Abstract
Objective
To provide the current burden of high blood pressure and related risk factors in urban setting in Cameroon.
Methods
We used the WHO STEPS approach for Surveillance of non-communicable diseases and their risk factors to collect data from 2,559 adults aged 15–99 years, residing at Cite des Palmiers in Douala, Cameroon.
Results
The level of education was low with up to 60% of participants totalizing less than primary school. Smoking habits were 6 times more frequent in men (p<0.001) and 85% of participants reported alcohol consumption. Sedentary lifestyles at work and at leisure time were prevalent. Women displayed high prevalence of obesity in general. The mean blood pressure and the prevalence of hypertension increased with age in men and women. The prevalence of hypertension was 20.8%, and the risk of hypertension significantly increased with clustering of risk factors in the general population (p=0.001) and in men (p=0.008).
Conclusions
This study provides additional evidence on the growing problem of hypertension and related risk factors in urban Cameroon; and confirms the feasibility of using the WHO STEPS approach for the surveillance of NCDs in Africa. There is a need for rapid implementation of preventive strategies in the country.
Keywords: Hypertension, risk factors, non-communicable diseases, Africa, Cameroon
Introduction
Non-communicable diseases (NCDs), such as hypertension and other cardiovascular diseases are becoming increasingly important as causes of mortality and morbidity in all developing countries.1 In sub-Saharan Africa, communicable diseases continue to have the greatest disease burden but it is estimated that in the next few decades NCDs will outstrip communicable diseases as major cause of death.2 Even allowing for the uncertainties of predicting future disease patterns posed by the unfolding of the HIV epidemic in sub-Saharan Africa it is clear that the relative importance of NCDs will increase This is illustrated by a combination of demographic changes, increasing urbanization and associated changes in levels of risk factors like tobacco smoking, alcohol consumption, obesity and physical inactivity.3,4
Available evidence suggests that NCDs currently contribute substantially to the burden of mortality and morbidity in adults. Studies conducted in Cameroon in 1994 and 1998 showed that age, obesity and hypertension were significantly associated with hyperglycemia.5–7 In 1994 the prevalence rates of hypertension and diabetes in the adult population were respectively 8.3% and 1.1%. In 1998 these rates increased to 17.6% (hypertension) and 6.2% (diabetes) for urban men. These studies have highlighted the need, recognised by the Ministry of Health, for community-based studies to properly assess the mortality and morbidity due to non-communicable diseases in Cameroon. Recognising the increasing importance of these NCDs, the MOH in the year 2002 adopted a 10-year health development strategic plan in which the control of NCDs were given unprecedented consideration. However, the needs rapidly emerged for more evidence to back-up the ensuing national program for diabetes and hypertension.
It is against this background that this study was deemed necessary. The aim of the study was to generate larger scale scientific evidence that will contribute in influencing and guiding the development of a national policy for surveillance, prevention and control of hypertension and its risk factors in Cameroon.
Methods
Study population
The study population consisted of adult Cameroonians residing in Cité des Palmiers, one of the health districts of the city of Douala (the economic capital of Cameroon). Cité de Palmiers is an urban health district with a population of 247,730 inhabitants.
Sampling
Sample size
The WHO STEPS approach(8) for collecting surveillance data for non-communicable diseases was used to collect prevalence data for hypertension and their risk factors. In the context of this study, the sample size was calculated using the following criteria: desired precision: 1.5%; expected prevalence: 4% and design Effect: 3.75%; gave a sample size of 2460 subjects. From 15 to 64 years, the population was divided into ten-year age groups: 15 – 24; 25 – 34; 35 – 44; 45 – 54; 55 – 64 and 65+.
Sampling technique
The sampling scheme used was a multilevel systematic sampling stratified by age group. A census was conducted to map out the characteristics of the population of the health district, and identify households with adults aged 15 years and above. A household was defined as a group of people who share a common residence and partake in common meals. The total number of subjects within each age group was determined and used to calculate the percentage contribution of each age group to the total population. This percentage was then used to determine the percentage of households for each age group in which the census population is found. The number of households obtained for each age group was divided by 410 to obtain the sampling interval. The first household was selected randomly and individual age group sampling intervals were then used to obtain the households from which all the subjects were obtained. Only subjects who had resided in the catchments area for at least months were included in the household survey.
Data collection
Household questionnaire
The questionnaire was designed and adapted for use in Cameroon based on WHO STEPS instrument for NCD risk factors surveillance. The questionnaire was used to collect socio-economic and demographic data, knowledge of hypertension, and its risk factors, lifestyle, risk perception and behavior.
Data collection procedure
All data were collected by medical personnel who were specifically trained according to the methodology of the surveys, between March and April 2004. All respondents were interviewed using the household questionnaire. Anthropometric measures used standardized methods. Weight was measured using Seca® scales, height with calibrated adult Leicester® stadiometers, waist and hip circumferences with a constant tension tape at the level of the midpoint between the lower rib margin and the iliac crest on the mid-axillary plane (waist) and the protuberances of the great trochanters (hip). Blood pressure was recorded on the right arm in a seated subject after 10 minute rest, using an automated blood pressure device (OMRON® M4) and appropriate cuff sizes. The average of two measurements taken at two minutes interval was considered. Hypertension was defined as systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, or use of antihypertensive drugs irrespective of the blood pressure.
Ethical considerations
This study was approved by the National Research Ethical Committee, and informed consent was obtained from each subject prior to inclusion in the study. Confidentiality of all information obtained from respondents was assured by safely and securely storing the questionnaires. People diagnosed with hypertension were referred to the district hospital for follow-up.
Data management and analysis
Data entry was done using the data entry program developed for this purpose. All analyses were performed with the use STATA 6.0 software. Age specific prevalence was reported for each age group. Due to the complex sampling design of the survey, the overall proportions of hypertension and obesity were estimated taking the stratified sampling design into consideration. Proportional weights for each stratum were attributed according to the inverse of the probability of each individual observation in that age group of being sampled from the corresponding age group in the census population. The resulting weights were recorded in a new variable (weighting variable). In STATA 6, survey proportions were estimated using the svy commands after having set strata to age group and p weight (Proportional weight) to the weighting variable. Comparison of qualitative data was done using the Chi square test. A p-value <0.05 was considered significant.
Results
General characteristics of the study population
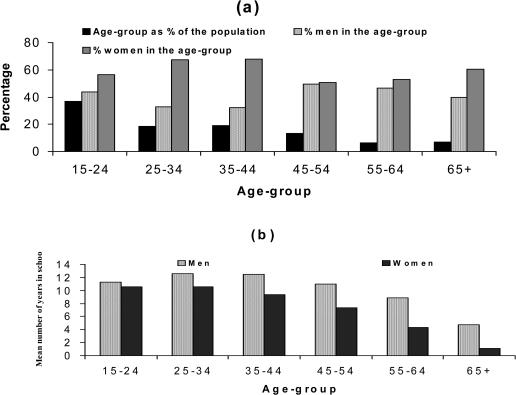
A total of 2,559 individuals, aged 15 to 99 years, from households, participated in the study. The mean number of subjects per household was 3. There were 40.3% of men and 59.7% women (figure 1). The non-response rate was 7.5%. Travelling out of the district, religious group, major illnesses were the main reason for non-participating. The age group 15–24 years was the most represented (36.6%). Apart from the age-groups 15–24 and 55–64 years, the mean age between men and women within age-groups was not different (figure 1a). The majority of participants performed house duties (28.1%), followed by students (21.4%) and self-employed individuals (19.6%). The level of education of the respondents was low with up to 60% totalizing either no formal schooling, less than primary or only primary school. Generally, women were less educated than men, P<0.001 at all age groups (figure 1b).
Figure 1.
Distribution of participants (a) and mean number of years schooling (b) by age group
Tobacco consumption
The adjusted prevalence of tobacco consumption was reported by 16% of participants. Smoking habit was 5 to 6 times more frequent in men than women (p<0.001). Daily smokers represented 77% of actual smokers. Daily smokers represented 5% of the general population, 10% of the male population and 1.5% of the female population. Manufactured cigarettes represent 96% of all the products smoked.
Alcohol consumption
Up to 85% of the respondents reported to have taken at least an alcoholic drink during the last 12 months (89 % and 82% for men and women respectively). The mean number of alcoholic drink per day was 2.50 for men and 1.73 for women (p<0.001). Sixty-three percent of men reported drinking more than 5 days per week, against 37% of women. Beer represented 94% of all the types of alcoholic drinks. The rest was represented by wine (2.2%), spirit (0.6%) and traditional alcoholic beverages.
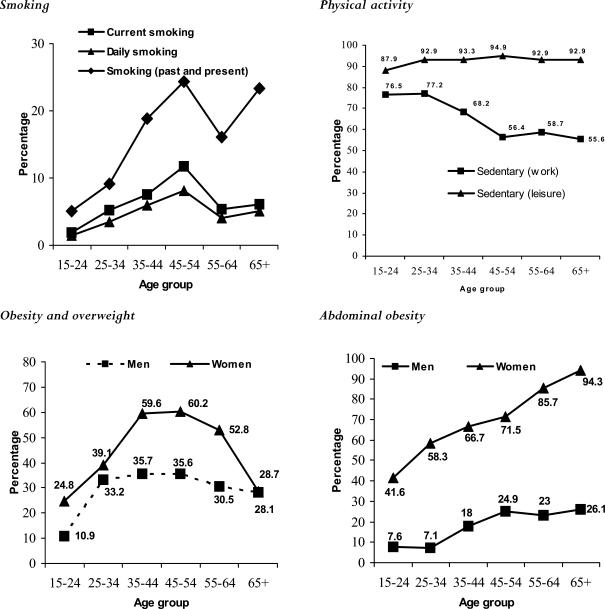
Physical activity
Physical activity was assessed at work place and during leisure time. Irrespective of the age group, most participants (79.6%) were sedentary at work and up to 91.5% of them reported no physical activity at leisure time. The analysis of the physical activities related to transport patterns revealed that almost all the respondents spent at least 1 hour per day to and from work. The intensity of physical effort in active subjects both at leisure and at work decreased with age (figure 2).
Figure 2.
Distribution of selected risk factors by age groups
Nutrition
In general, respondents consume fruits on average of two days per week though at very small quantities. Most of the respondents ate vegetables 3 days per week on an average. 49% of subjects reported cooking with palm oil, 9.1% with ground nut, cotton or Soya bean oil. The remaining 49.5% combined palm and ground nut oil. Young participants tended to use more sugar while adding salt in meal was more frequent in aged people.
Obesity
Apart from the age groups 25–34 and 65+, the mean BMI was significantly higher for women compared to men across age-groups (p<0.01). The standardized prevalence of overweight (25Kg/m2≤BMI<30Kg/m2) and obesity (BMI≥30Kg/m2) was respectively 23.8% and 11.1% for the study population, 23.7% and 7.5% for men, and 28.8% and 21.2% for women. Abdominal obesity was present in 14% of men and 59.5% of women. The distribution of overweight, obesity and abdominal obesity is displayed in figure 2.
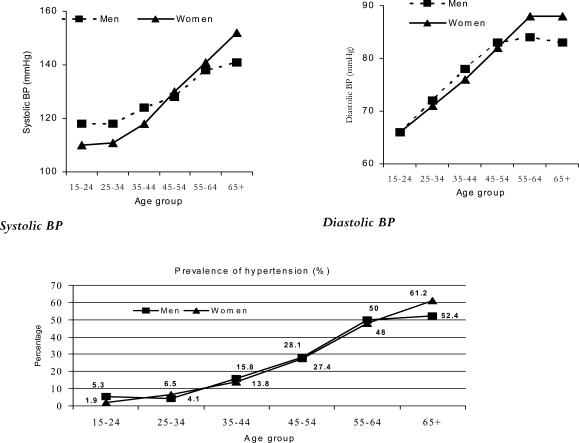
Prevalence of hypertension
The number of hypertensives identified during the survey was 377, giving an estimated prevalence of 8.9% (95%CI 5.1–12.5). This prevalence greatly varied according to sex and age group, and 50% of males or females above 55 years old had high blood pressure. After adjusting for age, using the WHO New World Population, this prevalence was 20.8% (95%CI 19.1–22.5) Figure 3 presents the gender specific distribution of hypertension by age groups.
Figure 3.
Gender-specific distribution of systolic, diastolic blood pressure (mean values) and prevalence of hypertension by age groups.
Clustering of hypertension and risk factors
Odds ratios and 95% confidence intervals for the association between hypertension and individual risk factors are described in Table 1. We further assess the association of high blood pressure and clustering of risk factors. As displayed in Table 2, the age adjusted odds ratio for hypertension gradually increased with the number of risk factors both in men, women and the study population as a group. This trend was significant for the whole population (p = 0.001) and men taken separately (p = 0.008). However, between 3 and four risk factors' clusters, there was a reverse trend. Similar trends were observed in each age stratum taken separately, but did not reach significance at any of the strata considered (data not shown).
Table 1.
Age adjusted odds ratios for hypertension according to the number of risk factors in the study population
| Number of risk factors | N | OR (95% CI) | P |
| No risk factor | 434 | 1 | |
| One risk factor | 866 | 1.2 (0.8 – 1.9) | 0.3 |
| Two risk factors | 739 | 1.6 (1.0 – 2.4) | 0.03 |
| Three risk factors | 174 | 2.9 (1.7 – 4.9) | 0.0001 |
| Four risk factors | 8 | 1.4 (0.4 – 5.7) | 0.6 |
| P | 0.001 |
Table 2.
Univariate and multivariate analysis between hypertension and common risk factors
| Variables | Univariate analysis | Multivariate analyses | ||
| OR (95% CI) | p | OR (95% CI) | p | |
| Age (years) | 1.08 (1.07–1.09) | 0.001 | 1.08 (1.07–1.09) | 0.001 |
| Alcohol consumption | 2.20 (1.71–3.05) | 0.001 | 1.09 (0.80–1.49) | 0.5 |
| Tobacco smoking | 1.72 (1.20–2.48) | 0.005 | 1.18 (0.83–1.66) | 0.9 |
| Obesity | 2.43 (1.87–3.16) | 0.001 | 1.87 (1.39–2.47) | 0.001 |
| Sedentarity | 1.51 (0.90–2.50) | 0.1 | 1.21 (0.83–1.76) | 0.3 |
Risks factors
Tobacco smoking: Current smokers versus ex and non smokers. Alcohol consumption: Current drinkers versus ex and non drinkers. Obesity: Normal weight + underweight versus overweight + obese Sedentarity: First uartile versus 2nd to 4th quartile. Age: continuous.
Discussion
This study provides the current prevalence of high blood pressure and selected risk factors in Douala. The large number of people involved and the standardized methodology used ensures the high quality of the data collected and a high accuracy in the estimation of the prevalence of hypertension. In our study, hypertension was associated with known risk factors like age, obesity, low physical activity and positive family history of hypertension. The findings of this study bring out the high prevalence of hypertension and its related risk factors in the urban adult population of Cameroon. This high prevalence of hypertension and its risk factors, associated with aging of the population will result to an increase in the number of patients in the very near future, adding a heavy burden to an already overloaded health system, if nothing is done.
Although comparison of these results with previous surveys is difficult, because they used different methodologies, there are some evidences suggesting the increase in the prevalence of hypertension in Cameroon. In 1994, Cooper et al9 reported an age-standardized prevalence of 19.1% among Cameroonian adults aged 25 and above, based on a single blood pressure measurement. In 1998, Mbanya et al6 reported an age standardized urban prevalence of hypertension of 16.4% and 12.1% in males and females respectively, based on WHO Criteria (160/95 mmHg) with 3 blood pressure measurements. The prevalence of hypertension in Cameroon, as estimated by this study and that of CamBoD Baseline Survey10 was higher than these previous figures and even higher than that of some developing and developed countries. Comparing the prevalence of hypertension between Cameroon, Egypt11, China12 and the USA13 revealed that, for the age groups 35–44, 45–54, and 55–64, Cameroon has the highest prevalence of hypertension in age group 35–44 years and 55–64. The high prevalence observed in Douala, similar to those of developing countries may be explained by the increase in risk factors resulting from changes in lifestyle, diet, economic development and increase in life expectancy. This hypothesis is suggested by findings in this study, and in others14, of a marked difference between hypertensive and non-hypertensive subjects in the prevalence of known risk factors for hypertension and its complication.
Many authors have described the situation of hypertension in Africa from various perspectives but the underlying fact is that it is an emerging public health problem throughout the continent. Hypertension is the most common cardiovascular condition in the world. It is a strong independent risk factor for death from heart diseases and stroke. It is also a common clinical condition affecting more than 900 million persons worldwide and seen in nearly all populations.15 Although reliable, large-scale, population-based data on high blood pressure in sub-Saharan Africa (SSA) are limited, recent studies provide important and worrisome findings in both epidemiology and clinical outcomes. Although enormous challenges still persist in the control of infectious diseases in sub-Saharan Africa, the emergence of noncommunicable diseases has added the threats to the health of adult Africans16. In most SSA settings, hypertension control assumes a relatively low priority and little experience exists in implementing sustainable and successful programs for drug treatment. Rapid urbanization and transition from agrarian life to the wage-earning economy of city life continue to fuel increases in average blood pressure levels and prevalence of hypertension. Although the true burden of high blood pressure in sub-Saharan Africa remains largely unmeasured, compelling preliminary evidence suggests that it is the foundation for epidemic cardiovascular disease in Africa and already contributes substantively to death and disability from stroke, heart failure, and kidney failure in this region.17 There is all evidence that Africa is undergoing an epidemiological transition for NCDs, especially hypertension.18
Limitations
Having to examine over 2500 subjects using more than 10 field staff in a socio-cultural heterogeneous community, using a variety of methods could not be hitch free. The sample size per age group required an estimate of at least 410 subjects. This size could not be reached for the 65 years and above age group. This was due to the natural demographic structure of the population, of which, the total number of subjects within this age group, living in the catchments health area was not up to 410.
Conclusion
The current work, conducted in Douala , the main city in Cameroon, confirms the high prevalence of hypertension in urban Sub-Saharan Africa and highlights the urgent need to implement at primary care level both community and health facility-based, cost-affective strategies, targeting risk factors, community awareness and management of this condition by health professionals. There is also a need for greater epidemiological studies into monitoring the trends of hypertension and related risk factors, as well as outcomes, both fatal and non-fatal.
Acknowledgments
We are grateful to Dr. Joseph Shu and Emmanuel Kiawi for their contribution to the initial phase of this research and thank the population of Cité des Palmiers for taking part in this study.
References
- 1.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349(9063):1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 2.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97(6):596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: Part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104(23):2855–2864. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman JS, Owoaje EE, Rotimi CN, Cooper RS. Blood pressure change in Africa: case study from Nigeria. Hum Biol. 1999;71(4):641–657. [PubMed] [Google Scholar]
- 5.Mbanya JC, Ngogang J, Salah JN, Minkoulou E, Balkau B. Prevalence of NIDDM and impaired glucose tolerance in a rural and an urban population in Cameroon. Diabetologia. 1997;40(7):824–829. doi: 10.1007/s001250050755. [DOI] [PubMed] [Google Scholar]
- 6.Mbanya JC, Minkoulou EM, Salah JN, Balkau B. The prevalence of hypertension in rural and urban Cameroon. Int J Epidemiol. 1998;27(2):181–185. doi: 10.1093/ije/27.2.181. [DOI] [PubMed] [Google Scholar]
- 7.Sobngwi E, Mbanya JC, Unwin NC, et al. Physical activity and its relationship with obesity, hypertension and diabetes in urban and rural Cameroon. Int J Obes Relat Metab Disord. 2002;26(7):1009–1016. doi: 10.1038/sj.ijo.0802008. [DOI] [PubMed] [Google Scholar]
- 8.Ng N, Stenlund H, Bonita R, Hakimi M, Wall S, Weinehall L. Preventable risk factors for noncommunicable diseases in rural Indonesia: prevalence study using WHO STEPS approach. Bull World Health Organ. 2006;84(4):305–313. doi: 10.2471/blt.05.023721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper R, Rotimi C, Ataman S, et al. The prevalence of hypertension in seven populations of west African origin. Am J Public Health. 1997;87(2):160–168. doi: 10.2105/ajph.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamadjeu RM, Edwards R, Atanga JS, Unwin N, Kiawi EC, Mbanya JC. Prevalence, awareness and management of hypertension in Cameroon: findings of the 2003 Cameroon Burden of Diabetes Baseline Survey. J Hum Hypertens. 2006;20(1):91–92. doi: 10.1038/sj.jhh.1001936. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim MM. The Egyptian National Hypertension Project (NHP): preliminary results. J Hum Hypertens. 1996;10(Suppl 1):S39–S41. [PubMed] [Google Scholar]
- 12.Gu D, Reynolds K, Wu X, et al. Prevalence, awareness, treatment, and control of hypertension in china. Hypertension. 2002;40(6):920–927. doi: 10.1161/01.hyp.0000040263.94619.d5. [DOI] [PubMed] [Google Scholar]
- 13.Wolz M, Cutler J, Roccella EJ, Rohde F, Thom T, Burt V. Statement from the National High Blood Pressure Education Program: prevalence of hypertension. Am J Hypertens. 2000;13(1 Pt 1):103–104. doi: 10.1016/s0895-7061(99)00241-1. [DOI] [PubMed] [Google Scholar]
- 14.Edwards R, Unwin N, Mugusi F, et al. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens. 2000;18(2):145–152. doi: 10.1097/00004872-200018020-00003. [DOI] [PubMed] [Google Scholar]
- 15.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 16.Forrester T, Cooper RS, Weatherall D. Emergence of Western diseases in the tropical world: the experience with chronic cardiovascular diseases. Br Med Bull. 1998;54(2):463–473. doi: 10.1093/oxfordjournals.bmb.a011701. [DOI] [PubMed] [Google Scholar]
- 17.Cooper RS, Amoah AG, Mensah GA. High blood pressure: the foundation for epidemic cardiovascular disease in African populations. Ethn Dis. 2003;13(2 Suppl 2):S48–S52. [PubMed] [Google Scholar]
- 18.Unwin N. Non-communicable disease and priorities for health policy in sub-Saharan Africa. Health Policy Plan. 2001;16(4):351–352. doi: 10.1093/heapol/16.4.351. [DOI] [PubMed] [Google Scholar]