Abstract
To facilitate the design of effective policies that can address adolescent’s reproductive health problems, it is necessary to gain a thorough understanding of patterns of adolescents’ sexual behavior, and the factors that affect them. Using a unique set of data collected in 2004 from a nationally-representative survey of adolescents, this study examines adolescents’ risky and protective sexual behavior in Burkina Faso. Findings show that 11% of adolescent males had sexual intercourse in last twelve months with more than two partners but did not use condoms. Logistic regression analysis shows that the odds of using condoms increased with years of schooling and self-efficacy in use of condoms. Females who were very confident of getting a male partner to wear a condom were six times more likely to have used a condom at last sex than those who were not confident at all.
Keywords: Burkina Faso, adolescents, risky sexual behaviors, condoms, HIV/AIDS
Introduction
HIV/AIDS is one of the most urgent public health challenges facing both developing and developed nations. Even though it affects all the social sectors of the population, the epidemic among adolescents is the fastest growing partly because of young people’s vulnerability and because of low use of preventive services. In spite of this, adolescents are also seen as a ‘window of hope’ because they have great potential for positive change of attitudes and behaviours. Focusing on young people is likely to be the most effective approach to confronting the epidemic, particularly in high prevalence countries. This was recognized at a global level by the 2001 UN General Assembly Special Session on HIV/AIDS who endorsed that “By 2003, establish time-bound national targets to achieve the internationally agreed global prevention goal to reduce by 2005 HIV prevalence among young men and women aged 15–24 in the most affected countries by 25% and by 25% globally by 2010”.1
Although HIV prevalence is lower in Burkina Faso other countries in sub-Saharan Africa, the epidemic is generalized to the whole population. Further, the population of young people is quite large and sexual experience starts early.2 Overall, the estimated HIV prevalence among adults in 2001 was 7%, whereas more recent HIV prevalence estimates for 2003 are 4% (based on UNAIDS estimates). Despite these signs of progress, halting the spread of the HIV virus remains a big challenge: HIV prevalence figures continue to show that women—particularly young women—are at a greater risk of HIV/AIDS and are infected at younger ages than men.3
Much research has been carried out on the determinants and consequences of sexual behaviour among adults, but until recently adolescents have received little attention in Burkina Faso. Gaps in knowledge regarding adolescents’ sexual behaviour persist. For example, not much is known about what motivates young people to initiate first sex, to have multiple sexual partners, or to use protection such as condoms.
Research on adolescents’ sexual behaviour carried out in other countries has shown that a range of factors including lack of reproductive health and HIV/AIDS information and services contribute to heightened risk of HIV among young people.4–5 However, the single most important determinant of HIV infection among young people in Africa is having unprotected sex with a person who is infected. To quote the Measure Evaluation program, “Any number of other factors may influence who has sex with whom and whether they use condoms, but the act that spreads the virus, in the overwhelming majority of cases, is an act of unprotected sex”.6(p.10)
Many factors have been proposed to explain why adolescents do not use condoms. In spite of efforts by national HIV prevention programs to reduce or eliminate the cost of condoms in many African countries, adolescents still report affordability as a reason for non-use.7 Negotiation to use condoms is also difficult since suggesting the use of condoms is often seen as a sign of mistrust in a sexual relationship. Furthermore, the ability by female adolescents to negotiate the use of condoms is made difficult if they have received gifts or money.8 Other reasons for non-use of condoms among adolescents include dislike of condoms, and embarrassment to purchase or ask for condoms from adult providers, which stems from disapproving attitudes from health providers.9
HIV programs that are designed to improve knowledge and awareness about HIV and sexually transmitted infections (STIs) are often based on the premise that greater knowledge among adolescents will lead to changes in their sexual behaviour. However, some studies have reported the lack of association between HIV knowledge and sexual behaviour.10–11 On the other hand, social and cultural barriers, attitudes and practices seem to be the major determinants of adolescents’ risky behaviour.12–13 Another premise is that use of protection will depend on the type of sexual partner, and while this premise may hold among adults, it is not clear that adolescents act in this way.
Without urgent measures to enable young people to protect themselves from HIV/AIDS, development efforts will be in jeopardy. Investing in adolescents and youth is one of the most cost-effective interventions to achieve ICPD goals. Support for young people is also critical for the attainment of the Millennium Development Goals of halting the further spread of HIV, reducing maternal mortality and improving child survival since consequences of unprotected sex include many aspects of reproductive ill-health.
Using a unique set of data collected in 2004 from a nationally-representative survey of adolescents in Burkina Faso, this study aims to examine adolescents’ risky and protective sexual behaviour by looking at use of condoms and the type of partner. Of specific focus to the paper is to see whether attitudes towards condoms and the type of sexual partner have a bearing on whether or not adolescents use condoms.
Methods
The data come from the Burkina National Adolescents Survey (BNAS) carried out in 2004 in collaboration with Macro International Inc and the Institut National de la Statistique et de la Démographie of Burkina Faso. The survey was a nationally-representative household where sampling was done as following: a first-stage systematic selection of census areas was made and a second stage selection of households within the selected census areas was made from a household listing. All eligible 12–19 de facto residents in each sampled household were included in the survey. However, consent from a parent or caretaker was requested for adolescents aged 12–17 years before the eligible adolescent was approached to participate in the survey. A total number of 5,955 adolescents of 12–19 years old were surveyed with a response rate of 96%. The 2004 BNAS is part of a larger, five-year study of adolescent sexual and reproductive health issues called Protecting the Next Generation: Understanding HIV Risk Among Youth (PNG). The PNG project, which is being carried out in Burkina Faso, Ghana, Malawi and Uganda, seeks to contribute to the global fight against the HIV/AIDS epidemic among adolescents by raising awareness of young people’s sexual and reproductive health needs with regard to HIV/AIDS, other sexually transmitted infections (STIs) and unwanted pregnancy; communicating new knowledge to a broader audience, including policymakers, healthcare providers and the media, in each country, regionally and internationally; and stimulating the development of improved policies and programs that serve young people.
The survey used two instruments: a household screener and an adolescent questionnaire. The household screener was used to list all usual members and visitors in the selected household. The age, sex, relationship to head of household and education characteristics was collected for each person listed. The purpose of the screener was to identify eligible 12–19 year olds for individual interview. The household screener also collected information on the household’s access to safe drinking water and improved sanitation, environmental conditions, land ownership, and possessions. The adolescent questionnaire collected detailed information on a range of issues such as adolescents’ views of health information and services; sexual relationships and partners’ characteristics; the consistency and correctness of condom use; exposure to and content of sex education in schools; and family and peer influences.
For these analyses, we used chi-square tests to compare proportions of respondents, within and across the groups who used condoms at last sex during the last 12 months and the proportions of respondents by attitudes towards condoms. Logistic regression was used to test the associations between adolescents’ use of condoms and their attitudes towards condoms as well as the type of sexual partners in the last 12 months. We also examined the association between adolescents’ use of condoms and their social and demographic characteristics (schooling, religion, residence and so on). Analyses were performed using the statistical package SPSS.
Results
Sample characteristics
Overall, the educational level of the adolescents in the study was very low. About 53% of males and 64% of females aged 15–19 years have never attended school (see Table 1). Among males who have ever attended school, 58% of 12–14 years old and 78% of 15–19 years old are not currently in school. The proportions are much higher for females (70% of 12–14 years old and 84% for 15–19 years old). Very few adolescents aged between 12 and 14 years had initiated sex at the time of the survey (2%). On the other hand, among males of the same age-range, 6% of them report that they had first sex. Among females who were 15–19 years old, 25% were in union while 16% of them had given birth to a child. About 55% of females and up to 66% of males aged 15–19 years reported that they had never had sex. For females who were 15–19 years old who had never experienced intercourse, the underlying reason given was that they wanted to wait until marriage. Among those who were sexually experienced, 6% of females and up to 21% of males reported to have had three or more lifetime sexual partners while 5% and 24% respectively for females and males had 2 or more sexual partners in the 12 months before the survey.
Table 1.
Percentage of adolescents aged 12–19 years by selected background characteristics, Burkina Faso, National Survey of Adolescents, 2004
| Characteristic | Females | Males | ||||
|---|---|---|---|---|---|---|
| 12–14 (N=1286) | 15–19 (N=1687) | Total (N=2973) | 12–14 (N=1350) | 15–19 (N=1707) | Total (N=3057) | |
| Residence | ||||||
| Urban | 20.1 | 30.4 | 26.1 | 17.2 | 24.2 | 21.2 |
| Rural | 79.9 | 69.6 | 73.9 | 82.8 | 75.8 | 78.8 |
| Highest level of education | ||||||
| None | 62.3 | 63.5 | 63 | 48.4 | 52.7 | 50.8 |
| Primary school | 33 | 21.5 | 26.2 | 43.7 | 27.9 | 34.8 |
| Secondary school and higher | 4.9 | 15 | 10.8 | 7.9 | 19.5 | 14.3 |
| Marital status | ||||||
| Currently in union | 0.5 | 24 | 13.8 | 0 | 1.2 | 0.7 |
| Not in Union | 99.5 | 76 | 86.2 | 100 | 98.8 | 99.3 |
| Ever had sex | ||||||
| Yes | 2 | 44.8 | 26.8 | 5.8 | 34.1 | 78.4 |
| No | 98 | 55.2 | 73.2 | 94.2 | 65.9 | 21.6 |
| Number of lifetime sex partners | ||||||
| 1 | [88.5] | 75.1 | 75.5 | 58.7 | 52.8 | 53.5 |
| 2 | [11.5] | 19.2 | 18.9 | 24 | 26.3 | 26.1 |
| ≥ 3 | [0.0] | 5.8 | 5.6 | 17.3 | 20.9 | 20.4 |
| Number of sexual partners in last 12 months | ||||||
| 0 | [12] | 14.1 | 14 | 28.4 | 25.6 | 25.9 |
| 1 | [84] | 81.3 | 81.3 | 55.4 | 56.9 | 56.8 |
| ≥ 2 | [4] | 4.7 | 4.7 | 16.2 | 17.5 | 17.3 |
]: N is 25 to 49
Adolescents’ attitudes towards condoms
This section describes young people’s attitudes towards condoms. A set of questions were asked to ascertain adolescents’ attitudes towards condoms: Do you agree with the statement that condoms reduce pleasure? Do you agree with the statement that the use of condoms is a sign of lack of trust towards the sexual partner? Do you think that it is embarrassing to buy or ask for a condom? The survey also obtained information on the level of confidence of females in getting their partner to wear condoms as well as the level of confidence of males in knowing how to use a condom (see Table 2). Overall, less than 3 in 10 female adolescents felt very confident that they can get a male partner to wear a condom while the same proportion of adolescent males felt very confident that they know how to wear a condom. However, there are significant differences between age groups with the eldest females being twice more likely to be very confident than youngest in getting the partner to wear a condom. As for males, the tendency is the same with the older adolescents being almost three times more likely to know how to wear a condom.
Table 2.
Attitudes towards male condoms among adolescents who had ever heard about condoms by age and sex, Burkina Faso, National Survey of Adolescents, 2004
| Characteristic | Females | Males | ||||
|---|---|---|---|---|---|---|
| 12–14 (N=797) | 15–19 (N=1424) | Total (N=2221) | 12–14 (N=982) | 15–19 (N=1515) | Total (N=2497) | |
| Condoms reduces pleasure | ||||||
| Agree | 12.9 | 21.7* | 18.6 | 20.1 | 32.8* | 27.9 |
| Disagree | 87.1 | 78.3 | 81.4 | 79.8 | 67.2 | 72.1 |
| Condoms use is a sign of lack of trust | ||||||
| Agree | 32.8 | 42.6* | 39.1 | 37.2 | 46.3* | 42.7 |
| Disagree | 67.2 | 57.4 | 60.1 | 62.8 | 53.7 | 57.3 |
| Embarrassing to buy/ask a condom | ||||||
| Agree | 61.5 | 59.5 | 60.2 | 54.6 | 44* | 48.2 |
| Disagree | 38.5 | 40.5 | 39.8 | 45.4 | 56 | 51.8 |
| Level of confidence in getting partner to wear condom‡ | ||||||
| Very confident | 13.6 | 26.6* | 21.9 | 12.1 | 32* | 24.2 |
| Somewhat confident | 10.7 | 16.5* | 14.5 | 14.8 | 21.6* | 18.9 |
| Not confident at all | 75.7 | 56.9* | 63.6 | 73.1 | 46.4* | 56.7 |
Significance different (p<.05) from adolescents aged 12–14 years old, based on findings from chi-square test.
For males the question was “Level of confidence in knowing how to use a condom”
Overall, 19% of females and up to 28% of males agreed that condoms reduce pleasure. The proportions are significantly higher among older adolescents aged 15–19 years. About 39% of females and 43% of males stated that the use of condoms during sex is a sign of lack of trust towards the partner and the proportions were significantly higher among older adolescents. Almost 1 male in 2 said that it is embarrassing to buy or ask for a condom. The proportion was significantly higher among young males (see Table 2). For females, about 60% agreed with the statement that it is embarrassing to buy or ask for condoms, and this proportion did not vary by age-group.
Type of sexual partner and use of condoms among adolescents
We considered two types of risk profiles for sexually active adolescents. The first profile was the risk for adolescents who did not use condoms at first sex, according to the type of sexual partners. The second profile focused on use or non-use of condoms by type of partner for those adolescents who were sexually active in the past 12 months. Overall, among females who were 15–19 years old, 53% of them had their first sex with a boyfriend, 42% with a cohabiting partner and 5% with a casual acquaintance. As for males, 66% of those aged between 12–14 years and 85% of older adolescents had their first sex with a girlfriend while 34% and 13% of those aged 12–14 and 15–19 years, respectively, had their first sex with a casual acquaintance. The proportions are different for last sex. Among females in the 15–19 years age-range who were not in union, 92% had their last sex with a boyfriend and 8% with a casual acquaintance while 100% of those who are in union said that they had their last sex with their cohabiting partner. As for males, 72% of younger and 84% of older adolescents, respectively, had their last sex with a girlfriend while 28% and 13% of the younger and older adolescents had last sex with a casual acquaintance.
Characteristics of users of condoms at last sex among adolescents who were sexually active in the 12 months before the survey are as follows: for 42% of females aged 15–19 years, the respondent herself suggested the use of condoms; in 20% of the cases, the suggestion was made by the partner while in 30% of the cases, the use of condoms was a joint decision. The proportions are radically different for males. About 73% of males aged 15–19 years report that they suggested the use of condoms while for only 6% the suggestion was made by their partner. For 15% of older adolescent males, the use of condoms was a joint decision. With regards to the use of condoms by type of partner, the data show very low use of condoms at first sex with a cohabiting partner compared to adolescents who had first sex with boyfriends or girlfriends. Contrary to expectations, use of condoms is low among adolescents who have had their first sex with a casual sexual partner. As for condom use in last 12 months, the overall pattern was roughly the same as for first sex showing lower use for sex within cohabiting unions and highest use for sex with boyfriends or girlfriends. However, the percentage of adolescents who reported to have used condoms at last sexual act was higher than use at first sex (see Table 3).
Table 3.
Percent of sexually experienced adolescents aged 15–19 years who used condoms at first sex and last sex by type of partner, Burkina Faso, National Survey of Adolescents, 2004
| Females | Males | |||||
|---|---|---|---|---|---|---|
| Used condom | Yes | No | N | Yes | No | N |
| First Sexual Intercourse Type of Partner | ||||||
| Husband/Wife/Cohabiting partner | 3.8* | 96.2 | 312 | [10] | [90] | 10 |
| Boy/Girl friend | 39.6* | 60.4 | 391 | 34.3 | 65.7 | 466 |
| Occasional partner | [21.4] | [78.6] | 42 | 21.2 | 78.8 | 85 |
| Last Sexual Intercourse Type of Partner | ||||||
| Husband/Wife/Cohabiting partner | 6.1* | 93.9 | 342 | — | — | 11Boy/ |
| Girl friend | 47.5* | 52.5 | 263 | 50.1 | 49.9 | 351 |
| Occasional partner | — | — | 17 | [39.1] | [60.9] | 46 |
p< 0.05: Significance level refers to findings from chi-square test; — N < 24; [ ] N is 25–49.
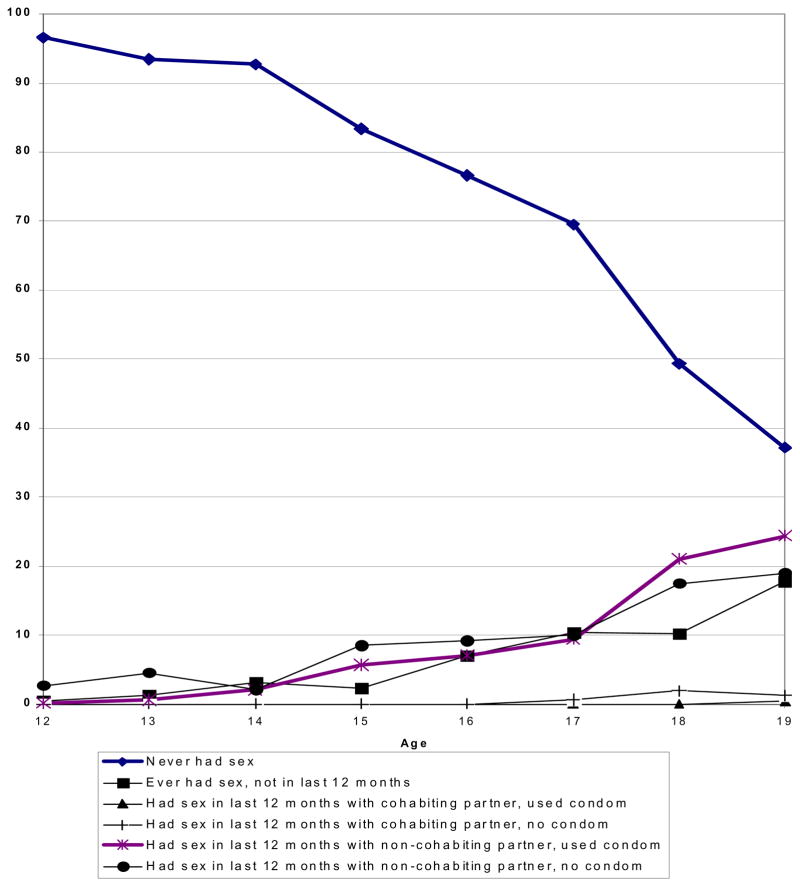
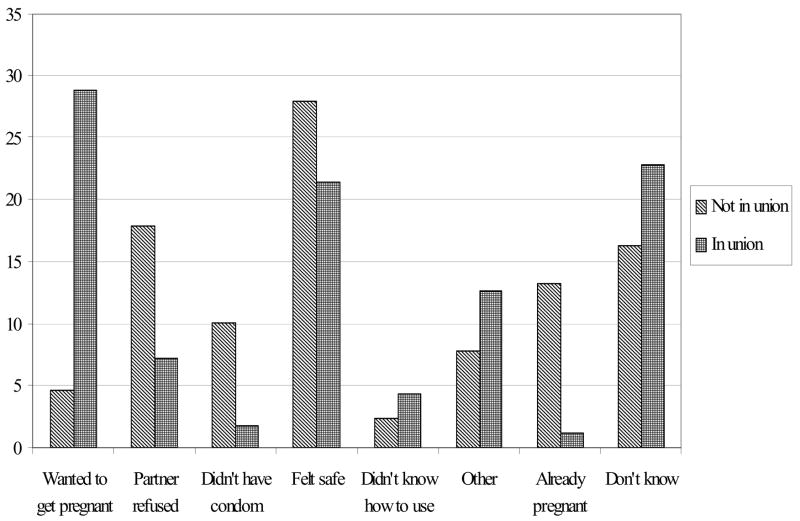
Figures 1 and 2 use the behavioural indicators developed by the WHO14 to summarize the profiles of adolescents, each highlighting different perspectives on exposure to the risk of HIV/STIs. It is important to point out that few 12–14 years adolescents report that they have initiated sex (2% of females and 6% of males). From the figures, we see that by age 17, more than half of the females have had sex, while the corresponding median age for males is about one year later. Analysis by disaggregating the data by age, sex and marital status shows that sexual behaviour varies widely between age groups. Indeed, among males the proportion of those who have had sex in the last 12 months with their girlfriend and did not use condoms increases with age: 7% at 15 years, 16% at 16, 33% at 17, 41% at 18 years.
Figure 1.
Sexual behavior and condom use at last sex among male 12 –19 year olds, Burkina Faso, National Survey of Adolescents, 2004
Figure 2.
Sexual behavior and condom use at last sex among male 12–19 year olds, Burkina Faso, National Survey of Adolescents, 2004
Among females, the corresponding proportions are between 5% and 15%, with the highest likelihood of having sex with non-cohabiting partner without using condoms among the 17-year olds. As we expected, use of condoms with cohabiting partners is very low.
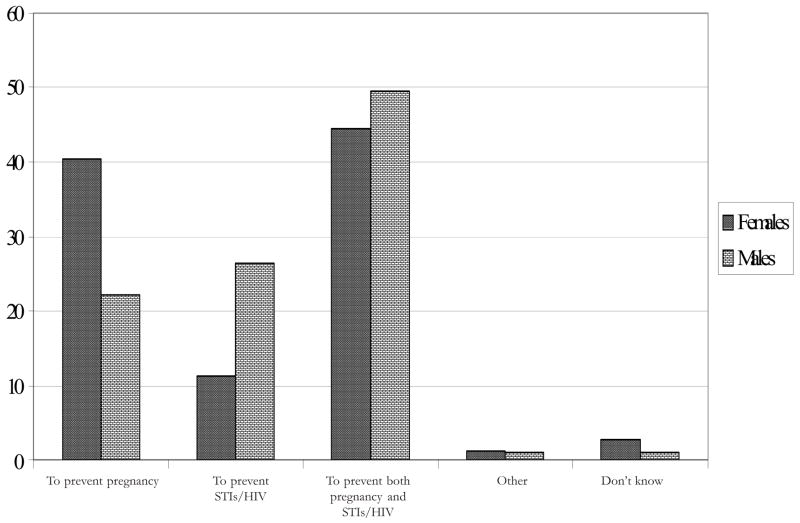
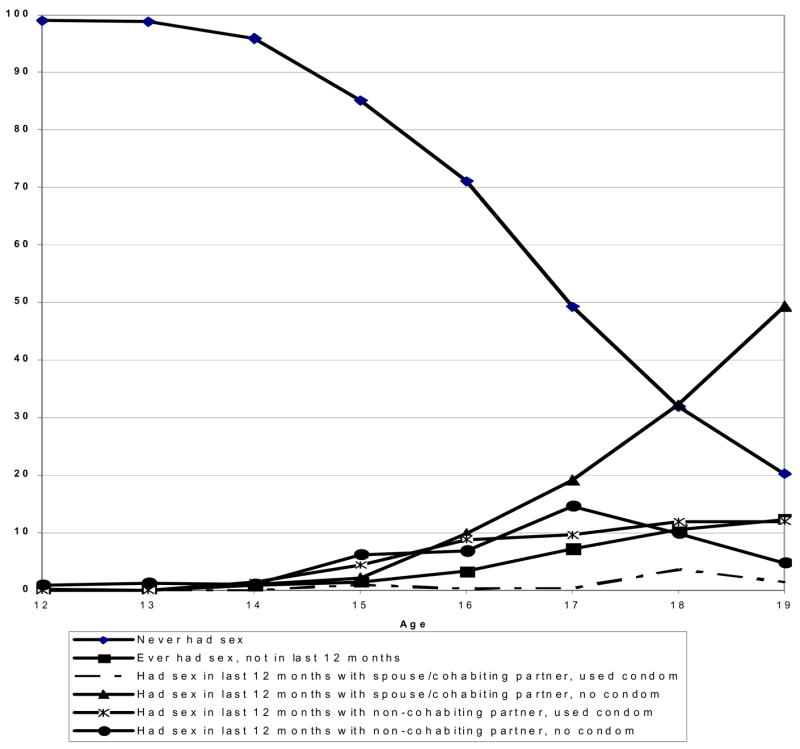
Several reasons were given by older female adolescents who did not use condoms at last sexual act (See figure 3). Among those who were not in union, 28% reported that they felt safe, 10% didn’t have condoms and 18% stated that the partner refused. For those in union, more than 25% stated that they wanted to get pregnant, about 20% said they felt safe, and about 22% said they did not know why they did not use condoms at last sex. Reasons for using condoms at last sexual act vary between male and female adolescents. Females were significantly more likely to cite pregnancy prevention as the reason for use (See figure 4) compared with males (42% and 18%, respectively). Males were two times more likely to mention HIV prevention than females (27% and 13%). For both sexes, more than 4 in 10 cited prevention of both pregnancy and STIs (including HIV) as the main reason for using condoms.
Figure 3.
Reasons for non use of male condom at last sex among girls of 15–19 years olds who have had sex during the last 12 months and did’nt use condom Burkina Faso, National Survey of Adolescents, 2004
Figure 4.
Reasons for using a male condom at last sex among adolescents of 15–19 years olds who have had sex the last 12 months and have used condo Burkina Faso National Survey of Adolescents, 2004
In Table 5, we present the results from the logistic regression models, where the dependent variable was coded as ‘1’ if condoms were used at last sexual act and ‘0’ if no condoms were used. Separate analyses were done for males and females. Adolescents’ attitudes towards condoms and their self-efficacy are the most important factors that are associated with use of condoms. To assess this self-efficacy, the survey asked female adolescents to evaluate their own level of confidence (feeling very confident, somewhat confident and not confident at all) to get their partner to wear a male condom. For males, the question asked them to assess their own level of confidence in knowing how to use a condom. The association between perceived self-efficacy to use condoms and their use was significant. Females who felt very confident in getting their partner to wear a condom had 6 times the odds of using condoms compared to those who were not confident at all. For males, the relationship between knowing how to use a condom and the use at last sex is obvious with those who felt very confident on how to use a condom having 27 times the odds of using condoms compared to those who were not confident at all.
Table 5.
Odds ratios of using condoms at last sexual act among adolescents in Burkina Faso
| Characteristics | Odds ratios and confidence intervals | |
|---|---|---|
| Males (N=435) | Females (N=577) | |
| Type of partner | ||
| Husband/Wife | RC | RC |
| Boy/girlfriend | 4.84 [0.93–25]* | 7.17 [3.95–13.02]*** |
| Casual partner | 3.97 | 6.67 [1.85–24.12]*** |
| Condom reduces pleasure | ||
| Agree | RC | RC |
| Disagree | 1.32 | 0.41 [0.24–0.70]** |
| Use of condoms is a lack of trust | ||
| Agree | RC | RC |
| Disagree | 0.78 | 1.93 [1.12–3.31]** |
| It is embarrassing to buy/ask for condoms | ||
| Agree | RC | RC |
| Disagree | 1.24 | 1.52 |
| Level of confidence to getting partner to wear condoms | ||
| Not confident at all | - | RC |
| Somewhat confident | - | 3.25 [1.61–6.58]** |
| Very confident | - | 6.03 [3.27–11.13]*** |
| Level of confidence to knowing how to wear condoms | ||
| Not confident at all | RC | - |
| Somewhat confident | 10.92 [4.49–26.63]*** | - |
| Very confident | 25.93 [10.95–61.37]*** | - |
| Education level | ||
| None | RC | RC |
| Primary school | 0.88 | 2.72 [1.49–4.95] *** |
| Secondary school and more | 2.77 [1.27–6.07]** | 3.09 [1.43–6.68]*** |
| Residence | ||
| Rural | RC | RC |
| Urban | 2.74 [1.46–5.14]*** | 2.51 [1.45–4.35]*** |
Significant at 1%;
significant at 5%;
significant at 10%; (RC) Reference category
Females’ positive attitudes towards condoms were associated with higher use of condoms. Indeed those who disagreed with the statement that condoms reduce pleasure as well as those who disagreed that the use of condoms is a sign of lack of trust were more likely to have used a condom at last sexual act. Contrary to what one would expect, for males, there was no significant association between these attitudes and the use of condoms at last sex.
To turn to the type of sexual partner, adolescents who had their last sex within a cohabiting union were less likely to have used condoms. For females, those who had sex with a boyfriend and those who had sex with a casual partner were most likely to have used condoms than adolescents in cohabiting union. On the other hand, for males, the relationship was not as clear as what has been observed for females.
The place of residence (urban or rural area) is a significant predictor of use of condoms, with those in urban areas being more than twice as likely to use as those in rural areas. The level of education is also strongly associated with use of condoms among adolescents in Burkina Faso. Indeed, the odds of using condoms increased with years of schooling. Adolescents who achieved a secondary school and higher education were three times more likely to use condoms compared to those without any education.
Discussion
In this paper we sought to present the current “picture” of young people and their sexual risk-taking and protective behaviours in Burkina Faso using recent data from a national survey of adolescents. To achieve the goals set in the National Population Policy and the National HIV/AIDS and STIs programs, the government of Burkina Faso advocates strongly for increased use of reproductive health facilities for adolescents, including youth friendly services. Our findings highlight room for improvement of young people’s awareness and use of condoms to prevent HIV transmission and unwanted pregnancies.
Overall, the use of condoms is low and inconsistent among adolescents. Among those who are using condoms, there are significant differences by social and demographic characteristics. For example, use of condoms for non-cohabiting adolescents is much higher than use within cohabiting unions. This finding is consistent with results from other studies on young adolescents in unions, where the use of condoms is very rare.15–16 On the other hand, one would expect adolescents whose sexual partner is a casual acquaintance to be more likely to use condoms compared to those whose partners are boy/girlfriend but our findings show that they are less likely to use condoms. This finding is consistent with results from an evaluation of a condoms social marketing campaign in urban Mozambique where fewer than half used condoms with casual partners. The authors concluded that the levels of condom use in non-regular partnership were considerably lower than what is needed to stop the HIV epidemic in Mozambique.17 Another recent study on 1300 adolescents of 15–21 years old in a northern hemisphere context (from Miami, Atlanta and Providence in the USA), showed that whether or not they were with a regular or a casual sexual partner, adolescents had similar numbers of unprotected sex acts within a 3-months period.18
A possible interpretation for the low use of condoms among adolescents despite high levels of awareness of HIV/AIDS is that the majority of adolescents do not plan to have sex. Indeed, in the BNAS, a question was asked of the main reason why adolescents had first sex. The finding was that 60% of females aged 12–14 years and 50% of those 15–19 years old said that “it just happened”. The proportions are much higher among males where 74% of those of 12–14 years old and 89% of older adolescents reported that they “just felt like it”. Results from a qualitative study on young people’s sexual behaviour in Burkina Faso also highlight the fact that in many cases sex is not planned but just happens during social events (weddings, birthday parties, special market days)19 so that even if adolescents have positive attitudes about condoms, they may not be readily available to them. Therefore, one can conclude that the majority of adolescents are still engaging in risky behaviours despite their awareness of HIV. This situation has also been shown in another study in Côte d’Ivoire where accuracy of knowledge about AIDS did not significantly predict the use of condoms.15
Our findings also confirm the negative perception of male condoms among adolescents. Indeed, many adolescents continue to state that condoms reduce pleasure during sex. This is consistent with the results of a previous study of 1630 adolescents aged between 13 and 25 years old in Burkina Faso by an NGO in charge of social marketing of condom who found similar levels of 25% of males and 45% of females agreeing that condoms reduce pleasure.20 Even though in the burkinabé context opinions of females are rarely taken into account in decision-making about sexual activity, our findings show that female adolescents’ negative attitudes towards condoms have a negative influence on the use of condoms. Indeed, those who think that using condoms is a sign of lack of trust are less likely to have used a male condom with their partner at last sex. These results are consistent with a study by Lescano et. al. who also reported that adolescents whose partners had negative attitudes towards condoms (for example finding them to be uncomfortable) were less likely to have used them18. Beliefs that one doesn’t have the same feeling during sex when using a condom are common among adolescents. The use of familiar expressions like “you don’t eat banana with its peel”20 or “you don’t take a shower with an umbrella”7 is illustrative of the situation. These attitudes have strong negative influence on condoms use and there is a great challenge for prevention campaigns to develop efficient strategies to convince adolescents that the non use of condoms can jeopardize their lives.
Another important reason for non-use of condoms is that both sexually-active female and male adolescents reported that they felt safe with their partner. Yet, feeling safe depends very much on the type of partner and whether or not there are other concurrent sexual relationships. HIV prevention programs, while emphasizing fidelity, also need to educate adolescents on the importance of taking personal responsibility to remain negative. From the survey, the cost of condoms did not appear to be a major deterrent to their use. The government made a deliberate effort to keep the price of condoms low since 1991. In 2006, the price of condoms rose by 25 CFA (50%) for a packet of four. The effect of this increase should be identifiable in future studies of this nature.
Use of condoms at last sex within a 12–months period is highly associated with adolescents’ self-efficacy towards condoms especially for females. Indeed, for females, the ability to get a partner to wear condoms is a strong predictor of use. Since this was a cross-sectional study, it is possible that condom use may have happened first and the self-efficacy was built afterwards. Alternatively, female adolescents who overcome social and cultural barriers and are able to communicate their needs with partners are more likely to protect themselves. Males who felt very confident in knowing how to use condoms were more likely to have used condoms at last sex compared to those who did not have these life skills at all. Again, the direction of causation cannot be identified from this cross-sectional survey. Despite this limitation, offering practical demonstration of how to use condoms may give the adolescents the needed self-efficacy to promote higher use of condoms.
Rural/urban differences in condoms use can be explained by a combination of factors. Access to condoms in rural areas is less than in urban areas, as is the case for most developing countries. In addition, in the burkinabé context it may be more difficult for a rural adolescent to buy a condom than a city-dweller. Our argument is that in rural areas there is sometimes only one place where adolescents can buy condoms and adolescents may fear to get condoms from this place for fear of the news spreading to others in the village. From our data, rural adolescents aged 12–14 years were significantly more likely to agree that it is embarrassing to buy or ask for condoms than their urban counterpart. Previous studies have shown that for many adults, adolescents and women, a trip to town is often their only opportunity to obtain male condoms or other contraceptive methods, despite the existence of community-based services.21 This suggests that it is critical to develop youth friendly services in rural areas.
The study found also a positive association between schooling and use of condoms with the odds of condoms use increasing with years of schooling. The converse of this finding suggests that the use of condoms among those who were not in school is very low. Given the low level of education in Burkina Faso, it is important to develop programs and strategies to reach out-of-school adolescents so that they too can protect themselves by using condoms and taking advantage of other preventive services.
Adolescents’ sexual behaviour and attitudes towards condoms may be shaped by a range of social, psychological, and cultural factors. This has been demonstrated in urban Cameroon22 and Ghana23 where a supportive social environment was associated with higher use of condoms among youth. Although we were not able to include social environment, psychological, and cultural factors in our analysis, evidence from other studies suggest that socio-cultural factors are the most common barriers to obtaining male condoms among sexually-experienced adolescents in Burkina Faso.12–24 Strong cultural taboos are especially restrictive for sexually active women.
Conclusion
Our findings showed that adolescents attitudes, males’ ability to use condoms, and females’ confidence in getting their partner to use condoms are very important factors associated with the use of condoms among adolescents in Burkina Faso. This last aspect has important implications in a country where females’ views with respect to sexual activity are not regarded highly. HIV prevention programs can contribute to higher use of condoms by focusing on increasing adolescents’ self-efficacy and life skills especially for females. Promoting positive attitudes towards condoms and encouraging adolescents to take responsibility for their own safety are also important strategies for increased use of condoms.
There is also a new critical factor that should be now taken into account: the cost of obtaining condoms has increased in Burkina despite the government and NGOs’ efforts to keep same pricing since 1991. It will be important to investigate the effect of this increase in future studies on condom use among adolescents.
Acknowledgments
The Protecting the Next Generation Project was funded by the Bill & Melinda Gates Foundation, the National Institute of Child Health and Human Development grant # R24 HD43610, and the Rockefeller Foundation. During the writing of this manuscript, the authors were partially supported by a World Bank capacity building grant number 304406-29. The authors are grateful to colleagues at the Institut Supérieur des Sciences de la Population (Burkina Faso), Guttmacher Institute (New York), and the African Population and Health Research Center for their useful comments.
References
- 1.World Health Organization (WHO) Child and adolescent health and development (CAH). Young people-a window of hope in the HIV/AIDS pandemic. Available from: http://www.who.int/child-adolescent-health/HIV/HIV_adolescents.htm.
- 2.Institut National de la Statistique et de la Démographie et ORC Macro. International. Enquête Démographique et de Santé du Burkina Faso 2003. Calverton, MD, USA: Macro International; 2004. [Google Scholar]
- 3.Baya B, et Sangli G. Etude multisite et sur les jeunes de Bobo-Dioulasso, Burkina Faso, Rapport d’analyse des données. Ouagadougou: UERD; 2000. [Google Scholar]
- 4.Biglan A, Wendler C, Ary D, Noell J, Ochs L, French C, Hood D, Wirt R. Social and behavioral factors associated with high-risk sexual behavior among adolescents. Journal of Behavioral Medicine. 1990;13:245–261. doi: 10.1007/BF00846833. [DOI] [PubMed] [Google Scholar]
- 5.Santelli JS, Lindberg LD, Abma J, McNeely CS, Resnick M. Adolescent sexual behaviour: Estimates and trends from four nationally representative surveys, Family Planning Perspectives. 2000;32(n4):156–194. [PubMed] [Google Scholar]
- 6.Measure Evaluation. Indicators for monitoring and evaluation of AIDS programs. Measure Evaluation Bulletin n°2, 2001
- 7.Samuelsen H. Love, lifestyles and the risk of AIDS: The moral worlds of young people in Bobo-Dioulasso, Burkina Faso, Culture, Health & Sexuality. 2006;8(3):211–224. doi: 10.1080/13691050600761185. [DOI] [PubMed] [Google Scholar]
- 8.Amuyunzu-Nyamongo M, Biddlecom AE, Ouedraogo C, Woog V. Protecting the Next Generation: Understanding HIV Risk among Youth. 2005. Qualitative Evidence on Adolescents’ Views of Sexual and Reproductive Health in Sub-Saharan Africa. Occasional Report No. 16. [Google Scholar]
- 9.MacPhail C, Cambell C. ‘I think condoms are good but, aai, I hate those things’: condom use among adolescents and young people in a Southern African township. Social Science and Medicine. 2001;52:1613–1627. doi: 10.1016/s0277-9536(00)00272-0. [DOI] [PubMed] [Google Scholar]
- 10.Maswanya ES, Moji K, Horiguchi I, Nagata K, Aoyagi K, Honda S, Takemoto T. Knowledge, risk perception of AIDS and reported sexual behaviour among students in secondary schools and colleges in Tanzania. Health Education Resources. 1999;14(2):185–196. doi: 10.1093/her/14.2.185. [DOI] [PubMed] [Google Scholar]
- 11.Akwara PA, Madise NJ, Hinde A. Perception of risk of HIV/AIDS and sexual behaviour in Kenya. Journal of Biosocial Science. 2003;35(3):385–411. doi: 10.1017/s0021932003003857. [DOI] [PubMed] [Google Scholar]
- 12.Meekers D, Klein M. (2002), Determinants of condom use among young people in urban Cameroon. Studies in Family Planning. 2002;33 (4):335–346. doi: 10.1111/j.1728-4465.2002.00335.x. [DOI] [PubMed] [Google Scholar]
- 13.Marandu EE, Chamme MA. Attitudes towards condom use for prevention of HIV infection in Botswana. Social Behaviour and Personality. 2004;32(5):491–510. [Google Scholar]
- 14.World Health Organization (WHO) National AIDS programs: A guide to indicators for monitoring and evaluating national HIV/AIDS prevention programs for young people. Geneva: WHO; 2004. [Google Scholar]
- 15.Zellner SL. Condom use and the accuracy of AIDS knowledge in Côte d’Ivoire. International Family Planning Perspectives. 2003;29 (1):41–47. doi: 10.1363/ifpp.29.041.03. [DOI] [PubMed] [Google Scholar]
- 16.Prata N, Morris L, Mazive E, Vahidria F, Stehr M. Relationship between HIV risk perception and condom use: evidence from a population-based survey in Mozambique. International Family Planning Perspectives. 2006;32 (4):192–200. doi: 10.1363/3219206. [DOI] [PubMed] [Google Scholar]
- 17.Agha S, Karlyn A, Meekers D. The promotion of condom use in non-regular sexual partnership in urban Mozambique. Health Policy and Planning. 2001;16 (2):144–151. doi: 10.1093/heapol/16.2.144. [DOI] [PubMed] [Google Scholar]
- 18.Lescano CM, Vazquez EA, Brown LK, Litwin EB, Pugatch D. Condom use with “casual” and “main” partners: what’s in a name? Journal of Adolescent Health. 2006;39(3):443.e1–443.e7. doi: 10.1016/j.jadohealth.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Ouédraogo C, Woog V, Sondo G. Expériences d’adolescents en santé sexuelle et reproductive au Burkina Faso. New York: Guttmacher Institute; 2006. Occasional Report No. 20. [Google Scholar]
- 20.PROMACO. Les jeunes du Burkina face au condom: étude sur les connaissances, attitudes, croyances et pratiques des jeunes de 13 à 25 ans, Rapport final. Ouagadougou: PROMACO; 2001. [Google Scholar]
- 21.Baya B, Guiella G, Ouedraogo C, Pictet G. Community Health Laboratory in Burkina Faso: Assessing a community-based distribution impact in Bazèga, Evaluation report. Ouagadougou: UERD; 1998. p. 69. [Google Scholar]
- 22.Meekers D, Klein M. Determinants of condom use among young people in urban Cameroon. Studies in Family Planning. 2002;33 (4):335–346. doi: 10.1111/j.1728-4465.2002.00335.x. [DOI] [PubMed] [Google Scholar]
- 23.Adih WK, Alexander CS. Determinants of condom use to prevent HIV infection among youth in Ghana. Journal of Adolescent Health. 1999;24 (1):63–72. doi: 10.1016/s1054-139x(98)00062-7. [DOI] [PubMed] [Google Scholar]
- 24.Yaro Y. Evaluation des programmes de santé de la reproduction des adolescents au Burkina, Rapport d’évaluation. CEDPA-FNUAP; 1997. [Google Scholar]