health (NIMH) Project Office and the Center for Survey Research which conducted the data collection. We thank Mary Ellen Colten, Dorothy Cerankowski, Phyllis Doucette, Jaime Glanovsky, Stacey Kadish, Michelle Poulin, and Karen Verrochi for their contributions to the project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Elizabeth A. Schilling, University of Connecticut Health Center East Hartford, Connecticut UNITED STATES
Robert H Aseltine, University of Connecticut Health Center, aseltine@uchc.edu.
Susan Gore, University of Massachusetts--Boston, Susan.Gore@umb.edu.
References
- Allison PD. Change score as dependent variables in regression analysis. Sociological Methodology. 1990;20:93–114. [Google Scholar]
- Anderson PL, Tiro JA, Price AW, Bender MA, Kaslow NJ. Additive impact of childhood emotional, physical, and sexual abuse on suicide attempts among low-income African American women. Suicide & Life-Threatening Behavior. 2002;Vol 32(2):131–138. doi: 10.1521/suli.32.2.131.24405. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, Rutter CM, Lachenbruch PA. Social structure, stress, and mental health: Competing conceptual and analytic models. American Sociological Review. 1991;56:166–178. [Google Scholar]
- Brown GW. Contextual measures of life events. In: Dohrenwend BS, Dohrenwend BP, editors. Stressful life events and their contexts. New York: Prodist; 1981. pp. 187–201. [Google Scholar]
- Brown GW, Harris T. Life events and illness. New York: Guilford Press; 1989. [Google Scholar]
- Caprara GV, Rutter M. Individual development and social change. In: Rutter M, Smith DJ, editors. Psychosocial disorders in young people. Chichester, U. K: Wiley; 1995. pp. 35–66. [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS. The conflict between statistical and theoretical significance. Journal of Health and Social Behavior. 1980;21(3):291–293. [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. Journal of the American Medical Association. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors. 2002;27(5):713–725. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- Elder GH. The Life Course and Human Development. In: Lerner RM, editor. Handbook of Child Psychology, Volume 1 Theoretical Models of Human Development. New York: Wiley; 1998. pp. 939–991. [Google Scholar]
- Gore S, Aseltine RH, Jr., Schilling EA. Transition to adulthood, mental health and adversity. In: Avison WR, McLeod JD, Pescosolido B, editors. Mental Health, Social Mirror. New York: Springer Verlag; 2007. pp. 219–237. [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: Differences in psychosocial functioning. Journal of Consulting and Clinical Psychology. 1995;63(1):90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;Vol 100(4):555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;Vol 68(5):782–787. [PubMed] [Google Scholar]
- Horwitz AV, White HR, Howell-White S. The use of multiple outcomes in stress research: a case study of gender differences in responses to marital dissolution. Journal of Health and Social Behavior. 1996;37(3):278–291. [PubMed] [Google Scholar]
- Kessler RC. A comment on 'A comparison of life-event-weighting schemes'. Journal of Health and Social Behavior. 1980;21(3):293–296. [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis: models of quantitative change. New York: Academic Press; 1981. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27(5):1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Macmillan R, Hagan J. Violence in the transition to adulthood: Adolescent victimization, education, and socioeconomic attainment in later life. Journal of Research on Adolescence. 2004;14(2):127–158. [Google Scholar]
- Mirowsky J, Ross CE. Weighting life events: A second look. Journal of Health and Social Behavior. 1980;21(3):296–300. [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13(2):355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Pearlin LI. The Sociological Study of Stress. Journal of Health & Social Behavior. 1989;30:241–256. [PubMed] [Google Scholar]
- Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica. 2000;101(1):46–59. doi: 10.1034/j.1600-0447.2000.101001046.x. [DOI] [PubMed] [Google Scholar]
- Pudrovska T, Schieman S, Pearlin LI, Nguyen K. The Sense of Mastery as a Mediator and Moderator in the Association Between Economic Hardship and Health in Late Life. Journal of Aging and Health. 2005;17(5):634–660. doi: 10.1177/0898264305279874. [DOI] [PubMed] [Google Scholar]
- Quinton D, Pickles A, Maughan B, Rutter M. Partners, peers, and pathways: Assortative pairing and continuities in conduct disorder. Development and Psychopathology. 1993;5(4):763–783. [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ronka A, Pulkkinen L. Accumulation of problems in social functioning in young adulthood: A developmental approach. Journal of Personality and Social Psychology. 1995;69(2):381–391. doi: 10.1037//0022-3514.69.2.381. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. A comparison of life-event-weighting schemes: Change, undesirability, and effect-proportional indices. Journal of Health and Social Behavior. 1979;20(2):166–177. [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Components of depressed mood in married men and women. The Center for Epidemiologic Studies' Depression Scale. American Journal of Epidemiology. 1984;119(6):997–1004. doi: 10.1093/oxfordjournals.aje.a113819. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64(1):80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Schraedley PK, Turner RJ, Gotlib IH. Stability of retrospective reports in depression: Traumatic events, past depressive episodes, and parental psychopathology. Journal of Health and Social Behavior. 2002;43:307–316. [PubMed] [Google Scholar]
- Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology. 2004;16(4):799–806. doi: 10.1017/s0954579404040015. [DOI] [PubMed] [Google Scholar]
- Settersten RA, Jr., Furstenberg FF, Jr., Rumbaut RG. The John D and Catherine T MacArthur foundation series on mental health and development Research network on transitions to adulthood and public policy. Chicago, IL: University of Chicago Press; 2005. On the frontier of adulthood: Theory, research, and public policy; p. 591. xvi. [Google Scholar]
- Turner HA, Butler MJ. Direct and indirect effects of childhood adversity on depressive symptoms in young adults. Journal of Youth and Adolescence. 2003;32:89–103. [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Social Science and Medicine. 2006;62(1):13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Lifetime traumas and mental health: the significance of cumulative adversity. Journal of Health and Social Behavior. 1995;36(4):360–376. [PubMed] [Google Scholar]
- Turner RJ, Wheaton B, Lloyd DA. The epidemiology of social stress. American Sociological Review. 1995;60:104–125. [Google Scholar]
- Turner RJ, Wheaton B. Checklist measurement of stressful life events. In: Cohen S, Kessler RC, Gordon LU, editors. Measuring stress: A guide for health and social scientists. Oxford University Press; 1997. pp. 29–58. [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40(4):374–404. [PubMed] [Google Scholar]
- Turner RJ, Avison WR. Status Variations in Stress Exposure: Implications for the Interpretation of Research on Race, Socioeconomic Status, and Gender. Journal of Health and Social Behavior. 2003;44(4):488–505. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: Racial/ethnic contrasts. Addiction. 2003;98(3):305–315. doi: 10.1046/j.1360-0443.2003.00312.x. [DOI] [PubMed] [Google Scholar]