Abstract
Introduction Few studies have investigated the long-term effect of posterolateral lumbar spinal fusion on functional outcome. Aim To investigate the long-term result after posterolateral lumbar spinal fusion with and without pedicle screw instrumentation. Methods Questionnaire survey of 129 patients originally randomised to posterolateral lumbar spinal fusion with or without pedicle screw instrumentation. Follow-up included Dallas Pain Questionnaire (DPQ), Oswestry Disability Index (ODI), SF-36 and a question regarding willingness to undergo the procedure again knowing the result as global outcome parameter. Results Follow-up was 83% of the original study population (107 patients). Average follow-up time was 12 years (range 11–13 years). DPQ-scores were significantly lower than preoperatively in both groups (P < 0.005) and no drift towards the preoperative level was seen. No difference between the two groups were observed (instrumented vs. non-instrumented): DPQ Daily Activity mean 37.0 versus 32.0, ODI mean 33.4 versus 30.6, SF-36 PCS mean 38.8 versus 39.8, SF-36 MCS mean 49.0 versus 53.3. About 71% in both groups were answered positively to the global outcome question. Patients who had retired due to low back pain had poorer outcome than patients retired for other reasons, best outcome was seen in patients still at work (P = 0.01 or less in all questionnaires, except SF-36 MCS P = 0.08). Discussion Improvement in functional outcome is preserved for 10 or more years after posterolateral lumbar spinal fusion. No difference between instrumented fusion and non-instrumented fusion was observed. Patients who have to retired due to low back pain have the smallest improvement.
Keywords: Lumbar spinal fusion, Randomised clinical trial, Outcome
Introduction
Lumbar spinal fusion is today the most rapidly growing orthopaedic procedure in the USA [9, 10]. The rates have been steadily rising through the 80s and 90s. It is however only within the last few years that randomised controlled studies have been published seeking to justify the procedure when compared to continuing conservative care [4, 5, 11, 13, 14, 17, 24].
Several studies have dealt with the most advantageous type of operation; especially focus has been on the beneficial effect of supplementary pedicle screw instrumentation. The latest Cochrane review [17] summarizes this into: Pedicle screw instrumentation produces a higher fusion rate, but any improvement in clinical outcome is probably marginal as compared to fusion without instrumentation.
Long-term follow-up on the studies comparing fusion with or without instrumentation has shown similar results. Ekman et al. [11] published data on an average of 9-year follow-up on a randomised controlled trial comparing fusion with and without instrumentation in spondylolisthesis patients. They were not able to show any difference between the two groups at this long-term follow-up. Christensen et al. [8] presented data on 5-year follow-up in a randomised controlled trial on fusion with or without instrumentation in a group of patients with mixed diagnosis. They could not demonstrate any overall differences between the two groups either. But trends were seen for a differential effect of instrumentation depending on the diagnosis of the patients. It seemed spondylolisthesis favoured non-instrumented fusion whereas degenerative changes in patients without prior spine surgery favoured instrumented fusion. Longitudinal analysis of the data in these two studies showed a preserved effect of the fusion procedure with no difference between the two groups, however, in the study by Ekman et al. there was a slight drift towards the preoperative values, whereas in the Christensen et al. study a continuous improvement was observed. About 5–10 years follow-up on the Swedish Spine Study also showed a stable effect of the fusion procedure, unfortunately without any information on differences between the different surgical groups [16].
This is a long-term follow-up on a randomised controlled trial comparing fusion with or without pedicle screw instrumentation previously reported on [8, 28].
Materials and methods
Patients
The original study included 130 patients [28], randomised to posterolateral lumbar fusion with or without Cotrell–Doubousset pedicle screw instrumentation in the period from November 1992 to November 1994. All patients suffered at inclusion from severe chronic low back pain due to localised lumbar or lumbosacral instability caused by either isthmic spondylolisthesis grade I–II, primary degeneration (no previous surgery), secondary or accelerating degeneration after decompressive surgery [8, 28]. The fusions were all done in situ without any attempt at peroperative reduction.
A total of 125 patients were available for 11–13 years follow-up. One patient (from the instrumented group) was peroperatively excluded from the study due to dysplastic pedicles. Four patients had died for unrelated reasons. All available patients were mailed a package of questionnaires described below in June 2005. The package was re-issued to non-responders after 4 months and a reminder was given per telephone 4 weeks after this. Five patients denied participation in the follow-up and 13 patients did not answer the mailed questionnaires. This resulted in an overall follow-up of 107 patients (83%): 53 patients in the instrumented 54 patients in the non-instrumented group. Average follow-up was 12 years ranging from 11 to 13 years. There was no difference in demographic data between the two groups with the exception that the patients in the instrumented group were now slightly older than those in the non-instrumented group (Table 1). Missing patients were equally distributed between the two groups (Table 2).
Table 1.
Characteristics of the follow-up population according to study group
| Instrumented | Non-instrumented | ||
|---|---|---|---|
| Sex (female/male) | 23/30 | 26/28 | NS |
| Age at operation (years) | 46.5 (20–66) | 42.7 (20–67) | NS (P = 0.0619) |
| Age at follow-up (years) | 58.5 (32–78) | 54.7 (33–80) | P = 0.0495 |
| Follow-up time (years) | 12 (11–13) | 12 (11–13) | NS |
| Duration of symptoms | NS | ||
| <2 years | 11 | 13 | |
| >2 years | 42 | 41 | |
| Diagnosis (+decompression) | NS (NS) | ||
| Isthmic spondylolisthesis | 14 (8) | 15 (5) | |
| Primary degeneration | 19 (11) | 17 (4) | |
| Secondary degeneration | 20 (11) | 22 (17) | |
| Additional neural decompression | 30 | 26 | NS |
| Operated level(s) | NS | ||
| 1 level | 32 | 34 | |
| 2 levels | 16 | 16 | |
| 3 levels | 5 | 4 | |
| One level | NS | ||
| Above L5-S1 | 28 | 27 | |
| L5-S1 | 25 | 27 | |
| Radiographic fusion at 2-year follow-up | 42 | 46 | NS |
Values are mean (range) or number
Table 2.
Characteristics of missing patients
| Case | Patient No. | Age at operation | Sex | Group | Diagnosis | Preoperative employment status | Cause of drop-out |
|---|---|---|---|---|---|---|---|
| 1 | 1 | 41 | Male | Instrumented | Spondylolisthesis | Sick leave | Non-compliance |
| 2 | 11 | 51 | Female | Non-instrumented | Primary degeneration | Pension | Dead |
| 3 | 16 | 60 | Female | Instrumented | Primary degeneration | Pension | Non-compliance |
| 4 | 17 | 56 | Male | Instrumented | Secondary degeneration | Pension | Dead |
| 5 | 23 | 60 | Female | Non-instrumented | Secondary degeneration | Pension | Non-compliance |
| 6 | 25 | 57 | Male | Non-instrumented | Spondylolisthesis | Working | Denied participation |
| 7 | 28 | 40 | Female | Instrumented | Secondary degeneration | Sick leave | Non-compliance |
| 8 | 32 | 40 | Female | Non-instrumented | Spondylolisthesis | Working | Non-compliance |
| 9 | 38 | 52 | Female | Instrumented | Secondary degeneration | Sick leave | Non-compliance |
| 10 | 39 | 47 | Female | Non-instrumented | Primary degeneration | Sick leave | Non-compliance |
| 11 | 45 | 35 | Male | Instrumented | Spondylolisthesis | Sick leave | Non-compliance |
| 12 | 72 | 35 | Male | Non-instrumented | Spondylolisthesis | Sick leave | Denied participation |
| 13 | 75 | 50 | Female | Non-instrumented | Primary degeneration | Working | Non-compliance |
| 14 | 82 | 32 | Male | Instrumented | Primary degeneration | Working | Denied participation |
| 15 | 84 | 48 | Male | Non-instrumented | Primary degeneration | Working | Dead |
| 16 | 103 | 39 | Female | Non-instrumented | Secondary degeneration | Working | Non-compliance |
| 17 | 109 | 31 | Male | Instrumented | Secondary degeneration | Sick leave | Non-compliance |
| 18 | 116 | 50 | Male | Non-instrumented | Primary degeneration | Sick leave | Denied participation |
| 19 | 119 | 47 | Male | Instrumented | Primary degeneration | Pension | Non-compliance |
| 20 | 121 | 41 | Male | Instrumented | Primary degeneration | Sick leave | Denied participation |
| 21 | 122 | 35 | Female | Non-instrumented | Spondylolisthesis | Sick leave | Non-compliance |
| 22 | 130 | 52 | Female | Non-instrumented | Primary degeneration | Sick leave | Dead |
Outcome parameters
All patients received a battery of questionnaires in order to get a comprehensive picture of pain, disability, quality of life as well as work related issues at this long-term follow-up.
The main outcome parameter was functional outcome as assessed by the Dallas Pain Questionnaire (DPQ) [22]. This had been the main outcome instrument throughout the whole study period and was obtained preoperatively and at 1, 2, 5 and this 11–13 year follow-up. The questionnaire assesses the impact of chronic spinal pain in four categories: Daily activities, Work-Leisure activities, Anxiety-Depression and Social interest. A high score indicates a high influence of back pain on the daily life of the patient and thus a poor outcome. Secondary functional outcome parameters used in this study were the SF-36 [2, 30] and the Oswestry Disability Index (ODI) [12], administered only at this long-term follow-up. The SF-36 is a generic health survey measure. It yields a profile of scores in eight scales covering different physical and mental components of health [30]. The score in each scale ranges from 0 (poorest health) to 100 (best health). Additionally two summary measures are produced: A Physical Component Summary (PCS) and a Mental Component Summary (MCS). The two summary measures are calculated so that a value of 50 is equal to the US population mean. The ODI is a condition specific outcome measure for spinal disorders [12]. It yields an index score which can range from 0 to 100, with a high percentage reflecting a high degree of disability.
Back and leg pain was assessed by the pain scales from the Low Back Pain Rating Scale (LBPRS) [23], which was administered at this as well as the 5-year follow-up. They are 11 point (0–10) numerical rating scales assessing both back and leg pain in three ways: Worst pain within the last 14 days, average pain within the last 14 days and actual pain level at the time of completing the questionnaire.
The patients answer to the question “Would you undergo the same treatment again, now that you know the result?” served as global outcome parameter.
Work status and employment was assessed by a questionnaire covering present employment status, questions regarding the cause of retirement if this was the case and questions regarding any legal ongoing cases [8].
Statistics
All analyses comparing the two intervention groups were done using the intention to treat principle. Comparison between two groups were done using either the Mann–Whitney rank-sum test for unpaired data or the Wilcoxon signed rank test for paired data or using chi-square statistics depending on the nature of the data. When comparing more than two groups the Kruskal–Wallis test for equality of groups were used with correction for ties. Significance level was 5% using two-tailed testing. Intercooled Stata version 9 for Windows was the software used for the statistical analysis.
Results
Functional outcome
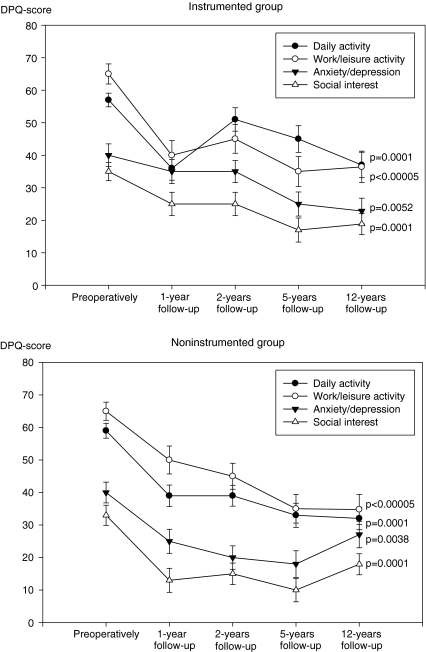
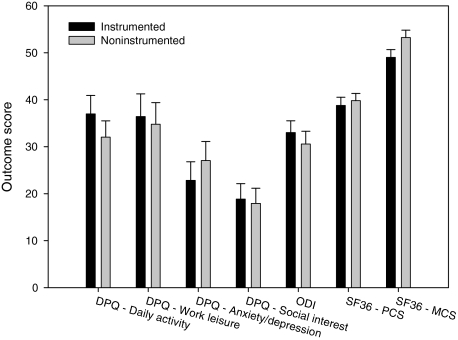
No significant difference in any of the outcome parameters was seen between the two groups. Dallas Pain Questionnaire scores showed no sign of a return towards preoperative levels except for anxiety-depression and social interest in the non-instrumented group were a slight increase was seen (Fig. 1). All scores were however significantly lower than the preoperative values. No difference between the two groups was seen in any of the four categories (Fig. 2). The mean change from preoperatively to this follow-up ranged from 13 to 26, being largest in the daily activity and work-leisure activity categories, but with no differences between the two groups. Back and leg pain as assessed by the LBPRS was unchanged from the 5-year follow-up with no difference between the instrumented and non-instrumented group (Table 3).
Fig. 1.
DPQ scores preoperatively and at each follow-up in the two treatment groups. Values are mean and standard error of mean. All 12-year follow-up scores are significantly improved from preoperatively
Fig. 2.
Different outcome scores for the two treatment groups. Values are mean and standard error. No significant difference between the two groups (Mann–Whitney rank-sum test) (Although MCS P = 0.0528)
Table 3.
Scores at 5 and 10-year follow-up for the LBPRS
| 5-year follow-up | 10-year follow-up | |||
|---|---|---|---|---|
| Instrumented | Non-instrumented | Instrumented | Non-instrumented | |
| Back pain right now | 4.0 (3.00) | 4.0 (3.02) | 3.0 (2.93) | 4.0 (2.88) |
| Worst back pain within last 14 days | 5.5 (3.43) | 6.0 (3.39) | 5.0 (3.24) | 5.0 (3.36) |
| Average back pain within last 14 days | 4.0 (2.90) | 4.0 (3.04) | 3.0 (2.71) | 4.0 (2.79) |
| Leg pain rigth now | 2.0 (3.26) | 2.0 (3.18) | 1.5 (2.70) | 3.0 (3.07) |
| Worst leg pain within last 14 days | 3.0 (3.50) | 4.0 (3.38) | 3.0 (3.16) | 3.0 (3.33) |
| Average leg pain within last 14 days | 2.0 (3.09) | 3.0 (3.02) | 2.0 (2.72) | 3.0 (3.06) |
Values are median (standard deviation). No significant differences were found at any timepoint between the two groups
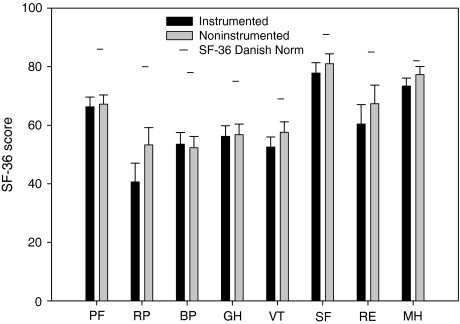
The overall score of the ODI was 33.0 in the instrumented group and 30.6 in the non-instrumented group (not significant) (Fig. 2). With respect to the SF-36 no significant difference between the two groups was observed. Neither in the two summary scales (Fig. 2) nor in the eight subscales (Fig. 3). Comparing the SF-36 health profile of the two groups with Danish norm material [1] results in a similar profile but with values below the Danish norm in all eight subscales. Differences were around 20 points except in the Role Physical scale were it was around 30 points and in the Social Functioning and Mental Health scales were it was around 10 points. Concerning the Physical Component Score 20.7% of the patients had a score which was above the age- and sex-adjusted Danish norm (data not shown).
Fig. 3.
Scores of the eight SF36 subscales according to treatment group. Values are mean and standard error. No significant difference between the two groups in any of the scales. Data on Danish norm material is adapted from Bjørner et al. [1]
The 5-year follow-up results suggested different results in the two groups depending on the operational diagnosis. These findings could not be confirmed at this long-term follow-up stage (Table 4). However the tendency towards favourable outcome in the non-instrumented spondylolisthesis patients as compared with those receiving instrumentation remained. Likewise the tendency towards a beneficial effect of instrumentation in the primary degeneration group could still be observed.
Table 4.
Score of the different outcome measures according to operational diagnosis
| Spondylolisthesis | Primary degeneration | Secondary degeneration | ||||
|---|---|---|---|---|---|---|
| Instrumented | Non-instrumented | Instrumented | Non-instrumented | Instrumented | Non-instrumented | |
| Dallas pain questionaire | ||||||
| Daily activities | 34.2 (22.4) | 21.4 (19.3) | 33.7 (30.9) | 45.2 (20.8) | 41.9 (29.1) | 28.4 (24.9) |
| Work-leisure | 27.7 (31.0) | 30.0 (33.0) | 35.0 (33.2) | 36.9 (28.0) | 45.0 (33.9) | 37.1 (34.0) |
| Anxiety/depression | 24.5 (30.6) | 18.7 (28.9) | 17.4 (22.7) | 26.6 (23.4)*** | 27.5 (27.1) | 33.8 (32.4) |
| Social interest | 15.4 (20.0) | 11.3 (23.0) | 17.5 (21.8) | 21.8 (23.6) | 23.4 (26.5) | 19.7 (22.7) |
| Oswestry disability index | ||||||
| ODI score | 30.9 (14.8) | 18.2 (13.9)* | 31.1 (21.6) | 35.1 (15.0) | 36.3 (17.0) | 34.4 (23.1) |
| SF-36 | ||||||
| Physical component score | 43.6 (10.3) | 42.7 (11.7) | 38.9 (13.6) | 36.5 (8.0) | 35.8 (10.3) | 40.3 (11.0) |
| Mental component score | 49.3 (8.8) | 55.5 (12.1)** | 50.0 (10.6) | 52.7 (9.5) | 47.8 (13.5) | 52.2 (10.9) |
Values are mean (standard deviation)
*P = 0.0287, **P = 0.0523, ***P = 0.0860
P-values are Mann–Whitney rank-sum test that the groups are equal
A total of 104 patients had answered the SF-36 health transition item and eight patients (8%) characterised themselves as much or somewhat better than 1 year ago, 76 (73%) as unchanged and 20 (19%) as somewhat or much worse, compared to 1 year ago. There was no difference in this distribution between the instrumented and non-instrumented group.
A total of 94 patients (46 in the instrumented and 48 in the non-instrumented group) had answered the question regarding willingness to undergo the procedure again knowing the result. About 72% in the instrumented and 71% in the non-instrumented group were positive and answered yes (not significant).
Work status and employability
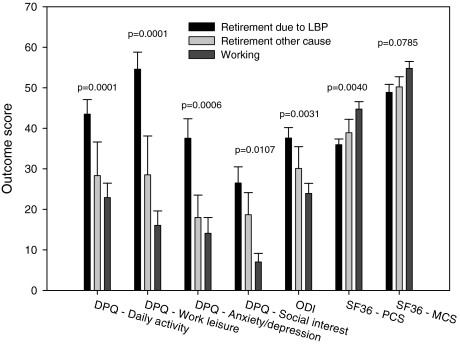
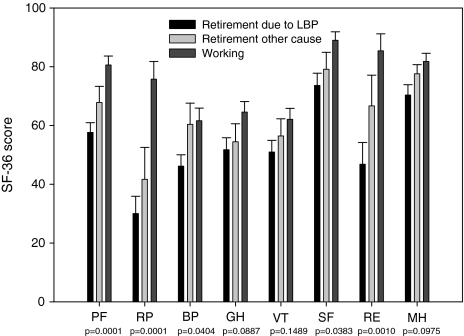
In total, 33 patients were working (31%), one seeking work (1%), three patients were sick-listed (3%). The reminders were retired (61%) or had applied for retirement (4%). About 68% of the retired patients noted low back pain as cause of retirement. There was no difference between the two treatment groups. For comparison of outcome in relation to work status those retired or applying for retirement due to low back pain was pooled and compared to those retired or applying for retirement due to other causes and the group of patients still working. The four patients’ sick-listed or seeking work, were excluded in this analysis for simplicity. Those still at work had significantly better outcome scores than the group retired due to other reasons, which again had better scores than those patients retired due to back pain (Figs. 4 and 5). SF-36 scores for the working group were similar to the Danish norm material. Poorest outcome scores were observed in those patients noting low back pain as cause of their retirement. With regards to the different categories of the SF-36 differences between the three groups were mostly marked in the Role-Physical (RP) and the Role-Emotional (RE) categories, and in the Physical component score (PCS). In the DPQ greatest differences between the three groups were seen in the work-leisure category.
Fig. 4.
Score of the different outcome measures according to employment status. P-values are Kruskal–Wallis test (with ties) that the groups are equal
Fig. 5.
Scores of the eight SF36 subscales according to employment status. Values are mean and standard error. P-values are Kruskal–Wallis test (with ties) for difference between the groups
It has to be noted that there was a significant difference in age at follow-up between the three groups (P = 0.0001). Those retired due to other causes were oldest (mean age 67 years) compared to those retired due to back pain (mean age 59 years old) and those still at work (mean age 47 years).
A total of 12 patients (seven in the instrumented group and five in the non-instrumented group) were involved in ongoing civil action procedures at 10-year follow-up. The procedures were work injury, patient insurance, indemnity or complaint suits. Six of the patients had ongoing procedures since the 5-year follow-up, whereas the other six were new claims. There was no significant difference between the patients with ongoing civil action procedures and those without with regards to any of the outcome variables.
Discussion
This long-term follow-up had an excellent follow-up rate of 83%, thus minimizing the risk of any eventual bias, furthermore were the missing patients equally distributed with respect to age, gender, diagnosis, preoperative employment status and assigned treatment group. It therefore seems reasonable to conclude that any significant non-responder bias is absent.
Using a comprehensive “battery” of validated questionnaires, to get a broad picture of the patients’ status at this long-term follow-up after a lumbar spinal fusion procedure, we could not demonstrate any difference between the two treatment groups in any of the measures used. This is in concordance with the results from previously published long-term results on randomised controlled trials comparing instrumented versus non-instrumented fusion. In the study reported by Ekman et al. [11] no differences between the instrumented and non-instrumented group was seen either. In the 5-year follow-up on this population no difference between the instrumented ad the non-instrumented group was seen [8].
Ekman et al. [11] reported a deterioration of functional outcome scores from 2 years to the late follow-up. We observed no diminishing effect of the operation but a stable effect kept over the years. This was also the case in the mid term (5–10 years) follow-up results on the Swedish Spine Study [16]. They did not report on differences between the surgical groups, but reported that the effect in the surgical groups were stable with only a slight increase in back pain. In a retrospective cohort study with more than 10-year follow-up Glaser et al. [18] observed slight improvement in several pain and functional outcome parameters from early to late follow-up in patients who underwent instrumented lumbar spinal fusion. Although the DPQ-score was the only longitudinal measure used in this study the stability of this result is further supported by the fact that the LBPRS scores were unchanged from 5 year to the present follow-up.
In the Swedish Spine Study a decrease from around 48 to 34–36 in the ODI was observed from preoperatively to 2-year follow-up, regardless of whether instrumentation was performed or not [15], thus values comparable to those obtained in this study in the two “degenerative groups”. With respect to the group of spondylolisthesis patients Ekman et al. [11] observed ODI scores of 30 and 27 in the non-instrumented and instrumented group, respectively, comparable to the instrumented group in our study. In a large study on fusion patients Glassmann et al. [19] observed ODI scores at 1 and 2 years similar to those reported in our study. They also observed higher scores in patients with a history of prior spine surgery. In a 5–9 year follow-up on a study comparing instrumented posterior fusion with 360°-fusion in a similar patient group Videbaek et al. reported a median ODI of 40 in the group with instrumented posterolateral fusion [29]. Thus it seems reasonable to conclude that the ODI scores observed in this study at long-term follow-up are well in the vicinity of previous reported short to mid-term data. This could indicate a stable effect of the fusion procedure, although the preoperative ODI score in this study is unknown.
Zanoli et al. [31] described preoperative SF-36 values obtained from Swedish patients with various diagnoses undergoing spinal surgery. Comparing the SF-36 values from this study with the Swedish preoperative data showed better scores in the PF, RP, BP categories, also in the VT, SF, RE, MH categories the scores were better although not to the same extent. Only the GH category showed no difference. Ekman et al. [11] observed SF-36 scores at long-term follow-up similar to those observed in this study.
We observed significant better outcome scores in the group of patients who were still at work at the time of follow-up. With regards to the SF-36 this might partially be an effect of as age as this group was youngest. However the group with the worst scores were that on retirement due to LBP and this group was on the average younger than the group on retirement due to other cause (e.g. age) which were older. Thus it seems obvious that those patients with the worst outcome after spinal surgery are those who need retirement due to their back problem. This further stresses the importance on the subject of keeping people with back problems in the work force.
We found no relation between outcomes and ongoing civil action procedure as opposed to the result from the 5-year follow-up. The reason for this remains unexplained as the questionnaire does not go into detail about the relation to patients back problem. The number of claims was however a mixture between ongoing and new procedures which could be an explanation.
The differences in outcome between instrumented and non-instrumented fusion observed when stratifying for operational diagnosis were not longer significant, as at the 5-year follow-up, but they were still present. This might either be due to a decrease in number of patients as the 5-year follow-up was 93% or it could be that differential effect has diminished. This stratified analysis suggests that patients with degenerative spines benefits from instrumentation, whereas spondylolisthesis patients have superior results when non-instrumented fusion is performed. However in the spondylolisthesis study by Ekman et al. [11] the non-instrumented group did not perform superiorly. A recent meta-analysis by Bono and Lee [3] has shown degenerative spondylolisthsis (as compared to isthmic) patients to benefit from instrumentation. Buttermann et al. [6] showed spondylolisthesis patients to get superior outcome as compared to patients with a diagnosis of degenerative changes, they did, however, not look into the effect of instrumentation because of small numbers. In the study by Videbaek et al. [29] those patients with a degenerative indication for surgery were shown to have additional benefit from a 360° procedure as compared to a instrumented posterior fusion, this was however not the case for the spondylolisthesis patients. As all fusions were done in situ this study cannot address any potential benefit of reduction in the spondylolisthesis patients. Both reduction and additional instrumentation in spondylolisthesis surgery has been debated [7, 21, 25, 26] and a recent review stated that in low-grade adult isthmic spondylolisthesis there was still no evidence to support the use of posterior instrumentation, but also that any effect of reduction has not been adequately studied [20].
Although the lack of difference between the two intervention groups might lead to the conclusion that non-instrumented posterolateral fusion is more cost-effective than its instrumented counterpart, one must acknowledge that this study has not been subjected to cost-effect evaluation. Studies performed at our institution have however shown instrumented fusion to be more expensive as compared with non-instrumented fusion. Furthermore the probability of posterior instrumentation being cost effective was found to be limited [27].
Conclusion
We found the effect of posterolateral lumbar spinal fusion to be preserved at long-term follow-up, with 70% being satisfied with the treatment result. No overall difference between instrumented and non-instrumented fusion was observed, however subgroup results might indicate that the effect of instrumentation is dependent on the diagnosis of the patient.
Reference
- 1.Bjorner JB, Kreiner S, Ware JE, Damsgaard MT, Bech P. Differential item functioning in the Danish translation of the SF-36. J Clin Epidemiol. 1998;51:1189–1202. doi: 10.1016/S0895-4356(98)00111-5. [DOI] [PubMed] [Google Scholar]
- 2.Bjorner JB, Thunedborg K, Kristensen TS, Modvig J, Bech P. The Danish SF-36 Health Survey: translation and preliminary validity studies. J Clin Epidemiol. 1998;51:991–999. doi: 10.1016/S0895-4356(98)00091-2. [DOI] [PubMed] [Google Scholar]
- 3.Bono CM, Lee CK. The influence of subdiagnosis on radiographic and clinical outcomes after lumbar fusion for degenerative disc disorders: an analysis of the literature from two decades. Spine. 2005;30:227–234. doi: 10.1097/01.brs.0000150488.03578.b5. [DOI] [PubMed] [Google Scholar]
- 4.Brox J.I, Sorensen R, Friis A, Nygaard O, Indahl A, Keller A, Ingebrigtsen T, Eriksen HR, Holm I, Koller AK, Riise R, Reikeras O. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine. 2003;28:1913–1921. doi: 10.1097/01.BRS.0000083234.62751.7A. [DOI] [PubMed] [Google Scholar]
- 5.Brox JI, Reikeras O, Nygaard O, Sorensen R, Indahl A, Holm I, Keller A, Ingebrigtsen T, Grundnes O, Lange JE, Friis A. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: a prospective randomized controlled study. Pain. 2006;122:145–155. doi: 10.1016/j.pain.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 6.Buttermann GR, Garvey TA, Hunt AF, Transfeldt EE, Bradford DS, Boachie-Adjei O, Ogilvie JW. Lumbar fusion results related to diagnosis. Spine. 1998;23:116–127. doi: 10.1097/00007632-199801010-00024. [DOI] [PubMed] [Google Scholar]
- 7.Cheung EV, Herman MJ, Cavalier R, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: II. surgical management. J Am Acad Orthop Surg. 2006;14:488–498. doi: 10.5435/00124635-200608000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Christensen FB, Hansen ES, Laursen M, Thomsen K, Bunger CE. Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral spinal fusion: randomized clinical study with a 5-year follow-up. Spine. 2002;27:1269–1277. doi: 10.1097/00007632-200206150-00006. [DOI] [PubMed] [Google Scholar]
- 9.Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery—the case for restraint. N Engl J Med. 2004;350:722–726. doi: 10.1056/NEJMsb031771. [DOI] [PubMed] [Google Scholar]
- 10.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine. 2005;30:1441–1445. doi: 10.1097/01.brs.0000166503.37969.8a. [DOI] [PubMed] [Google Scholar]
- 11.Ekman P, Moller H, Hedlund R. The long-term effect of posterolateral fusion in adult isthmic spondylolisthesis: a randomized controlled study. Spine J. 2005;5:36–44. doi: 10.1016/j.spinee.2004.05.249. [DOI] [PubMed] [Google Scholar]
- 12.Fairbank JC, Pynsent PB. The oswestry disability index. Spine. 2000;25:2940–2953. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 13.Fairbank J, Frost H, Wilson-MacDonald J, Yu LM, Barker K, Collins R. Randomised controlled trial to compare surgical stabilisation of the lumbar spine with an intensive rehabilitation programme for patients with chronic low back pain: the MRC spine stabilisation trial. BMJ. 2005;330:1233. doi: 10.1136/bmj.38441.620417.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fritzell P, Hagg O, Wessberg P, Nordwall A. 2001 volvo award winner in clinical studies: lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish lumbar spine study group. Spine. 2001;26:2521–2532. doi: 10.1097/00007632-200112010-00002. [DOI] [PubMed] [Google Scholar]
- 15.Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002;27:1131–1141. doi: 10.1097/00007632-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 16.Fritzell P, Hagg O, Nordwall (2006) A 5–10 years follow up in the Swedish lumbar spine study. Abstract A124, Spineweek 2004, Porto
- 17.Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis: updated cochrane review. Spine. 2005;30:2312–2320. doi: 10.1097/01.brs.0000182315.88558.9c. [DOI] [PubMed] [Google Scholar]
- 18.Glaser J, Stanley M, Sayre H, Woody J, Found E, Spratt K. A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine. 2003;28:1390–1395. doi: 10.1097/00007632-200307010-00008. [DOI] [PubMed] [Google Scholar]
- 19.Glassman S, Gornet MF, Branch C, Polly D, Jr, Peloza J, Schwender JD, Carreon L. MOS short form 36 and oswestry disability index outcomes in lumbar fusion: a multicenter experience. Spine J. 2006;6:21–26. doi: 10.1016/j.spinee.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs WC, Vreeling A, De KM. Fusion for low-grade adult isthmic spondylolisthesis: a systematic review of the literature. Eur Spine J. 2006;15:391–402. doi: 10.1007/s00586-005-1021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lamberg TS, Remes VM, Helenius IJ, Schlenzka DK, Yrjonen TA, Osterman KE, Tervahartiala PO, Seitsalo SK, Poussa MS. Long-term clinical, functional and radiological outcome 21 years after posterior or posterolateral fusion in childhood and adolescence isthmic spondylolisthesis. Eur Spine J. 2005;14:639–644. doi: 10.1007/s00586-004-0814-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawlis GF, Cuencas R, Selby D, McCoy CE. The development of the Dallas Pain Questionnaire. An assessment of the impact of spinal pain on behavior. Spine. 1989;14:511–516. doi: 10.1097/00007632-198905000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Manniche C, Asmussen K, Lauritsen B, Vinterberg H, Kreiner S, Jordan A. Low back pain rating scale: validation of a tool for assessment of low back pain. Pain. 1994;57:317–326. doi: 10.1016/0304-3959(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 24.Moller H, Hedlund R. Surgery versus conservative management in adult isthmic spondylolisthesis: A prospective randomized study: part 1. Spine. 2000;25:1711–1715. doi: 10.1097/00007632-200007010-00016. [DOI] [PubMed] [Google Scholar]
- 25.Mulholland RC. Comment on topographic relations of neural and ligamentous structures of the lumbosacral junction: in vitro investigation. Spondylolisthesis-no reduction, partial reduction or total reduction? Eur Spine J. 2001;10:133–134. doi: 10.1007/s005860000235. [DOI] [PubMed] [Google Scholar]
- 26.Poussa M, Remes V, Lamberg T, Tervahartiala P, Schlenzka D, Yrjonen T, Osterman K, Seitsalo S, Helenius I. Treatment of severe spondylolisthesis in adolescence with reduction or fusion in situ: long-term clinical, radiologic, and functional outcome. Spine. 2006;31:583–590. doi: 10.1097/01.brs.0000201401.17944.f7. [DOI] [PubMed] [Google Scholar]
- 27.Soegaard R, Christensen FB, Christiansen T, Bunger C. Costs and effects in lumbar spinal fusion. A follow-up study in 136 consecutive patients with chronic low back pain. Eur Spine J. 2007;16:657–668. doi: 10.1007/s00586-006-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE. 1997 volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine. 1997;22:2813–2822. doi: 10.1097/00007632-199712150-00004. [DOI] [PubMed] [Google Scholar]
- 29.Videbaek TS, Christensen FB, Soegaard R, Hansen ES, Hoy K, Helmig P, Niedermann B, Eiskjoer SP, Bunger CE. Circumferential fusion improves outcome in comparison with instrumented posterolateral fusion: long-term results of a randomized clinical trial. Spine. 2006;31:2875–2880. doi: 10.1097/01.brs.0000247793.99827.b7. [DOI] [PubMed] [Google Scholar]
- 30.Ware JE., Jr SF-36 health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 31.Zanoli G, Jonsson B, Stromqvist B. SF-36 scores in degenerative lumbar spine disorders. Analysis of prospective data from 451 patients. Acta Orthop. 2006;77:298–306. doi: 10.1080/17453670610046064. [DOI] [PubMed] [Google Scholar]