Abstract
Pain-related fear has been associated with avoidance behavior and increased risk for chronic low back pain; however, few studies have examined how pain-related fear relates specifically to motion of the spine following an acute episode of back pain. Thirty-six participants with a recent episode of low back pain were recruited from the general population using a combination of fliers and radio advertisements. To explore the natural recovery from low back pain we recruited individuals who were not seeking medical care. Participants performed a forward bending task at 3, 6, and 12 weeks following onset of low back pain. Three-dimensional joint motions of the spine and hip were recorded using an electromagnetic tracking device. Initial assessments of low back pain and pain-related fear were then correlated with joint excursions observed during each forward bending. Lumbar motion was inversely related to pain-related fear, but not low back pain, at all three testing sessions. In contrast, hip motion was inversely related to pain at all three testing sessions but was not related to fear. These findings suggest that pain-related fear results in avoidance behavior that specifically limits or restricts motion of the lumbar spine.
Keywords: Lumbar flexion, Pain-related fear, Back Pain
Introduction
Physical examination of low back pain includes the evaluation of trunk range of motion, typically using a trunk flexion task in which the patient bends forward as far as possible with the knees extended and then returns to an upright posture. The examiner observes the relative excursions of the spine and hip while noting any change in symptoms [29]. Although this procedure is a part of the clinical assessment of disability determination, it has not been shown to be closely related to function [23].
Whereas there is evidence that lumbar range of motion is reduced in patients with sub-acute and chronic low back pain [9, 18, 25, 31, 36, 42], range of motion has been an unpredictable correlate of disability. For example, Parks and colleagues reported no relationship between lumbar motion and functional test scores in chronic back pain [23], Poitras et al. [24] reported weak positive associations between lumbar range of motion and disability in sub-acute and chronic back pain, and Simmonds and colleagues [31] found that lumbar flexion was inversely related to disability in chronic back pain patients. An important individual difference factor that may help clarify these inconsistent findings is pain-related fear.
According to the fear-avoidance model of low back pain [3, 39], individuals who perceive pain in a threatening, catastrophic manner (e.g., as a sign of potential tissue damage) are more likely to avoid behaviors that increase their anxiety. Consistent with this model, acute and chronic low back pain patients with high pain-related fear typically show submaximal performance on a variety of physical challenges such as straight leg raise, knee-extension-flexion, trunk-extension-flexion, and weight lifting [1, 2, 5, 7, 11, 12, 16, 30, 34, 38, 41]. These findings suggest that performance during forward bend tasks, as measured by thoracic, lumbar and hip excursions, may be influenced by individual differences in pain-related fear. Fritz and colleagues have previously reported significant correlations between measures of fear avoidance behavior and a composite index of physical impairment that included four lumbar range of motion variables (total flexion, extension, average side bending, and average straight leg raise), two measures of muscle strength (sit-up, bilateral straight leg raise), and a measure of spinal tenderness [10, 11]. Further, a recent study by George et al found a negative correlation between fear avoidance beliefs and total lumbar flexion in an acute population of back pain patients [14]. In our own laboratory we have recently demonstrated an inverse relationship between pain-related fear and lumbar motion during target reaching tasks, suggesting that a similar relationship may also be evident in forward bending [37].
The present study examined the relationship between pain-related fear and forward bending performance in individuals with sub-acute low back pain. Participants were recruited shortly after the onset of an episode of low back pain and were evaluated at 3, 6, and 12 weeks during natural recovery. Our primary aim was to examine the influence of initial levels of pain-related fear on joint motions used to perform forward bending. A second aim was to examine the relationships between fear and joint motions measured at initial testing (i.e., 3 weeks) with subsequent disability at 6 and 12 weeks following onset of low back pain.
Method
Participants
Forty-three participants with sub-acute, self-reported low back pain were recruited from the general population using a combination of fliers and radio advertisements. None of the participants sought medical care for their back pain. Participants were initially tested at 3 weeks (±5 days) following onset of an episode of low back pain. During this initial assessment participants completed a series of questionnaires and completed a forward bending task (see below). Joint motions during a forward bending task were subsequently retested at 6 and 12 weeks to determine if their movement strategies changed over time. Participants were excluded if they had a history of chronic back pain or a prior episode of back pain within the preceding year. Thirty-six participants (23 women and 13 men) completed all three testing sessions and data for these participants will be reported for all analyses. Participant characteristics are presented in Table 1.
Table 1.
Participant characteristics
| Mean | SD | |
|---|---|---|
| Age (years) | 26.9 | 6.9 |
| Height (cm) | 169.5 | 7.6 |
| Weight (kg) | 69.5 | 14.0 |
| Pain anxiety symptoms scale | 58.3 | 23.9 |
| Tampa scale for kinesiophobia | 36.9 | 7.8 |
| Pain catastrophizing scale | 15.1 | 9.3 |
| McGill pain questionnaire-pain rating index | 9.4 | 6.9 |
| Roland Morris disability questionnaire | 7.2 | 5.9 |
Questionnaires
Tampa scale for kinesiophobia
The Tampa scale for kinesiophobia (TSK) [17] is a 17-item questionnaire that assesses fear of re-injury due to movement. Respondents rate their degree of agreement with each of the 17 statements and these ratings are summed to yield a total score that ranges from 17–68. Higher scores reflect greater fear of re-injury. The TSK has been shown to have acceptable internal consistency (Cronbach’s = 0.77), and concurrent validity [7].
McGill pain questionnaire
The McGill pain questionnaire (MPQ) [21, 22] is one of the most widely used methods of pain evaluation in both clinical and experimental research. The McGill pain questionnaire provides quantitative, multidimensional pain ratings. In addition to a present pain intensity rating (MPQ-PPI), respondents choose adjectives from 20 categories of words that describe pain, and a sum of ranks from each category is used to compute a total pain-rating index (MPQ-PRI). Although separate scores for sensory, affective, and evaluative dimensions of pain can also be derived from this scale, modest alpha coefficients for some of the subscales (i.e., 0.68–0.81), combined with continuing debate over the factor structure, suggest that the pain rating index is the preferred measure of pain experience derived from this scale. Further, the MPQ has also been shown to have good test-retest reliability [15].
Pain anxiety symptoms scale
The pain anxiety symptoms scale (PASS) [19] is a 40-item measure of pain-related fear that provides both a total score and subscale scores of (1) fearful appraisal of pain, (2) cognitive anxiety, (3) physiological anxiety, and (4) escape and avoidance behavior. For each item respondents indicate the degree to which they agree with statements regarding what they think about or do when in pain. Responses are provided on a 5-point scale, with the anchors of (0) “never” and (5) “always”. The PASS has demonstrated adequate internal consistency, test-retest reliability, and concurrent validity across a variety of clinical pain samples [19, 20, 26].
Pain catastrophizing scale
The pain catastrophizing scale (PCS) [33] consists of 13 items describing different thoughts and feelings that individuals may experience when they are in pain. Respondents reflect on past painful experiences and then indicate the degree to which they experienced each of 13 thoughts or feelings when experiencing pain, on 5-point scales with the end points (0) “not at all” and (4) “all the time”. The PCS has excellent psychometric properties, including internal consistency (Cronbach’s alpha = 0.87), test-retest reliability (r = 0.75 at 6 weeks), and construct validity [32].
Roland Morris disability questionnaire
The Roland Morris disability questionnaire (RMDQ) [27] consists of 24 statements concerning restriction of daily activities due to back pain, including items related to mobility, self-care and sleep. Items are scored as either 0 (false) or 1 (true), resulting in a range of scores from 0–24 with higher scores representing greater dysfunction. Psychometric properties of reliability and validity are well supported across a range of clinical studies [28].
Forward bend task
Participants were asked to bend forward as far as possible while keeping their knees extended. They were told to move at a comfortable pace, pause once they have bent as far as possible, and then return to an upright posture.
Data collection
Movements of the trunk and limb segments were recorded using a magnetic based kinematic system that can track the three-dimensional coordinates of sensors with a spatial resolution of 0.03 inch (Ascension™). Sensors were attached by Velcro® straps to the limb segments (at the midpoint between the joints) of the right and left shank, thigh, arm, and forearm, as well as the thoracic vertebra (T1), lumbar vertebra (L1), and the sacrum. Kinematic data were collected at 100 Hz for a total of 5 s, and data collection began 500 ms prior to the “go” signal.
Data reduction and analyses
Motion Monitor software (Innovation Sports, Chicago, IL) was used to derive time series joint angle data of the thoracic spine, lumbar spine, and hip joints using an Euler angle sequence (flexion, rotation, lateral flexion). Thoracic spine motion was defined by the change in orientation of the sensor on T-1 relative to the sensor on L-1. Lumbar spine motion was defined by the change in orientation of the sensor on L-1 relative to the sensor on the sacrum. Hip motion was defined as the change in orientation of the sensor on the sacrum relative to the sensor on the right thigh. Since the motions used to perform these movements were primarily in the sagittal plane, we restricted our analyses to thoracic spine, lumbar spine, and hip flexion angles. The time series joint angle data were first filtered using a fourth order zero lag Butterworth filter with cutoff frequency of 6 Hz. The peak-to-peak changes in joint angles were extracted from the time series data for analyses.
Results
Relationships between psychological measures and motion parameters
Pearson-correlation analyses were conducted to examine the relationships between psychological measures (MPQ, TSK, PASS, and PCS) and motion (thoracic spine, lumbar spine, and hip) evaluated at 3, 6, and 12 weeks following onset of back pain. As seen in Table 2, there were no significant relationships between the psychological measures and thoracic flexion for any testing session. Kinesiophobia (TSK), pain-related fear (PASS), and pain catastrophizing (PCS) were each associated with less lumbar flexion during a maximum forward bending task at 3 weeks following onset of back pain. Pain-related fear showed the highest correlation to lumbar flexion at each testing session. While lumbar flexion was not significantly related to pain, higher levels of pain were associated with less hip flexion at each follow up interval.
Table 2.
Relationships between psychological measures obtained at initial assessment (week 3) and joint excursions measured at 3, 6, and 12 weeks following onset of back pain
| Thoracic flexion | Lumbar flexion | Hip flexion | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 3 weeks | 6 weeks | 12 weeks | 3 weeks | 6 weeks | 12 weeks | 3 weeks | 6 weeks | 12 weeks | |
| MPQ | −0.17 | −0.14 | −0.20 | −0.24 | −0.21 | −0.04 | −0.36* | −0.35* | −0.37* |
| TSK | −0.18 | −0.01 | −0.13 | −0.41** | −0.27 | −0.22 | −0.19 | −0.14 | −0.03 |
| PASS | −0.17 | −0.00 | −0.02 | −0.54** | −0.32* | −0.27* | −0.04 | −0.01 | 0.05 |
| PCS | −0.08 | −0.16 | −0.01 | −0.35* | −0.21 | −0.14 | −0.14 | −0.15 | −0.03 |
MPQ McGill pain questionnaire, TSK Tampa scale for Kinesiophobia, PASS pain anxiety symptoms scale, PCS pain catastrophizing scale
** p < 0.001; * p < 0.05, one-tailed
Repeated measures MANOVA high versus low pain-related fear
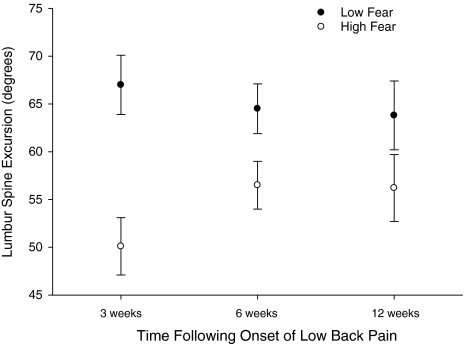
To further examine group differences in lumbar spine motion during recovery, participants were assigned to either a high or low pain-related fear group based on a median split of PASS scores from the initial testing session. To assure groups balanced by gender, the median split was conducted separately by sex due to differences in PASS scores for women (Mdn = 56) and men (Mdn = 69). A 3-way MANCOVA for repeated measures design was performed with between subject factors of group (high fear, low fear) and sex and a within subject factor of time from onset of back pain (3, 6, 12 weeks). The weekly back pain ratings from the McGill pain questionnaire-pain rating index were included as covariates. Results involving the repeated measures factor were evaluated based on the multivariate Pillai’s trace statistic. Results of this 2 group × 2 sex × 3 time MANCOVA revealed a significant main effect of group (p < 0.01, ηp2 = 0.23, observed power = 0.82) and a significant group by time interaction (p < 0.05, ηp2 = 0.19, observed power = 0.59). As can be seen in Fig. 1, the group by time interaction reflected a significant increase in lumbar flexion from 3 to 6 weeks in the high fear group (p < 0.01, ηp2 = 0.23, observed power = 0.89), but no change between 6 and 12 weeks. Conversely, lumbar flexion did not change across the three testing sessions for the low fear group. A direct comparison between groups revealed significantly reduced lumbar flexion in the high versus low fear group at 3 weeks (p < 0.01, one-tailed, ηp2 = 0.32, observed power = 0.95), 6 weeks (p < 0.05, one-tailed, ηp2 = 0.14, observed power = 0.57) and 12 weeks (p < 0.05, one-tailed, ηp2 = 0.09, observed power = 0.39). Figure 2 illustrates the effect of pain-related fear on movement strategy for participants in the low and high pain-related fear groups. This figure suggests that high fear is associated with reduced motion of the lumbar spine, necessitating compensatory adjustments in the joints of the reaching limb and the lower extremities.
Fig. 1.
The effects of group and day on the peak to peak joint excursions of the lumbar spine are depicted
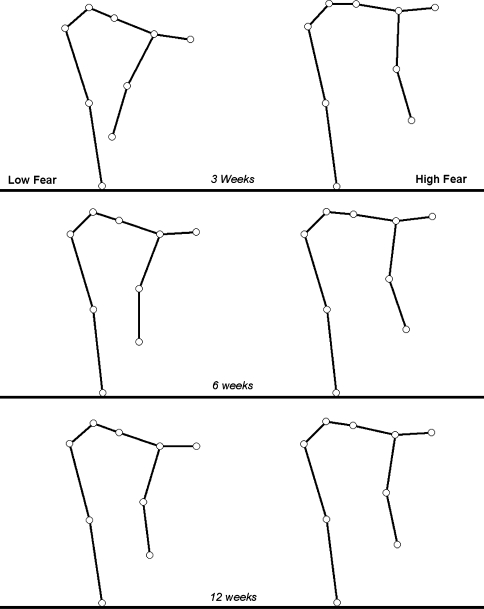
Fig. 2.
The effect of fear-related pain on the maximal excursions of the lumbar spine at each testing session is illustrated. These figures were derived from the mean joint excursions and the mean segment lengths of the participants. The stick-figures clearly illustrate the group differences in lumbar excursions used to perform a forward bend
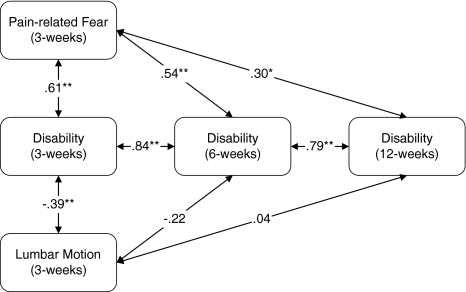
Relationships between pain-related fear, lumbar motion and disability
Correlational analyses were conducted to examine the relationships between pain-related fear, lumbar motion and disability during recovery (i.e., 3, 6, 12 weeks). As illustrated in Fig. 3, initial pain-related fear was positively correlated with reported disability at 3, 6, and 12 weeks following onset of back pain. Although initial pain-related fear was negatively correlated with lumbar motion at each testing session (see Table 2), initial lumbar motion was only related to disability at 3 weeks following onset of back pain. A partial correlation between lumbar motion and disability, controlling for pain-related fear, was not significant (r = −0.10, p = 0.28).
Fig. 3.
Correlations between pain-related fear, lumbar motion, and self-reports of disability at 3, 6, and 12 weeks following onset of back pain. **p < 0.001; *p < 0.05, one-tailed
Discussion
The results of this study provide evidence that performance on the forward bend task, a standard clinical examination procedure, is significantly influenced by fear of pain in men and women with sub-acute low back pain. This relationship was observed across three different standardized measures associated with fear of pain and harm upon movement (i.e., PASS, TSK, and PCS), suggesting a robust and potentially important clinical finding. Although pain-related fear has previously been related to submaximal performance on a variety of physical challenges [1, 2, 5, 7, 11, 12, 16, 30, 34, 35, 38, 41] a unique feature of this study is a mapping of this construct to joint movements during performance of a routine assessment procedure for patients with low back pain. Specifically, at each testing session participants with high levels of fear displayed less lumbar flexion during forward bending, even after statistically controlling for pain. Failure to find similar relationships between fear and flexion of the thoracic spine and hip suggests that this is not a generalized tendency to avoid all joint movement but rather a specific restriction of lumbar motion. Interestingly while decreased hip flexion was not related to high levels of fear, it was related to pain at each testing session. Thus, patient performance during forward bending may be influenced by a complex combination of pain and fear, each with independent effects on spine and hip joint motion.
A second noteworthy aspect of the current study is the change in the nature of the relationship between pain-related fear and lumbar motion over time. Participants with low levels of fear had relatively large excursions of the lumbar spine that did not change from 3 to 12 weeks during recovery. While those with high levels of fear displayed increased lumbar flexion between the 3 and 6 week testing sessions, they did not show continued improvement at the 12-week testing session and continue to exhibit less lumbar flexion compared to those with low fear (Fig. 2). The observed changes in lumbar flexion over time in the high fear group may be due to physical changes related to healing and reduced pain, to decreases in fear resulting from repeated exposure to the forward bend task [8], and/or to decreases in fear due to repeated exposure to similar movements in everyday life [6, 40]. Nonetheless, persistent differences between the groups at week 12 suggest that fear continues to influence range of motion and possibly recovery. Hence it is important to consider patients’ level of fear when interpreting performance on a forward bending task in follow-up examinations.
While the current results provide evidence that pain-related fear influences the lumbar motion during forward bending, they also suggest that lumbar motion measured at 3 weeks is not significantly correlated with disability at 6 and 12 weeks following the onset of low back pain (Fig. 3). In line with our initial prediction, the current findings suggest that pain-related fear may help clarify why range of motion on the forward bend task has been an inconsistent predictor of disability [23, 24, 31, 36]. Results of the partial correlation analyses demonstrate that the relationship between performance on the forward bend task and disability is driven by the tendency of people with high fear to restrict motion of the lumbar spine. Our findings indicate that initial levels of pain-related fear are significantly correlated with disability up to 3 months following the onset of low back pain, which is consistent with the existing evidence that fear avoidance behavior is a potent predictor of future disability and risk for chronic pain [4, 6, 7, 10, 11, 13, 41].
Although our sample was sufficient to detect significant relationships between fear and disability, it should be noted that larger and more diverse back pain samples are needed to more fully explore the relationships between pain-related fear, restriction of movement, and individual differences in recovery. These relationships may differ as a function of a variety of factors, such as age, sex, and number of prior episodes of back pain, and therefore further research is needed that considers these potential moderating factors. Future studies would also benefit by examining these relationships in other movement paradigms as forward bending may be perceived as particularly threatening to those with fear of pain and reinjury, and hence performance on this task may reveal more about avoidance due to fear rather than actual range of motion. In response to this potential limitation we have been conducting assessments of movement strategies adopted by acute and chronic low back pain patients during the performance of natural reaching tasks [37]. Finally, future studies need to examine if differences in pain-related fear influence lumbar excursions in a sample of individuals with no history of low back pain.
What implications do these findings have for clinical practice? The forward bend task, a standard procedure in clinical examination of the spine, is a composite motion that requires coordination of the hips, lumbar spine and thoracic spine. The relative contribution of these joints in this movement task is often used to help make clinical judgments regarding potential physiologic mechanisms underlying the patients’ low back pain (e.g., shortened muscles) [29]. However, our data suggest that performance on this task is influenced by a combination of pain and fear, each with independent effects on spine and hip joint motions. Thus clinicians should consider the potential role of psychological mechanisms (e.g., fear of pain and harm) when interpreting patient performance on this task.
Acknowledgments
This work was supported by National Institutes of Health Grant grants RO1-HD045512.
Footnotes
The authors of the manuscript have no financial or other relationships that might lead to a conflict of interest, and the study was conducted in accordance with the current American Psychological Association guidelines for human research and was approved by the Ohio University Institutional Review Board.
References
- 1.Al-Obaidi SM, Nelson RM, Al-Awadhi S, Al-Shuwaie N. The role of anticipation and fear of pain in the persistence of avoidance behavior in patients with chronic low back pain. Spine. 2000;25(9):1126–1131. doi: 10.1097/00007632-200005010-00014. [DOI] [PubMed] [Google Scholar]
- 2.Al-Obaidi SM, Al-Zoabi B, Al-Shuwaie N, Al-Zaabie N, Nelson RM. The influence of pain and pain-related fear and disability beliefs on walking velocity in chronic low back pain. Int J Rehabil Res. 2003;26(2):101–108. doi: 10.1097/00004356-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Asmundson GJ, Norton PJ, Vlaeyen JW. Fear avoidance models of chronic pain: an overview. In: Asmundson GL, Vlaeyen JW, Crombez G, editors. Understanding and treating fear of pain. Oxford: Oxford University Press; 2004. pp. 3–24. [Google Scholar]
- 4.Buer N, Linton SJ. Fear-avoidance beliefs and catastrophizing: occurrence and risk factor in back pain and ADL in the general population. Pain. 2002;99(3):485–491. doi: 10.1016/S0304-3959(02)00265-8. [DOI] [PubMed] [Google Scholar]
- 5.Burns JW, Mullen JT, Higdon LJ, Wei JM, Lansky D. Validity of the pain anxiety ymptoms scale (PASS): prediction of physical capacity variables. Pain. 2000;84(2–3):247–252. doi: 10.1016/S0304-3959(99)00218-3. [DOI] [PubMed] [Google Scholar]
- 6.Crombez G, Vervaet L, Lysens R, Baeyens F, Eelen P. Avoidance and confrontation of painful, back-straining movements in chronic back pain patients. Behav Modif. 1998;22(1):62–77. doi: 10.1177/01454455980221004. [DOI] [PubMed] [Google Scholar]
- 7.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1–2):329–339. doi: 10.1016/S0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 8.Crombez G, Eccleston C, Vlaeyen JW, Vansteenwegen D, Lysens R, Eelen P. Exposure to physical movements in low back pain patients: restricted effects of generalization. Health Psychol. 2002;21(6):573–578. doi: 10.1037/0278-6133.21.6.573. [DOI] [PubMed] [Google Scholar]
- 9.Esola MA, McClure PW, Fitzgerald GK, Siegler S. Analysis of lumbar spine and hip motion during forward bending in subjects with and without a history of low back pain. Spine. 1996;21(1):71–78. doi: 10.1097/00007632-199601010-00017. [DOI] [PubMed] [Google Scholar]
- 10.Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain. 2001;94(1):7–15. doi: 10.1016/S0304-3959(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 11.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82(10):973–983. [PubMed] [Google Scholar]
- 12.Geisser ME, Roth RS, Theisen ME, Robinson ME, Riley JL., III Negative affect, self-report of depressive symptoms, and clinical depression: relation to the experience of chronic pain. Clin J Pain. 2000;16(2):110–120. doi: 10.1097/00002508-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 13.George SZ, Fritz JM, Erhard RE. A comparison of fear-avoidance beliefs in patients with lumbar spine pain and cervical spine pain. Spine. 2001;26(19):2139–2154. doi: 10.1097/00007632-200110010-00019. [DOI] [PubMed] [Google Scholar]
- 14.George SZ, Fritz JM, McNeil DW. Fear-avoidance beliefs as measured by the fear-avoidance beliefs questionnaire: change in fear-avoidance beliefs questionnaire is predictive of change in self-report of disability and pain intensity for patients with acute low back pain. Clin J Pain. 2006;22(2):197–203. doi: 10.1097/01.ajp.0000148627.92498.54. [DOI] [PubMed] [Google Scholar]
- 15.Grafton KV, Foster NE, Wright CC. Test-retest reliability of the short-form McGill pain questionnaire: assessment of intraclass correlation coefficients and limits of agreement in patients with osteoarthritis. Clin J Pain. 2005;21(1):73–82. doi: 10.1097/00002508-200501000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Klenerman L, Slade PD, Stanley IM, Pennie B, Reilly JP, Atchison LE, et al. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine. 1995;20(4):478–484. doi: 10.1097/00007632-199502001-00012. [DOI] [PubMed] [Google Scholar]
- 17.Kori KS, Miller RP, Todd DD. Kinesiophobia: a new view of chronic behavior. Pain Manage. 1990;Jan/Feb:35–43. [Google Scholar]
- 18.Lariviere C, Gagnon D, Loisel P. The effect of load on the coordination of the trunk for subjects with and without chronic low back pain during flexion-extension and lateral bending tasks. Clin Biomech. 2000;15(6):407–416. doi: 10.1016/S0268-0033(00)00006-1. [DOI] [PubMed] [Google Scholar]
- 19.McCracken LM, Zayfert C, Gross RT. The pain anxiety symptoms scale: development and validation of a scale to measure fear of pain. Pain. 1992;50(1):67–73. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- 20.McCracken LM, Gross RT, Aikens J, Carnrike CL., Jr The assessment of anxiety and fear in persons with chronic pain: a comparison of instruments. Behav Res Ther. 1996;34(11–12):927–933. doi: 10.1016/S0005-7967(96)00057-5. [DOI] [PubMed] [Google Scholar]
- 21.Melzack R. The McGill pain questionnaire: Major properties and scoring methods. Pain. 1975;1:277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 22.Melzack R, Katz J. The McGill pain questionnaire: appraisal and current status. In: Turk DC, Melzack R, editors. Handbook of pain assessment. New York: Guilford; 2001. [Google Scholar]
- 23.Parks KA, Crichton KS, Goldford RJ, McGill SM. A comparison of lumbar range of motion and functional ability scores in patients with low back pain: assessment for range of motion validity. Spine. 2003;28(4):380–384. doi: 10.1097/00007632-200302150-00014. [DOI] [PubMed] [Google Scholar]
- 24.Poitras S, Loisel P, Prince F, Lemaire J. Disability measurement in persons with back pain: a validity study of spinal range of motion and velocity. Arch Phys Med Rehabil. 2000;81(10):1394–1400. doi: 10.1053/apmr.2000.9165. [DOI] [PubMed] [Google Scholar]
- 25.Porter JL, Wilkinson A. Lumbar-hip flexion motion. A comparative study between asymptomatic and chronic low back pain in 18- to 36-year-old men. Spine. 1997;22(13):1508–1513. doi: 10.1097/00007632-199707010-00017. [DOI] [PubMed] [Google Scholar]
- 26.Roelofs J, McCracken L, Peters ML, Crombez G, Breukelen G, Vlaeyen JW. Psychometric evaluation of the pain anxiety symptoms scale (PASS) in chronic pain patients. J Behav Med. 2004;27(2):167–183. doi: 10.1023/B:JOBM.0000019850.51400.a6. [DOI] [PubMed] [Google Scholar]
- 27.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 29.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. Mosby: Saint Louis; 2002. [Google Scholar]
- 30.Sieben JM, Vlaeyen JW, Tuerlinckx S, Portegijs PJ. Pain-related fear in acute low back pain: the first two weeks of a new episode. Eur J Pain. 2002;6(3):229–237. doi: 10.1053/eujp.2002.0341. [DOI] [PubMed] [Google Scholar]
- 31.Simmonds MJ, Olson SL, Jones S, Hussein T, Lee CE, Novy D, et al. Psychometric characteristics and clinical usefulness of physical performance tests in patients with low back pain. Spine. 1998;23(22):2412–2421. doi: 10.1097/00007632-199811150-00011. [DOI] [PubMed] [Google Scholar]
- 32.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524–532. doi: 10.1037/1040-3590.7.4.524. [DOI] [Google Scholar]
- 34.Swinkels-Meewisse IE, Swinkels RA, Verbeek AL, Vlaeyen JW, Oostendorp RA. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8(1):29–36. doi: 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- 35.Swinkels-Meewisse IE, Roelofs J, Oostendorp RA, Verbeek AL, Vlaeyen JW. Acute low back pain: pain-related fear and pain catastrophizing influence physical performance and perceived disability. Pain. 2006;120(1–2):36–43. doi: 10.1016/j.pain.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Thomas E, Silman AJ, Papageorgiou AC, Macfarlane GJ, Croft PR. Association between measures of spinal mobility and low back pain. An analysis of new attenders in primary care. Spine. 1998;23(3):343–347. doi: 10.1097/00007632-199802010-00011. [DOI] [PubMed] [Google Scholar]
- 37.Thomas JS, France CR. Pain-related fear is associated with avoidance of spinal motion during recovery from low back pain. Spine. 2007;32(16):E460–E466. doi: 10.1097/BRS.0b013e3180bc1f7b. [DOI] [PubMed] [Google Scholar]
- 38.Vlaeyen JW, Kole-Snijders AM, Boeren RG, Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62(3):363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 39.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 40.Vlaeyen JW, Jong J, Geilen M, Heuts PH, Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18(4):251–261. doi: 10.1097/00002508-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear- avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 42.Wong TK, Lee RY. Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum Mov Sci. 2004;23(1):21–34. doi: 10.1016/j.humov.2004.03.004. [DOI] [PubMed] [Google Scholar]