Abstract
Although a variety of biomechanical laboratory investigations and radiological studies have highlighted the potential problems associated with total lumbar disc replacement (TDR), no previous study has performed a systematic clinical failure analysis. The aim of this study was to identify the post-operative pain sources, establish the incidence of post-operative pain patterns and investigate the effect on post-operative outcome with the help of fluoroscopically guided spine infiltrations in patients from an ongoing prospective study with ProDisc II. Patients who reported unsatisfactory results at any of the FU-examinations received fluoroscopically guided spine infiltrations as part of a semi-invasive diagnostic and conservative treatment program. Pain sources were identified in patients with reproducible (≥2×) significant (50–75%) or highly significant (75–100%) pain relief. Results were correlated with outcome parameters visual analogue scale (VAS), Oswestry disability index (ODI) and the subjective patient satisfaction rate. From a total of 175 operated patients with a mean follow-up (FU) of 29.3 months (range 12.2–74.9 months), n = 342 infiltrations were performed in n = 58 patients (33.1%) overall. Facet joint pain, predominantly at the index level (86.4%), was identified in n = 22 patients (12.6%). The sacroiliac joint was a similarly frequent cause of post-operative pain (n = 21, 12.0%). Pain from both structures influenced all outcome parameters negatively (P < 0.05). Patients with an early onset of pain (≤6 months) were 2–5× higher at risk of developing persisting complaints and unsatisfactory outcome at later FU-stages in comparison to the entire study cohort (P < 0.05). The level of TDR significantly influenced post-operative outcome. Best results were achieved for the TDRs above the lumbosacral junction at L4/5 (incidence of posterior joint pain 14.8%). Inferior outcome and a significantly higher incidence of posterior joint pain were observed for TDR at L5/S1 (21.6%) and bisegmental TDR at L4/5/S1 (33.3%), respectively. Lumbar facet and/or ISJ-pain are a frequent and currently underestimated source of post-operative pain and the most common reasons for unsatisfactory results following TDR. Further failure-analysis studies are required and adequate salvage treatment options need to be established with respect to the underlying pathology of post-operative pain. The question as to whether or not TDR will reduce the incidence of posterior joint pain, which has been previously attributed to lumbar fusion procedures, remains unanswered. Additional studies will have to investigate whether TDR compromises the index-segment in an attempt to avoid adjacent segment degeneration.
Keywords: Total lumbar disc replacement, Spine arthroplasty, Prospective studies, Spine infiltrations, Failure analysis
Introduction
Fusion of lumbar motion segments is often associated with a variety of negative side effects such as persisting post-operative pain from the facet and iliosacral joints (ISJ). These post-operative pain patterns have been linked to increased stress distribution and motion adjacent to the fused segments as well as to pathologically altered lumbar segmental, sagittal and spinopelvic alignment [1, 21, 29, 32, 35, 42, 43, 63]. The reported incidence of symptomatic “fusion-related” pain patterns from posterior joint structures ranges from 32 to 61%, and it’s clinical relevance has been confirmed in a variety of studies using fluoroscopically guided spine infiltrations [29, 42, 43].
In an attempt to avoid fusion related negative side effects, total lumbar disc replacement (TDR) has become increasingly popular for the treatment of low back pain (LBP). Hypothetically, lumbar disc arthroplasty should serve to avoid stress to the adjacent segments by maintaining motion. Furthermore, it has been shown that physiological sagittal alignment is maintained following TDR [5, 6, 10, 33, 61].
However, an increasing number of radiological studies, biomechanical in vitro- and finite-element models (FEM) have recently focussed on the influence of TDR on the lumbar facet joints [16, 17, 22, 24, 27, 41, 47, 51, 55, 62]. The authors reported problems associated with biomechanical alterations such as segmental hyperlordosis, increased segmental instability, increased load on facet joints with abnormal stress distribution patterns as well as subluxation of the facet joints.
To date, no previous clinical study has evaluated the actual incidence of facet joint problems following TDR. Furthermore, despite repeated focus on the lumbar facet joints, no previous study has yet evaluated whether the iliosacral joint is a potential cause of the post-operative pain following TDR.
In this study, an analysis of post-operative pain patterns following TDR with ProDisc II (Synthes, Paoli, USA) was performed in a clinical setting using fluoroscopically guided spine infiltrations to evaluate the source and incidence of complaints arising from posterior joint structures and their influence on clinical outcome.
Materials and methods
Study protocol
From 07/2000 to 11/2006, TDR with ProDisc II was performed mono-, bi- and multi-segmentally in 240 patients. The study design was a prospective, non-randomized study. The minimum FU required for inclusion in this study was 12 months.
This study evaluated the results obtained from fluoroscopically guided spine infiltrations in patients who had been operated on during a 60 month period between July 2000 and July 2005 and complained of post-operative pain. Data from this analysis were then correlated with the post-operative outcome parameters obtained from the ongoing prospective study.
Pre-operative diagnosis and patient selection
Pre-operative diagnosis was made on the basis of lumbar X-rays in ap- and lateral-view, functional flexion/extension images and pre-operative MRI-imaging.
Low back pain (LBP) was the predominant and leading complaint in all patients. In cases of accompanying sciatica, the amount of LBP exceeded 80% of overall complaints. All patients were non-responders to an intensive inpatient and outpatient conservative treatment program (≥6 months).
Pre-operative diagnosis included lumbar degenerative disc disease (DDD) with (n = 63) and without Modic-changes (n = 50), DDD with accompanying central/mediolateral contained soft-disc-herniation (n = 16) with predominant low back pain and patients with DDD following previous discectomy at the index-level (n = 37). In n = 6 patients, TDR was combined with a lumbar fusion procedure. Another n = 3 patients underwent TDR due to adjacent segment degeneration following a previous 360°-instrumented fusion.
Due to the high rate of patients who failed to distinguish between concordant and non-concordant pain [7], a high rate of false positive and negative results equally [8], 100% “memory pain” in patients with abnormal psychometric testing [7] as well as a 0.5% infection rate [3, 7]
discography was not employed as a diagnostic tool for the diagnosis of symptomatic lumbar degenerative disc disease in this study.
Female patients above the age of 45 and male patients exceeding the age of 55 years received DXA (dual-X-ray)-bone-density-measurements. In accordance with the WHO-definition of osteopenia, patients with a T-score of ≤−1.5 were excluded from this study.
The disc spaces were approached through a mini-open laparotomy as described previously [45, 46] and insertion of the implant was performed according to the manufacturers guidelines [2].
Pre- and post-operative fluoroscopically guided spine infiltrations
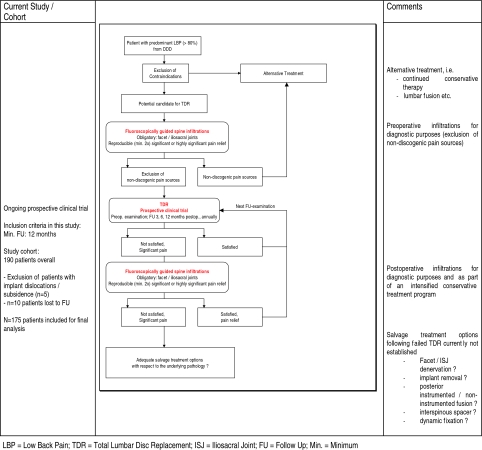
An overview delineating the timing and indication for all pre- and post-operative infiltrations is provided in Table 1.
Table 1.
Flow chart delineating patient selection for TDR, study cohort and timing of infiltrations
Pre-operative
Pre-operatively, all patients underwent fluoroscopically guided spine infiltrations to rule out any non-discogenic pain sources. As with previously published studies, the clinical examination was considered a useful aid in determining a potential source of pain but was not relied upon for diagnostic purposes [18, 31].
Obligatory injections that were performed in all patients included infiltrations of the facet joints at the affected level, the adjacent levels as well as the iliosacral joints bilaterally.
Patients with a significant (50 to ≤75%) or highly significant (>75%) and reproducible (≥2×) pain relief upon infiltration of the facet and/or iliosacral joints which revealed a non-discogenic pain source as the predominant complaint were excluded from artificial disc replacement. Patients with negligible (<25%) or only mild (25 to <50%) pain relief were considered potential candidates for TDR in the absence of other contraindications.
Post-operative
Patients who reported significant complaints and unsatisfactory results at any one of the FU examinations received fluoroscopically guided spine infiltrations. The injections were part of an intensified conservative post-operative treatment program and were also used for diagnostic purposes to confirm the source of post-operative pain.
For each set of infiltrations, a patient received a minimum of four injections, which similarly included the facet joints at the index level, the adjacent level, as well as the iliosacral joints. Infiltrations were first performed at the structure, which by clinical observation appeared most likely to be the potential source of pain. In case of “non-responders” with negligible or only mild pain relief (<50%) subsequent infiltrations were performed to investigate other possible pain sources.
Injection technique
All injections were performed in a standardized fashion by trained and experienced members of the clinic’s spine unit. Patients were in a prone position on the fluoroscopy table and the skin was prepared in a sterile manner. Any structure to be infiltrated was identified under fluoroscopic imaging. Surface landmarks were marked on the patient’s skin. A 22-/25-gauge needle was directed from the surface landmark to the target structure under fluoroscopic guidance.
Infiltrations were performed using a combination of local anesthetic and low-dose corticoid (Scandicain® 1%; Triamcinolon® 40 mg) in a 5:1 ml ratio. The applied volume was approx. 1–1.5 ml for a facet joint infiltration and 2–3 ml for an infiltration of the iliosacral joint. All infiltrations were performed as direct joint infiltrations as described previously [18, 19, 29, 31, 42, 43].
Study documentation
Results from fluoroscopically guided spine infiltrations
Data was recorded and classified according to the origin of pain, intensity of pain relief and the level at which disc replacement was performed. The patients categorized the effect of each infiltration and pain relief into four groups, namely “highly significant” (defined as >75% pain relief), “significant” (50 to ≤75% pain relief), “minor/mild” (25 to <50% pain relief) or “insignificant” (pain relief <25%) according to the subjective relief of their complaint, which was achieved within the first few hours following the injection.
An injection was recorded as “positive” for an infiltrated structure if the subjective degree of pain relief was considered “significant” or “highly significant”. A second infiltration of the same structure with significant reproducible pain relief was required in all patients to rule out any false positive findings as previously published for single injections [18].
For patients who received several sets of infiltrations at different time intervals, an infiltrated structure was recorded only once for final analysis if the following set of infiltrations confirmed the same structure as a source of pain; it was recorded twice if the second set of infiltrations revealed pain from a different origin.
Patients with implant-related complications (e.g. dislocation or subsidence) following TDR were not included in the final analysis. Thus, results from this study refer to patients with a correct implant positioning.
Clinical results
Study documentation was standardized and included visual analogue scale (VAS), the Oswestry disability index (ODI) [20] as well as numerous clinical and radiological parameters. All clinical and radiological data were recorded prospectively. Patients were examined pre-operatively, followed by routine FU examinations 3, 6 and 12 months post-operatively, annually from then. The success of the operation was determined according to the subjective satisfaction rate and categorized into three groups, namely “highly satisfied”, “satisfied” and “not satisfied”.
Statistical analysis
All data were acquired using Microsoft Excel 2002 (Microsoft Inc., Redmond, WA). Statistical analysis of quantitative data was performed using the paired Student’s t-test. Non-parametric data were evaluated by the Chi-square test. Statistical significance was defined and accepted as P < 0.05.
Results
Study group and sample size
Results from 190 patients were included in this study. In n = 5 patients (2.6%), dislocation or subsidence of the prosthesis which required revision surgery was observed in the early post-operative period. Although two of those patients received fluoroscopically guided spine infiltrations, results from these patients were not included according to the study criteria. Ten patients were lost to FU (5.3%), leaving a final FU rate of 94.6%.
Thus, results from 175 patients were included in this study for final analysis as outlined in Tables 1 and 2.
Table 2.
Overall results
| Cohort of patients who did not require fluoroscopically guided spine infiltrations | Cohort of all patients with fluoroscopically guided spine infiltrations following TDR | Cohort of patients with confirmed facet joint pain (at all levels) | Cohort of patients with confirmed facet joint pain at the level L5/S1 | Cohort of patients with confirmed iliosacral joint pain | Entire study cohort (all patients) | |
|---|---|---|---|---|---|---|
| Number of patients | n = 117 | n = 58 | n = 22 | n = 17 | n = 21 | n = 175 |
| Sex | ||||||
| Male (%) | 38.5 | 37.9 | 27.3 | 23.5 | 28.6 | 38.3 |
| Female (%) | 61.5 | 62.1 | 72.7 | 76.5 | 71.4 | 61.7 |
| Agemean (years) | 43.5 | 44.2 | 43.3 | 42.8 | 44.8 | 43.7 |
| Range | (21.9–70.9) | (28.9–65.8) | (28.9–63.7) | (28.9–63.7) | (29.4–60.4) | (21.9–70.9) |
| FUmean (months) | 30.5 | 26.8 | 26.9 | 30.6 | 28.1 | 29.3 |
| Range | (12.2–67.3) | (12.2–74.9) | (12.6–60.3) | (16.4–60.3) | (13.8–58.4) | (12.2–74.9) |
| Patient satisfaction rate | ||||||
| Completely satisfied | 70.2% | 28.6 | 19.0% | 17.6% | 36.8% | 56.1% |
| Satisfied | 22.8% | 32.1 | 19.0% | 23.5% | 31.6% | 25.7% |
| Not satisfied | 7.0% | 39.3 | 61.9% | 58.8% | 31.6% | 18.1% |
| Good + excellent | 93.9% | 60.7% | 38.0% | 41.2% | 68.4% | 81.8% |
| Economic Changes | ||||||
| Former job, full time | 55.6% | 33.9% | 40.0% | 46.7% | 47.6% | 48.0% |
| Former job, part time | 6.8% | 14.3% | 10.0% | 6.7% | 4.8% | 9.1% |
| New job | 11.1% | 8.9% | 5.0% | 0% | 4.8% | 10.3% |
| Back to work | 73.5% | 57.1% | 55.0% | 53.3% | 57.1% | 67.4% |
| TDR including lumbosacral junction | n = 88 (75.2%) | n = 51 (87.9%) | n = 18 (81.8%) | n = 16 (94.1%) | n = 20 (95.2%) | n = 139 (79.4%) |
| Level of TDR | ||||||
| Monosegmental | n = 101 (86.3%) | n = 46 (79.3%) | n = 19 (86.4%) | n = 15 (88.2%) | n = 16 (76.2%) | n = 147 (84%) |
| L2/3 | 2 | 0 | 2 | |||
| L3/4 | 0 | 1 | 1 | |||
| L4/5 | 3 | 4 | 3 | 1 | 1 | 27 |
| L5/6 | 3 | 1 | 1 | 4 | ||
| L4/S1 | 1 | 1 | 1 | 2 | ||
| L5/S1 | 72 | 39 | 15 | 14 | 14 | 111 |
| Bisegmental | n = 16 (13.9%) | n = 11 (19.0%) | n = 3 (13.6%) | n = 2 (12.5%) | n = 5 (23.8%) | n = 27 (15.4%) |
| L3/4/5 | 1 | 1 | 0 | 0 | 2 | |
| L5/6/S1 | 0 | 1 | 0 | 1 | 1 | |
| L4/5/S1 | 15 | 9 | 3 | 2 | 4 | 24 |
| 3-segmental | n = 0 (0%) | n = 1 (1.7%) | n = 0 (0%) | n = 1 (0.6%) | ||
| L3/4/5/S1 | 1 | 1 | ||||
TDR Total lumbar disc replacement, FU follow-up
Due to significant post-operative pain, n = 58 patients (33.1%) required fluoroscopically guided spine infiltrations at some stage throughout their post-operative course as part of a semi-inasive diagnostic and conservative treatment program.
Overall, 342 infiltrations were performed (5.9 infiltrations/patient) with bilateral infiltrations of a structure (eg. bilateral facet or iliosacral joint infiltration) being counted as one infiltration. An overview of all infiltrations is outlined in Table 3.
Table 3.
Results from 342 fluoroscopically guided spine infiltrations with significant pain relief ≥50% following total lumbar disc replacement in n = 175 patients
| Fluoroscopically guided spine infiltrations (structure) | Number of infiltrations performed (total) | Class 1 pain relief (50–75%) | Class 2 pain relief (75–100%) | Incidence of posterior pain-[combined data (% of all patients)] |
|---|---|---|---|---|
| Facet joints L3/4 | n = 13 | n = 1 | n = 1 (0.6%) | |
| Facet joints L4/5 | n = 51 | n = 3 | n = 3 (1.7%) | |
| Facet joints L5/6 | n = 2 | n = 1 | n = 1 (0.6%) | |
| Facet joints L5/S1 | n = 90 | n = 12 | n = 5 | n = 17 (9.7%) |
| Facet joints L6/S1 | n = 1 | |||
| ISJ | n = 105 | n = 15 | n = 6 | n = 21 (12.0%) |
| ILL | n = 15 | n = 0 | n = 0 | n = 0 (0%) |
| Interspinous inf. L3/4 | n = 9 | n = 1 | n = 1 (0.6%) | |
| Interspinous inf. L4/5 | n = 16 | n = 2 | n = 1 | n = 3 (1.7%) |
| Interspinous inf. L5/S1 | n = 10 | |||
| Epidural infiltration L3/4 | n = 3 | |||
| Epidural infiltration L4/5 | n = 10 | n = 1 | n = 1 (0.6%) | |
| Epidural infiltration L5/S1 | n = 3 | |||
| Selective nerve root infiltration L4 | n = 2 | |||
| Selective nerve root infiltration L5 | n = 9 | n = 1 | n = 1 | n = 2 (1.1%) |
| Selective nerve root infiltration S1 | n = 2 | |||
| Caudal epidural infiltration | n = 1 | |||
| Total (facet joint pain) | n = 18 | n = 4 | n = 22 (12.6%) | |
| Total (ISJ pain) | n = 15 | n = 3 | n = 21 (12.0%) | |
| Total (facet + ISJ pain) | n = 33 | n = 7 | n = 43 (24.5%) | |
| Total posterior joint pain (combined data all infiltrations) | n = 38 | n = 8 | n = 41a (23.4%) |
ISJ Iliosacral joint, ILL iliolumbar ligaments
aPatients with multiple-diagnosed pain structures (e.g. facet and ISJ pain) only counted once
Specific pain analysis
In n = 17 out of 58 patients (29.3%), the results of the infiltrations were not of diagnostic value due to non-reproducible or insignificant pain relief (<50%). Thus, a positive test result was observed in n = 41 patients, which represents an overall incidence of post-operative posterior joint pain of 23.4%.
Lumbar facet joints
In n = 22 patients, the lumbar facet joints were diagnosed as a symptomatic source of pain (12.6% overall), predominantly located at the index level (n = 19/22; 86.4%).
The majority of all facet joint problems (n = 17/22; 77.3%) occurred at the level L5/S1.
An analysis of results from all monosegmental TDRs revealed an incidence of facet joint problems of 13.3% (n = 15/113 patients) for all TDRs performed at the lumbosacral junction and 11.8% for TDRs performed above the lumbosacral junction (n = 4/34 patients; P > 0.05).
Iliosacral joints/iliolumbar ligaments
In n = 21/175 patients (12%), the iliosacral joint was diagnosed as a significant cause of post-operative pain.
Analysis of this subgroup shows that 20/21 disc replacement procedures (95.2%) included the lumbosacral junction. Pain from the iliolumbar ligaments was never confirmed as a significant cause of post-operative pain.
Interspinous pain (“kissing spine”)
A post-operative Baastrup-phenomena (“kissing spine”) was diagnosed with conventional X-rays and shown to be a clinically relevant source of pain with significant pain relief achieved through the use of interspinous infiltrations in n = 3 patients (1.7%).
Various
Post-operative L5-radiculopathy was diagnosed in n = 2 patients following TDR at L5/S1.
Another patient showed signs of spinal claudication following bisegmental TDR at L4/5/S1. Further diagnostics and epidural infiltrations confirmed a clinically relevant narrowing of the spinal canal at the level L4/5. The patient underwent decompressive surgery with a highly satisfactory outcome thereafter.
Clinical impact of post-operative pain patterns
Subjective patient satisfaction
According to the subjective satisfaction rate of patients that reported a “satisfied” or “highly satisfied” outcome, the success rate was 81.8% at the last FU overall.
This rate dropped to 68.4% for patients with iliosacral joint pain (P < 0.05) and 38.0% for patients with facet joint pain. No statistically significant differences in the subjective outcome evaluation between patients with ISJ pain and diagnosed pain from the facet joints were detected (P > 0.05).
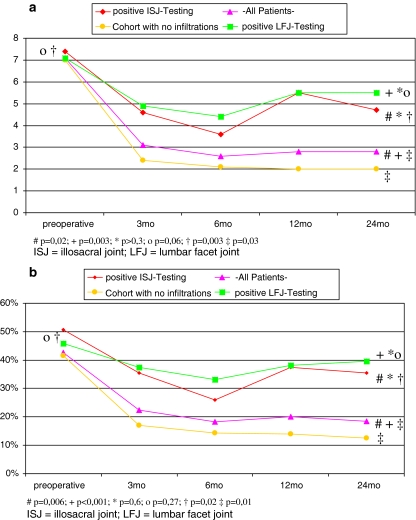
VAS, ODI
Both the parameters VAS and ODI deteriorated significantly in patients with confirmed facet and/or ISJ pain in comparison to the entire study cohort and the group of patients who did not require any infiltrations (P < 0.02; Fig. 1a, b).
Fig. 1.
Pre-/post-operative results from fluoroscopically guided spine (a + b) infiltrations for (a) visual analogue scale (VAS) and (b) Oswestry disability index (ODI)
Differences between patients with facet joint pain and those with ISJ pain were not statistically significant (P > 0.3). However, all outcome parameters were inferior for patients with facet joint complaints. Furthermore, whilst post-operative improvement was still statistically significant for patients with ISJ pain (P < 0.02), there was either no or only a tendency for improvement in patients with confirmed facet joint pain for VAS and ODI (P = 0.06; P = 0.27).
Correlation between diagnosis of early facet/ISJ pain and final outcome
A considerable proportion of all infiltrations were performed in the early post-operative period within the first 3 months (n = 27, 34.6%), 21 of those in the immediate post-operative phase within the first 6 weeks (n = 21; 26.9%). Another seven patients (9.0%) received infiltrations between 3 and 6 months post-operatively.
The earliest positive test result was considered relevant in patients with multiple infiltrations at different time intervals.
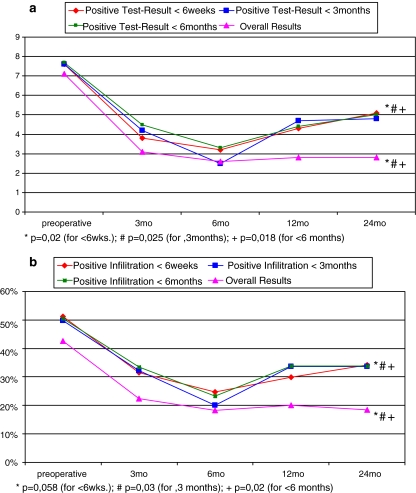
In n = 18 out of 34 patients, clinically relevant pain from the facet and/or iliosacral joints was diagnosed within the first 6 months following TDR. Despite improvement at the 6 month-FU, the results deteriorated throughout the subsequent post-operative course (Fig. 2a, b). At the 24-month FU, the results were significantly inferior in comparison to the entire study cohort for both VAS and ODI (P = 0.02).
Fig. 2.
Correlation between early onset and diagnosis of symptomatic (a + b) facet and/or ISJ pain (<6 months; <3 months; <6 weeks) and mid-term clinical outcome for (a) visual analogue scale (VAS) and (b) Oswestry disability index (ODI)
Whilst the overall rate of patients with an unsatisfactory post-operative outcome at the last FU-examination was 18.1% in the entire study cohort of 175 patients and only 7% in the cohort of patients who did not receive any infiltrations, this rate increased approx. 2 to 5-fold to 37.5% patients with an early onset and diagnosis of facet and/or ISJ pain (P < 0.05).
A similar scenario was observed in those patients with an even earlier onset and diagnosis of posterior joint pain in the immediate post-operative period (≤6 weeks) with a 40.0% rate of unsatisfied patients at the last FU.
Level of disc replacement
The incidence of post-operative pain from posterior joint structures was diagnosed in n = 30 out of all 147 monosegmental disc replacement procedures (20.4%). This number increased to n = 10 out of 27 bisegmental TDR’s (37.0%), respectively.
The most frequently operated levels included the levels L4/5, L5/S1 and bisegmental TDR at L4/5/S1 (Table 2). Whilst the incidence of posterior joint pain was 14.8% following monosegmental TDR at L4/5, it increased to 21.6% following TDR at L5/S1 and 33.3% after bisegmental TDR at L4/5/S1, respectively.
Eighty-eight percent of patients were “satisfied” or “highly satisfied” following TDR at L4/5. This number decreased to 82.6 and 79.1% for TDR at L5/S1 and L4/5/S1, respectively.
The same negative trend was observed for post-operative VAS- and ODI-scores with best results being achieved following monosegmental TDR at L4/5.
Reoperations
The overall rate of complications and re-operations from this ongoing prospective study have been published previously [46, 57, 58]. Secondary surgery which was indicated as a direct result from fluoroscopically guided spine infiltrations in this study was performed in 9/175 patients overall (5.1%).
A microsurgical decompression was indicated in two patients due to spinal canal stenosis with signs of spinal claudication in the one and post-operative L5-radiculopathy in the other.
Treatment of patients with persisting facet joint complaints included 4× posterior instrumented fusion, 2× implantation of an interspinous spacer (X-Stop®, InSpace®) and 1× dynamic neutralization using Dynesys® (Zimmer Spine, Warsaw, IN) due to post-operative secondary hyperlordosis.
Influence of Gender
The male:female ratio was 1:1.6 in the entire study cohort of 175 patients (67 m, 108f; Table 2). This ratio increased in patients with symptomatic ISJ pain to 1:2.5 (6 m, 15f). For patients with confirmed facet-joint-complaints at the lumbosacral junction, it was 1:3.3 (4 m, 13f).
Due to the low number of patients in our sub-cohorts, statistical testing did not reveal any significant differences between the groups (P = 0.18).
Discussion
Fusion procedures have been linked to a variety of negative side effects such as adjacent segment degeneration and instability, superior segment facet joint violation, adjacent segment spondylarthrosis with consecutive spinal canal stenosis as well as persisting pain from harvesting of the autologous bone graft [9, 21, 23, 30, 35, 49, 63]. Previous studies have revealed the facet and iliosacral joints to be a source of post-operative pain in a considerable number of patients [29, 42, 43]. Alterations of the segmental, sagittal and spinopelvic alignment as well as increased motion and stress adjacent to fused levels have been held responsible for post-fusion pain patterns [1, 21, 29, 32, 42, 43, 63].
In an attempt to avoid fusion-related negative side effects, lumbar disc replacement procedures have become increasingly popular and various clinical trials have shown satisfactory results following TDR [4, 11, 15, 26, 34, 38, 46, 48, 57, 58, 66−68]. One of the primary aims of TDR is to preserve motion and thereby ultimately avoid stress and degeneration of the adjacent segment. Radiographic studies have demonstrated maintained physiological sagittal and spinopelvic alignment following TDR [5, 10, 33, 61]. It has therefore been hypothesized that the above-mentioned fusion-related negative side effects and post-fusion pain patterns could be avoided with TDR. To date, however, this hypothesis has not been confirmed with substantial evidence based data.
In a study with CT osteoabsorptiometry, Trouillier et al. [62] reported morphological findings following TDR with SB Charité (Depuy Spine, Raynham, MA, USA). The authors suggested that there was not only an absence of facet joint degeneration but also possibly a reversal of an already existing facet osteoarthritis which was referred to as “improved segmental kinematics and restored intervertebral disc space height with consecutive unloading of the facet joints”. Conversely, however, Shim et al. [56] in a recent retrospective comparative study between ProDisc and Charité reported a high progression rate of facet joint osteoarthritis for both types of prosthesis in 32–36.4% of all patients. According to the authors, this high incidence of facet degeneration after an average FU of only 38–41 months seemed to be too short to be explained by the natural course of degeneration.
Other study group’s findings have similarly tempered the initial enthusiasm [51, 52, 64]. An increasing number of radiographic and biomechanical studies are suggesting that TDR interferes with the highly sensitive biomechanics of the spine. The authors have predominantly focused on problems associated with the lumbar facet joints.
Biomechanical studies
A variety of studies have carefully analyzed the biomechanical properties and motion characteristics of different artificial disc-design prosthesis [12, 13, 16, 17, 22, 24, 25, 36, 47, 50, 53, 54]. Reported problems associated with TDR include excessive ligament torsions, increased facet pressures, a high risk of instability at the index and adjacent level, up to 2.5× increased load on posterior structures and altered load patterns with sudden rather than gradual load increase in the facet joints [17, 39]. Furthermore, it has been shown that TDR with Charité III did not restore the physiological segmental rotational stability with additive destabilising effects for multilevel versus mono-segmental TDRs [13,47].
Radiological studies
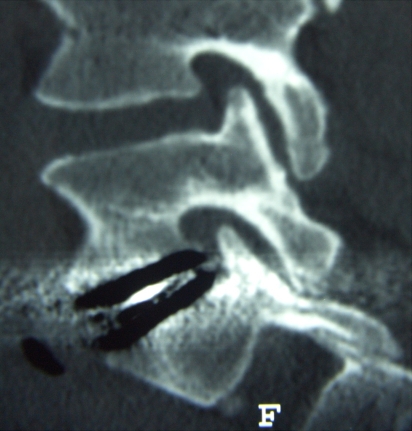
Similarly, Sariali et al. [55] revealed normal values for axial rotation when TDR was performed monosegmentally at L4/5, whereas abnormally increased mobility was found in 50% of cases following bisegmental TDR at L4/5/S1 in comparison to results reported for healthy volunteers. Despite motion preservation in the majority of cases, a variety of recently published studies have reported low flexion/extension ROM-values in a considerable number of cases with unknown consequences [28, 37, 59]. Furthermore, implant positioning and disc-/implant-height have been shown to influence and increase post-operative segmental lordosis which may ultimately lead to a subluxation of the facet joints (Fig. 3) [5, 41, 53].
Fig. 3.
Post-operative subluxation of the facet joints
Clinical studies
Previous studies have mentioned isolated incidences of facet and/or iliosacral joint pain following TDR [14, 34, 38, 69]. In comparison to lumbar fusion procedures, however, no clinical study has systematically evaluated the impact of these biomechanical alterations on posterior joint structures and post-operative outcome.
The increasing number of disc replacement procedures being performed worldwide [60] therefore highlights the crucial importance of further failure-analysis studies and salvage treatment options following failed TDR.
Diagnostic challenges
To date, no pathognomonic non-invasive radiographic findings are available that would allow one to definitively identify possible pain sources. Imaging techiques such as MRI, CT or radionuclide bone scanning are unreliable in predicting symptomatic pain from posterior joint structures and physical examination has similarly been shown to be unreliable for diagnostic purposes [18].
There is no or only conflicting evidence suggesting that fluoroscopically guided spine infiltrations can achieve any mid- or long-term improvement for the treatment of LBP [19, 44, 65]. Similarly, our results showed only a short term-improvement, whilst longer FU revealed recurrent symptoms and deteriorating results (Fig. 2a, b).
However, their role for diagnostic purposes remains undisputable. A reproducible, near total pain relief after controlled injections into the facet/ISJ joints or their nerve supply is a widely accepted standard reference technique for diagnosis of symptomatic lumbar zygoapophyseal- or sacroiliac-joint pain, with both techniques believed to produce equivalent diagnostic results [18, 19, 29, 31, 40, 42–44].
The clinical findings observed in this study closely correspond with the above-cited biomechanical and radiological investigations reported by a variety of independent study groups. We observed satisfactory results following TDR in 81.8% of all patients at an average FU of 29.3 months in a highly selected patient population. However, 33.1% (n = 58) of all patients required intensified post-operative pain management, which included fluoroscopically guided spine infiltrations throughout their post-operative course. A potential for recovery was seen in approximately half of these patients, whereas 18.1% reported persisting complaints at the last FU-examination.
We were able to identify the facet and/or iliosacral joints as the source of post-operative pain in a substantial number of patients (n = 41; 23.4%). Pain from both structures led to a significant deterioration of all outcome parameters (P < 0.05). When comparing patients with facet joint pain to those with sacroiliac joint pain we found that all post-operative outcome parameters were inferior for patients with facet joint pain. However, statistical analysis did not reveal any significant difference between both groups (P > 0.05).
It was further established that patients with an early onset of symptomatic facet and/or iliosacral joint pain (≤6 months) in particular were at a high risk of developing persisting complaints and unsatisfactory results at later FU-stages (P = 0.02).
This study indicates that the index-level is predominantly at risk following TDR. In the majority of patients with post-operative facet joint pain (n = 19/22, 86.4%) and in all patients with interspinous pain (“kissing spine”) the source of pain was located at the index level. However, patients with TDR performed at the lumbosacral junction stand an additional risk of inferior post-operative outcome due to a high incidence of sacroiliac joint problems.
This supports our findings that the level of disc replacement plays a significant role in post-operative outcome following TDR and demonstrates that the lumbosacral motion segment remains a weak and volatile link of the lumbar spine despite adaptation of motion preserving technology. Whilst best results and the lowest incidence of posterior joint pain (14.8%) was observed following TDR at L4/5, outcome parameters deteriorated and the incidence of posterior joint pain increased to 21.6 and 33.3% for TDR at L5/S1 and bisegmental TDR at L4/5/S1, respectively.
Potential problems associated with the sacroiliac joints have, to date, not been adressed adequately. In a radiographic study with 35 patients, LeHuec et al. [33] concluded that the Maverick prosthesis had enough freedom of motion to maintain the natural sagittal and spinopelvic balance needed to prevent potential undue stress on the muscles and the sacroiliac joints. However, this is the first study to demonstrate that the lumbar facet and sacroiliac joints are a similarly frequent cause of post-operative pain. The reasons for sacroiliac joint pain following TDR remain unknown. A variety of recently published studies have reported low ROM-values [28, 37, 59]. The pathomechanism of post-operative ISJ pain in these patients may therefore be similar to that of lumbosacral fusion procedures [29, 42, 43]. Other potential reasons could include abnormal motion patterns of the artificial implants as also described previously [50, 54].
Future investigations should therefore include radiological studies with special emphasis on the quality and range of motion. Results obtained from such studies could be the crucial answer in the search for appropriate salvage procedures, which have become essential in light of the rapidly increasing market volume of lumbar disc replacement procedures [60]. Whilst patients with confirmed pain from the facet joints may benefit from minimally invasive techniques such as implantation of an interspinous spacer or posterior fusion, the adequate treatment for patients with persisting complaints from the sacroiliac joints remains yet to be established. Fusion of the lumbosacral junction, similarly associated with sacroiliac joint pain [29, 42, 43] may not be beneficial for these patients and could potentially aggravate symptoms.
Symptomatic complaints from the ISJs following TDR may therefore be a much more challenging entity to treat in comparison to post-operative facet joint pain. However, the small number of patients with re-operations in this study did not allow for any further investigation into the effectiveness of different types of re-operations with regards to the underlying pathology.
Future prospective randomized studies will have to demonstrate if TDR can actually reduce the incidence of post-operative posterior joint pain in comparison to lumbar fusion procedures. Moreover, upcoming morphological studies should evaluate whether the index-segment is compromised in an attempt to avoid adjacent segment degeneration.
Conclusion
Complaints originating from the facet or iliosacral joints were observed in a considerable number of patients following total lumbar disc replacement, which negatively influenced post-operative outcome. The sacroiliac joints and the lumbar facet joints were a similarly frequent cause of post-operative pain and the most common reason for an unsatisfactory result. Patients with an early onset of symptomatic pain (≤6 months) in particular stand an increased risk of persisting complaints and unsatisfactory results at later FU-stages.
The level of TDR plays a significant role on post-operative outcome and the incidence of pain from posterior joint structures. Whilst the index-level is at risk at all levels, patients with TDR including the lumbosacral junction stand an additional increased risk of developing post-operative sacroiliac joint problems.
The incidence of posterior joint pain following TDR and the impact on post-operative outcome is currently underestimated. Due to a globally increasing number of TDRs, adequate salvage treatment options for patients with failed-disc-replacement procedures need to be established.
Whether lumbar disc replacement procedures will be able to reduce the incidence of posterior joint pain previously attributed to fusion procedures is presently unknown and will require longer FU and further investigation in prospective randomized controlled trials.
Future morphological studies will have to evaluate if the index-segment is compromised in an attempt to avoid adjacent segment degeneration.
Contributor Information
Christoph J. Siepe, Phone: +49-89-62110, FAX: +49-89-62112012, Email: CSiepe@Schoen-Kliniken.de
H. Michael Mayer, Email: MMayer@Schoen-Kliniken.de.
References
- 1.Akamaru T, Kawahara N, Tim Yoon S, Minamide A, Su Kim K, Tomita K, Hutton WC. Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments: a biomechanical analysis. Spine. 2003;28:1560–1566. doi: 10.1097/00007632-200307150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Bertagnoli R, Marnay T, Mayer HM (2003) The Prodisc book. Spine solutions GmbH, Tuttlingen
- 3.Block AR, Vanharanta H, Ohnmeiss DD, Guyer RD. Discographic pain report. Influence of psychological factors. Spine. 1996;21:334–338. doi: 10.1097/00007632-199602010-00017. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, Garcia R, Jr, Regan JJ, Ohnmeiss DD. A prospective, randomized, multicenter food and drug administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine. 2005;30:1565–1575. doi: 10.1097/01.brs.0000170587.32676.0e. [DOI] [PubMed] [Google Scholar]
- 5.Cakir B, Richter M, Kafer W, Puhl W, Schmidt R. The impact of total lumbar disc replacement on segmental and total lumbar lordosis. Clin Biomech (Bristol, Avon) 2005;20:357–364. doi: 10.1016/j.clinbiomech.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 6.Cakir B, Schmidt R, Huch K, Puhl W, Richter M. [Sagittal alignment and segmental range of motion after total disc replacement of the lumbar spine] Z Orthop Ihre Grenzgeb. 2004;142:159–165. doi: 10.1055/s-2004-816275. [DOI] [PubMed] [Google Scholar]
- 7.Carragee EJ, Chen Y, Tanner CM, Hayward C, Rossi M, Hagle C. Can discography cause long-term back symptoms in previously asymptomatic subjects? Spine. 2000;25:1803–1808. doi: 10.1097/00007632-200007150-00011. [DOI] [PubMed] [Google Scholar]
- 8.Carragee EJ, Tanner CM, Yang B, Brito JL, Truong T. False-positive findings on lumbar discography. Reliability of subjective concordance assessment during provocative disc injection. Spine. 1999;24:2542–2547. doi: 10.1097/00007632-199912010-00017. [DOI] [PubMed] [Google Scholar]
- 9.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Chung SS, Lee CS, Kang CS, Kim SH. The effect of lumbar total disc replacement on the spinopelvic alignment and range of motion of the lumbar spine. J Spinal Disord Tech. 2006;19:307–311. doi: 10.1097/01.bsd.0000208255.14329.1e. [DOI] [PubMed] [Google Scholar]
- 11.Cinotti G, David T, Postacchini F. Results of disc prosthesis after a minimum follow-up period of 2 years. Spine. 1996;21:995–1000. doi: 10.1097/00007632-199604150-00015. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham BW. Basic scientific considerations in total disc arthroplasty. Spine J. 2004;4:219S–230S. doi: 10.1016/j.spinee.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham BW, Gordon JD, Dmitriev AE, Hu N, McAfee PC. Biomechanical evaluation of total disc replacement arthroplasty: an in vitro human cadaveric model. Spine. 2003;28:S110–S117. doi: 10.1097/01.BRS.0000092209.27573.90. [DOI] [PubMed] [Google Scholar]
- 14.David T. Lumbar disc prosthesis: surgical technique, indications and clinical results in 22 patients with a minimum of 12 months follow-up. Eur Spine J. 1993;1:254–259. doi: 10.1007/BF00298370. [DOI] [PubMed] [Google Scholar]
- 15.Delamarter RB, Fribourg DM, Kanim LE, Bae H. ProDisc artificial total lumbar disc replacement: introduction and early results from the United States clinical trial. Spine. 2003;28:S167–175. doi: 10.1097/01.BRS.0000092220.66650.2B. [DOI] [PubMed] [Google Scholar]
- 16.Denoziere G, Ku DN. Biomechanical comparison between fusion of two vertebrae and implantation of an artificial intervertebral disc. J Biomech. 2006;39:766–775. doi: 10.1016/j.jbiomech.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 17.Dooris AP, Goel VK, Grosland NM, Gilbertson LG, Wilder DG. Load-sharing between anterior and posterior elements in a lumbar motion segment implanted with an artificial disc. Spine. 2001;26:E122–E129. doi: 10.1097/00007632-200103150-00004. [DOI] [PubMed] [Google Scholar]
- 18.Dreyfuss PH, Dreyer SJ. Lumbar zygapophysial (facet) joint injections. Spine J. 2003;3:50S–59S. doi: 10.1016/S1529-9430(02)00450-3. [DOI] [PubMed] [Google Scholar]
- 19.Dreyfuss PH, Dreyer SJ, Herring SA. Lumbar zygapophysial (facet) joint injections. Spine. 1995;20:2040–2047. doi: 10.1097/00007632-199509150-00019. [DOI] [PubMed] [Google Scholar]
- 20.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 21.Gillet P. The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech. 2003;16:338–345. doi: 10.1097/00024720-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Goel VK, Grauer JN, Patel T, Biyani A, Sairyo K, Vishnubhotla S, Matyas A, Cowgill I, Shaw M, Long R, Dick D, Panjabi MM, Serhan H. Effects of charite artificial disc on the implanted and adjacent spinal segments mechanics using a hybrid testing protocol. Spine. 2005;30:2755–2764. doi: 10.1097/01.brs.0000195897.17277.67. [DOI] [PubMed] [Google Scholar]
- 23.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res. 1997;339:76–81. doi: 10.1097/00003086-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Grauer JN, Biyani A, Faizan A, Kiapour A, Sairyo K, Ivanov A, Ebraheim NA, Patel T, Goel VK. Biomechanics of two-level Charite artificial disc placement in comparison to fusion plus single-level disc placement combination. Spine J. 2006;6:659–666. doi: 10.1016/j.spinee.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 25.Hitchon PW, Eichholz K, Barry C, Rubenbauer P, Ingalhalikar A, Nakamura S, Follett K, Lim TH, Torner J. Biomechanical studies of an artificial disc implant in the human cadaveric spine. J Neurosurg Spine. 2005;2:339–343. doi: 10.3171/spi.2005.2.3.0339. [DOI] [PubMed] [Google Scholar]
- 26.Hochschuler SH, Ohnmeiss DD, Guyer RD, Blumenthal SL. Artificial disc: preliminary results of a prospective study in the United States. Eur Spine J. 2002;11(Suppl 2):S106–110. doi: 10.1007/s00586-002-0439-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang RC, Girardi FP, Cammisa FP, Jr, Wright TM. The implications of constraint in lumbar total disc replacement. J Spinal Disord Tech. 2003;16:412–417. doi: 10.1097/00024720-200310000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Huang RC, Girardi FP, Cammisa FP, Jr, Tropiano P, Marnay T. Long-term flexion-extension range of motion of the prodisc total disc replacement. J Spinal Disord Tech. 2003;16:435–440. doi: 10.1097/00024720-200310000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003;16:96–99. doi: 10.1097/00024720-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001;10:309–313. doi: 10.1007/s005860000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laslett M, McDonald B, Aprill CN, Tropp H, Oberg B. Clinical predictors of screening lumbar zygapophyseal joint blocks: development of clinical prediction rules. Spine J. 2006;6:370–379. doi: 10.1016/j.spinee.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 32.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Le Huec J, Basso Y, Mathews H, Mehbod A, Aunoble S, Friesem T, Zdeblick T. The effect of single-level, total disc arthroplasty on sagittal balance parameters: a prospective study. Eur Spine J. 2005;14:480–486. doi: 10.1007/s00586-004-0843-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le Huec JC, Basso Y, Aunoble S, Friesem T, Bruno MB. Influence of facet and posterior muscle degeneration on clinical results of lumbar total disc replacement: two-year follow-up. J Spinal Disord Tech. 2005;18:219–223. [PubMed] [Google Scholar]
- 35.Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988;13:375–377. doi: 10.1097/00007632-198803000-00029. [DOI] [PubMed] [Google Scholar]
- 36.LeHuec JC, Kiaer T, Friesem T, Mathews H, Liu M, Eisermann L. Shock absorption in lumbar disc prosthesis: a preliminary mechanical study. J Spinal Disord Tech. 2003;16:346–351. doi: 10.1097/00024720-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Leivseth G, Braaten S, Frobin W, Brinckmann P. Mobility of lumbar segments instrumented with a ProDisc II prosthesis: a two-year follow-up study. Spine. 2006;31:1726–1733. doi: 10.1097/01.brs.0000224213.45330.68. [DOI] [PubMed] [Google Scholar]
- 38.Lemaire JP, Carrier H, Ali el HS, Skalli W, Lavaste F. Clinical and radiological outcomes with the Charite artificial disc: a 10-year minimum follow-up. J Spinal Disord Tech. 2005;18:353–359. doi: 10.1097/01.bsd.0000172361.07479.6b. [DOI] [PubMed] [Google Scholar]
- 39.Lemaire JP, Skalli W, Lavaste F, Templier A, Mendes F, Diop A, Sauty V, Laloux E. Intervertebral disc prosthesis. Results and prospects for the year 2000. Clin Orthop Relat Res. 1997;337:64–76. doi: 10.1097/00003086-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Lippitt AB. The facet joint and its role in spine pain. Management with facet joint injections. Spine. 1984;9:746–750. doi: 10.1097/00007632-198410000-00016. [DOI] [PubMed] [Google Scholar]
- 41.Liu J, Ebraheim NA, Haman SP, Shafiq Q, Karkare N, Biyani A, Goel VK, Woldenberg L. Effect of the increase in the height of lumbar disc space on facet joint articulation area in sagittal plane. Spine. 2006;31:E198–E202. doi: 10.1097/01.brs.0000206387.67098.a0. [DOI] [PubMed] [Google Scholar]
- 42.Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J. 2005;14:654–658. doi: 10.1007/s00586-004-0692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Manchikanti L, Boswell MV. Sacroiliac joint pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2005;18(Suppl):S135. doi: 10.1097/01.bsd.0000128057.80589.e7. [DOI] [PubMed] [Google Scholar]
- 44.Marks RC, Houston T, Thulbourne T. Facet joint injection and facet nerve block: a randomised comparison in 86 patients with chronic low back pain. Pain. 1992;49:325–328. doi: 10.1016/0304-3959(92)90239-8. [DOI] [PubMed] [Google Scholar]
- 45.Mayer HM, Wiechert K. Microsurgical anterior approaches to the lumbar spine for interbody fusion and total disc replacement. Neurosurgery. 2002;51:S159–S165. doi: 10.1097/00006123-200211002-00022. [DOI] [PubMed] [Google Scholar]
- 46.Mayer HM, Wiechert K, Korge A, Qose I. Minimally invasive total disc replacement: surgical technique and preliminary clinical results. Eur Spine J. 2002;11(Suppl 2):S124–S130. doi: 10.1007/s00586-002-0446-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McAfee PC, Cunningham BW, Hayes V, Sidiqi F, Dabbah M, Sefter JC, Hu N, Beatson H. Biomechanical analysis of rotational motions after disc arthroplasty: implications for patients with adult deformities. Spine. 2006;31:S152–S160. doi: 10.1097/01.brs.0000234782.89031.03. [DOI] [PubMed] [Google Scholar]
- 48.McAfee PC, Fedder IL, Saiedy S, Shucosky EM, Cunningham BW. SB Charite disc replacement: report of 60 prospective randomized cases in a US center. J Spinal Disord Tech. 2003;16:424–433. doi: 10.1097/00024720-200308000-00016. [DOI] [PubMed] [Google Scholar]
- 49.Moshirfar A, Jenis LG, Spector LR, Burke PJ, Losina E, Katz JN, Rand FF, Tromanhauser SG, Banco RJ. Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine. 2006;31:2624–2629. doi: 10.1097/01.brs.0000240691.35707.e8. [DOI] [PubMed] [Google Scholar]
- 50.O’Leary P, Nicolakis M, Lorenz MA, Voronov LI, Zindrick MR, Ghanayem A, Havey RM, Carandang G, Sartori M, Gaitanis IN, Fronczak S, Patwardhan AG. Response of Charite total disc replacement under physiologic loads: prosthesis component motion patterns. Spine J. 2005;5:590–599. doi: 10.1016/j.spinee.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 51.Polly DW., Jr Adapting innovative motion-preserving technology to spinal surgical practice: what should we expect to happen? Spine. 2003;28:S104–S109. doi: 10.1097/01.BRS.0000092208.09020.16. [DOI] [PubMed] [Google Scholar]
- 52.Putzier M, Funk JF, Schneider SV, Gross C, Tohtz SW, Khodadadyan-Klostermann C, Perka C, Kandziora F. Charite total disc replacement-clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006;15:183–195. doi: 10.1007/s00586-005-1022-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rohlmann A, Zander T, Bergmann G. Effect of total disc replacement with ProDisc on intersegmental rotation of the lumbar spine. Spine. 2005;30:738–743. doi: 10.1097/01.brs.0000157413.72276.c4. [DOI] [PubMed] [Google Scholar]
- 54.Rousseau MA, Bradford DS, Bertagnoli R, Hu SS, Lotz JC. Disc arthroplasty design influences intervertebral kinematics and facet forces. Spine J. 2006;6:258–266. doi: 10.1016/j.spinee.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 55.Sariali el H, Lemaire JP, Pascal-Mousselard H, Carrier H, Skalli W. In vivo study of the kinematics in axial rotation of the lumbar spine after total intervertebral disc replacement: long-term results: a 10–14 years follow up evaluation. Eur Spine J. 2006;15:1501–1510. doi: 10.1007/s00586-005-0016-5. [DOI] [PubMed] [Google Scholar]
- 56.Shim CS, Lee SH, Shin HD, Kang HS, Choi WC, Jung B, Choi G, Ahn Y, Lee S, Lee HY. CHARITE versus ProDisc: a comparative study of a minimum 3-year follow-up. Spine. 2007;32:1012–1018. doi: 10.1097/01.brs.0000260795.57798.a0. [DOI] [PubMed] [Google Scholar]
- 57.Siepe CJ, Mayer HM, Heinz-Leisenheimer M, Korge A. Total lumbar disc replacement: different results for different levels. Spine. 2007;32:782–790. doi: 10.1097/01.brs.0000259071.64027.04. [DOI] [PubMed] [Google Scholar]
- 58.Siepe CJ, Mayer HM, Wiechert K, Korge A. Clinical results of total lumbar disc replacement with ProDisc II: three-year results for different indications. Spine. 2006;31:1923–1932. doi: 10.1097/01.brs.0000228780.06569.e8. [DOI] [PubMed] [Google Scholar]
- 59.Siepe CJ, Wiechert K, Khattab MF, Korge A, Mayer HM. Total lumbar disc replacement in athletes: clinical results, return to sport and athletic performance. Eur Spine J. 2007;16:1001–1013. doi: 10.1007/s00586-006-0257-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Singh K, Vaccaro AR, Albert TJ. Assessing the potential impact of total disc arthroplasty on surgeon practice patterns in North America. Spine J. 2004;4:195S–201S. doi: 10.1016/j.spinee.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 61.Tournier C, Aunoble S, Le Huec JC, Lemaire JP, Tropiano P, Lafage V, Skalli W. Total disc arthroplasty: consequences for sagittal balance and lumbar spine movement. Eur Spine J. 2007;16:411–421. doi: 10.1007/s00586-006-0208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Trouillier H, Kern P, Refior HJ, Muller-Gerbl M. A prospective morphological study of facet joint integrity following intervertebral disc replacement with the CHARITE™ Artificial Disc. Eur Spine J. 2006;15:174–182. doi: 10.1007/s00586-005-1010-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Umehara S, Zindrick MR, Patwardhan AG, Havey RM, Vrbos LA, Knight GW, Miyano S, Kirincic M, Kaneda K, Lorenz MA. The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine. 2000;25:1617–1624. doi: 10.1097/00007632-200007010-00004. [DOI] [PubMed] [Google Scholar]
- 64.Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: a report of 27 patients with the SB Charite disc. J Spinal Disord Tech. 2003;16:369–383. doi: 10.1097/00024720-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 65.Tulder MW, Koes B, Seitsalo S, Malmivaara A. Outcome of invasive treatment modalities on back pain and sciatica: an evidence-based review. Eur Spine J. 2006;15(Suppl 1):S82–92. doi: 10.1007/s00586-005-1049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zeegers WS, Bohnen LM, Laaper M, Verhaegen MJ. Artificial disc replacement with the modular type SB Charite III: 2-year results in 50 prospectively studied patients. Eur Spine J. 1999;8:210–217. doi: 10.1007/s005860050160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zigler J, Delamarter R, Spivak JM, Linovitz RJ, Danielson GO, 3rd, Haider TT, Cammisa F, Zuchermann J, Balderston R, Kitchel S, Foley K, Watkins R, Bradford D, Yue J, Yuan H, Herkowitz H, Geiger D, Bendo J, Peppers T, Sachs B, Girardi F, Kropf M, Goldstein J. Results of the prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine. 2007;32:1155–1162. doi: 10.1097/BRS.0b013e318054e377. [DOI] [PubMed] [Google Scholar]
- 68.Zigler JE. Clinical results with ProDisc: European experience and U.S. investigation device exemption study. Spine. 2003;28:S163–S166. doi: 10.1097/00007632-200310151-00009. [DOI] [PubMed] [Google Scholar]
- 69.Zigler JE, Burd TA, Vialle EN, Sachs BL, Rashbaum RF, Ohnmeiss DD. Lumbar spine arthroplasty: early results using the ProDisc II: a prospective randomized trial of arthroplasty versus fusion. J Spinal Disord Tech. 2003;16:352–361. doi: 10.1097/00024720-200308000-00007. [DOI] [PubMed] [Google Scholar]