Abstract
Objective
To examine whether use of multivitamins and intake of specific nutrients in multivitamins is associated with ovulatory infertility.
Design and Setting
The Nurses’ Health Study II, a prospective cohort study.
Participants
18,555 married, pre-menopausal women without a history of infertility who attempted a pregnancy or became pregnant between 1991 and 1999.
Main outcome measures
Incident reports of infertility due to anovulation.
Results
During 8 years of follow-up 438 women reported infertility due to ovulatory disorder. There was an inverse association between frequency of multivitamin use and ovulatory infertility. The multivariate-adjusted relative risk (95% confidence interval) of ovulatory infertility was 0.88 (0.60, 1.28) for women consuming 2 tablets/week or less, 0.69 (0.51, 0.95) for women consuming 3 to 5 tablets/week and 0.59 (0.46, 0.75) for women consuming 6 or more tablets/week, when compared to women who did not use these supplements (P, trend <0.001). Folic acid appeared to explain part of the association between multivitamin supplement use and risk of ovulatory infertility.
Conclusions
Regular use of multivitamin supplements may decrease the risk of ovulatory infertility.
Keywords: Infertility, ovulation, multivitamins, folic acid, epidemiology, reproductive medicine
INTRODUCTION
Infertility is a common condition affecting as many as one out of six couples during their lifetime (1). Some authors have proposed that the already high frequency of this disorder is likely to rise as the postponement of childbearing increases, particularly in developed regions of the world (2, 3). Assisted reproductive technologies are the main strategy used to control the burden of infertility. However, their large costs (4, 5) and frequency of adverse events (6–10) warrant the consideration of alternative approaches to control infertility including prevention.
The role of dietary factors in human fertility has not been investigated in detail, but intake of some micronutrients may enhance female fertility. Previous studies have documented higher pregnancy rates among users of micronutrient supplements either with (11) or without (12) fertility disorders. Although these studies could not identify specific nutrients or mechanisms explaining the beneficial effect of these supplements, recent findings suggest that folate status may be important in the ovarian response to FSH (13). Therefore, we evaluated whether use of multivitamin supplements was associated with the incidence of ovulatory disorder infertility and explored which nutrients could explain the association if it existed.
MATERIALS AND METHODS
Study Population
The Nurses’ Health Study II is a prospective cohort study designed to investigate the role of diet and other lifestyle factors in common chronic diseases. In 1989, 116,671 female registered nurses ages 24 to 42 were enrolled in the study and have been followed every two years since then with mailed questionnaires. Here we present a prospective analysis of incident ovulatory infertility among participants of this cohort. The study was approved by the Institutional Review Board of Brigham and Women’s Hospital. None of the authors have conflicts of interest with the material presented in this manuscript, financial or otherwise.
Follow-up for the current study started in 1991, when diet was first measured, and concluded in 1999. On biennial questionnaires participants were asked if they had tried to become pregnant for more than 1 year without success since the previous questionnaire administration, and to indicate whether their inability to conceive was caused by tubal blockage, ovulatory disorder, endometriosis, cervical mucous factor, spousal factor, was not found, was not investigated or was caused by other reason. In a validation study among members of this cohort not included in the present analyses, self-reported diagnosis of ovulatory infertility was confirmed by review of medical records in 95% of the cases (14). Self-reports of infertility of women in the current analysis were not confirmed by review of medical records. Women were also asked if they became pregnant during the preceding two-year period, including pregnancies resulting in miscarriages or induced abortions. Using this information we simulated a cohort of women attempting to become pregnant. Only married women, with available dietary information and without a history of infertility, were eligible to enter the analysis. These women contributed information to the analysis during each two-year period in which they reported a pregnancy or a failed pregnancy attempt, and were followed until they reported an infertility event from any cause, reached menopause or underwent a sterilization procedure (themselves or their partner), whichever came first. Only 10 diabetic women met these criteria. Because insulin resistance and hyperinsulinemia, hallmark characteristics of type 2 diabetes, may affect ovulatory function (15), we excluded these 10 women from the analysis. After exclusions, we identified 18,555 women without a history of infertility who tried to become pregnant or became pregnant during the 8-year follow-up period. In each two-year period, women who met these criteria and reported infertility due to ovulatory disorder were considered cases and the remaining women were considered non-cases.
Dietary information was collected in 1991 and 1995 using a previously validated food-frequency questionnaire (FFQ) (16–18). Participants were asked to report how often, on average, they consumed each of the foods and beverages included in the FFQ during the previous year. The questionnaire offered nine options for frequency of intake, ranging from never or less than once per month to six or more times per day. Participants were also asked whether they used multivitamin supplements and other nutrient supplements. Multivitamin users were asked to specify the brand of the multivitamin and its frequency of use. Women were also asked to report the use of several commonly used supplements of specific vitamins; those reporting use were asked to specify the daily dose. Nutrient intakes were estimated by summing the nutrient contribution of all food items in the questionnaire, taking into consideration the brand, type and dose of dietary supplements used. The nutrient content of each food and specified portion size was obtained from a nutrient database derived from the US Department of Agriculture (19) and additional information obtained from food manufacturers. To reduce extraneous variation in nutrient intakes, nutrient intakes were adjusted for total energy intake using the nutrient residual method (20).
Statistical analyses
The relative risk (calculated as an odds ratio) of ovulatory infertility according to categories of multivitamin supplement use and intake of B-vitamins was estimated using logistic regression. The generalized estimating equation approach (21) with an exchangeable working correlation structure, was used to account for the within-person correlation in outcomes at different time periods. Women were initially divided into users and non-users of multivitamins according to their most recent dietary assessment. Multivitamin users were further divided into 4 categories according to their frequency of use: ≤ 2 tablets/week, 3 – 5 tablets/week, ≥ 6 tablets/week, and those who did not provide a frequency of use. The relative risk of ovulatory infertility was computed as the risk among women in a specific level of supplement use divided by the risk among non-users. Women were also divided into five groups according to quintiles of intake of individual B vitamins (B1, B2, B6, B12, folic acid, niacin and pantothenic acid). In these models, the relative risk was computed as the risk of infertility in a specific quintile of cumulative averaged intake (22) compared to the risk in the lowest quintile. Tests for linear trend were conducted by using the median values of intake in each category as a continuous variable.
To control for confounding by age and take into account potential time trends in infertility (23), all models were adjusted for age in years at the beginning of each mailing cycle and calendar time of the current questionnaire cycle. Multivariate models included additional terms for BMI, parity, smoking history, physical activity, history of oral contraceptive use, dietary factors found to be related to infertility in preliminary analyses (intakes of alcohol, coffee, protein and major types of fatty acids) and total energy intake. Multivariate models for intake of B-vitamins were further adjusted for iron intake. The values of the dietary and non-dietary variables were updated as new data became available.
We performed additional analyses to assess what components of multivitamins were responsible for the association between this supplement and ovulatory infertility. First, we identified the nutrients for which multivitamins are the main source in this population and introduced them, one at a time, into the multivariate models including multivitamins. Then, we examined the association between long term intake of B-vitamins and ovulatory infertility, with and without adjustment for multivitamin use, and among non-users of multivitamins.
We examined whether the association between the use of multivitamin supplements and ovulatory infertility was modified by subject characteristics (age, parity and BMI), the presence of long menstrual cycles (≥40 days), alcohol intake or use of iron supplements by introducing cross-product terms between use of multivitamin supplements and the variable of interest.
The population attributable risk (PAR) and its 95% confidence interval (CI) (24) was used to estimate the proportion of ovulatory infertility cases within this cohort that could have been avoided had all women consumed multivitamins at certain frequencies, assuming that the association between multivitamins and ovulatory infertility is causal. Analyses were performed in SAS version 9.1.
RESULTS
During 8 years of follow-up, 26,971 eligible pregnancies and pregnancy attempts were accrued among 18,555 women. Of these events, 3,430 were incident reports of infertility from any cause, of which 2,165 were of women reporting at least one diagnosis for infertility and 438 (20% of women that reported a specific diagnosis) were incident reports of ovulatory infertility. Women reporting ovulatory infertility were more than 4 times more likely to report long and irregular menstrual cycles or clinical signs of excess androgens when compared to women reporting infertility due to other causes (OR [95% CI] = 4.15 [2.98 – 5.76]) or when compared to women who became pregnant during follow-up (OR [95% CI] = 4.43 [3.35 – 5.86]).
At baseline, women differed on several characteristics based on their use of multivitamin supplements (Table 1). Multivitamin users tended to consume less alcohol and coffee, to smoke less and to be more physically active than non-users. Also, multivitamin users were less likely to be users of hormonal contraception or intrauterine devices at the beginning of the first two-year period where they reported an eligible event. Frequency of multivitamin use was strongly correlated with the total intake (diet plus supplements) of specific B-vitamins. The Spearman correlation coefficients between intake of B-vitamins and multivitamin use frequency were 0.79 for B-1, 0.78 for B-2, 0.77 for B-6, 0.67 for B-12, 0.81 for folic acid, 0.76 for niacin and 0.58 for pantothenic acid.
Table 1.
Baseline characteristics * of users and non-users of multivitamin supplements.
| Characteristic | Multivitamins |
|
|---|---|---|
| Users N=10451 | Non-Users N=8104 | |
| Age, years | 32.5 | 32.6 |
| Alcohol intake, g/day | 2.7 | 3.1 |
| Coffee intake ≥ 2 cups/day. % | 21 | 28 |
| Current smoker, % | 6 | 9 |
| Body Mass Index, kg/m2 | 23.9 | 23.9 |
| Physical activity, METs/week | 22 | 20 |
| Cycles ≥ 40 days, % | 3 | 3 |
| Hyperandrogenism, % | 0.3 | 0.3 |
| Nulliparous, % | 23 | 24 |
| Contraceptive use †, % | ||
| Oral contraceptives | 12 | 22 |
| Other hormonal contraceptive ‡ | 0.1 | 0.3 |
| Intrauterine devices | 1 | 1.6 |
| Two or more contraceptives | 12 | 12 |
Baseline refers to the year of entry into the study for each individual. Values are presented as age-standardized means and proportions with the exception of values for age.
Two years before the first event was reported
Injectable or implantable progestins.
In analyses adjusted for age and calendar time, use of multivitamin supplements was associated with a decreased risk of ovulatory infertility in a dose-dependent manner (Table 2). Multivitamin users had approximately one-third lower risk of developing ovulatory infertility when compared to non-users (p<0.001). When multivitamin users were grouped by their frequency of use, those consuming no more than two multivitamin tablets per week did not have a significantly different risk compared to women who did not use multivitamins, whereas women who consumed 3 or more tablets per week had a significantly reduced risk of ovulatory infertility. In addition, there was a linear trend towards decreased ovulatory infertility risk with increasing frequency of multivitamin supplement use. We considered multiple known and suspected risk factors for infertility as potential confounders for the observed association. Simultaneously adjusting for these factors changed the age-adjusted results minimally (Table 2). We estimate that 20% of ovulatory infertility cases could be avoided if women consumed 3 or more multivitamins per week (PAR [95% CI] = 20% [11% – 28%]), assuming this association is causal.
Table 2.
Relative Risks (RR) and 95% confidence intervals (CI) for ovulatory infertility by categories of multivitamin supplement use.
| Cases / Non-cases * | Age-Adjusted † RR (95% CI) | Multivariate-Adjusted ‡ RR (95% CI) | |
|---|---|---|---|
| Multivitamin Use | |||
| Non Users | 224 / 10,926 | 1.00 (referent) | 1.00 (referent) |
| Users | 214 / 15,607 | 0.67 (0.55, 0.80) | 0.65 (0.53, 0.80) |
| Frequency of use | |||
| Non Users | 224 / 10,926 | 1.00 (referent) | 1.00 (referent) |
| ≤ 2 tablets/wk | 32 / 1,808 | 0.84 (0.58, 1.23) | 0.88 (0.60, 1.28) |
| 3 – 5 tablets/ wk | 52 / 3,796 | 0.66 (0.49, 0.90) | 0.69 (0.51, 0.95) |
| ≥ 6 tablets/ wk | 127 / 9,783 | 0.63 (0.51, 0.79) | 0.59 (0.46, 0.75) |
| P trend § | <0.001 | <0.001 | |
223 multivitamin users (3 cases and 220 non-cases) did not provide information about the frequency of multivitamin use.
Adjusted for age (continuous) and calendar time (4 two-year intervals).
Age adjusted model further adjusted for total energy intake (continuous), body mass index (<20, 20–24.9, 25–29.9, ≥30 and missing), parity (0, 1, ≥2 and missing), smoking history (never, past 1–4 cig/day, past 5–14 cig/day, past 15–24 cig/day, past ≥ 25 cig/day or unknown amount, current 1–4 cig/day, current 5–14 cig/day, current 15–24 cig/day and current ≥ 25 cig/day or unknown amount), physical activity (<3 MET-h/wk, 3–8.9 METh/wk, 9–17.9 MET-h/wk, 18–26.9 MET-h/wk, 27–41.9 MET-h/wk, ≥ 42 MET-h/wk and missing), contraceptive use (current user, never user, past user 0–23 months ago, past user 24–47 months ago, past user 48–71 months ago, past user 72–95 months ago, past user 96–119 months ago, past user ≥ 120 months ago and missing), and intakes of alcohol (no intake, < 2 g/day, 2–4.9 g/day, ≥ 5 g/day), coffee (<1 serving/month, 1 serving/month, 2–6 servings/week, 1 serving/day, 2–3 servings/day, ≥ 4 servings/day), major types of fatty acids and protein.
Calculated with the median frequency of use in each category as a continuous variable.
Since multivitamin use was associated with lower use of contraception and multivitamin use may be higher among women planning a pregnancy, we performed two sensitivity analyses. We first restricted the analysis to non-contracepting women and then conducted a case-control analysis using women diagnosed with infertility due to other causes as controls. Among women who were not using any type of contraception, the multivariate-adjusted relative risk (RR) and 95% confidence interval (CI) comparing all users of multivitamins with non-users was 0.46 (0.35, 0.61). Among these women there was also a linear trend towards decreasing ovulatory infertility with increasing frequency of multivitamin use (Table 3). The results were similar when the analyses were restricted to women not using specific types of contraception. In the case-control analysis, the multivariate-adjusted RR (95% CI) of ovulatory infertility comparing all users of multivitamins with non-users was 0.77 (0.62, 0.95) and there was a linear trend towards decreased risk of ovulatory infertility with increased frequency of multivitamin use (p, trend = 0.04).
Table 3.
Multivariate adjusted relative risks of ovulatory infertility by frequency of multivitamins among non-users of contraception.
| Frequency of Multivitamin Use |
|||||
|---|---|---|---|---|---|
| Subgroup | Never | ≤ 2 /wk | 3 – 5 / wk | ≥ 6 / wk | P trend * |
| All participants | |||||
| Cases / non-cases | 224 / 10,926 | 32 / 1,808 | 52 / 3,796 | 127 / 9,783 | |
| Relative risk (95% CI) † | 1.00 (referent) | 0.88 (0.60, 1.28) | 0.69 (0.51, 0.95) | 0.59 (0.46, 0.75) | <0.001 |
| Not using any contraceptive method | |||||
| Cases / non-cases | 128 / 3,872 | 16 / 667 | 25 / 1,548 | 71 / 4,997 | |
| Relative risk (95% CI) † | 1.00 (referent) | 0.72 (0.42, 1.24) | 0.50 (0.32, 0.78) | 0.41 (0.29, 0.56) | <0.001 |
| Not using hormonal contraception ‡ | |||||
| Cases / non-cases | 184 / 8,760 | 25 / 1,524 | 49 / 3,251 | 113 / 8,822 | |
| Relative risk (95% CI) † | 1.00 (referent) | 0.80 (0.52, 1.22) | 0.75 (0.54, 1.04) | 0.57 (0.44, 0.73) | <0.001 |
| Not using barrier methods § | |||||
| Cases / non-cases | 172 / 6,355 | 23 / 998 | 29 / 2,201 | 88 / 6,190 | |
| Relative risk (95% CI) † | 1.00 (referent) | 0.82 (0.53, 1.29) | 0.49 (0.33, 0.73) | 0.49 (0.37, 0.65) | <0.001 |
Calculated with the median frequency of use in each category as a continuous variable.
Adjusted for age (continuous), calendar time (4 two-year intervals), total energy intake (continuous), body mass index (<20, 20–24.9, 25–29.9, ≥30 and missing), parity (0, 1, ≥2 and missing), smoking history (never, past 1–4 cig/day, past 5–14 cig/day, past 15–24 cig/day, past ≥ 25 cig/day or unknown amount, current 1–4 cig/day, current 5–14 cig/day, current 15–24 cig/day and current ≥ 25 cig/day or unknown amount), physical activity (<3 MET-h/wk, 3–8.9 MET-h/wk, 9–17.9 MET-h/wk, 18–26.9 MET-h/wk, 27–41.9 METh/wk, ≥ 42 MET-h/wk and missing), and intakes of alcohol (no intake, < 2 g/day, 2–4.9 g/day, ≥ 5 g/day), coffee (<1 serving/month, 1 serving/month, 2–6 servings/week, 1 serving/day, 2–3 servings/day, ≥ 4 servings/day) major types of fatty acids and protein. The model including all participants regardless of recent contraception also includes terms for recency of contraceptive use (current user, never user, past user 0–23 months ago, past user 24–47 months ago, past user 48–71 months ago, past user 72–95 months ago, past user 96–119 months ago, past user ≥ 120 months ago and missing).
Oral contraceptives and injected or implantable progestins
Condoms, diaphragms or cervical caps.
Because multivitamins are the most important contributor to the intake of numerous micronutrients in the study population, we evaluated which of these nutrients might be responsible for the observed association. First, we added one at a time the total intake (diet and supplements) of each of these nutrients (iron, magnesium, zinc, copper, manganese, folic acid, niacin, pantothenic acid, retinol and vitamins B-1, B-2, B-6, B-12, C, D and E) to the final multivariate-adjusted models for multivitamin supplements among the entire study population and observed whether their inclusion attenuated the association between multivitamins and ovulatory infertility. In the models comparing multivitamin non-users to users according to the frequency of use, adding intakes of folic acid, iron, vitamins B-1, B-2 and D attenuated the association between multivitamins and ovulatory infertility. The multivariate-adjusted RRs (95% CIs; p, trend) comparing women using 6 or more multivitamins per week to non users were 0.59 (0.46, 0.75; <0.001) in the initial model without added nutrients, 0.74 (0.54, 1.00; 0.05) after adjusting for iron intake, 0.70 (0.48, 1.02; 0.08) after adjusting for vitamin D intake, 0.70 (0.44, 1.09; 0.11) after adjusting for vitamin B-1 intake, 0.68 (0.45, 1.03; 0.08) after adjusting for vitamin B-2 intake and 0.88 (0.58, 1.32; 0.59) after adjusting for folic acid intake. Adjustment for the remaining micronutrients considered did not affect the association (data not shown).
Since the previous analysis suggested that some B vitamins might mediate the association between multivitamin supplements and ovulatory infertility we then examined whether long term intake of individual B vitamins was associated with the risk of developing ovulatory infertility. In age and energy-adjusted analyses, intakes of vitamins B-1, B-2, B-6, B-12, folic acid and niacin were inversely related to the risk of ovulatory infertility while the intake of pantothenic acid was unrelated to ovulatory infertility (Table 4). Adjustment for known and suspected risk factors for infertility, particularly adjustment for iron intake, attenuated these associations. After adjustment, only intake of folic acid was associated with a reduced risk of ovulatory infertility (Table 4). When this analysis was restricted to non-contracepting women there was a strong inverse association between folic acid intake and ovulatory infertility (p, trend = 0.007) (Figure 1). Additional adjustment for multivitamin supplement use attenuated the association between folic acid intake and risk of ovulatory infertility in the entire study population. In this model, the RRs (95% CI) of ovulatory infertility for women in successively higher quintiles of folic acid intake were 0.83 (0.61, 1.13), 0.90 (0.61, 1.31), 0.63 (0.39, 1.02) and 0.64 (0.36, 1.14), compared to women in to lowest intake of folic acid intake (p, trend = 0.17). A similar pattern was observed when folic acid intake was examined among non-users of multivitamin supplements only. The corresponding multivariate-adjusted RRs (95% CIs) among non multivitamin users were 0.88 (0.57, 1.36), 1.06 (0.68, 1.65), 0.78 (0.48, 1.27) and 0.83 (0.49, 1.40) in relation to women not using multivitamins in the lowest quintile of intake (p, trend = 0.43).
Table 4.
Relative risks (95% confidence intervals) for ovulatory infertility by total intake quintiles of B vitamins.
| Quintile of Total Intake (Diet and Supplements) |
||||||
|---|---|---|---|---|---|---|
| Nutrient | 1 | 2 | 3 | 4 | 5 | P trend * |
| Thiamin (B1) | ||||||
| Median Intake (mg/day) | 1.3 | 1.7 | 2.3 | 3.1 | 4.8 | |
| Cases / non-cases | 117 / 5,239 | 96 / 5,330 | 83 / 5,316 | 64 / 5,345 | 78 / 5,303 | |
| Age and energy-adjusted † | 1.00 (referent) | 0.87 (0.67, 1.15) | 0.76 (0.57, 1.02) | 0.58 (0.43, 0.80) | 0.67 (0.50, 0.90) | 0.005 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 0.93 (0.70, 1.26) | 0.87 (0.62, 1.21) | 0.77 (0.52, 1.14) | 0.84 (0.58, 1.22) | 0.44 |
| Riboflavin (B2) | ||||||
| Median Intake (mg/day) | 1.6 | 2.1 | 2.9 | 3.9 | 5.8 | |
| Cases / non-cases | 104 / 5,291 | 104 / 5,317 | 88 / 5,280 | 72 / 5,304 | 70 / 5,341 | |
| Age and energy-adjusted † | 1.00 (referent) | 1.07 (0.81, 1.42) | 0.92 (0.68, 1.23) | 0.74 (0.55, 1.01) | 0.69 (0.50, 0.93) | 0.002 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 1.07 (0.80, 1.44) | 1.02 (0.73, 1.43) | 0.99 (0.67, 1.46) | 0.86 (0.58, 1.28) | 0.32 |
| Vitamin B6 | ||||||
| Median Intake (mg/day) | 1.8 | 2.3 | 3.3 | 4.7 | 11.4 | |
| Cases / non-cases | 99 / 5,350 | 106 / 5,151 | 95 / 5,418 | 75 / 5,249 | 63 /5,365 | |
| Age and energy-adjusted † | 1.00 (referent) | 1.17 (0.89, 1.54) | 1.03 (0.77, 1.37) | 0.81 (0.60, 1.09) | 0.66 (0.47, 0.90) | 0.001 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 1.06 (0.79, 1.45) | 0.96 (0.68, 1.34) | 0.89 (0.60, 1.32) | 0.78 (0.51, 1.18) | 0.15 |
| Vitamin B12 | ||||||
| Median Intake (mcg/day) | 4 | 6 | 9 | 12 | 18 | |
| Cases / non-cases | 101 / 5,624 | 112 / 5,203 | 94 / 5,679 | 64 / 5,024 | 67 /5,003 | |
| Age and energy-adjusted † | 1.00 (referent) | 1.27 (0.96, 1.67) | 0.98 (0.71, 1.31) | 0.74 (0.54, 1.01) | 0.76 (0.55, 1.03) | 0.002 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 1.34 (1.01, 1.77) | 1.07 (0.79, 1.45) | 0.88 (0.61, 1.26) | 0.94 (0.65, 1.37) | 0.24 |
| Folic acid | ||||||
| Median Intake (mcg/day) | 243 | 337 | 495 | 726 | 1138 | |
| Cases / non-cases | 113 / 5,310 | 99 / 5,254 | 101 / 5,300 | 68 / 5,332 | 57 / 5,337 | |
| Age and energy-adjusted † | 1.00 (referent) | 0.91 (0.69, 1.20) | 0.94 (0.71, 1.24) | 0.62(0.45, 0.84) | 0.51 (0.37, 0.71) | <0.001 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 0.82 (0.60, 1.11) | 0.85 (0.61, 1.18) | 0.60 (0.40, 0.89) | 0.61 (0.37, 1.00) | 0.04 |
| Niacin | ||||||
| Median Intake (mg/day) | 20 | 25 | 32 | 40 | 51 | |
| Cases / non-cases | 98 / 5,276 | 108 / 5,309 | 78 / 5,287 | 68 / 5,373 | 86 / 5,288 | |
| Age and energy-adjusted † | 1.00 (referent) | 1.15 (0.87, 1.51) | 0.86 (0.64, 1.16) | 0.74 (0.54, 1.02) | 0.86 (0.64, 1.16) | 0.05 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 1.10 (0.81, 1.48) | 0.89 (0.64, 1.25) | 0.87 (0.60, 1.30) | 0.91 (0.63, 1.31) | 0.39 |
| Pantothenic acid | ||||||
| Median Intake (mcg/day) | 4.0 | 5.0 | 6.0 | 10.6 | 17.1 | |
| Cases / non-cases | 96 / 5,375 | 92 / 5,263 | 75 / 5,283 | 86 / 5,340 | 89 / 5,272 | |
| Age and energy-adjusted † | 1.00 (referent) | 1.05 (0.78, 1.41) | 0.89 (0.65, 1.22) | 0.99 (0.73, 1.35) | 0.96 (0.71, 1.28) | 0.79 |
| Multivariate-adjusted ‡ | 1.00 (referent) | 0.98 (0.71, 1.33) | 0.77 (0.55, 1.09) | 0.91 (0.65, 1.28) | 0.89 (0.64, 1.25) | 0.85 |
Calculated with median nutrient intake in each quintile as a continuous variable.
Adjusted for age (continuous), calendar time (4 two-year intervals) and total energy intake (continuous)
Age and energy-adjusted model further adjusted for body mass index (<20, 20–24.9, 25–29.9, ≥30 and missing), parity (0, 1, ≥2 and missing), smoking history (never, past 1–4 cig/day, past 5–14 cig/day, past 15–24 cig/day, past ≥ 25 cig/day or unknown amount, current 1–4 cig/day, current 5–14 cig/day, current 15–24 cig/day and current ≥ 25 cig/day or unknown amount), physical activity (<3 MET-h/wk, 3–8.9 MET-h/wk, 9–17.9 METh/wk, 18–26.9 MET-h/wk, 27–41.9 MET-h/wk, ≥ 42 MET-h/wk and missing), contraceptive use (current user, never user, past user 0–23 months ago, past user 24–47 months ago, past user 48–71 months ago, past user 72–95 months ago, past user 96–119 months ago, past user ≥ 120 months ago and missing), intake of alcohol (no intake, < 2 g/day, 2–4.9 g/day, ≥ 5 g/day), coffee (<1 serving/month, 1 serving/month, 2–6 servings/week, 1 serving/day, 2–3 servings/day, ≥ 4 servings/day), major types of fatty acids, protein and quintiles of iron intake.
Figure 1. Multivariate-adjusted* relative risk of ovulatory infertility by total intake of folic acid among non-contracepting† women.
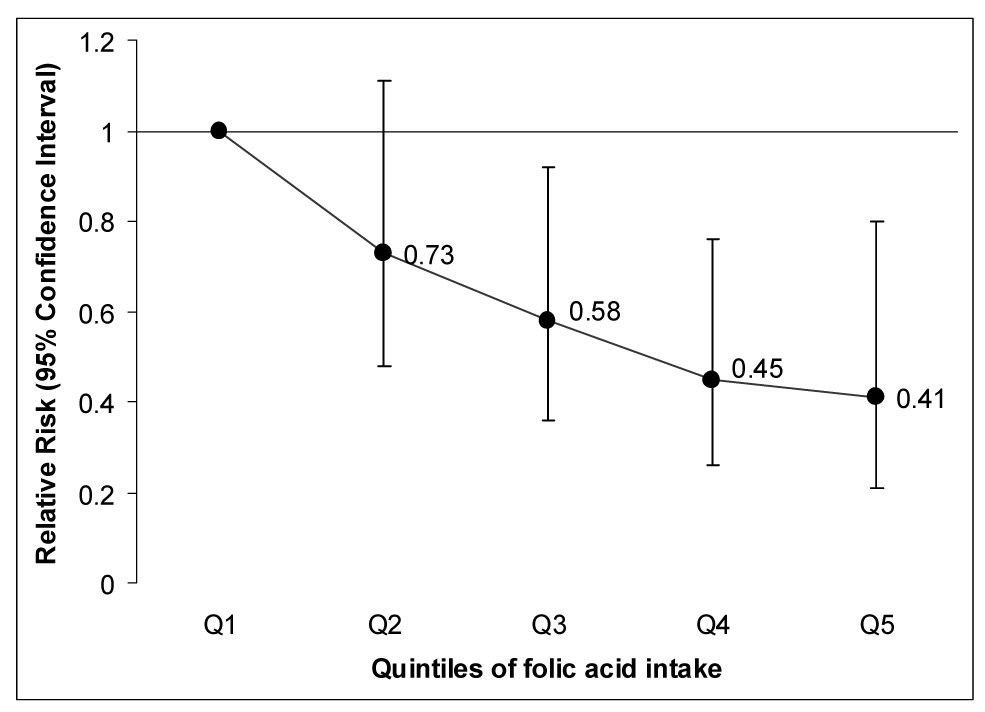
* Adjusted for age (continuous), calendar time (4 two-year intervals), total energy intake (continuous), for body mass index (<20, 20–24.9, 25–29.9, ≥30 and missing), parity (0, 1, ≥2 and missing), smoking history (never, past 1–4 cig/day, past 5–14 cig/day, past 15–24 cig/day, past ≥ 25 cig/day or unknown amount, current 1–4 cig/day, current 5–14 cig/day, current 15–24 cig/day and current ≥ 25 cig/day or unknown amount), physical activity (<3 MET-h/wk, 3–8.9 MET-h/wk, 9–17.9 MET-h/wk, 18–26.9 MET-h/wk, 27–41.9 MET-h/wk, ≥ 42 MET-h/wk and missing), intake of alcohol (no intake, < 2 g/day, 2–4.9 g/day, ≥ 5 g/day), coffee (<1 serving/month, 1 serving/month, 2–6 servings/week, 1 serving/day, 2–3 servings/day, ≥ 4 servings/day), major types of fatty acids, protein and quintiles of iron intake.
† Women who did not report recent use of hormonal contraception, barrier methods, intrauterine devices or spermicides.
We evaluated the possibility that personal characteristics or other dietary behaviors might modify the association between use of multiple vitamin supplements and ovulatory infertility. We found no evidence of interaction between use of multivitamin supplements and age (p=0.18) and presence of long menstrual cycles (p=0.56). Similarly, the association between multivitamins and ovulatory infertility did not differ significantly between nulliparous and parous women (p=0.50), alcohol drinkers and non-drinkers (p=0.17), users and non-users of iron supplements (p=0.83) or lean and overweight/obese women (p=0.46).
DISCUSSION
We examined the association between use of multivitamin supplements and risk of ovulatory infertility and found that using these supplements at least three times per week was associated with a reduced risk of ovulatory infertility. Our results suggest that B-vitamins, particularly folic acid, explain some of the association between multivitamin supplements and ovulatory infertility.
Only two previous studies have evaluated whether supplements containing multiple micronutrients may have an impact on fertility (11, 12). The first study was a double-blind randomized controlled trial designed to evaluate the efficacy of folic acid-containing multivitamin/multimineral supplement in reducing the occurrence of neural tube defects and other congenital malformations as part of a Hungarian family planning program. Over 7,900 women without a history of infertility entered the trial. A secondary analysis of this trial revealed that, after a year, 71% of the women assigned to the multivitamin/multimineral arm of the trial become pregnant while 68% of the women in the placebo arm became pregnant (p<0.01) (12). The second study was a 3-month pilot controlled trial conducted among 30 women who had not been able to become pregnant after 6 to 36 months of unprotected intercourse. During the trial, 4 women on the supplement arm (27%) and none in the placebo arm of the study became pregnant (11).
An important difference between our study and the previous ones is the type of outcome assessed. Since previous studies have used pregnancies, rather than specific infertility diagnoses as their outcome, it is possible that the previously observed effects are not due to improved ovulatory function. Nevertheless, analyses from the Hungarian trial found that multivitamin supplementation improved menstrual cycle regularity (25), suggesting that a decrease in the frequency of ovulatory problems may account for the beneficial effects of multivitamins. Our findings are in agreement with the previous two studies, although the magnitude of the association across studies varies widely. It is possible that the difference in magnitude between our results and those from the Hungarian trial stem from a dilution of the actual multivitamin effect in the trial as a result of not assessing specific outcomes likely to be influenced by multivitamins, but rather a composite of infertility types influenced and not influenced by the intervention. On the other hand, the difference in magnitude between our study and the smaller trial may reflect the small number of outcomes observed due to the limited size of the study.
Our data suggests that folic acid may be responsible for part of the association between multivitamin use and ovulatory infertility. Although, to our knowledge, there have not been other studies of folic acid intake and risk of infertility in general or ovulatory infertility in particular, our findings are in agreement with previous clinical observations and animal studies. In women undergoing controlled ovarian hyperstimulation with recombinant FSH, carriers of the T allele in position 677 of the MTHFR gene (which leads to decreased enzyme activity and 5-methyltetrahydrofolate concentrations) have a decreased ovarian responsiveness to this hormone (13). Although currently unknown, it is possible that ovarian response to endogenous FSH pulses is also decreased in low folate conditions which can be overcome by greater intake of folic acid. Our findings are in agreement with this hypothesis. Folic acid supplementation has been found to increase litter size in pigs (26). In addition, experimentally induced folate deficiency has resulted in decreased ovulation in rats (27).
Our study has some limitations that need to be considered in the interpretation of our results. First, in reconstructing this cohort we assumed that pregnancies occurring among married women were planned. Cases, who were clearly attempting to conceive, could have been more health-conscious than some pregnancy non-cases, who may have conceived accidentally. However, this situation would have resulted in a positive association between multivitamin use, or any other health-conscious behavior, and ovulatory infertility rather than the strong inverse association we observed. In addition, we restricted the study to married women, whose pregnancies are more likely to be intentional than those of unmarried women (28), and included in the non-case group women diagnosed with infertility from other causes, making it less likely that pregnancy intention affected our findings. Also, the association between multivitamins and ovulatory infertility persisted when we restricted our analyses to women who had not recently used contraceptives and when ovulatory infertility cases where compared to infertile women who received other diagnoses, supporting the notion that pregnancy intention did not have an important impact in this study. Second, being an observational study we cannot completely rule out the possibility that our findings may be due in part to unmeasured characteristics associated with both ovulatory infertility and use of multivitamin supplements. Nevertheless, we considered the potential confounding effects of many variables meeting these characteristics, as well as of recognized risk factors for infertility, and found that statistical adjustment for these variables had minimal impact on our results. Lastly, due to the high correlation between multivitamin supplements use and folic acid intake it is difficult to distinguish their independent effects. This issue could be better addressed by larger studies or studying populations with a wider range of folic acid intake from sources other than multivitamins.
In conclusion, in this prospective study we found that consuming multivitamin supplements at least 3 times per week was associated with a reduced risk of ovulatory infertility. This association appeared to be mediated in part by folic acid. Since there are very few studies exploring this relationship, it is desirable that our results are confirmed or refuted, preferably in large randomized trials. However, since supplementation with folic acid by itself or as part of a multivitamin has been shown to reduce the risk of neural tube defects (29, 30) and may prevent other congenital malformations (31), women planning to become pregnant should consider taking a multivitamin as this may also help them to become a pregnant.
ACKNOWLEDGEMENTS
Results of this study were presented in part during the 62nd Annual Meeting of the American Society for Reproductive Medicine, ASRM 2006, in New Orleans, LA October 23, 2006.
Financial Support: The work reported in this manuscript was supported by CA50385, the main Nurses’ Health Study II grant, and by the training grant T32 DK-007703.
The Nurses Health Study II is supported for other specific projects by the following NIH grants: CA55075, CA67262, AG/CA14742, CA67883, CA65725, DK52866, HL64108, HL03804.
Footnotes
CAPSULE In a group of 18,555 healthy women followed for 8 years, consuming 3 or more multivitamin supplements per week was associated with a lower risk of infertility due to anovulation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA, et al. Population study of causes, treatment, and outcome of infertility. Br Med J. 1985;291:1693–1697. doi: 10.1136/bmj.291.6510.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evers JLH. Female subfertility. Lancet. 2002;360:151–159. doi: 10.1016/S0140-6736(02)09417-5. [DOI] [PubMed] [Google Scholar]
- 3.Pinelli A, Di Cesare M. Human fertility: sociodemographic aspects. Contraception. 2005;72:303–307. doi: 10.1016/j.contraception.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Neumann PJ, Gharib SD, Weinstein MC. The cost of a successful delivery with in vitro fertilization. N Engl J Med. 1994;331:239–243. doi: 10.1056/NEJM199407283310406. [DOI] [PubMed] [Google Scholar]
- 5.Katz P, Nachtigall R, Showstack J. The economic impact of the assisted reproductive technologies. Nature Med. 2002;8:S29–S32. doi: 10.1038/ncb-nm-fertilityS29. [DOI] [PubMed] [Google Scholar]
- 6.Olson CK, Keppler-Noreuil KM, Romitti PA, Budelier WT, Ryan G, Sparks AET, et al. In vitro fertilization is associated with an increase in major birth defects. Fertil Steril. 2005;84:1308–1315. doi: 10.1016/j.fertnstert.2005.03.086. [DOI] [PubMed] [Google Scholar]
- 7.Klemetti R, Gissler M, Sevon T, Koivurova S, Ritvanen A, Hemminki E. Children born after assisted fertilization have an increased rate of major congenital anomalies. Fertil Steril. 2005;84:1300–1307. doi: 10.1016/j.fertnstert.2005.03.085. [DOI] [PubMed] [Google Scholar]
- 8.Shevell T, Malone FD, Vidaver J, Porter TF, Luthy DA, Comstock CH, et al. Assisted Reproductive Technology and Pregnancy Outcome. Obstet Gynecol. 2005;106:1039–1045. doi: 10.1097/01.AOG.0000183593.24583.7c. [DOI] [PubMed] [Google Scholar]
- 9.Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal Outcomes in Singletons Following In Vitro Fertilization: A Meta-Analysis. Obstet Gynecol. 2004;103:551–563. doi: 10.1097/01.AOG.0000114989.84822.51. [DOI] [PubMed] [Google Scholar]
- 10.McDonald S, Murphy K, Beyene J, Ohlsson A. Perinatal outcomes of in vitro fertilization twins: A systematic review and meta-analyses. Am J Obstet Gynecol. 2005;193:141–152. doi: 10.1016/j.ajog.2004.11.064. [DOI] [PubMed] [Google Scholar]
- 11.Westphal LM, Polan ML, Sontag Trant A, Mooney SB. A nutritional supplement for improving fertility in women. A pilot study. J Reprod Med. 2004;49:289–293. [PubMed] [Google Scholar]
- 12.Czeizel AE, Metneki J, Dudas I. The effect of preconceptional multivitamin supplementation on fertility. Int J Vit Nutr Res. 1996;66:55–58. [PubMed] [Google Scholar]
- 13.Thaler CJ, Budiman H, Ruebsamen H, Nagel D, Lohse P. Effects of the Common 677C>T Mutation of the 5,10-Methylenetetrahydrofolate Reductase (MTHFR) Gene on Ovarian Responsiveness to Recombinant Follicle-Stimulating Hormone. American Journal of Reproductive Immunology. 2006;55:251–258. doi: 10.1111/j.1600-0897.2005.00357.x. [DOI] [PubMed] [Google Scholar]
- 14.Rich-Edwards JW, Goldman MB, Willett WC, Hunter DJ, Stampfer MJ, Colditz GA, et al. Adolescent body mass index and ovulatory infertility. Am J Obstet Gynecol. 1994;171:171–177. doi: 10.1016/0002-9378(94)90465-0. [DOI] [PubMed] [Google Scholar]
- 15.Cataldo NA, Abbasi F, McLaughlin TL, Basina M, Fechner PY, Giudice LC, et al. Metabolic and ovarian effects of rosiglitazone treatment for 12 weeks in insulin-resistant women with polycystic ovary syndrome. Hum Reprod. 2006;21:109–120. doi: 10.1093/humrep/dei289. [DOI] [PubMed] [Google Scholar]
- 16.Giovannucci E, Stampfer MJ, Colditz GA, Hunter DJ, Fuchs C, Rosner BA, et al. Multivitamin use, folate, and colon cancer in women in the Nurses' Health Study. Ann Intern Med. 1998;129:517–524. doi: 10.7326/0003-4819-129-7-199810010-00002. [DOI] [PubMed] [Google Scholar]
- 17.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 18.Willett WC, Sampson L, Browne ML, Stampfer MJ, Rosner B, Hennekens CH, et al. The use of a self-administered questionnaire to assess diet four years in the past. Am J Epidemiol. 1988;127:188–199. doi: 10.1093/oxfordjournals.aje.a114780. [DOI] [PubMed] [Google Scholar]
- 19.USDA Nutrient Database for Standard Reference Release 14. US Department of Agriculture ARS. 2001
- 20.Willett WC, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol. 1986;124:17–27. doi: 10.1093/oxfordjournals.aje.a114366. [DOI] [PubMed] [Google Scholar]
- 21.Fitzmaurice GM, Laird NM, Ware JH. In: Applied longitudinal analysis. Hoboken NJ, editor. Hoboken, NJ: Wiley & Sons; 2004. [Google Scholar]
- 22.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149:531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 23.Stephen EH, Chandra A. Declining estimates of infertility in the United States: 1982–2002. Fertil Steril. 2006;86:516–523. doi: 10.1016/j.fertnstert.2006.02.129. [DOI] [PubMed] [Google Scholar]
- 24.Spiegelman D, Hertzmark E, Wand H. Point and interval estimates of partial population attributable risks in cohort studies: examples and software. Cancer Causes Control. doi: 10.1007/s10552-006-0090-y. in press. [DOI] [PubMed] [Google Scholar]
- 25.Dudas I, Rockenbauer M, Czeizel AE. The effect of preconceptional multivitamin supplementation on the menstrual cycle. Arch Gynecol Obstet. 1995;256:115–123. doi: 10.1007/BF01314639. [DOI] [PubMed] [Google Scholar]
- 26.Matte JJ, Girard CL, Brisson GJ. Folic acid and reproductive performance of sows. J Anim Sci. 1984;59:1020–1025. doi: 10.2527/jas1984.5941020x. [DOI] [PubMed] [Google Scholar]
- 27.Willmott M, Bartosik DB, Romanoff EB. The effect of folic acid on superovulation in the immature rat. J Endocrinol. 1968;41:439–445. doi: 10.1677/joe.0.0410439. [DOI] [PubMed] [Google Scholar]
- 28.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: Data from the 2002 National Survey of Family Growth. Vital Health Statistics Series 23, No 25: National Center for Health Statistics. 2005 [PubMed]
- 29.Czeizel AE, Dudas I. Prevention of the first occurrence of neural tube defects by periconceptual vitamin supplementation. N Engl J Med. 1992;327:1832–1835. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- 30.MRC Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. Lancet. 1991;338:131–137. [PubMed] [Google Scholar]
- 31.Czeizel AE, Dobo M, Vargha P. Hungarian cohort-controlled trial of periconceptional multivitamin supplementation shows a reduction in certain congenital abnormalities. Birth Defects Res A Clin Mol Teratol. 2004;70:853–861. doi: 10.1002/bdra.20086. [DOI] [PubMed] [Google Scholar]


