Abstract
Full-scale three-dimensional (3D) models offer a useful tool in preoperative planning, allowing full-scale stereoscopic recognition from any direction and distance with tactile feedback. Although skills and implants have progressed with various innovations, rheumatoid cervical spine surgery remains challenging. No previous studies have documented the usefulness of full-scale 3D models in this complicated situation. The present study assessed the utility of full-scale 3D models in rheumatoid cervical spine surgery. Polyurethane or plaster 3D models of 15 full-sized occipitocervical or upper cervical spines were fabricated using rapid prototyping (stereolithography) techniques from 1-mm slices of individual CT data. A comfortable alignment for patients was reproduced from CT data obtained with the patient in a comfortable occipitocervical position. Usefulness of these models was analyzed. Using models as a template, appropriate shape of the plate-rod construct could be created in advance. No troublesome Halo-vests were needed for preoperative adjustment of occipitocervical angle. No patients complained of dysphasia following surgery. Screw entry points and trajectories were simultaneously determined with full-scale dimensions and perspective, proving particularly valuable in cases involving high-riding vertebral artery. Full-scale stereoscopic recognition has never been achieved with any existing imaging modalities. Full-scale 3D models thus appear useful and applicable to all complicated spinal surgeries. The combination of computer-assisted navigation systems and full-scale 3D models appears likely to provide much better surgical results.
Keywords: Occipitocervical spine, Rapid prototyping, 3D model, Complication, Rheumatoid arthritis
Introduction
Full-scale three-dimensional (3D) models are accepted as a useful tool for preoperative planning [3, 4, 6, 7, 17–19, 21, 23, 24]. Such models have been developed for the aerospace and automotive industries, as models fabricated using rapid prototyping (stereolithography) techniques can reconstruct precise configurations. Full-scale 3D models have also been applied to the medical field, as these techniques can accurately reproduce complicated osseous anatomy.
Full-scale 3D models permit actual stereoscopic understanding of the complex anatomy in each patient, as accurate personal own anatomy can be duplicated from individual computed tomography (CT) data. In the last decade, the usefulness of full-scale 3D models has been reported for oral and maxillofacial surgery [17–19, 21, 23, 24], hip-joint surgery [3, 4] and complex spinal surgery [6, 7]. These models are used to make surface-matched drilling guides and determine surgical plans in advance of osteotomy, to evaluate tumor size and resection area, and so on. Many reports have concluded that full-scale 3D models are useful.
The rheumatoid cervical spine continues to present challenging problems, although innovative progress has been made in surgical skills, implants and results [1, 2, 5, 9–11, 14, 22]. Severe deformities in mutilating rheumatoid spine, very poor bone quality, erosive pedicles and aberrant vertebral artery (VA) are among the inherent risks in connection with rheumatoid cervical spine surgery. Complications have been reported in association with these conditions, such as high frequency of peudoarthrosis and the loosening of wires due to osteoporotic spine [15]. Cervical pedicle screw enables one-stage decompression and reconstruction in the rheumatoid cervical spine [1, 2]. Cervical pedicle screws are biomechanically the strongest, but are highly technically demanding. In rheumatoid patients, a much higher level of technique is required. Safe cervical pedicle screw placement is sometimes obscured due to the existence of an erosive pedicle or aberrant VA. In such situations, elaborate planning is essential to ensure successful surgical results.
If full-scale 3D models offer an advantage in complicated situations, the use of such models should be encouraged, to facilitate better surgical results in rheumatoid cervical spine surgery. No reports have yet described the application of full-scale 3D models in planning rheumatoid spine surgery. The present study assessed the usefulness of these models in preoperative planning for rheumatoid spine surgery.
Materials and methods
Patients and surgical procedures
Full-scale 3D models were custom-made for 15 patients with rheumatoid cervical lesions (2 men, 13 women). All study protocols were approved by the institutional review board of our institute. Patient characteristics are shown in Table 1. Mean age at time of surgery was 60.7 years (range 44–76 years). Occipitocervical or occipitothoracic fixation was performed for all three patients with vertical subluxation and two patients with irreducible atlantoaxial subluxation. Occipitocervical/thoracic fixation was performed using the occipital plate and cervical pedicle screws. Atlantoaxial fixation was performed using the C1 lateral mass and C2 pedicle screws for the remaining ten patients with reducible atlanto-axial subluxation.
Table 1.
Patient’s characteristics
| Case | Age (years) | Gender | Disorders | Note |
|---|---|---|---|---|
| 1 | 53 | F | VS | Ponticulus posticus |
| 2 | 65 | F | VS, SAS | |
| 3 | 72 | F | VS, SAS | |
| 4 | 44 | F | Irreducible AAS | |
| 5 | 59 | F | Irreducible AAS | |
| 6 | 51 | F | Reducible AAS | |
| 7 | 51 | F | Reducible AAS | |
| 8 | 63 | F | Reducible AAS | |
| 9 | 65 | F | Reducible AAS | |
| 10 | 76 | M | Reducible AAS | |
| 11 | 53 | F | Reducible AAS | |
| 12 | 67 | F | Reducible AAS | |
| 13 | 54 | F | Reducible AAS | |
| 14 | 70 | F | Reducible AAS | |
| 15 | 58 | M | Reducible AAS |
AAS atlanto-axial subluxation, F female, M male, SAS subaxial subluxation, VS vertical subluxation
Production of full-scale 3D models
After patients provided informed consent and were informed of the importance and costs of full-scale 3D models, Digital Imaging and Communications in Medicine (DICOM) data were obtained from CT, with 1 mm slices for each patient. During CT, patients lay down with neck position adjusted to remove any discomfort on swallowing and maximize comfort. DICOM data were converted into stereolithography format, and models were produced by Tenpaku-R Corporation (Nagoya, Japan). Appropriate contours of rod and occipitocervical angle were thus reproduced on a full-scale model.
Full-scale 3D models are produced using rapid prototyping (stereolithography) techniques. First, resin powder is sprayed on the platform, and the resin powder is irradiated by laser light and melted down to a mold for one slice of a CT image. The melted resin is sintered to complete 1 layer of resin. The platform then moves down 0.05 mm to mold another layer. Layering is continued until the full-scale 3D model is complete.
Results
In all cases, full-scale 3D models were useful for preoperative planning. First, using the full-scale 3D model, appropriate occipitocervical angle and contour of plate-rod constructs could be determined in preoperative virtual surgery (Figs. 1, 2). Virtual surgery on full-scale 3D models can determine the entire shape of the plate-rod construct. We can simultaneously evaluate mutual positional relationships of the transverse sinus, vertebral artery groove, transverse foramen, and all of the plate/rod/screw positions due to reciprocal surveying from any direction including outer and inner aspect of the occiput. The templating-rod was adapted on the model and then sterilized. In the operating room, an implanting plate-rod construct was created in the same shape as the sterilized templating-rod. The occipitocervical spine was then adapted to the pre-bent plate-rod construct. The shape of the construct thus displayed an alignment optimizing patient comfort, as CT data had been obtained with the patient in a comfortable position. Occipitocervical fusion was thus completed successfully. Postoperatively, no patients complained of dysphagia. And no patients required Halo vest application.
Fig. 1.
Preoperative planning and virtual surgery for occipitocervical fixation. Adequate occipitocervical angle of the plate can be determined in advance. If images from computed tomography (CT) are obtained in a position in which the patient does not feel discomfort while swallowing, the templating plate/rod is bent and fitted to produce the appropriate angle on the full-scale three-dimensional (3D) model. After bringing the sterilized templating plate/rod into the operating room, the true implanting plate/rod construct was bent as the same shape of the templating plate/rod during surgery
Fig. 2.
Postoperative plain radiography. Appropriate plate-rod construct and occipitocervical angle are achieved
Second, the entry point, screw trajectory and length were determined and confirmed simultaneously using full-scale 3D models. To determine screw trajectory, by holding the model in the hand and surveying from any direction and distance, we could determine parameters such as the entry point on the extended line of the pedicle axis, considering pedicle diameter, shape of the facet, and the so-called notch at outer edge of the lateral mass. We could then confirm whether the pedicle diameter was sufficient or not by virtual surgery. From this perspective, full-scale 3D models were superior to reconstructed CT images in providing perspective and synchronized multi-dimensional recognition.
In one patient, modeling revealed that the posterior arch was too thin and narrow to place screws after arch thickness was measured using calipers. Screw placement was therefore altered from via the posterior arch to directly into the lateral mass to avoid misplacement. Even in patients with aberrant VA, steep trajectory of C2 pedicle screws could be confirmed with reference to life-sized transverse foramen and erosive pedicles (Fig. 3, right). And even in one patient with ponticulus posticus, surveying and measuring whether the caudal part of the posterior arch was thick enough to place the screw allowed complete and safe screw placement into the lateral mass of the atlas. In such complicated cases, safe placement of screws could be confirmed by virtual surgery using models (Fig. 4). On traditional 2D CT images using sagittal, coronal and axial planes we were unable to make simultaneous confirmation of screw trajectory, entry point and anatomical deformity. These images had to be mentally “reconstructed” in the imagination of the surgeon. Full-scale 3D models were superior to reconstructed CT images in providing perspective and synchronized multi-dimensional recognition, although we could complete screw planning using traditional 2D CT images.
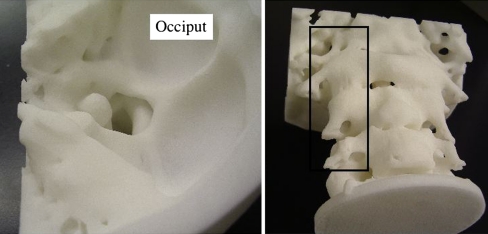
Fig. 3.
Left: full-scale 3D model of vertical subluxation. Basilar impaction of the odontoid peg is clearly apparent in true dimensions. Right: transverse foramen and pedicle are readily surveyed in true perspective
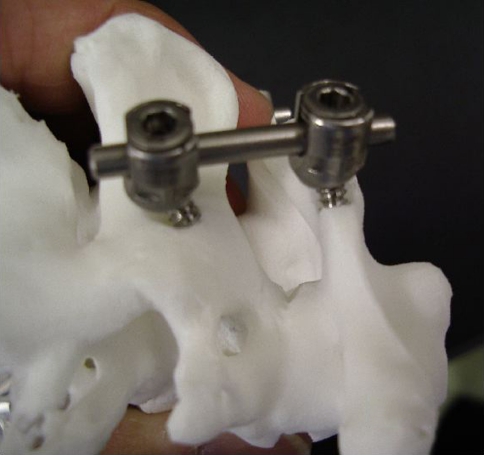
Fig. 4.
Virtual surgery for atlantoaxial fixation. Surgeons can see that insertion of C1 screws is not destroying the posterior arch and that C2 screws are inserted safely, without perforation of the transverse foramen
Discussion
This study found various uses for full-scale 3D models in preoperative planning, with the advantages of planning for occipitocervical fixation appearing among the most significant.
Occipitocervical fusion
Previous reports have mentioned pre-contouring and positioning template-plates on computer-produced models prior to surgery, to facilitate plate application [4]. For the first time, we attempted to apply the templating-rod to full-scale 3D occipitocervical models not only for easy application of the plate-rod construct, but also for the prevention of complications.
One complication of occipitocervical fixation is dysphagia, caused by malpositioning of the occipitocervical plate-rod construct [12, 13]. A Halo vest is usually used to adjust occipitocervical angle preoperatively. This is a good procedure, but application of the Halo vest causes patient discomfort. Recent plate-rod systems are rigid enough that a Halo vest is not needed postoperatively. If adequate plate-rod contours could be determined in advance, preoperative application of Halo vests to adjust and confirm appropriate occipitocervical angle would not be required (Fig. 1). Using a pre-contoured template-rod created on the full-scale 3D model, occipitocervical fusion can be achieved without use of Halo vests in selected patients.
Incorrect location of the plate and improper screw trajectory would also violate the transverse sinus and improperly long screws for the occiput would penetrate the dura mater [8, 16]. Thickness can be evaluated on plain CT, but occipital plate positioning cannot be determined on plain CT, as proper screw length in each screw hole cannot be analyzed simultaneously with suitable perspectives. Even using reconstructed surface model in a computer-aided surgery (CAS) system, a templating-rod cannot be applied. Full-scale 3D models thus offer a useful tool for occipitocervical fixation.
Planning cervical pedicle screwing
Screw trajectory and entry point were easily and simultaneously assessed with full-scale 3D models. With regard to lumbar spine surgery, previous reports have mentioned the usefulness of full-scale 3D models [4], even though placement of lumbar pedicle screws is easy. We emphasize that 3D models facilitate cervical pedicle screwing, which is much more technically demanding and for which failure causes catastrophic complications, such as violation of the VA. Full-scale 3D models allow confirmation of whether safe screw placement is possible in virtual surgery.
Simultaneously comprehensive analysis of anatomical factors and implants with 3D perspective
This study confirmed that models allow a simultaneous understanding of factors such as angle, distance, length, shape and thickness. Reconstructed 3D CT images also offer sagittal, coronal and axial plane images, but the anatomy then must be re-built in the imagination of the clinician. More tangible skeletal anatomy such as with the present models allows simultaneous evaluation of all significant points, including screw entry point, trajectory and length, pedicle diameter, thickness, existing aberrant VA and more. This cannot be achieved using existing imaging modalities. Surgeons gain confidence about completing the highly technically demanding surgery when using full-scale 3D models that offer comprehensive stereoscopic analysis with life-size.
Advantages in combination with CAS system and limitations of full-scale 3D models
The CAS systems have been accepted as a useful tool, but still cannot achieve 100% accuracy of screw placement [20]. Use of a full-scale 3D model alone would likewise not provide 100% safe surgery. Even when using a CAS system, if the patient displays severe deformity, such as in cases involving revision or severe mutilating rheumatoid spine, screw entry points and trajectory can differ substantially from those in more typical cases. Surgeons become confused when the entry points indicated by the CAS system and those intended by the surgeons differ widely, and sometimes encounter unexpected measurement errors beyond fiducial limits due to loosening of tightened reference frames on spinous processes during surgery. Surgeons can become confused that dissociation far from anatomical landmarks is due to some trouble in the CAS system or anatomical abnormality. A full-scale 3D model provides pre- and intraoperative confirmation of abnormal landmarks that can be obscured and difficult to identify.
Conversely, although 3D models offer comprehensive confirmation of screw planning, actualizing the screw trajectory with 100% accuracy cannot be achieved. Further investigation and verification is warranted. During screw insertion, the CAS system can identify and depict real-time screw trajectory. We thus consider that full-scale 3D models combined with a CAS system will offer better surgical results.
Conclusions
Full-scale 3D models are useful in rheumatoid cervical spine surgery. Such models allow preoperative planning as a template, particularly for determining entire plate-rod contours for occipitocervical junctions, avoiding postoperative dysphagia. The biggest advantage of full-scale 3D models lies in the confirmation of any surgical procedure and any anatomy as the surgeon was in the operating room. However, acquisition of this accuracy in actual surgery remains a limitation. Full-scale 3D models combined with a CAS system thus seem likely to provide much better surgical results.
Acknowledgments
We wish to thank Ms.Yoko Sugiyama and Yoko Hirose for secretarial assistance. This study was supported by a Grant-in-Aid for Scientific Research (C: No. 19591728) from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and a Grant-in-Aid for Research from Nagoya City University (EX-3-L, No. 1).
References
- 1.Abumi K, Takada K, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine. 1999;24:1425–1434. doi: 10.1097/00007632-199907150-00007. [DOI] [PubMed] [Google Scholar]
- 2.Abumi K, Kaneda K, Shono Y, Fujiya M. One-stage posterior decompression and reconstruction of the cervical spine by using pedicle screw fixation systems. J Neurosurg. 1999;90:19–26. doi: 10.3171/spi.1999.90.1.0019. [DOI] [PubMed] [Google Scholar]
- 3.Brown GA, Milner B, Firoozbakhsh K. Application of computer-generated stereolithography and interpositioning template in acetabular fractures: a report of eight cases. J Orthop Trauma. 2002;16:347–352. doi: 10.1097/00005131-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Brown GA, Firoozbakhsh K, DeCoster TA, Reyna JR, Moneim M. Rapid prototyping: the future of trauma surgery? J Bone Joint Surg Am. 2003;85A(Suppl 4):49–55. [PubMed] [Google Scholar]
- 5.Chen JF, Wu CT, Lee SC, Lee ST. Posterior atlantoaxial transpedicular screw and plate fixation. J Neurosurg Spine. 2005;2:386–392. doi: 10.3171/spi.2005.2.3.0386. [DOI] [PubMed] [Google Scholar]
- 6.Dick M, Smit TH, Jiya TU, Wuisman PI. Polyurethane real-size models used in planning complex spinal surgery. Spine. 2001;26:1920–1926. doi: 10.1097/00007632-200108010-00008. [DOI] [PubMed] [Google Scholar]
- 7.D’Urso PS, Askin G, Earwaker JS, Merry GS, Thompson RG, Baker et.al TM. Spinal biomodeling. Spine. 1999;24:1247–1251. doi: 10.1097/00007632-199906150-00013. [DOI] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Lu J, Biyani A, Brown JA, Yeasting RA. An anatomic study of the thickness of the occipital bone. Implications for occipitocervical instrumentation. Spine. 1996;21:1725–1729. doi: 10.1097/00007632-199608010-00002. [DOI] [PubMed] [Google Scholar]
- 9.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw, rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 10.Magerl F, Seemann PS, Gallen S. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine 1. New York: Springer; 1987. pp. 322–327. [Google Scholar]
- 11.Matsubara T, Mizutani J, Fukuoka M, Hatoh T, Kojima H, Otsuka T. Safe atlantoaxial fixation using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery. Spine. 2007;32:E30–E33. doi: 10.1097/01.brs.0000250994.24462.ec. [DOI] [PubMed] [Google Scholar]
- 12.Morishita N, Ohota K, Miura Y. The influences of Halo-Vest fixation and cervical hyperextension on swallowing in healthy volunteers. Spine. 2005;30:E179–E182. doi: 10.1097/01.brs.0000157475.47514.75. [DOI] [PubMed] [Google Scholar]
- 13.Garfin SR, Botte MJ, Waters RL. Complication in the use of the halo fixation device. J Bone Joint Surg. 1986;68-A:320–325. [PubMed] [Google Scholar]
- 14.Mizutani J, Tsubouchi S, Fukuoka M, Otsuka T, Matsui N. Surgical treatment of the rheumatoid cervical spine in patients aged 70 years or older. Rheumatology. 2002;41:910–916. doi: 10.1093/rheumatology/41.8.910. [DOI] [PubMed] [Google Scholar]
- 15.Mizutani J, Tsubouchi S, Fukuoka M, Otsuka T, Matsui N. Syringomyelia caused by loosening of multistrand cables following C1–2 Brooks-type fusion in the rheumatoid cervical spine. J Neurosurg. 2002;97(Suppl 3):366–368. doi: 10.3171/spi.2002.97.3.0366. [DOI] [PubMed] [Google Scholar]
- 16.Nadim Y, Lu J, Sabry FF, Ebraheim N. Occipital screws in occipitocervical fusion, their relation to the venous sinuses: an anatomic and radiographic study. Orthopedics. 2000;23:717–719. doi: 10.3928/0147-7447-20000701-20. [DOI] [PubMed] [Google Scholar]
- 17.Nicholas JM, Andrew MC, Noel GS. The display of three-dimensional anatomy with stereolithographic models. J Digit Imaging. 1990;3:200–203. doi: 10.1007/BF03167610. [DOI] [PubMed] [Google Scholar]
- 18.Onishi K, Maruyama Y. Three-dimensional solid model integrated with dental model for maxillofacial surgery. Plast Reconstr Surg. 2001;108:1696–1699. doi: 10.1097/00006534-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 19.Ono I, Abe K, Shiotani S, Hirayama K. Producing a full-scale model from computed tomographic data with the rapid prototyping technique using the binder jet method: a comparison with the laser lithography method using a dry skull. J Craniofac Surg. 2000;11:527–537. doi: 10.1097/00001665-200011060-00004. [DOI] [PubMed] [Google Scholar]
- 20.Seichi A, Takeshita K, Nakajima S, Akune T, Kawaguchi H, Nakamura K. Revision cervical spine surgery using transarticular or pedicle screws under a computer-assisted image-guidance system. J Orthop Sci. 2005;10:385–390. doi: 10.1007/s00776-005-0902-z. [DOI] [PubMed] [Google Scholar]
- 21.Stoker NG, Mankovich NJ, Valentino D. Stereolithographic models for surgical planning: preliminary report. J Oral Maxillofac Surg. 1992;50:466–471. doi: 10.1016/S0278-2391(10)80317-9. [DOI] [PubMed] [Google Scholar]
- 22.Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine. 2003;28:888–895. doi: 10.1097/00007632-200305010-00010. [DOI] [PubMed] [Google Scholar]
- 23.Wagner JD, Baack B, Brown GA, Kelly J. Rapid 3-dimensional prototyping for surgical repair of maxillofacial fractures: a technical note. J Oral Maxillofac Surg. 2004;62:898–901. doi: 10.1016/j.joms.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 24.Winder J, Bibb R. Medical rapid prototyping technologies: state of the art and current limitations for application in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2005;63:1006–1015. doi: 10.1016/j.joms.2005.03.016. [DOI] [PubMed] [Google Scholar]