Abstract
Objective
Diabetes care has become increasingly complex. We set out to quantify recent trends in the complexity of medication regimens and test ordering for diabetes patients continuously enrolled in health plans affiliated with a large, regional US health maintenance organization, with representation in the South and Midwest.
Research design and methods
We provide descriptive trends analysis of overall diabetes care complexity (number of components [i.e., glucose, blood pressure, cholesterol control], number of medications/tests) from 1995 to 2003 for adults with diabetes (N = 304233).
Main outcome measures
The main outcomes were (1) the proportion of patients receiving diabetes-related medications (blood glucose, blood pressure, and cholesterol control agents), (2) the average number of medications, (3) the proportion of patients receiving diabetes-related tests (glycosylated hemoglobin [HbA1c], urine microalbumin, and serum cholesterol), (4) and the average number of tests ordered within the first year that a patient had any indication of diabetes.
Results
The proportion of patients on cholesterol lowering drugs (18% → 39%, p < 0.01) and blood pressure lowering drugs (51% → 62%, p = 0.04) rose significantly, while the proportion on glucose lowering drugs fell (76% → 47%, p < 0.01). Among patients prescribed medications, the average total number of diabetes-related medications rose from 2.96 to 3.70 medications (p < 0.01) with smaller increases seen for glucose lowering (1.45 → 1.65, p < 0.01) and blood pressure lowering regimens (2.14 → 2.51, p < 0.01), and no change for cholesterol lowering drugs (1.23 → 1.19, p = 0.19). For laboratory tests, the proportion receiving cholesterol (40% → 58%), and urine microalbumin (4% → 18%) (all p’s < 0.01) rose significantly, while the testing rates for HbA1c remained unchanged. The average total number of tests ordered per year increased significantly from 3.34 to 4.10 (p < 0.01) with more modest increases observed for individual tests.
Limitation
Trends analyses are unadjusted for many clinical characteristics that might influence the complexity of diabetes care.
Conclusions
Diabetes care grew more complex with the largest change in the number of patients receiving multi-component diabetes care. While the use of blood pressure and cholesterol lowering drugs rose overall, the proportion of patients using glucose lowering drugs declined and the average number of prescribed glucose lowering drugs did not increase in a clinically significant manner.
Keywords: Complexity, Diabetes care, Pharmacotherapy
Introduction
In the past decade, clinical trials have clearly illustrated the benefits of multiple components of preventive care for patients with type 2 diabetes mellitus. In 1998, the United Kingdom Prospective Diabetes Study published its findings regarding the benefits of intensive glucose and blood pressure control1,2. In the same period, trials assessing the effects of cholesterol lowering medications reported large cardiovascular benefits in diabetic patients3,4. More recently, the STENO trial demonstrated the benefits of comprehensive diabetes care5. With the publication of these trials, comprehensive, multi-component diabetes care has come to include intensive control of blood pressure, cholesterol, prophylactic aspirin use, dietary changes, and regular exercise, in addition to intensive glucose control. The notion that standard comprehensive diabetes care includes multiple components of care beyond glucose control has strengthened over time.
In response to this emerging data, clinical practice guidelines have recommended a more intensive form of diabetes care with lower risk factor targets and greater frequency of risk factor testing6-11. For blood glucose control, the target glycosylated hemoglobin A1c (HbA1c) has been < 7% over the past 10 years and the recommended frequency of testing increased to 1-2 times per year in 199712. For blood pressure control, the target blood pressure changed from < 130/85 mmHg to < 130/80 mmHg in 200013,14. For serum cholesterol control, the recommended LDL cholesterol target changed in 1999 from < 100 mg/dL in patients with heart disease to < 100 mg/dL in all patients15. The recommendation for frequency of cholesterol testing also became more stringent in 1997 moving from annual testing in those with cholesterol abnormalities to annual testing for all12. In addition to changes in practice guidelines, the comprehensive nature of diabetes care has been promoted in several prominent national initiatives including the National Diabetes Education Program (ABCs of Diabetes) and the Diabetes Quality Improvement Program16,17.
Each of these changes in risk factor goal recommendations and new quality improvement initiatives encouraged greater use of medications and more frequent laboratory testing. The complexity of routine diabetes care (i.e., the number of components of care addressed and the number of medications/tests undertaken) has important implications for the safety and quality of life of patients, and the quality of diabetes care. First, documenting the average number of medications attributable to diabetes is important for public health concerns regarding polypharmacy. New care guidelines regarding the care of older diabetes patients have expressed specific concerns regarding the presence of more than four prescription drugs that can increase the risk of falls, hypoglycemia, and other adverse drug events18. Furthermore, knowledge of the average number of medications and diagnostic tests are important for communicating with patients with new onset diabetes. As these numbers rise we may in fact be affecting the quality of life of patients and these quality of life perceptions may be important determinants of treatment adherence19. Second, documenting the number of medications is important because it is an intermediate indicator of how the intensity and comprehensiveness of diabetes management is changing. In some cases, some investigators have actually suggested that tracking use of medication prescribing should in fact be the quality metric that physicians are measured by given the fact that actual risk factor control is oftentimes dictated by forces beyond the control of the physician20.
Most descriptions of the current state of diabetes care come from the quality of care literature, which has provided descriptions of risk factor levels achieved21-24 and the proportion of patients receiving specific processes of care23,25-28. These studies have typically not described the complexity of medication regimens required to achieve these risk factor levels. A select group of studies have begun to provide evidence that treatment related to diabetes care has grown more complex over time, but several questions remain unaddressed29,30. Neither of these studies provides a basic description of trends in the number of medications attributable to diabetes for individual patients over time. In the case of the National Ambulatory Medical Care Survey, the unit of analysis is the visit and not the patient, so the comprehensiveness of care in terms of medications and laboratory tests over time cannot be assessed. In addition, the survey places a cap on the total number of medications that may be recorded so the average number of medications cannot be determined. It is also unknown whether changes in the complexity of diabetes-related medications and changes in laboratory testing have occurred simultaneously or separately. Inaction in the face of abnormal risk factors or laboratory results has been labeled as clinical inertia31. Finally, we do not know the extent to which these trends in the complexity of care have varied across health plans.
We set out to address these questions by assessing recent trends in prescriptions and risk factor testing for the period 1995-2003 using the database of a large managed care organization. We assess changes in care for individual components of diabetes care and determine whether more patients are receiving multi-component comprehensive care.
Patients and methods
Data source
We examined claims data for patients enrolled in a large, regional US health plan from 1995 to 2004. This large umbrella organization includes over 30 separate managed care plans and spans the Midwest and Southern regions of the country. During the study period, there was no special organized effort to improve diabetes care across health plans.
Study population
Our study sample was non-pregnant adults (over 18 years of age) with diabetes using the union of HEDIS and Hebert criteria for identifying diabetes patients in administrative data32. Patients were eligible for inclusion based on ICD-9 codes (250-250.93, 357.2, 362-362.03, 366.41, 648.0) or use of any glucose lowering drugs32. Patients were excluded if they had any of the following ICD-9 codes (255.0, 256.4, 577.8, 648.8) or had an indication of steroid use. The patients were grouped in separate calendar year cohorts depending on the first date when they were identified as having diabetes. This date was defined as their first utilization date. Patients were then followed for a period of 1 year starting from their first utilization date. Therefore, we had nine cohorts corresponding to calendar years 1995-2003.
Outcomes of interest
We studied trends in both medication use and laboratory test ordering. Medication use was defined by prescriptions filled over the course of a year. For medications, we assessed the proportion of patient receiving glucose, blood pressure, and cholesterol lowering medications. In addition, we evaluated trends in the average number of distinct medications, in total and for each of the three categories of medications [i.e., (1) glucose, (2) blood pressure, (3) cholesterol lowering], prescribed to patients for the 1 year after their initial utilization of services. When counting medications, we could not distinguish between switches or additions of medications. We developed a comprehensive list of medications from quarterly National Drug Code directories for the period of interest. This listing of medications was compared with a list of unique medications prescribed to the plan’s diabetes patients to ensure no generic or brand names of drugs were missed. Individual glucose, blood pressure, and cholesterol medications were categorized by mode of action as defined by the NDC. Combination drugs were counted as individual agents for this analysis. Each form of insulin (e.g., Regular vs. Lantus) was categorized as an individual agent.
For laboratory tests, we tracked the proportion of eligible patients receiving different tests as well as the average number of tests ordered in the year following initial utilization of services. Specifically, we tracked (1) HbA1c (CPT code 83036), (2) any form of cholesterol testing [CPT codes: lipid panel (80061) or individual cholesterol elements: total cholesterol (82465) or LDL cholesterol (83721) or HDL cholesterol (83718) or triglycerides (84478)], and (3) urine microalbumin testing (CPT code 82043 or 82044).
Finally, we assessed trends in the proportion of patients receiving only medications, only laboratory tests, or both medications and laboratory tests related to diabetes.
Analysis
We present connected plots of the adjusted mean of the outcome variables over time illustrating the trend of diabetes care in this sample. The means were adjusted for age, age-squared, female, and interactions of female with age variable using random coefficient models where both the intercept and the coefficient on the time variable were specified as random, accounting for clustering of observations within managed care plans. The age-squared and the gender-age interaction terms were included in models in order to improve the precision of our time trend analysis. Clustering within plans was accounted for in an attempt to minimize the contribution that individual health plans might have had on secular trends. We tested to see if these trends were statistically significant. These tests were based on the estimated coefficients on the time variable in our random coefficient models. We also conducted unadjusted time trend analyses for the five largest and five smallest managed care plans for each of the outcomes of interest. All analyses of the UCHP data were undertaken after IRB approval from the University of Chicago.
Results
We identified a total of 304 233 patients with diabetes over all the years. The number of subjects varied from year to year, reflecting both changes in the number of newly diagnosed patients with diabetes and changes in health plan affiliation. The mean age of patients was 57 years of age and 46-52% of patients were women (Table 1). The proportion of diabetes patients on any medication related to glucose, blood pressure, and cholesterol control fell slightly between 1995 and 2003 (p = 0.0182) from 82% to 74%. For individual classes of drugs, the proportion of patients on glucose lowering medicines (76% → 47%, p-value < 0.001) declined, while the proportion of patients receiving blood pressure (51% → 62%, p = 0.04) and cholesterol lowering drugs (17.5% → 39%, p < 0.001) increased significantly over this period [Figure 1(A)]. The rate of decline in the receipt of any diabetes-related medications (8%) was slightly higher than the difference in the rate of decline for glucose lowering drugs and the sum of the rates of increase for the cholesterol and blood pressure drugs (3.5%). This suggests that despite the decline in the overall use of any diabetes related drugs over time, patients with diabetes were receiving treatments for more components of diabetes care. This is supported by the fact that the adjusted proportion of patients receiving all three components of diabetes drugs increased from 13% to 22% (p < 0.001) over this time.
Table 1. Population characteristics.
| Cohort | Total number of patients | Age (years) mean (sd) | Percentage of females |
|---|---|---|---|
| All | 304 233 | 56.7 (14.3) | 49.7% |
| 1995 | 14 331 | 54.4 (12.3) | 46.6% |
| 1996 | 19 955 | 56.2 (13.3) | 47.5% |
| 1997 | 33 205 | 57.9 (13.9) | 49.4% |
| 1998 | 51 239 | 56.5 (14.5) | 49.7% |
| 1999 | 48 196 | 55.3 (14.5) | 50.4% |
| 2000 | 74 846 | 58.4 (14.9) | 50.8% |
| 2001 | 13 889 | 56.8 (12.7) | 46.4% |
| 2002 | 35 826 | 54.6 (14.1) | 49.5% |
| 2003 | 12 746 | 58.8 (14.5) | 51.8% |
Figure 1.
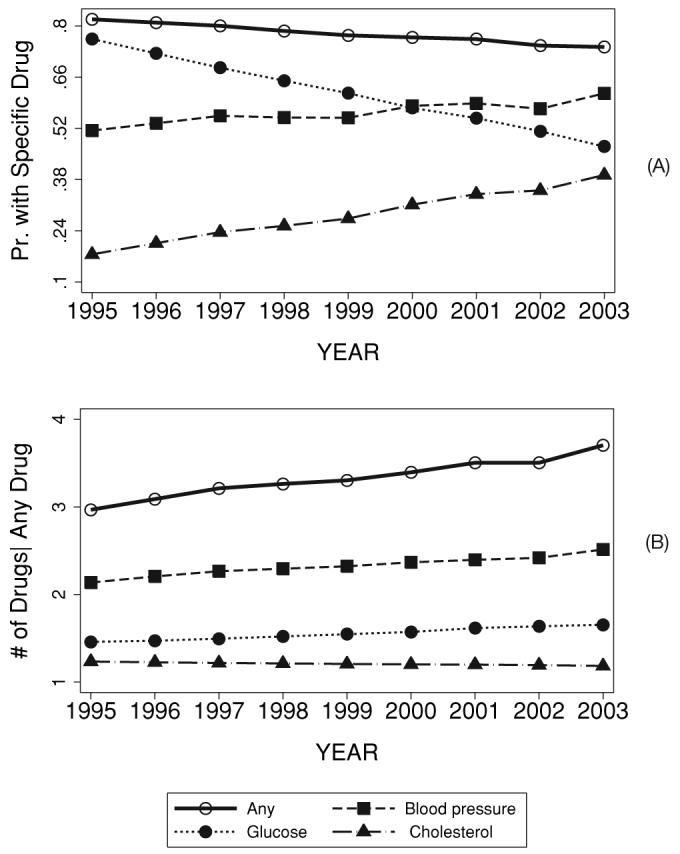
Adjusted trends in (A) the proportion of patients with any or specific types of diabetes drugs, and (B) the total number of diabetes related drugs conditional on any use of drugs (adjusted for age, age-squared, female and interactions of female with age variables)
Conditional on any usage of a specific class of medication, the number of specific medications taken by patients did increase significantly for glucose lowering (1.45 → 1.65, p-value < 0.0001) and blood pressure lowering medications (2.14 → 2.51, p-value < 0.0001), but not for cholesterol lowering medications (1.23 → 1.19, p-value = 0.187) [Figure 1(B)]. Among patients with any diabetes-related medication, the average total number of medications rose significantly from 2.96 medications to 3.70 medications (p-value < 0.0001). The growth rate in the total number of medications prescribed was faster than the increase in the number of medications for individual components of care.
The proportion of diabetes patients receiving any of the three tests studied did rise between 1995 and 2003 but the increase was not statistically significant (63% → 66%, p = 0.125) [Figure 2(A)]. However, significant increases were seen for the proportion of patients receiving a test for urine microalbuminuria (3.9% → 17.7%, p < 0.001) or a test for cholesterol levels (40% → 58%, p < 0.001) [Figure 2(A)]. The proportion of patients receiving a HbA1c test remained fairly constant at around 52% over this period (p-value = 0.812). Again, the rate of increase in the receipt of any diabetes-related test was lower than the sum of the rate of increases for the individual components. This is a comparison of the change in the observed total number of tests with the estimated change based on observations of individual tests. The difference in these numbers indicates that the growth in the number of patients receiving multiple tests was larger than the growth in the overall number of patients receiving any individual test over this time period. This is supported by the fact that the adjusted proportion of patients receiving all three component of diabetes tests increased from 12% to 30% (p < 0.001) over this time.
Figure 2.
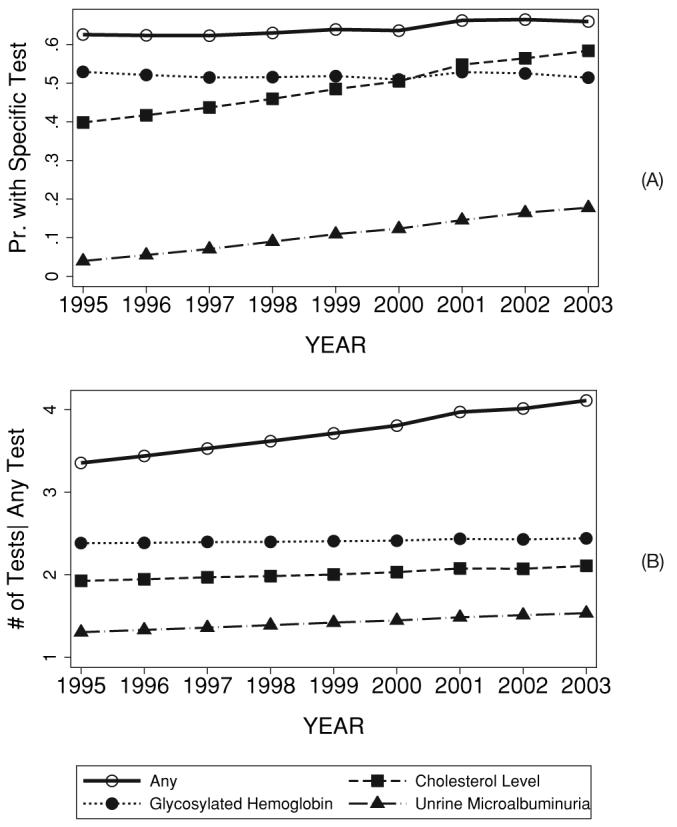
Adjusted trends in (A) the proportion of patients with any or specific types of laboratory tests, and (B) the total number of tests conditional on any use of tests (adjusted for age, age-squared, female and interactions of female with age variables)
Conditional on the receipt of any specific test, the average number of that specific test received by the diabetic patients within a year increased significantly for urine microalbuminuria (1.29 → 1.53, p-value = 0.003) and cholesterol levels (1.91 → 2.10, p-value =0.003) but not for HbA1c (2.37 → 2.42, p-value = 0.474). The increase in the total number of tests given the receipt of any test during the first year of enrollment was also significant (3.34 → 4.10, p-value < 0.001). The growth rate in the total number of tests given the receipt of any test was faster than that of any of the individual tests, again indicating that the growth in the number of patients receiving multiple tests was larger than the growth in the number of times patients received any individual test during the year of observation.
We find variability in the time trends for medication usage and laboratory testing across the managed care plans. This is first illustrated in Figure 3(A) where we plot the time trends of any medication usage for the five largest and the five smallest managed care plans. Any medication usage showed less variability in the baseline rates but more variability in the time trends across the managed care plans. Unlike medication usage, for laboratory test usage there was marked heterogeneity at the baseline across HMOs but less heterogeneity among health centers over time. This is illustrated in Figure 3(B) where we plot the unadjusted time trends of any test usage for the five largest and the five smallest managed care plans.
Figure 3.
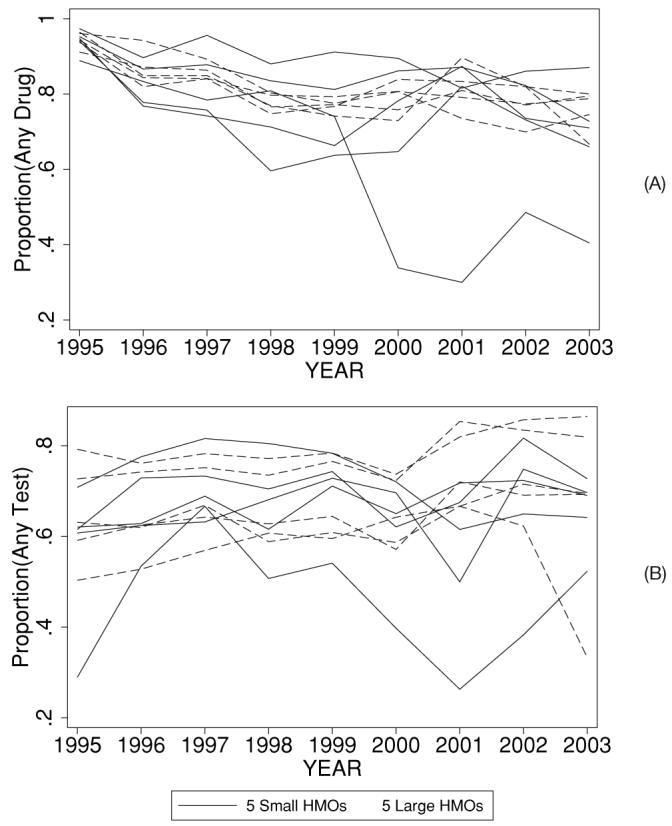
Unadjusted trends in the use of (A) any drugs and (B) any tests for the five smallest and five largest managed care plans
Finally, in terms of over-arching care trends, we found that the proportion of patients receiving at least one drug or one laboratory test declined slightly from 91.5% in 1995 to 90% in 2003 (p-value = 0.765) (Figure 4). This decline was mainly due to the decline in the proportion of patients who had at least one drug but no tests (29-24%, p = 0.01), but partially recovered by the growth in the proportion of patients who had at least one test but no drugs (10% → 16%, p = 0.07). The changes in the other factions of the population, i.e., those who had at least one test and at least one drug was insignificant (52% → 50%, p = 0.974).
Figure 4.
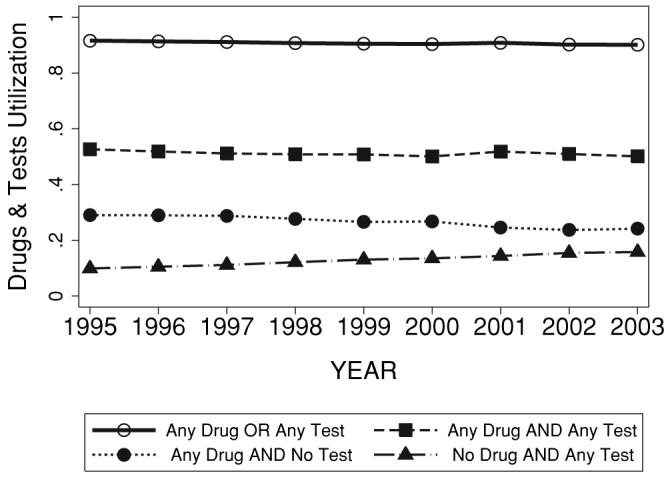
Complexity of diabetes care over time (adjusted for age, age-squared, female and interactions of female with age variables)
Discussion
Our study illustrates that the proportion of diabetes patients receiving multi-component diabetes care increased from 1995 to 2003 in the health plans of a large managed care organization. Among patients who received medications or laboratory tests, the average number of medications prescribed and the average number of laboratory tests ordered in 1 year of follow-up increased significantly. These changes are largely attributable to enhanced management of multiple components of diabetes care and less so to changes in the number of medications or tests used to address individual components of care. For example, the total number of medications prescribed related to diabetes increased significantly over the 8 years, while increases in the number of glucose and blood pressure control medications prescribed were modest. Similar patterns were observed for laboratory testing as well.
While more patients received multi-component diabetes care over time, we found divergent trends for treatment and testing related to cholesterol, blood pressure, and glucose control. The proportion of patients receiving treatments related to cholesterol and blood pressure management increased steadily over time, as did the proportion receiving cholesterol and urine microalbumin tests. Conversely, the proportion of individuals treated with glucose lowering medications declined, the percentage receiving HbA1c tests remained unchanged, and the frequency of HbA1c testing was stagnant. The decline in the proportion of patients on glucose lowering medications is inconsistent with what would be expected from recent care recommendations for glucose control. The observed decline may have several contributing factors. First, patients in the earlier years of our managed care dataset may have actually been individuals with established diabetes and, therefore, may have been on more glucose lowering medications. In the later years, as we had more years to follow patients within the health plan, patients may have been at or near the time of diagnosis and these patients may have been treated with diet and exercise alone. If this scenario is the case, then diabetes patients are being more aggressively treated with blood pressure and cholesterol lowering medications at an earlier stage of the disease. A second possibility is that some of these patients in later years may actually have been individuals at risk of having diabetes and may have been merely tested for diabetes. This type of misidentification would be attributable to an increase in screening for diabetes over time. If this scenario is the case, then patients at risk for diabetes are also being more aggressively treated with blood pressure and cholesterol lowering medications.
These results add greater depth to the picture of diabetes treatment complexity provided by previous studies. Our documentation of a rise in the proportion of patients using cholesterol lowering and blood pressure lowering drugs across multiple health plans is consistent with those of other studies29,30. A study of the National Ambulatory Medical Care Survey (NAMCS) from 1991 to 2000 found that the proportion of visits for diabetes patients associated with cholesterol lowering medications (4.1% → 17.3%) or blood pressure medications (35.9% → 42.3%) increased29. An analysis of data of two managed care plans also found increases in the proportion of patients using cholesterol lowering drugs and angiotensin-converting enzyme inhibitors30. On the other hand, our findings related to glucose lowering treatments diverge somewhat from prior reports. The NAMCS study reported a slight increase in the proportion of patients taking glucose lowering drugs. In contrast, we found a steep decline in the proportion on glucose lowering medications. Again, this decline in the proportion on glucose lowering medications may be attributable to the nature of our dataset and our approach to diabetes case finding.
Our study also provides new evidence that diabetes care trends do vary across health care settings for both drug and laboratory test utilization. Among our study health plans, initial baseline utilization of medications was similar across plans but diverged over time. Laboratory testing rates became less heterogeneous over time but still varied qualitatively. It is also important to note that the overall proportion of patients in our study health plans receiving HbA1c tests (52%) differed significantly from rates observed in contemporaneous studies. Among Medicare beneficiaries, 71% of patients had a HbA1c test in the period 1997-199927. In the TRIAD study, Veterans Affairs patients had a testing rate of 93% and managed care patients had a testing rate of 83% during the period 2000-200128. Differences in drug and laboratory test utilization may reflect differences in the populations but more likely reflect differences in the health care environments, where quality of diabetes care and efforts to standardize and improve diabetes care may be dramatically different.
The changes in diabetes care that we observed in this managed care organization are a reflection of secular trends. It is striking to note that in this care setting that clear changes occurred with regard to cholesterol and blood pressure management with little or no change in glucose control management. Since no coordinated intervention was in place to encourage cardiovascular prevention for diabetes patients among these health plans, the observed care trends suggest that public health efforts including multiple new care guidelines may have had an affect on daily practice13,17,33. At the same time, it is possible that glucose control management did not receive adequate attention without the presence of a coordinated diabetes quality improvement program. The inconsistent nature of these care trends indicates the importance of continuing to improve diabetes care in a comprehensive manner in order to meet multiple goals set by care guidelines and performance measures8,17.
There are several limitations of this study. Prescribing of medications and the use of laboratory tests are crude measures of what represents comprehensive diabetes care or care complexity. A mere count of the number of medications does not acknowledge differences between insulin and oral medications; we plan to account for this in future analyses. In addition, daily diet and exercise, routine glucose monitoring, as well as routine visits with specialists such as ophthalmologists, podiatrists, and dieticians are services that were not specifically examined here. We also did not have access to actual risk factor levels, which are important for judging the quality of diabetes care received. However, the purpose of our study was not to assess the quality of diabetes care per se, but to describe the dissemination of medical technology related to diabetes. Our trends are also unadjusted for many clinical characteristics that might influence the nature of diabetes care. However, there were no specific changes in the health plan’s enrollment policy that would have led to systematic changes in the demographic characteristics of enrolled patients. Lastly, despite the regional representation of our study, our results may not be generalizable to the overall population of patients with diabetes mellitus in the United States because all of our patients were insured in managed care plans that had a drug benefit program.
The emergence of new clinical trial data regarding the benefits of various components of diabetes care have resulted in an evolution of clinical practice recommendations for diabetes care. These recommendations essentially call for greater use of medications and laboratory tests and our study illustrates that the proportion of diabetes patients receiving medications or laboratory tests across multiple components of care has increased, while the intensity of care for individual components of care has changed less so. In the case of medications, the current average number of four medications is already at or near the threshold for increased risks of falls, hypoglycemia, and other adverse drug events. This is a particular concern for elderly patients. As care for diabetes continues to evolve, it is important to consider issues of treatment complexity as they may impact the quality of life of the large numbers of individuals living with diabetes and the routine costs of caring for such patients.
Conclusions
The proportion of diabetes patients receiving multi-component diabetes care increased in the last decade in a large managed care organization. Among patients who received diabetes-related care, the average number of medications prescribed increased from 2.96 to 3.70 medications and the average number of laboratory tests ordered in 1 year of follow-up increased from 3.34 to 4.10 tests. More patients appear to be receiving multi-component diabetes care, which may decrease important complications but may also increase the daily burdens of routine diabetes care.
Acknowledgments
Declaration of interest: This study was supported by a grant from The Robert Wood Johnson Foundation Changes in Health Care Financing and Organization (HCFO ) titled ‘Utilization Review: Cost Savings and Quality of Care’, (Grant No. 44194), a National Institute on Aging Career Development Award (ESH, K23 AG21963), and a NIDDK Diabetes Research and Training Center (ESH and WM P60 DK20595). The authors acknowledge the assistance of Thomas Horstman with data preparation.
Footnotes
This study was presented in part at the 2004 Annual Meeting of the Society for Medical Decision Making and at the 2005 Annual Meeting of the Society of General Internal Medicine
References
- 1.UK Prospective Diabetes Study Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 2.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. Br Med J. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 3.Pyorala K, Pedersen TR, Kjekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) Diabetes Care. 1997;20:614–20. doi: 10.2337/diacare.20.4.614. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg RB, Mellies MJ, Sacks FM, et al. Cardiovascular events and their reduction with pravastatin in diabetic and glucose-intolerant myocardial infarction survivors with average cholesterol levels: subgroup analyses in the Cholesterol and Recurrent Events Trial. Circulation. 1998;98:2513–9. doi: 10.1161/01.cir.98.23.2513. [DOI] [PubMed] [Google Scholar]
- 5.Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. New Eng J Med. 2003;348:383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2002;25:S33–S49. doi: 10.2337/diacare.26.2007.s33. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003;26:S33–S50. doi: 10.2337/diacare.26.2007.s33. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association Standards of medical care in diabetes. Diabetes Care. 2004;27:S15–S35. doi: 10.2337/diacare.27.2007.s15. [DOI] [PubMed] [Google Scholar]
- 9.The American Association of Clinical Endocrinologists Medical guidelines for the management of diabetes mellitus: the AACE system of intensive diabetes self-management - 2002 update. Endocrine Practice. 2002;9:41–82. [PubMed] [Google Scholar]
- 10.Vijan S, Hayward RA. Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med. 2003;138:593–602. doi: 10.7326/0003-4819-138-7-200304010-00018. [DOI] [PubMed] [Google Scholar]
- 11.Vijan S, Hayward RA. Pharmacologic lipid-lowering therapy in type 2 diabetes mellitus: background paper for the American College of Physicians. Ann Intern Med. 2004;140:650–8. doi: 10.7326/0003-4819-140-8-200404200-00013. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association Standards of medical care for patients with diabetes mellitus. Diabetes Care. 1997;20:S5–S13. [Google Scholar]
- 13.Joint National Committee on Prevention, Detection, Evaluation. Treatment of High Blood Pressure. the National High Blood Pressure Education Program Coordinating Committee The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–46. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. J Am Med Assoc. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association Standards of medical care for patients with diabetes mellitus. Diabetes Care. 1999;22:S32–S41. [PubMed] [Google Scholar]
- 16.Clark CM, Fradkin JE, Hiss RG, et al. The national diabetes education program, changing the way diabetes is treated: comprehensive diabetes care. Diabetes Care. 2001;24:617–8. doi: 10.2337/diacare.24.4.617. [DOI] [PubMed] [Google Scholar]
- 17.Fleming BB, Greenfield S, Engelgau MM, et al. The diabetes quality improvement project. Diabetes Care. 2001;24:1815–20. doi: 10.2337/diacare.24.10.1815. [DOI] [PubMed] [Google Scholar]
- 18.Brown AF, Mangione CM, Saliba D, Sarkisian CA. California Healthcare Foundation/American Geriatrics Society Panel on Improving Care for Elders with Diabetes. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51(Suppl 5):S265–S280. doi: 10.1046/j.1532-5415.51.5s.1.x. [DOI] [PubMed] [Google Scholar]
- 19.Vijan S, Hayward RA, Ronis DL, Hofer TP. The burden of diabetes therapy: implications for the design of effective patient-centered treatment regimens. J Gen Intern Med. 2005;20:479–82. doi: 10.1111/j.1525-1497.2005.0117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerr EA, Smith DM, Hogan MM, et al. Building a better quality measure: are some patients with ‘poor quality’ actually getting good care? Medical Care. 2003;41:1173–82. doi: 10.1097/01.MLR.0000088453.57269.29. [DOI] [PubMed] [Google Scholar]
- 21.Saydah SH, Fradkin JE, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. J Am Med Assoc. 2004;291:335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 22.George PB, Tobin KJ, Corpus RA, et al. Treatment of cardiac risk factors in diabetic patients: how well do we follow the guidelines? Am Heart J. 2001;142:857–63. doi: 10.1067/mhj.2001.119132. [DOI] [PubMed] [Google Scholar]
- 23.Saaddine JB, Engelgau MM, Beckles GL, et al. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 24.Smith NL, Savage PJ, Heckbert SR, et al. Glucose, blood pressure, and lipid control in older people with and without diabetes mellitus: the cardiovascular health study. J Am Geriatr Soc. 2002;50:416–32. doi: 10.1046/j.1532-5415.2002.50103.x. [DOI] [PubMed] [Google Scholar]
- 25.Beckles GL, Engelgau MM, Narayan KMV, et al. Population-based assessment of the level of care among adults with diabetes in the U.S. Diabetes Care. 1998;21:1432–8. doi: 10.2337/diacare.21.9.1432. [DOI] [PubMed] [Google Scholar]
- 26.Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries. J Am Med Assoc. 2000;284:1670–6. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- 27.Arday DR, Fleming BB, Keller DK, et al. Variation in diabetes care among states. Diabetes Care. 2002;25:2230–7. doi: 10.2337/diacare.25.12.2230. [DOI] [PubMed] [Google Scholar]
- 28.Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141:272–81. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 29.Grant RW, Pirraglia PA, Meigs JB, et al. Trends in complexity of diabetes care in the United States from 1991 to 2000. Arch Intern Med. 2004;164:1134–9. doi: 10.1001/archinte.164.10.1134. [DOI] [PubMed] [Google Scholar]
- 30.Nau DP, Garber MC, Herman WH. The intensification of drug therapy for diabetes and its complications: evidence from 2 HMOs. Am J Managed Care. 2004;10:118–23. [PubMed] [Google Scholar]
- 31.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 32.Hebert PL, Geis LS, Tierney EF, et al. Identifying persons with diabetes using Medicare claims data. Am J Med Qual. 1999;14:270–7. doi: 10.1177/106286069901400607. [DOI] [PubMed] [Google Scholar]
- 33.Expert Panel on Detection Evaluation. Treatment of High Blood Cholesterol in Adults Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults [Adult Treatment Panel III] J Am Med Assoc. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]


