Abstract
Aim
The purpose of this paper is to critically analyse the current state of the science literature in order to develop an accurate conception of fever.
Rationale
The measurement of body temperature and treatment of fever have long been considered to be within the domain of nursing practice. What body temperature constitutes ‘fever’, however, is often not clear from nursing protocols or the literature.
Methods
Literature for this concept analysis was obtained by computerized searches of PubMed, CINAHL and BIOSYS for the years 1980−2004. Additional sources were obtained after reviewing the bibliographies of the literature identified by the initial search. The Wilsonian method of concept analysis provided the framework for the analysis.
Findings
Fever has characteristically been recognized as a cardinal sign of illness and has traditionally had negative connotations for patient well-being. Substantive advances over the past 20 years in immunology and neurophysiology have expanded understanding of the process of fever. This new knowledge has shifted the perception of fever as part of the acute-phase response to one of an adaptive nature. This knowledge has yet to be fully translated into changes in the fever management practices of nurses.
Conclusions
Consistent usage of terminology in relation to fever should lead to improved and evidence-based care for patients, and to fever management practices consistent with current research. It is important to use clear language about fever and hyperthermia in discussions and documentation between nurses and among disciplines. By creating clarity in our language, we may help to achieve praxis.
Keywords: concept analysis, hyperthermia, literature review, nursing
Introduction
Fever is encountered or experienced frequently by healthcare professionals and laypersons alike. Its meaning is assumed to be clear and universally understood, when in actuality the interpretation is often uniquely personal. According to Mackowiak et al. (1997), ‘after over a millennium of clinical investigation, there is not even a generally accepted [clinical] definition of fever’ (p. 119).
Similarly, the definition of fever within the nursing and medical literature varies widely. In numerous articles, it is defined or operationalized as simply an elevation of body temperature (McGowan et al. 1987, Cunha & Tu 1988, Lohmann 1988, Roberts et al. 1988, Morgan 1990, Caruso et al. 1992, Segatore 1992, Settle et al. 1994, Pals et al. 1995, Sharber 1997, O'Grady et al. 1998, Volker 1998, Whybrew et al. 1998, Creechan et al. 2001, Dinarello & Gelfand 2004). The level of temperature elevation warranting the diagnosis of ‘fever’ also varies widely within that literature.
As early as the sixth century BC, fever was noted to be a cardinal sign of disease, as Akkadian cuneiform descriptions used a flaming brazier to symbolize both fever and the localized heat that occurs with inflammation (Atkins 1982). In the era of Hippocrates, fever was explained within the doctrine of the four humors: blood, phlegm, black bile, and yellow bile. Yellow bile was associated with the element of fire, and thus fever was considered to be caused by an excess of yellow bile. Fever was thought, at that time, to be a beneficial sign during infection, because the increased heat or ‘fire’ caused by the excess of yellow bile would cook the infection out of the patient (Atkins 1982, Younger & Brown 1985, Holtzclaw 1992, Kluger et al. 1996).
The humoral concept of fever was the mainstay of clinical practice until the 17th century, when Harvey discovered that blood circulated through the body. Subsequently, the belief that fever was beneficial changed dramatically, and physicians thought that fever was produced in body fluids as a result of fermentation and putrefaction or because of friction from increased flow of blood (Atkins 1982, Mackowiak et al. 1997).
Fever was then considered to be synonymous with infectious disease as, until the mid-19th century, most of these diseases were grouped under the generic term of ‘fever’ (Currie 1997). Because patients with fevers were considered to be associated with disease and often death, they were frequently isolated in order to protect the community. As a result, fever came to be feared, and thus warranted intervention. With the discovery of antipyretic drugs in the late 19th century, practitioners began to advocate their use to treat fever (Kluger et al. 1996). This practice continues today, despite new understanding about the intricacies and benefits of the febrile process. Fever is currently treated as ‘the origin of, rather than the response to, an illness’ (Holtzclaw 1992, p. 482).
A growing body of research in immunology and neuro-physiology has led to the recent understanding that fever is generally an adaptive physiological response to some threat (e.g. Kluger 1979, 1986, Saper & Breder 1994, Cooper 1995, Kozak et al. 1995, Dinarello 1996, Kluger et al. 1996, Mackowiak et al. 1997, Mackowiak 1997, Rowsey 1997a, Kluger et al. 1998, Wang et al. 1998). This notion goes against the thinking of the last two centuries that fever was a sinister sign and required intervention to lower or control it. Unfortunately, this information has not always been translated to bedside practitioners caring for febrile patients today.
The lack of clarity of the concept of fever is evident in three recent descriptive, exploratory studies (Grossman et al. 1995, Emmouth & Mansson 1997, Edwards et al. 2001). In each of these, one conducted in the United States of America (USA), one in Sweden, and one in Australia, the authors found lack of consistency in the ways nurses describe who has a fever and when patients with fevers should be treated. Emmouth and Mansson (1997) concluded that, because nurses describe febrile patients in very different terms, misunderstandings result. They recommended the identification and subsequent use of clarified language for use in nursing documentation.
The study
Aim
The purpose of this analysis was to critically examine the concept of fever by analysing the current state of the science literature in order to develop an accurate conception of this commonly-encountered phenomenon in nursing.
Method
The Wilsonian concept analysis technique, as described and used by Avant (2000), formed the foundation of this analysis. It is essential for nurses and other healthcare professionals to have a clear and accurate concept of fever in order to provide optimal and evidenced-based care to patients. It is clear from the discussion in the preceding paragraphs that an analysis of the concept of fever was warranted in order that nurses have a clear definition of fever to guide the nursing process. The Wilsonian concept analysis technique was chosen for this analysis as the literature sampling method is focused and systematic. Since the nursing and medical literature was often at odds with the basic science literature, a systematic and integrative approach was important.
Wilson (1963) stated that the technique of concept analysis is designed to allow its users to develop clarity of thinking and communication about a concept that may otherwise prove problematic. The technique is particularly valuable when a concept has more than one meaning, as in the case of fever (Avant 2000). The Wilsonian technique is designed as a stepwise format, providing a framework for the concept analysis. Wilson explicated an 11-step process, and these are followed until the ultimate goal of ‘results in language’ is achieved (see Table 1).
Table 1.
Steps in the Wilsonian method of concept analysis
| Step | Process |
|---|---|
| 1. Isolating questions of concept | Distinguish between questions of fact, values and concept |
| 2. Finding right answers | Examines the multiple uses of the concept and determines which are essential to the core concept |
| 3. Model cases | Analyst describes clear-cut case of the concept from real-life. Chosen based upon working definition of the concept. Analysis of case allows for the explication of essential elements of the concept |
| 4. Contrary cases | Analyst identifies and describes clear-cut case from real-life that does not illustrate the concept. Analysis of this case allows for identification of elements that makes it ‘not-the-concept’ (Avant, p. 55). |
| 5. Related cases | Analyst identifies and describes case from real-life that is similar or occurs in a similar environment. Critical analysis of case allows for explication of which elements of the concept are essential and which are non-essential |
| 6. Borderline cases | Analyst identifies and describes case from real-life which they are unsure whether or not it is an exemplar of the concept. By examining which elements of the case makes it difficult to classify, the analyst is further able to determine which are essential and which are not. |
| 7. Invented cases | Used when there are insufficient cases to clarify the essential elements of the concept. A case is developed to use the concept outside the realm of the analyst's experience to further clarify the concept's essential elements. (Not used in this concept analysis as there were clear cases for the concept of fever in the other steps) |
| 8. Social context | Analyst identifies who uses the concept, in what manner and environments in order to determine the context in which the concept is used |
| 9. Underlying anxiety | Analyst explicates the underlying feelings and discussions surrounding the concept. Identifies any controversies or debate surrounding the concept |
| 10. Practical results | Analyst identifies the results of understanding the concept's essential elements. These results should be useful for everyday practice |
| 11. Results in language | Analyst defines the concept and its' essential elements in order to identify the best meaning of the concept |
Findings
Step 1: isolating questions of concept
Given the lack of clarity in the fever literature, several questions arise. These include: (1) What is the nature of fever? (2) What are the signs and symptoms of fever? (3) Does fever differ from hyperthermia? (4) Should fever be treated? It is important to separate these questions into the categories of concept, fact, and value. This is because questions of concept are the focus of this analysis, and it is only within this conceptual foundation that ensuing questions of fact and value can be adequately addressed. Thus, in this framework, the first and third questions are questions of concept. The second question is a question of fact. The third question is also a question of fact as it requires explication of the similarities and differences between the concepts of fever and hyperthermia. The last question is one of value, needing both a clear definition of fever and a decision based in values. The first and third questions will be answered by this concept analysis but, as answering one will help delineate the other, this analysis will focus on deriving the nature of the concept of fever.
Step 2: finding right answers
An examination of the ontology of fever reveals that it has two principal uses: the first refers to a physiological process, and the second to a state of heightened emotional or activity level.
The first use has two related definitions according to the online Merriam-Webster's Collegiate Dictionary (2004): (1) ‘a rise of body temperature above the normal’ and (2) ‘any of various diseases of which fever is a prominent symptom’.
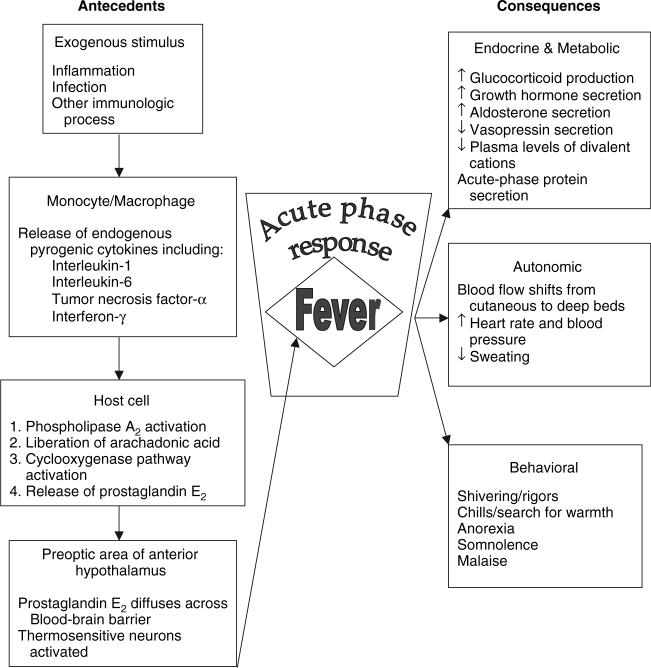
The first has the associated ideas of being a part of the acute-phase response, being a symptom of a disease/pathological process, the temperature being tightly regulated by the hypothalamus as an alteration of the body's set point, initiating heat preservation (e.g. shunting of blood flow away from cutaneous beds) and production (e.g. shivering) mechanisms, and the existence of three distinct phases during fever (Styrt & Sugarman 1990, Holtzclaw 1992, Miller 1993, Saper & Breder 1994, Cooper 1995, Dinarello 1996, Mackowiak 1997, Rowsey 1997a, Holtzclaw 1998, Henker 1999, Dinarello & Gelfand 2004). Figure 1 illustrates the current state of knowledge of the relationship between these ideas. Thus, fever differs from hyperthermia, which is an elevation of body temperature without a change in the set point and is due solely to insufficient heat dissipation (Dinarello & Gelfand 2004).
Figure 1.
Antecedents and consequences of fever (adapted from Mackowiak et al. (1997) and Saper and Breder (1994)).
The second subcategory includes such diseases as scarlet fever and Rocky Mountain Spotted Fever. This use describes fever as a main symptom of the disease of interest, and thus involves all the ideas noted in the first subcategory.
The second use of the word fever, according to the Merriam-Webster's Collegiate Dictionary (2004), is as ‘a state of heightened or intense emotion or activity; a contagious usually transient enthusiasm’. Shakespeare (1974) used this definition in his sonnet 147:
My love is as a fever, longing still
For that which longer nurseth the disease
Feeding on that which doth preserve the ill
The unsickly appetite to please. (p. 1776) This use of the word involves the individual's state of emotion rather than a physiological process. These lines also demonstrate the change in mindset at that time in the perception of fever, indicating that fever would prolong the course of a disease. It is the first use of the word fever that will be considered in this analysis as it is the physiological process that is of interest here. The following case examples will be used to explicate the essential elements of this concept.
Steps 3−7: case examples
The next steps in the Wilsonian method of concept analysis are to use case studies to identify the essential elements of the concept, in this case fever. These elements are present in the following model case and absent to some degree in the others.
Model case
BP is a hospitalized patient in the Neuroscience Intensive Care Unit (NSICU). He is comatose after a traumatic brain injury. His normal diurnal body temperature is 36.7°C. On initial assessment by the day shift nurse, BP's temperature is 37.9°C, his extremities are pale and slightly cool, he is shivering and, on auscultation of his breath sounds, coarse crackles are heard in the right base. A chest X-ray shows right lower lobe pneumonia. Culture results on sputum are positive for bacterial growth. The nurse places BP on a cooling blanket in order to lower his temperature as he is still having episodes of increased intracranial pressure. After 5 minutes on the blanket, his shivering intensifies.
In this case, the patient has an elevated temperature, greater than 1°C above his normal set point. There is a pathological process underlying this elevation, that of pneumonia. BP's body is using both heat production techniques (shivering) and heat retention techniques (blood shunting away from the skin surface beds) to raise his temperature (see Figure 1). He is in the chill phase of the fever. Additionally, his response to cooling measures is to increase heat production techniques to defend his body's higher set point temperature (Holtzclaw 1992, Cooper 1995, Mackowiak 1997, Henker 1999). These are essential elements of the concept of fever.
Contrary case
As a contrary case, a sprint runner is training for an upcoming meet. During intensive training runs, her temperature rises to greater than 1.2°C above her baseline diurnal temperature. After the cool-down period, the runner's temperature returns to normal.
This is a significant elevation in body temperature without an associated pathological process. The increased temperature is related to increased heat production caused by muscle activity that exceeds the body's ability to lose heat. Once the activity stops, the body's heat-dissipating ability is able to regain control and return the body temperature to normal. As a result, the higher temperature is not the runner's protected set point, but the lower temperature is. This phenomenon is termed hyperthermia and is not synonymous with fever (Dinarello & Gelfand 2004).
Related case
A related case, JJ is a patient who presents to a student health centre in the spring with a chief complaint of itchy, watery eyes, sore throat, and runny nose. On initial assessment by the nurse practitioner, her temperature is 37.6°C. She reports her normal diurnal temperature to be 37.4°C. JJ is found to have reddened and boggy nasal passages, reddened sclera, and a clear postnasal discharge. She is prescribed an anti-histamine and counselled to avoid triggering agents. She takes the antihistamine as prescribed, with relief of symptoms and no change in body temperature.
This patient is experiencing an altered immune process, allergic rhinitis, with associated symptoms. Her temperature, although above what is considered to be a ‘normal’ adult body temperature, is not significantly higher than her baseline temperature. No physiological mechanisms for heat conservation or production are employed during the episode of increased temperature (Holtzclaw 1992, Mackowiak 1997, Henker 1999, Dinarello & Gelfand 2004).
Borderline case
A borderline case would be BP, the patient from the model case, who has now been transferred from the NSICU to the acute care unit. He remains in a comatose state after the transfer. BP has been experiencing an elevated temperature of 38.1−38.3°C for the past 14 days. When touched, he has cool, slightly pale extremities and a very warm trunk, but does not have profuse perspiration. BP shivers when attempts are made to reduce his temperature by application of cooling devices; thus he is defending this elevation in temperature. Acetaminophen is ineffective in reducing his fever. All cultures, X-rays, and diagnostic tests are negative for pathological sources of fever. A diagnosis of ‘neurogenic’ fever is made, related to a history of traumatic brain injury.
This is a borderline case as it contains only some of the essential elements of fever. These include increased temperature, defended set point, and utilization of heat production and conservation techniques (Holtzclaw 1992, Mackowiak 1997, Henker 1999). This example lacks the required element of an antecedent, which is a pathological process – a threat to the immune system (see Figure 1) (Saper & Breder 1994). In this example, there is injury to the hypothalamus itself, causing a change in the set point without requiring the presence of endogenous or exogenous pyrogens that would induce an acute-phase response (Thompson et al. 2003, Dinarello & Gelfand 2004). Thus, this is a borderline case and the diagnosis would be better termed post-traumatic hyperthermia.
Step 8: social context
The concept of fever is most often used in healthcare contexts by patients, their families, nurses, and physicians. They are concerned with the following questions: when is an elevated temperature truly a fever, what are the antecedents to and consequences of the fever, and when and how should fever be treated? The social contexts of health-seeking behaviour, patient/family intervention, nursing intervention, medical intervention, the nurse–patient dyad, nurse–provider (nurse practitioner or physician) dyad, and the patient–provider–nurse triad are all complexities that must be considered when making decisions about fever management practices. The evolving notion of fever as an adaptive process makes the process of delineating the concept even more critical. This is because current care practices have not kept up with the latest research findings (Miller 1993, Thomas et al. 1994, Grossman et al. 1995, Rowsey 1997b, Watts et al. 2003, Dinarello & Gelfand 2004).
With the advent of molecular biology and advanced laboratory techniques, basic scientists have greatly expanded our knowledge of the febrile response. Interest in the febrile response as an important and adaptive host defence began over 30 years ago. This identifies that the acute-phase response, which includes fever, results in increased and improved immune system activity against the initial threat to the immune system (see Figure 1). These adaptations include increased neutrophil migration, increased secretion of inter-leukin-1, proliferation of t-lymphocytes, increased production of interferon, hypoferremia, and an increased secretion of chemicals that are antibacterial, antitumour, and/or antiviral in nature (Duff & Durum 1982, Cunha et al. 1984, Fletcher 1987, Styrt & Sugarman 1990, Holtzclaw 1992, Miller 1993, Letizia & Janusek 1994, Saper & Breder 1994, Cooper 1995, Dinarello 1996, Mackowiak 1997, Rowsey 1997a, 1997b). If these findings are clinically validated, then use of routine interventions designed to reduce the temperature associated with fever may be unwarranted.
Additional evidence for fever as an adaptive process comes from several studies conducted with patients having a diagnosis of sepsis. Bryant et al. (1971) and Weinstein et al. (1983) found that patients with bacteraemia or fungaemia who were able to mount a febrile response had a higher survival rate than those who were not. The ability of a patient with sepsis to react to this significant immune insult with a febrile response has been associated with a survival rate nearly double that in comparison with hypothermic patients (Arons et al. 1999). Animal models have repeatedly shown that fever is an important feature of the acute phase response, and is associated with improved survival and shortened duration of illness (Jiang et al. 2000). In one such study, Jiang et al. (2000) induced bacterial peritonitis in mice and found that those with febrile core temperatures had decreased bacterial load and improved survival in comparison with normothermic controls.
Further possible support for the notion of fever as an adaptive process has been gained from studies examining the response of infected patients treated with antipyretics. Graham et al. (1990) found that patients treated with aspirin, acetaminophen, and ibuprofen during infection with rhino-virus had an extended period of viral shedding. Additionally, Dorn et al. (1989) found that children with chicken pox given acetaminophen have a significantly longer time to total crusting of their lesions than those treated with a placebo. These two studies, while not demonstrating a firm causal link between non-treatment of fever and improved clinical outcome, do provide additional support for the theory that fever is beneficial to patients.
Step 9: underlying anxiety
There are several issues that may cause underlying anxiety to patients, families, and healthcare providers in examining the social context of the concept of fever, some of which have been touched on briefly above. These include discussion of the adaptive vs. deleterious nature of fever. Is it truly deleterious in some instances? Clearly, in certain cases there may be a high metabolic toll related to an abnormally high fever that may worsen outcome. This includes older people, neonates, head-injured patients with elevated intracranial pressure, children with a history of febrile seizures, those with severe burns, those with neoplastic disease, those with cardiovascular compromise, and the immunocompromised, but these cases are relatively few (Cunha et al. 1984, Fletcher 1987, Morgan 1990, Holtzclaw 1992, Miller 1993, Rowsey 1997b, Price & McGloin 2003, Diringer et al. 2004). These patients have conditions that necessitate early intervention for fever (Holtzclaw 1992). People who experience discomfort associated with fever may benefit from intervention, but the interventions should be individualized to meet the comfort needs of the patient.
The other anxiety associated with the social context is the perceived need to intervene, to be ‘doing something’ to treat the fever. This pressure may be exerted by physicians or nurses, or by patients or families (Younger & Brown 1985, Fletcher & Creten 1986, Fletcher 1987, Watts et al. 2003). The litigious climate of health care today may raise the level of caregiver anxiety in regard to this concept. Education on the clarified concept of fever for medical and nursing staff as well as patients and families is clearly indicated in order that inappropriate intervention, such as routine use of antipyretics, is avoided (Younger & Brown 1985, Fletcher & Creten 1986, Griffin 1986, Fletcher 1987, Thomas et al. 1994, Dinarello & Gelfand 2004).
Step 10: practical result
This analysis has shown that fever is an adaptive process that is part of the larger context of the body's acute-phase response. It has resulted in a clarified concept of fever that should enable healthcare providers to recognize fever appropriately and to determine when to intervene and when to withhold inappropriate intervention.
What is already known about this topic
Fever is frequently encountered by nurses in a variety of clinical settings.
The clinical definition of fever varies widely, often from practitioner to practitioner, and this variation may lead to practice differences that negatively affect the care of patients.
What this paper adds
Fever is an adaptive, coordinated and systemic response to an immune stimulus, is a self-limiting response in which thermoregulatory control remains intact, and generally requires no treatment.
People with physiologically induced hyperthermia, such as occurs with exercise, clearly do not require intervention.
Those with hyperthermia because of a disruption in set point temperature are often unable to self-regulate their temperature and, although this is not fever as it is not accompanied by the acute phase response, nursing intervention to prevent secondary brain injury is warranted.
Febrile patients not at risk or in discomfort should be monitored and educated about the beneficial effects of fever on the immune system.
Step 11: results in language
The result of this concept analysis is identification of the essential elements of the concept of fever, as follows:
Fever is an element of a coordinated response to a perceived immunological threat (biological or chemical).
The acute-phase response including fever is adaptive and involves autonomic, behavioural, and neuroendocrine processes.
Fever involves an increase in the body's set point temperature. Thermoregulatory control remains intact during fever; fever is self-limiting.
This rise in temperature is the cardinal sign of fever and is an elevation of greater than 1°C above normal diurnal body temperature. There is no ‘absolute’ temperature at which fever is defined.
The altered set point is defended by heat production and heat conservation mechanisms of the body until the initiating threat is removed.
Implications for practice
From the list of critical elements, a clear picture of the concept of fever emerges (see Table 2). It is then possible, using these elements, to determine if an elevation in body temperature is truly a febrile event. People with physiologically induced hyperthermia, such as occurs with exercise, clearly do not require intervention. Others may present with hyperthermia from a disruption in set point temperature, for example those with a traumatic brain injury. These patients are often unable to self-regulate their temperature and, although this is not fever as it is not accompanied by the acute phase response, nursing intervention to prevent secondary brain injury is warranted. As fever is likely an adaptive response of the body to a threat, and thus beneficial, only those who are at secondary risk because of the metabolic effects of fever or those in discomfort should receive interventions aimed at lowering it. Febrile patients not at risk or in discomfort should be monitored and educated about the beneficial effects of fever on the immune system.
Table 2.
Fever: misconceptions and facts
| Misconception | Fact |
|---|---|
| Fever is a cause of illness | Fever is a response to illness |
| Fever is maladaptive | Fever is an adaptive systemic response to immune stimuli |
| Fever is solely an elevation body temperature | Fever is part of the coordinated acute phase response and includes autonomic, behavioural, and neuroendocrine responses |
| There is an absolute temperature at which fever is defined (usually above 100·4°F) | There is no universal temperature at which fever is defined. It is based on the individual's normal diurnal body temperature |
| Fever requires medical or nursing intervention to prevent negative consequences | Fever is self-limiting and generally requires no intervention |
Conclusion
This analysis of the concept of fever will allow for consistent usage in healthcare research on this topic, leading to more substantive and meaningful results. This, in turn, should lead to improved and evidence-based care for patients, and to fever management practices consistent with current research. It is important to use clear language about fever and hyperthermia in discussions and documentation between nurses and among disciplines. By creating clarity in our language, we may help to achieve praxis.
Acknowledgements
The author would like to thank Drs Anne P. Keane and Nancy C. Tkacs of the University of Pennsylvania School of Nursing for their helpful comments on this work, which has been supported, in part, by NIH grants F31 NR07694 and T32 NR 07106.
References
- Arons MM, Wheeler AP, Bernard GR, Christman BW, Russell JA, Schein R, Summer WR, Steinberg KP, Fulkerson W, Wright P, Dupont WD, Swindell BB. Effects of ibuprofen on the physiology and survival of hypothermic sepsis. Critical Care Medicine. 1999;27:699–707. doi: 10.1097/00003246-199904000-00020. [DOI] [PubMed] [Google Scholar]
- Atkins E. Fever: its history, cause, and function. The Yale Journal of Biology and Medicine. 1982;55:283–289. [PMC free article] [PubMed] [Google Scholar]
- Avant KC. The Wilson method of concept analysis. In: Rogers BL, Knafl KA, editors. Concept Development in Nursing: Foundations, Techniques, and Applications. 2nd edn W.B. Saunders; Philadelphia, PA: 2000. pp. 55–64. [Google Scholar]
- Bryant RE, Hood AF, Hood CE, Koenig MG. Factors affecting mortality of gram-negative rod bacterermia. Archives of Internal Medicine. 1971;127:120–128. [PubMed] [Google Scholar]
- Caruso CC, Hadley MJ, Shukula R, Frame P, Khoury J. Cooling effects and comfort of four cooling blanket temperatures in humans with fever. Nursing Research. 1992;41:68–72. [PubMed] [Google Scholar]
- Cooper KE. Fever and Antipyresis: The Role of the Nervous System. Cambridge University Press; Cambridge, UK: 1995. [Google Scholar]
- Creechan T, Vollman K, Kravutske ME. Cooling by convection vs. cooling by conduction for treatment of fever in critically ill adults. American Journal of Critical Care. 2001;10:52–59. [PubMed] [Google Scholar]
- Cunha BA, Tu RP. Fever in the neurosurgical patient. Heart and Lung. 1988;17:608–611. [PubMed] [Google Scholar]
- Cunha BA, Digamon-Beltran M, Gobba PN. Implications of fever in the critical care setting. Heart and Lung. 1984;13:460–465. [PubMed] [Google Scholar]
- Currie MR. The rise and demise of fever nursing. International History of Nursing Journal. 1997;3:5–19. [PubMed] [Google Scholar]
- Dinarello CA. Thermoregulation and the pathogenesis of fever. Infectious Disease Clinics of North America. 1996;10:433–449. doi: 10.1016/s0891-5520(05)70306-8. [DOI] [PubMed] [Google Scholar]
- Dinarello CA, Gelfand JA. Fever and hyperthermia. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison's Principles of Internal Medicine. 16th edn McGraw-Hill; New York: 2004. pp. 104–108. [Google Scholar]
- Diringer MN, Reaven NL, Funk SE, Uman GC. Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Critical Care Medicine. 2004;32:1489–1495. doi: 10.1097/01.ccm.0000129484.61912.84. [DOI] [PubMed] [Google Scholar]
- Dorn TF, DeAngelis C, Baumgardner RA. Acetaminophen: more harm than good for chicken pox? Journal of Pediatrics. 1989;114:1045–1048. doi: 10.1016/s0022-3476(89)80461-5. [DOI] [PubMed] [Google Scholar]
- Duff GW, Durum SK. Fever and immunoregulation: hyperthermia, interleukins-1 and –2, and T-cell proliferation. Yale Journal of Biology and Medicine. 1982;55:437–442. [PMC free article] [PubMed] [Google Scholar]
- Edwards HE, Courtney MD, Wilson JE, Monagha SJ, Walsh AM. Fever management practices: what pediatric nurses say. Nursing and Health Sciences. 2001;3:119–130. doi: 10.1046/j.1442-2018.2001.00083.x. [DOI] [PubMed] [Google Scholar]
- Emmouth U, Mansson ME. Nursing care for the feverish patient. Vard I Norden. 1997;17(4):4–8. doi: 10.1177/010740839701700402. [DOI] [PubMed] [Google Scholar]
- Fletcher JL. Current concepts in the nature and treatment of fever. Physician Assistant. 1987;11:95–106. [Google Scholar]
- Fletcher JL, Creten D. Perceptions of fever among adults in a family practice setting. Journal of Family Practice. 1986;22:427–430. [PubMed] [Google Scholar]
- Graham MH, Burrell CJ, Douglas RM. Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers. Journal of Infectious Disease. 1990;162:1277–1282. doi: 10.1093/infdis/162.6.1277. [DOI] [PubMed] [Google Scholar]
- Griffin JP. Fever: when to leave it alone. Nursing. 1986;86:58–61. [PubMed] [Google Scholar]
- Grossman D, Keen MF, Singer M, Asher M. Current nursing practices in fever management. MEDSURG Nursing. 1995;4(3):193–198. [PubMed] [Google Scholar]
- Henker R. Evidence-based practice: fever-related interventions. American Journal of Critical Care. 1999;8:481–487. [PubMed] [Google Scholar]
- Holtzclaw B. The febrile response in critical care: state of the science. Heart and Lung. 1992;21(5):482–500. [PubMed] [Google Scholar]
- Holtzclaw B. Managing fever in HIV disease. Journal of the Association of Nurses in AIDS Care. 1998;9:97–101. doi: 10.1016/S1055-3290(98)80050-2. [DOI] [PubMed] [Google Scholar]
- Jiang Q, Cross AS, Singh IS, Chen TT, Viscardi RM, Hasday JD. Febrile core temperature is essential for optimal host defense in bacterial peritonitis. Infection and Immunity. 2000;68:1265–1270. doi: 10.1128/iai.68.3.1265-1270.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluger MJ. Fever: Its Biology, Evolution, and Function. Princeton University Press; Princeton, NJ: 1979. [Google Scholar]
- Kluger MJ. Is fever beneficial? Yale Journal of Biology and Medicine. 1986;59:89–95. [PMC free article] [PubMed] [Google Scholar]
- Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D. The adaptive value of fever. Infectious Disease Clinics of North America. 1996;10:1–20. doi: 10.1016/s0891-5520(05)70282-8. [DOI] [PubMed] [Google Scholar]
- Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D. Role of fever in disease. Annals of the New York Academy of Sciences. 1998;856:224–233. doi: 10.1111/j.1749-6632.1998.tb08329.x. [DOI] [PubMed] [Google Scholar]
- Kozak W, Zheng H, Conn CA, Soszynski D, Van Der Ploeg LHT, Kluger MJ. Thermal and behavioral effects of lipopolysaccharide and influenza in interleukin-1β-deficient mice. American Journal of Physiology. 1995;269:R969–R977. doi: 10.1152/ajpregu.1995.269.5.R969. [DOI] [PubMed] [Google Scholar]
- Letizia M, Janusek L. The self-defense mechanism of fever. MEDSURG Nursing. 1994;3:373–377. [PubMed] [Google Scholar]
- Lohmann M. Fever: different types, different causes. Nursing. 1988;88(4):98–101. doi: 10.1097/00152193-198804000-00025. [DOI] [PubMed] [Google Scholar]
- Mackowiak PA. Fever: Basic Mechanisms and Management. 2nd edn Lippincott-Raven; Philadelphia, PA: 1997. [Google Scholar]
- Mackowiak PA, Bartlett JG, Borden EC, Goldblum SE, Hasday JD, Munford RS, Nasraway SA, Stolley PD, Woodward TE. Concepts of fever: recent advances and lingering dogma. Clinical Infectious Diseases. 1997;25:119–138. doi: 10.1086/514520. [DOI] [PubMed] [Google Scholar]
- McGowan JE, Jr., Rose RC, Jacobs NF, Schaberg DR, Haley RW. Fever in hospitalized patients. American Journal of Medicine. 1987;82:580–586. doi: 10.1016/0002-9343(87)90103-3. [DOI] [PubMed] [Google Scholar]
- Merriam-Webster's Collegiate Dictionary [21 September 2004];2004 Online, available at: http://www.m-w.com/cgi-bin/dictionary.
- Miller C. Fever: mechanisms, controversy, and research based interventions. CACCN. 1993;4(4):30–33. [Google Scholar]
- Morgan SP. A comparison of three methods of managing fever in the neurologic patient. Journal of Neuroscience Nursing. 1990;22:19–24. doi: 10.1097/01376517-199002000-00006. [DOI] [PubMed] [Google Scholar]
- O'Grady NP, Barie PS, Bartlett J, Bleck T, Garvey G, Jacobi J, Linden P, Maki DG, Nam M, Pasculle W, Pasquale MD, Tribett DL, Masur H. Practice parameters for evaluating new fever in critically ill adult patients. Critical Care Medicine. 1998;26(2):392–408. doi: 10.1097/00003246-199802000-00046. [DOI] [PubMed] [Google Scholar]
- Pals JK, Weinbery AD, Beal LF, Levesque PG, Cunningham TJ, Minaker KL. Clinical triggers for detection of fever and dehydration. Journal of Gerontological Nursing. 1995;21(4):13–19. doi: 10.3928/0098-9134-19950401-04. [DOI] [PubMed] [Google Scholar]
- Price T, McGloin S. A review of cooling patients with severe cerebral insult in ICU (part 1). Nursing Critical Care. 2003;8:30–36. doi: 10.1046/j.1478-5153.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- Roberts J, Barnes W, Pennock M, Browne G. Diagnostic accuracy of fever as a measure of postoperative pulmonary complications. Heart and Lung. 1988;17:166–170. [PubMed] [Google Scholar]
- Rowsey PJ. Pathophysiology of fever part 1: the role of cytokines. Dimensions of Critical Care Nursing. 1997a;16:202–207. doi: 10.1097/00003465-199707000-00004. [DOI] [PubMed] [Google Scholar]
- Rowsey PJ. Pathophysiology of fever part 2: relooking at cooling interventions. Dimensions of Critical Care Nursing. 1997b;16:251–256. doi: 10.1097/00003465-199709000-00003. [DOI] [PubMed] [Google Scholar]
- Saper CB, Breder CD. The neurologic basis of fever. The New England Journal of Medicine. 1994;330:1880–1886. doi: 10.1056/NEJM199406303302609. [DOI] [PubMed] [Google Scholar]
- Segatore M. Fever after traumatic brain injury. Journal of Neuroscience Nursing. 1992;24:104–109. doi: 10.1097/01376517-199204000-00010. [DOI] [PubMed] [Google Scholar]
- Settle JT, Neff-Smith M, Wan G. Infections related to venous access devices in patients with AIDS. Journal of the Association of Nurses in AIDS Care. 1994;5(5):43–46. [PubMed] [Google Scholar]
- Shakespeare W. Sonnet 147. In: Evans GB, editor. The Riverside Shakespeare. Houghton-Mifflin; Boston: 1974. p. 1776. original work published 1609. [Google Scholar]
- Sharber J. The efficacy of tepid sponge bathing to reduce fever in young children. American Journal of Emergency Medicine. 1997;15:188–192. doi: 10.1016/s0735-6757(97)90099-1. [DOI] [PubMed] [Google Scholar]
- Styrt B, Sugarman B. Antipyresis and fever. Archives of Internal Medicine. 1990;150:1589–1597. [PubMed] [Google Scholar]
- Thomas V, Riegel B, Andrea J, Murray P, Gerhart A, Gocka I. National survey of pediatric fever management practices among emergency department nurses. Journal of Emergency Nursing. 1994;20:505–510. [PubMed] [Google Scholar]
- Thompson HJ, Tkacs NC, Saatman KE, Raghupathi R, McIntosh TK. Hyperthermia following traumatic brain injury: a critical evaluation. Neurobiology of Disease. 2003;12:163–173. doi: 10.1016/s0969-9961(02)00030-x. [DOI] [PubMed] [Google Scholar]
- Volker D. Fever of unknown origin. Nurse Practitioner Forum. 1998;9:170–176. [PubMed] [Google Scholar]
- Wang WC, Goldman LM, Schleider DM, Appenheimer MM, Subjeck JR, Repasky EA, Evans SS. Fever-range hyperthermia enhances L-selectin-dependent adhesion of lymphocytes to vascular endothelium. Journal of Immunology. 1998;160:96–969. [PubMed] [Google Scholar]
- Watts R, Robertson J, Thomas G. Nursing management of fever in children: a systematic review. International Journal of Nursing Practice. 2003;9:S1–S8. doi: 10.1046/j.1440-172x.2003.00412.x. [DOI] [PubMed] [Google Scholar]
- Weinstein MP, Murphy JR, Reller LB, Lichtenstein KA. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. Review of Infectious Diseases. 1983;5:54–70. doi: 10.1093/clinids/5.1.54. [DOI] [PubMed] [Google Scholar]
- Whybrew K, Murray M, Morley C. Diagnosing fever by touch: observational study. British Medical Journal. 1998;317:321. doi: 10.1136/bmj.317.7154.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J. Thinking with Concepts. Cambridge University Press; Cambridge, UK: 1963. [Google Scholar]
- Younger JB, Brown BS. Fever management: rational or ritual? Pediatric Nursing. 1985;11(1):26–29. [PubMed] [Google Scholar]