Abstract
Objective
When to start hepatitis C treatment in HIV/hepatitis C virus (HCV)–coinfected patients remains unresolved. Our objective was to determine if a baseline CD4 count ≥350 cells/mm3 predicts a sustained HCV response to pegylated interferon plus ribavirin.
Methods
We conducted a multicenter cohort study of HIV/HCV-coinfected patients treated for HIV in hospitals in Nice, Tourcoing, and Marseille (France). Sustained viral response (SVR) was defined as undetectable HCV RNA 24 weeks after treatment. The relation between CD4 cell count and SVR was examined separately for patients with HCV genotype 1 or non-1.
Results
One hundred seventy-five patients were included. In patients with HCV genotype 1, the rate of SVR was 13% and was not related to baseline CD4 cell count (odds ratio [OR] = 1.0, 95% confidence interval [CI]: 0.1 to 9.3). In patients with HCV genotype non-1, the rate of SVR was 46% and was not significantly increased by a baseline CD4 count ≥350 cells/mm3 (OR = 1.8, 95% CI: 0.6 to 5.9).
Conclusions
Higher CD4 cell count at treatment initiation with pegylated interferon plus ribavirin did not improve treatment success probability, regardless of HCV genotype.
Keywords: antiviral agents, cohort studies, genotype, hepatitis C, chronic, HIV infections
Hepatitis C virus (HCV) is present in approximately one third of patients infected with HIV in developed countries.1,2 The accelerated progression of chronic hepatitis C and the increase in life expectancy of HIV-infected patients with the use of combination antiretroviral therapy (ART) have led to an increase in hospitalizations and deaths attributable to HCV in HIV/HCV-coinfected patients.3–5 The efficacy of HCV therapy is usually assessed by the presence of a sustained viral response (SVR), defined as the persistence of undetectable plasma HCV RNA 24 weeks after treatment. The combination of pegylated interferon plus ribavirin has been shown superior to other treatments for HCV in HIV-infected patients, with SVRs varying from 16% to 40%.6–13 Early eradication of HCV is encouraged to avoid cirrhosis and because HCV may accelerate HIV disease progression and impair response to ART, although this is controversial.3,4,14–16 HCV therapy is 6 to 12 months in duration, however, and has potentially severe side effects and interactions with some antiretrovirals.6–12,17,18 Predictive factors for SVR are still unclear, except for HCV genotype non-1.6,7,9–13 Yet, knowledge of these predictive factors is critical to determine the optimal timing to start HCV treatment.
Clinical guidelines have used CD4 cell count as a selection criterion, although there is no clear evidence to date of a relation between CD4 cell count at baseline and response to therapy.6–12,19,20 Moreover, clinical trials frequently exclude subjects with CD4 counts <300 cells/mm3, thus limiting experience in a significant subset of HIV-infected patients who are at risk for significant morbidity from progressive HCV disease. The aim of this study was to determine if CD4 cell count is predictive of sustained HCV viral response to pegylated interferon plus ribavirin in HIV/HCV-coinfected patients.
METHODS
Study Design
We conducted a retrospective multicenter cohort study with 3 French cohorts of HIV/HCV-coinfected patients followed in Nice University Hospital, Marseille University Hospital, and Tourcoing Hospital. Patients were treated for various durations. Follow-up lasted from the first pegylated interferon plus ribavirin therapy initiation date to 24 weeks after treatment. We considered premature treatment discontinuation and loss to follow-up as failures (ie, no SVR).
Data Sources
Data were drawn from the NADIS medical record. The NADIS (Fedialis Medica, Marly le Roi, France) is an electronic medical record designed for the management of HIV- or HCV-infected patients, allowing prospective real-time data collection.21,22 It has been used in the 3 study centers since 2000. The typical follow-up for HIV-infected patients consists of 1 outpatient visit every 3 months. At each visit, the physician enters clinical, laboratory, and treatment data into the record. When necessary for the study, additional data were added from the gastroenterology department medical files and from the laboratory registries at these 3 hospitals.
We included all HIV/HCV-coinfected patients from the Nice, Marseille, and Tourcoing NADIS cohorts who began pegylated interferon plus ribavirin therapy before June 2004. This included patients on and off ART. Two patients who did not have a CD4 cell count measurement in the 6 months before HCV treatment initiation were excluded.
Outcome Variable: Sustained Viral Response
Treatment success (ie, SVR) was defined as an undetectable serum HCV RNA level 24 weeks after the end of treatment. Serum HCV RNA measurements were performed by quantitative or qualitative polymerase chain reaction (PCR) assays. Using the date of treatment initiation, relevant HCV RNA levels were collected 24 weeks after treatment.
Exposure and Confounding Variables
Baseline CD4 cell count was measured in the 6 months before HCV treatment initiation. Because it has been recommended that HCV therapy ideally should be prescribed if the CD4 count is greater than 350 cells/mm3, baseline CD4 cell count was used as a binary variable (<350 or ≥350 cells/mm3).20 Other baseline variables included age, gender, body mass index (BMI in kg/m2), hepatitis B virus coinfection, HCV genotype, liver fibrosis stage (METAVIR score), mode of infection, alanine aminotransferase (ALT) level, pegylated interferon dose (reduced dose, defined as <1.2 μg/kg/wk, vs. standard dose), previous HCV treatment (yes/no), HIV disease stage (Centers for Disease Control and Prevention [CDC]/World Health Organization [WHO] classification), presence of antiretroviral therapy (yes/no), class of antiretroviral drugs (nonnucleoside reverse transcriptase inhibitors or protease inhibitors), historical nadir CD4 cell count, and HIV RNA level. Because of the extended study period, HCV RNA quantitative measurement was not always available. Indeed, in previous years, HCV RNA was detected by qualitative measurement but often not quantified before HCV treatment. Because we included all patients treated, we included a large number of patients who had no HCV RNA quantitative measurement before treatment. Therefore, because of the high proportion of missing data regarding this variable (n = 72), we did not include it in the analysis.
Statistical Analysis
The analysis was conducted using the intention-to-treat principle and stratified according to HCV genotype (1 or non-1). We conducted univariate analyses to identify factors associated with SVR (Fisher exact test, Wilcoxon). We then fitted logistic regression models using stepwise selection of a priori SVR predictive factors and factors associated with a significance level <0.20. The binary variable CD4 count (<350 or ≥350 cells/mm3) was forced into the model. Entry level was chosen at 0.2, and suppression level was chosen at 0.10. We also conducted a sensitivity analysis with CD4 cell count as a continuous variable using the same methods. The statistical power was too limited to study whether SVR is lower in patients with a baseline CD4 count <200 cells/mm3.
In patients with HCV genotype non-1, because SVR is quite common, odds ratios (ORs) may exaggerate the effect of baseline CD4 cell count on the probability of SVR. We therefore also computed the risk ratio of SVR with a baseline CD4 count ≥350 cells/mm3, using the method proposed by Zhang and Yu.23
All tests were 2-sided, with a 0.05 level of significance. The statistical analysis was conducted using SAS 9 software (SAS Institute, Cary, NC).
RESULTS
We included 175 HIV/HCV-coinfected patients who initiated treatment for HCV infection from April 2000 to May 2004. Breakdown of the patients by center was 58% from Nice, 33% from Marseille, and 9% from Tourcoing. Sixty-nine percent of patients were men. Median age was 40 years (interquartile range [IQR]: 36 to 42 years). Injection drug use was the mode of infection in 81% of patients. Fifty-two percent of patients had HCV genotype 1. The median time since HCV infection was 14.2 years (IQR: 10.1 to 16.6 years). Fifteen percent of patients had previous HCV treatment (7% interferon alone, 8% interferon/ribavirin combination). METAVIR scores were available from liver biopsies in 159 patients and from measurement of noninvasive markers of fibrosis (FibroTest; BioPredictive, Paris, France) in 6 others. Seventy-two (44%) of these 165 patients had advanced fibrosis (METAVIR score of F3 to F4). A reduced dose of pegylated interferon (<1.2 μg/kg/wk) was prescribed initially in 30% of cases. With regard to HIV disease, 18% of patients classified as CDC/WHO stage C. Eighty-six percent of patients were on ART at HCV therapy initiation, and 6% were ART naive. Median ART duration was 5.8 years (IQR: 4.0 to 8.4 years). The median nadir CD4 count was 199 cells/mm3 (IQR: 100 to 346 cells/mm3). Ten patients had CD4 cell counts <200/mm3 at baseline (4 patients with HCV genotype 1, 6 with HCV genotype non-1). HIV RNA level was <400 copies/mL in 77% of patients.
SVR was assessed in 168 of the patients (96%). The rate of SVR was 29% overall, 13% in patients with HCV genotype 1, 46% in patients with genotype 2 or 3, and 42% in patients with genotype 4. One patient had genotype 6 and had an SVR.
HCV Genotype 1
In patients with HCV genotype 1 (n = 91), there was no significant difference in baseline characteristics between patients with a CD4 count <350 cells/mm3 or ≥350 cells/mm3, except for nadir CD4 cell count (Table 1). The SVR rate was 13%. In univariate analysis, younger age, shorter HCV infection duration, and lower HIV RNA level were significantly associated with SVR (Table 2). CD4 count ≥350 cells/mm3 was not associated with SVR (OR = 0.5; P = 0.46).
TABLE 1.
Baseline Characteristics of the Population, According to Genotype
| HCV Genotype 1
|
HCV Genotype Non-1
|
|||||
|---|---|---|---|---|---|---|
| CD4 Count
|
CD4 Count
|
|||||
| <350 Cells/mm3 | ≥350 Cells/mm3 | P | <350 Cells/mm3 | ≥350 Cells/mm3 | P | |
| No. patients | 24 | 66 | 23 | 61 | ||
| Center | ||||||
| Marseille | 46% | 35% | 0.55 | 26% | 30% | 0.86 |
| Tourcoing | 12% | 11% | 4% | 8% | ||
| Nice | 42% | 54% | 70% | 62% | ||
| Age (y) | 39.5 [35.5 to 41.5] | 39.0 [35.0 to 43.0] | 0.64 | 40.0 [37.0 to 45.0] | 39.0 [36.0 to 42.0] | 0.31 |
| Male gender | 71% | 65% | 0.80 | 74% | 70% | 1.00 |
| BMI (kg/m2) | 21 [19 to 22] | 21 [19 to 24] | 0.59 | 22 [19 to 24] | 22 [21 to 24] | 0.81 |
| HBV coinfection | 9% | 8% | 1.00 | 4% | 17% | 0.28 |
| HCV infection duration (y) | 14.3 [7.7 to 17.1] | 13.8 [10.1 to 16.6] | 0.89 | 14.7 [9.9 to 17.6] | 14.3 [10.5 to 16.1] | 0.88 |
| Infection by IDU | 79% | 84% | 0.75 | 83% | 77% | 0.77 |
| ALT (IU/L) | 93 [51 to 115] | 62 [43 to 87] | 0.17 | 57 [44 to 129] | 91 [52 to 126] | 0.17 |
| Advanced fibrosis (F3 to F4) | 48% | 45% | 1.00 | 43% | 40% | 0.80 |
| METAVIR activity score | 2 [1 to 2] | 1 [1 to 2] | 0.12 | 2 [1 to 2] | 2 [1 to 2] | 0.92 |
| Pegylated IFN reduced dose | 32% | 30% | 1.00 | 40% | 25% | 0.25 |
| CDC/WHO stage C | 25% | 15% | 0.35 | 17% | 18% | 1.00 |
| Antiretroviral therapy | ||||||
| Never | 4% | 2% | 0.46 | 4% | 11% | 0.44 |
| Current (any) | 79% | 92% | 0.12 | 91% | 80% | 0.33 |
| Current NNRTI | 25% | 27% | 1.00 | 26% | 20% | 0.56 |
| Current PI | 46% | 50% | 0.81 | 48% | 38% | 0.46 |
| ART duration (y) | 5.8 [3.1 to 9.1] | 6.3 [4.5 to 8.8] | 0.44 | 6.6 [3.6 to 8.6] | 5.7 [4.0 to 7.3] | 0.32 |
| Historical nadir CD4 count (cells/mm3) | 116 [72 to 181] | 217 [102 to 367] | <0.01 | 112 [64 to 240] | 302 [150 to 417] | <0.01 |
| CD4 count (cells/mm3) | 263 [220 to 316] | 574 [439 to 723] | <0.01 | 250 [251 to 308] | 580 [444 to 720] | <0.01 |
| HIV RNA (log10 copies/mL) | 1.7 [1.3 to 3.3] | 2.1 [1.3 to 3.3] | 0.56 | 1.3 [1.3 to 2.3] | 1.6 [1.3 to 2.4] | 0.65 |
| HIV RNA <400 copies/mL | 62% | 73% | 0.44 | 87% | 82% | 0.75 |
Values are proportion or median [IQR].
HBV indicates hepatitis B virus; IDU, injection drug use; NNRTI, nonnucleoside reverse transcriptase inhibitor; PI, protease inhibitor.
TABLE 2.
SVR Potential Predictive Factors
| HCV Genotype 1 (n = 87)
|
HCV Genotype Non-1 (n = 80)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients With SVR (n = 11)
|
Patients With SVR (n = 37)
|
|||||||||||
| n | Rate or Median [IQR] | P* | ORa† | 95% CI | P | n | Rate or Median [IQR] | P* | ORa† | 95% CI | P | |
| Center | ||||||||||||
| Marseille | 32 | 19% | 0.47 | 22 | 50% | 0.48 | ||||||
| Tourcoing | 10 | 10% | 6 | 67% | ||||||||
| Nice | 45 | 9% | 52 | 42% | ||||||||
| Age (y) | 87 | 35.0 [33.0 to 41.0] | 0.02 | 0.8 | 0.6 to 1.0 | 0.04 | 80 | 40.0 [37.0 to 42.0] | 0.79 | |||
| Gender | ||||||||||||
| Female | 29 | 10% | 0.74 | 23 | 52% | 0.62 | ||||||
| Male | 58 | 14% | 57 | 44% | ||||||||
| BMI (kg/m2) | 87 | 20 [19 to 22] | 0.93 | 80 | 22 [20 to 23] | 0.21 | ||||||
| HCV infection duration | 73 | 9.8 [5.2 to 13.5] | 0.02 | 66 | 14.5 [11.0 to 16.2] | 0.86 | ||||||
| Mode of infection | ||||||||||||
| IDU | 69 | 13% | 1.00 | 63 | 43% | 0.28 | ||||||
| Other | 13 | 15% | 17 | 59% | ||||||||
| ALT (IU/L) | 83 | 75 [37 to 93] | 0.74 | 78 | 66 [48 to 126] | 0.29 | ||||||
| METAVIR fibrosis score | 81 | 2 [2 to 4] | 0.79 | 75 | 3 [2 to 4] | 0.01 | 2.2 | 1.3 to 3.7 | <0.01 | |||
| Advanced fibrosis (F3 to F4) | ||||||||||||
| Yes | 39 | 10% | 0.52 | 31 | 64% | 0.02 | ||||||
| No | 43 | 16% | 44 | 36% | ||||||||
| Previous HCV treatment | ||||||||||||
| Yes | 15 | 13% | 1.00 | 10 | 40% | 0.74 | ||||||
| No | 72 | 12% | 70 | 47% | ||||||||
| Pegylated IFN reduced dose | ||||||||||||
| Yes | 24 | 17% | 0.49 | 21 | 33% | 0.29 | ||||||
| No | 53 | 11% | 47 | 49% | ||||||||
| Antiretroviral therapy | ||||||||||||
| Current (any) | ||||||||||||
| Yes | 77 | 14% | 0.35 | 66 | 47% | 1.00 | ||||||
| No | 10 | 0% | 14 | 43% | ||||||||
| Current NNRTI | ||||||||||||
| Yes | 23 | 22% | 0.15 | 17 | 41% | 0.79 | ||||||
| No | 64 | 9% | 63 | 48% | ||||||||
| Current PI | ||||||||||||
| Yes | 43 | 9% | 0.52 | 31 | 45% | 1.00 | ||||||
| No | 44 | 16% | 49 | 47% | ||||||||
| ART duration (y) | 84 | 4.4 [2.5 to 7.3] | 0.06 | 0.6 | 0.4 to 0.9 | 0.02 | 71 | 5.8 [4.0 to 8.1] | 0.47 | |||
| Historical nadir CD4 count (cells/mm3) | 86 | 213 [110 to 346] | 0.63 | 80 | 302 [103 to 396] | 0.32 | ||||||
| CD4 count ≥350 cells/mm3 | ||||||||||||
| Yes | 65 | 11% | 0.46 | 1.0 | 0.1 to 9.3 | 0.98 | 60 | 48% | 0.61 | 1.7 | 0.5 to 5.4 | 0.39 |
| No | 22 | 18% | 20 | 40% | ||||||||
| HIV RNA (log10 copies/mL) | 84 | 1.3 [1.3 to 1.3] | <0.01 | 0.1 | 0.0 to 0.8 | 0.03 | 79 | 1.3 [1.3 to 1.7] | 0.36 | 0.6 | 0.4 to 1.1 | 0.09 |
Comparison with patients without SVR.
Multivariate analysis.
IDU indicates injection drug use; NNRTI, nonnucleoside reverse transcriptase inhibitor; PI, protease inhibitor.
Potential confounders of the relation between CD4 cell count and SVR that we submitted to selection in the multivariate analysis were site, age, gender, HCV infection duration, ALT level, pegylated interferon dose, ART duration, presence of protease inhibitors in the ART regimen, nadir CD4 count, and HIV RNA level. Stepwise selection led to a final logistic regression model that included age, HIV RNA level, and ART duration. After controlling for these factors, CD4 count at treatment initiation ≥350 cells/mm3 was still not predictive of SVR (odds ratio adjusted [ORa] = 1.0; P = 0.98). Age, ART duration, and HIV RNA were significantly and inversely associated with SVR (see Table 2). The use of CD4 cell count as a continuous variable did not change the results (data not shown).
HCV Genotype Non-1
In patients with HCV genotype non-1 (n = 84), there was no significant difference in baseline characteristics between patients with a CD4 count <350 cells/mm3 or ≥350 cells/mm3, except for nadir CD4 cell count (see Table 1).
The SVR rate was 46% in patients with HCV genotype non-1. In univariate analysis, a higher METAVIR fibrosis score was the only significant predictive factor for SVR (see Table 2).
Potential confounders submitted to selection for the multivariate analysis were site, age, gender, BMI, mode of infection, HCV infection duration, ALT level, METAVIR fibrosis score, pegylated interferon dose, presence of a protease inhibitor in the ART regimen, nadir CD4 cell count, and HIV RNA level. Stepwise selection led to a final model that included METAVIR fibrosis score, and HIV RNA level. After controlling for these factors, the probability of SVR with a CD4 count ≥350 cells/mm3 was not significantly increased (ORa = 1.7, 95% confidence interval [CI]: 0.5 to 5.4). Using the formula of Zhang and Yu,23 the risk ratio was 1.3 (95% CI: 0.6 to 2.0). The METAVIR fibrosis score remained a significant predictor of SVR (ORa = 2.2; P < 0.01). There was a trend toward an association between HIV RNA level and SVR (ORa = 0.6; P = 0.09). The use of CD4 cell count as a continuous variable did not change the results (data not shown).
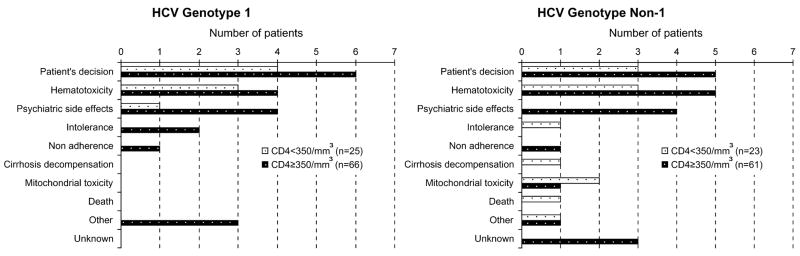
Causes of HCV Treatment Discontinuation
HCV treatment duration ranged from 1 to 84 weeks and was similar for patients with HCV genotype 1 and non-1 (median duration of 41 vs. 40 weeks, IQR: 26 to 50 weeks; P = 0.80). Of the 175 patients, 61 (35%) discontinued treatment prematurely. The most common reasons were patient decision (10%), hematologic toxicity (9%), and psychiatric side effects (5%). Treatment discontinuation attributable to patient decision was usually related to toxicity or other burdens of therapy that did not justify a treatment discontinuation from the physician’s perspective. In the group with HCV genotype non-1, discontinuation was more frequent in patients with a CD4 count <350 cells/mm3 than in others (52% vs. 33%; P = 0.03). There was no such difference in patients with HCV genotype 1 (32% vs. 30%; P = 0.92; Fig. 1).
FIGURE 1.
Treatment discontinuation causes, according to HCV genotype and CD4 cell count.
DISCUSSION
In this multicenter cohort study of pegylated interferon plus ribavirin combination therapy in 175 HIV/HCV-coinfected French patients, there was no clear relation between CD4 cell count at treatment initiation and SVR. In patients with HCV genotype 1 and in patients with HCV genotype non-1, a baseline CD4 count ≥350 cells/mm3 was not associated with SVR. In patients with HCV genotype 1, lower HIV RNA level, younger age, and shorter duration of ARTwere associated with a higher probability of SVR. In patients with HCV genotype non-1, a higher METAVIR fibrosis score was associated with a higher probability of SVR. Treatment discontinuation was frequent, especially in patients with HCV genotype non-1, when the baseline CD4 count was <350 cells/mm3.
The characteristics of this study population are similar to those of several cohorts from developed countries.2 Thus, this study is a good representation of HCV treatment in HIV/HCV-coinfected patients in a “real-life” clinical setting. The high prevalence of severe fibrosis at the time of treatment suggests that HCV treatment is often delayed and liver fibrosis progression is accelerated in HIV/HCV-coinfected patients. Eighty-one percent of patients were infected as a result of injection drug use, reflecting the shared routes of transmission of HIV and HCV.
Although guidelines generally recommend selecting patients for HCV treatment whose CD4 cell count is high, no study of pegylated interferon plus ribavirin to date has shown a significant association between CD4 cell count at treatment initiation and SVR.20 Because response rates are known to be significantly different by genotype, mechanisms and factors influencing treatment success might well be different in patients with HCV genotype 1 or non-1.6–13 In this case, SVR joint ORs would not allow for identification of predictive factors in these 2 subgroups. Therefore, we thought that it was important to stratify the analysis by HCV genotype, even at the expense of statistical power. This study is the first cohort study to address this question separately for HCV genotypes 1 and non-1. In patients with HCV genotype 1, we did not find a higher SVR rate when the baseline CD4 count was ≥350 cells/mm3, although power was limited, as demonstrated by the wide corresponding CI. In patients with HCV genotype non-1, CD4 cell count did not significantly predict SVR. Moreover, the risk ratio, a better estimate of the relative risk, argued for a lack of difference rather than a lack of statistical power. In exploratory analysis of the RIBAVIC trial, Carrat et al12 looked for SVR predictive factors in 125 patients with HCV genotype 1 or 4 and in 80 patients with HCV genotype 2, 3, or 5 treated with pegylated interferon plus ribavirin or with interferon plus ribavirin. The baseline CD4 cell count was not independently associated with SVR in either group of patients.
As for other potential SVR predictive factors, the only consistent factor associated with SVR in previous studies is HCV genotype. This study suggests an association between HIV RNA and decreased probability of SVR, regardless of genotype. We reported a negative influence of prolonged ART in patients with HCV genotype 1. These results support the hypothesis that long-lasting control of HIV viremia on ART increases HCV quasispecies diversity as a means for immune escape, and thus compromises SVR.24–26 Few studies have examined the impact of the use of HIV protease inhibitors on SVR, and results are discordant so far.6,12,27 This study does not argue for an effect of HIV protease inhibitors on anti-HCV therapy outcome. In patients with HCV genotype non-1 (but not in those with genotype 1), we found that the more advanced the liver fibrosis, the better was the chance of SVR. Even though the association between severity of liver fibrosis and SVR has not been consistently reported across studies, this result is not consistent with the concept that advanced fibrosis negatively affects the probability of SVR. Because there is no clear biologic argument to support this result, we hypothesize that it may be attributable to type 1 or α error.
The treatment discontinuation rate in our study was 35%, comparable to that seen in clinical trials (25% to 44%).6,7,11,12 Zinkernagel et al13 reported only 13% of premature discontinuations related to adverse events in the Swiss HIV Cohort Study, but intermittent treatment discontinuation of pegylated interferon or ribavirin was frequent (18% and 10%, respectively). In our study, premature discontinuations were more frequent with a baseline CD4 count <350 cells/mm3 only in patients with HCV genotype non-1. Treatment interruptions attributable to patient decision or hematologic toxicity, especially, were twice as common as with a baseline CD4 count ≥350 cells/mm3. These results suggest that better support of patients with a CD4 count <350 cells/mm3 might avoid some of the premature treatment discontinuations.
In contrast to clinical trials, our study design did not allow for random allocation of therapy with pegylated interferon plus ribavirin, but we did not find any significant difference in the baseline characteristics of patients with a CD4 count <350 cells/mm3 or ≥350 cells/mm3. We controlled for potential confounders in the multivariate analysis, but we cannot rule out residual confounding from unmeasured parameters such as alcohol consumption or the patient’s psychologic or socioeconomic status. In particular, we were not able to control for HCV RNA level, but this factor was not consistently independently associated with SVR in previous studies.6,9,11,12
This study suggests that initiation of anti-HCV therapy with pegylated interferon plus ribavirin in HIV/HCV-coinfected patients is possible without waiting for the patients to reach a high CD4 cell count on ART. Because premature treatment discontinuation attributable to patient decision or psychiatric side effects is frequent, other factors such as socioeconomic status, psychologic status, or active addictions might well be more important than the CD4 cell count for predicting SVR. Sustained support is needed to decrease the number of premature treatment interruptions.
Footnotes
This publication was made possible with help from the Recherche et Développement en Pathologie infectieuse et Tropicale, Association des Amis de la Faculté de Médecine de Nice, and the National Institute of Allergy and Infectious Diseases (P30 AI060354, K24 AI062476, and R01 AI42006).
References
- 1.Sherman KE, Rouster SD, Chung RT, et al. Hepatitis C Virus prevalence among patients infected with Human Immunodeficiency Virus: a cross-sectional analysis of the US Adult AIDS Clinical Trials Group. Clin Infect Dis. 2002;34:831–837. doi: 10.1086/339042. [DOI] [PubMed] [Google Scholar]
- 2.Rockstroh JK, Mocroft A, Soriano V, et al. Influence of hepatitis C virus infection on HIV-1 disease progression and response to highly active antiretroviral therapy. J Infect Dis. 2005;192:992–1002. doi: 10.1086/432762. [DOI] [PubMed] [Google Scholar]
- 3.Benhamou Y, Bochet M, Di Martino V, et al. Liver fibrosis progression in human immunodeficiency virus and hepatitis C virus coinfected patients. The Multivirc Group. Hepatology. 1999;30:1054–1058. doi: 10.1002/hep.510300409. [DOI] [PubMed] [Google Scholar]
- 4.Graham CS, Baden LR, Yu E, et al. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta-analysis. Clin Infect Dis. 2001;33:562–569. doi: 10.1086/321909. [DOI] [PubMed] [Google Scholar]
- 5.Verucchi G, Calza L, Manfredi R, et al. Human immunodeficiency virus and hepatitis C virus coinfection: epidemiology, natural history, therapeutic options and clinical management. Infection. 2004;32:33–46. doi: 10.1007/s15010-004-3063-7. [DOI] [PubMed] [Google Scholar]
- 6.Chung RT, Andersen J, Volberding P, et al. Peginterferon alfa-2a plus ribavirin versus interferon alfa-2a plus ribavirin for chronic hepatitis C in HIV-coinfected persons. N Engl J Med. 2004;351:451–459. doi: 10.1056/NEJMoa032653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Torriani FJ, Rodriguez-Torres M, Rockstroh JK, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med. 2004;351:438–450. doi: 10.1056/NEJMoa040842. [DOI] [PubMed] [Google Scholar]
- 8.Myers RP, Benhamou Y, Bochet M, et al. Pegylated interferon alpha 2b and ribavirin in HIV/hepatitis C virus-co-infected non-responders and relapsers to IFN-based therapy. AIDS. 2004;18:75–79. doi: 10.1097/00002030-200401020-00009. [DOI] [PubMed] [Google Scholar]
- 9.Moreno L, Quereda C, Moreno A, et al. Pegylated interferon alpha2b plus ribavirin for the treatment of chronic hepatitis C in HIV-infected patients. AIDS. 2004;18:67–73. doi: 10.1097/00002030-200401020-00008. [DOI] [PubMed] [Google Scholar]
- 10.Perez-Olmeda M, Nunez M, Romero M, et al. Pegylated IFN-alpha2b plus ribavirin as therapy for chronic hepatitis C in HIV-infected patients. AIDS. 2003;17:1023–1028. doi: 10.1097/00002030-200305020-00011. [DOI] [PubMed] [Google Scholar]
- 11.Laguno M, Murillas J, Blanco JL, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for treatment of HIV/HCV co-infected patients. AIDS. 2004;18:F27–F36. doi: 10.1097/00002030-200409030-00003. [DOI] [PubMed] [Google Scholar]
- 12.Carrat F, Bani-Sadr F, Pol S, et al. Pegylated interferon alfa-2b vs standard interferon alfa-2b, plus ribavirin, for chronic hepatitis C in HIV-infected patients: a randomized controlled trial. JAMA. 2004;292:2839–2848. doi: 10.1001/jama.292.23.2839. [DOI] [PubMed] [Google Scholar]
- 13.Zinkernagel AS, von Wyl V, Ledergerber B, et al. Eligibility for and outcome of hepatitis C treatment of HIV-coinfected individuals in clinical practice: the Swiss HIV Cohort Study. Antivir Ther. 2006;11:131–142. [PubMed] [Google Scholar]
- 14.Greub G, Ledergerber B, Battegay M, et al. Clinical progression, survival, and immune recovery during antiretroviral therapy in patients with HIV-1 and hepatitis C virus coinfection: the Swiss HIV Cohort Study. Lancet. 2000;356:1800–1805. doi: 10.1016/s0140-6736(00)03232-3. [DOI] [PubMed] [Google Scholar]
- 15.Piroth L, Duong M, Quantin C, et al. Does hepatitis C virus co-infection accelerate clinical and immunological evolution of HIV-infected patients? AIDS. 1998;12:381–388. doi: 10.1097/00002030-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Piroth L, Grappin M, Cuzin L, et al. Hepatitis C virus co-infection is a negative prognostic factor for clinical evolution in human immunodeficiency virus-positive patients. J Viral Hepat. 2000;7:302–308. doi: 10.1046/j.1365-2893.2000.00227.x. [DOI] [PubMed] [Google Scholar]
- 17.Lafeuillade A, Hittinger G, Chadapaud S. Increased mitochondrial toxicity with ribavirin in HIV/HCV coinfection. Lancet. 2001;357:280–281. doi: 10.1016/S0140-6736(00)03618-7. [DOI] [PubMed] [Google Scholar]
- 18.Moreno A, Quereda C, Moreno L, et al. High rate of didanosine-related mitochondrial toxicity in HIV/HCV-coinfected patients receiving ribavirin. Antivir Ther. 2004;9:133–138. [PubMed] [Google Scholar]
- 19.Opravil M, Sasadeusz J, Cooper D, et al. Effect of baseline CD4+ count on the efficacy and safety of peginterferon alfa-2a (40KD) (PEGASYS®) plus ribavirin (COPEGUS®) in HIV-HCV co-infection: the AIDS PEGASYS Ribavirin International Co-infection Trial (APRICOT). Presented at: 12th Conference on Retroviruses and Opportunistic Infections; Boston. 2005. [Google Scholar]
- 20.Soriano V, Puoti M, Sulkowski M, et al. Care of patients with hepatitis C and HIV co-infection. AIDS. 2004;18:1–12. doi: 10.1097/00002030-200401020-00001. [DOI] [PubMed] [Google Scholar]
- 21.Agher R, Duvivier C, Katlama C, et al. The NADIS cohort: 6236 HIV-infected patients followed up in French university hospitals [in French] Med Mal Infect. 2005;35:407–410. doi: 10.1016/j.medmal.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Pugliese P, Cuzin L, Enel P, et al. NADIS 2000, development of an electronic medical record for patients infected by HIV, HBV and HCV [in French] Presse Med. 2003;32:299–303. [PubMed] [Google Scholar]
- 23.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 24.Babik JM, Holodniy M. Impact of highly active antiretroviral therapy and immunologic status on hepatitis C virus quasispecies diversity in human immunodeficiency virus/hepatitis C virus-coinfected patients. J Virol. 2003;77:1940–1950. doi: 10.1128/JVI.77.3.1940-1950.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abbate I, Lo Iacono O, Di Stefano R, et al. HVR-1 quasispecies modifications occur early and are correlated to initial but not sustained response in HCV-infected patients treated with pegylated- or standard-interferon and ribavirin. J Hepatol. 2004;40:831–836. doi: 10.1016/j.jhep.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 26.Solmone M, Girardi E, Lalle E, et al. Evolution of HVR-1 quasispecies after 1-year treatment in HIV/HCV-coinfected patients according to the pattern of response to highly active antiretroviral therapy. Antivir Ther. 2006;11:87–94. [PubMed] [Google Scholar]
- 27.Poizot-Martin I, Marimoutou C, Benhaim S, et al. Efficacy and tolerance of HCV treatment in HIV-HCV coinfected patients: the potential interaction of PI treatment. HIV Clin Trials. 2003;4:262–268. doi: 10.1310/50jb-vnbb-7hrg-7gur. [DOI] [PubMed] [Google Scholar]