Abstract
The extent of fusion for degenerative lumbar scoliosis has not yet been determined. The purpose of this study was to compare the results of short fusion versus long fusion for degenerative lumbar scoliosis. Fifty patients (mean age 65.5 ± 5.1 years) undergoing decompression and fusion with pedicle screw instrumentation were evaluated. Short fusion was defined as fusion within the deformity, not exceeding the end vertebra. Long fusion was defined as fusion extended above the upper end vertebra. The lower end vertebra was included in the fusion in all the patients. The short fusion group included 28 patients and the long fusion group included 22 patients. Patients’ age and number of medical co-morbidities were similar in both the groups. The number of levels fused was 3.1 ± 0.9 segments in the short fusion group and 6.5 ± 1.5 in the long fusion group. Before surgery, the average Cobb angle was 16.3° (range 11–28°) in the short fusion group and 21.7° (range 12–33°) in the long fusion group. The correction of the Cobb angle averaged 39% in the short fusion group and 72% in the long fusion group with a statistical difference (P = 0.001). Coronal imbalance improved significantly in the long fusion group more than in the short fusion group (P = 0.03). The correction of lateral listhesis was better in the long fusion group (P = 0.02). However, there was no difference in the correction of lumbar lordosis and sagittal imbalance between the two groups. Ten of the 50 patients had additional posterolateral lumbar interbody fusion at L4-5 or L5-S1. The interbody fusion had a positive influence in improving lumbar lordosis, but was ineffective at restoring sagittal imbalance. Early perioperative complications were likely to develop in the long fusion group. Late complications included adjacent segment disease, loosening of screws, and pseudarthrosis. Adjacent segment disease developed in ten patients in the short fusion group, and in five patients in the long fusion group. In the short fusion group, adjacent segment disease occurred proximally in all of the ten patients. Loosening of distal screws developed in three patients, and pseudarthrosis at L5-S1 in one patient in the long fusion group. Reoperation was performed in four patients in the long fusion group and three patients in the short fusion group. In conclusion, short fusion is sufficient for patients with small Cobb angle and good spinal balance. For patients with severe Cobb angle and rotatory subluxation, long fusion should be carried out to minimize adjacent segment disease. For patients who have severe sagittal imbalance, spinal osteotomy is an alternative technique to be considered. As long fusion is likely to increase early perioperative complications, great care should be taken for high-risk patients to avoid complications.
Keywords: Degenerative lumbar scoliosis, Short fusion, Long fusion
Introduction
Patients with degenerative lumbar scoliosis exhibited a combination of low back pain, leg pain and spinal imbalance [6]. Claudication or radicular pain is caused by spinal stenosis or rotatory subluxation of vertebra. The nerve roots are compressed by pedicular kinking on the concave side or stretched on the convex side. The realignment of the rotatory subluxation contributes to decompression of the nerve root, and results in relief of leg pain [8]. Low back pain is caused by facet joint arthrosis, disk degeneration, and the loss of lumbar lordosis [10]. Sagittal imbalance leads to muscular discomfort and results in low back pain. To relieve low back pain, it is recommended to restore sagittal imbalance.
The goals of surgical treatment for degenerative lumbar scoliosis include relief of leg and back pain, and the correction of deformities. A combination of neural decompression, spinal fusion, and correction of deformities should be performed to achieve the goals of surgical treatment. However, these complex surgeries are accompanied by substantial complications. Degenerative lumbar scoliosis mostly presents in the elderly population [9]. Elderly patients often have medical co-morbidities. Old age and co-morbidities are associated with a higher complication rate. Moreover, long segment fusion and abundant blood loss may increase the incidence of complications [4]. Higher complication rates make it difficult for surgeons to select an appropriate surgical procedure for degenerative lumbar scoliosis.
Several surgical options were performed for the patients with degenerative lumbar scoliosis [7, 13]. Decompression surgery is essential for the symptoms of neurogenic claudication. Most surgeons recommend fusion and instrumentation at the time of decompression [5, 14]. However, no consensus exists for the levels included in the fusion. To our knowledge, there was lack of studies evaluating the results of surgical procedures in patients with degenerative lumbar scoliosis.
The purpose of this study was to compare the clinical and radiographic results of short fusion versus long fusion for degenerative lumbar scoliosis. Our hypotheses were:
Correction of the scoliotic curvature and coronal imbalance would be better in the long fusion group.
Restoration of lumbar lordosis and sagittal imbalance would be better in the long fusion group.
Interbody fusion would be effective in restoring lumbar lordosis and sagittal imbalance.
Complications would be more substantial in the long fusion group.
Improvement of Oswestry disability index would be better in the long fusion group.
Materials and methods
Fifty patients who underwent decompression and fusion with pedicle screw instrumentation for degenerative lumbar scoliosis were evaluated. Two surgeons at two institutions performed the operations. Thirty-three patients had operations at one institution, and 17 patients had them at the other. This study included the patients who had a Cobb angle of more than 10° before surgery. The average age of the patients was 65.5 ± 5.1 years (range 48–83). There were 8 men and 42 women. The average follow-up period was 4.3 ± 1.9 years (range 2–8.9 years) with a minimum 2 years follow up.
Hospital records were reviewed for patients’ medical co-morbidities, smoking history, estimated intraoperative blood loss, operative time, and hospital stay. Hypertension, diabetes, heart disease, pulmonary disease, gastrointestinal disease, and kidney disease were considered to have medical co-morbidities. The number of levels fused and the number of levels decompressed were measured. Complications were defined as any event for which the patient required specific treatment. The complications were categorized as early perioperative (<3 months after surgery) or late complications.
Anteroposterior and lateral radiographs were reviewed preoperatively and at the ultimate follow up periods. The Cobb angle, lumbar lordosis, lateral listhesis of apical vertebra, coronal and sagittal balance were assessed. Lumbar lordosis was measured from the upper endplate of T12 to the endplate of S1. Rotatory subluxation or lateral listhesis was measured by the horizontal distance between the superior-lateral corner of the caudal vertebra and the inferior-lateral corner of the cephalad vertebra. Sagittal balance was measured by C7 sagittal plumb line. Clinical outcomes were assessed with the Oswestry disability index.
Short fusion was defined as fusion within the deformity, not exceeding the end vertebra, though not necessarily including the end vertebra itself in the fusion. Long fusion was defined as any fusion extended above the upper end vertebra. Twenty-eight patients matched the short fusion definition and 22 patients corresponded to long fusion definition.
The statistical analysis was performed using SPSS version 11.5. We used t tests and Pearson chi-square tests. The significance was defined as P < 0.05.
Operative procedures
Fifty patients had undergone posterolateral fusion with autogenous iliac bone graft and segmental pedicle screw instrumentation. The major indications of surgery were claudication and low back pain. All the patients had decompression surgery at the level of spinal stenosis. The most common level of decompression was L3-5 in 14 patients, followed by L2-5 in 8 patients. The number of levels decompressed was 2.6 segments in the short fusion group and 2.8 segments in the long fusion group without statistical difference.
Short fusion was usually performed on the patients who exhibited a small Cobb angle and a minor rotatory subluxation. Long fusion was mostly performed in the patients with a greater Cobb angle and coronal or sagittal imbalance. The restoration of lumbar lordosis and the realignment of spinal imbalance were attempted while performing instrumentation.
Ten patients had supplemental posterolateral lumbar interbody fusion at L4-5 or L5-S1. Three of the ten patients were included in the short fusion group, and the remaining seven patients were included in the long fusion group.
The upper end vertebra was T11 in 2 patients, T12 in 6 patients, L1 in 23 patients, L2 in 17 patients, and L3 in 2 patients. The lower end vertebra was L3 in 9 patients, L4 in 30 patients, and L5 in 11 patients.
Results
The average number of levels fused was 3.1 segments (range 1–5) in the short fusion group and 6.5 segments (range 4–9) in the long fusion group with a statistical difference (P < 0.001). In the short fusion group, the upper instrumented vertebra was L1 in 3 patients, L2 in 15 patients, L3 in 7 patients and L4 in 3 patients. In the long fusion group, the upper instrumented vertebra was T9 in 1 patient, T10 in 12 patients, T11 in 1 patient, T12 in 4 patients, and L1 in 4 patients. The lower instrumented vertebra was L4 in 1 patient, L5 in 24 patients, and S1 in 25 patients. In all the patients, the lower end vertebra was included in the fusion area.
Clinical parameters between two groups (Table 1)
Table 1.
Clinical parameters between short fusion and long fusion
| Short fusion (n = 28) | Long fusion (n = 22) | P-value | |
|---|---|---|---|
| No. of levels fused (n) | 3.1 ± 0.9 | 6.5 ± 1.5 | <0.001 |
| Age (year) | 64.4 ± 8.1 | 66.9 ± 6.4 | 0.23 |
| No. of co-morbidities | 1.7 ± 0.7 | 1.8 ± 0.7 | 0.66 |
| Blood loss (ml) | 1,671 ± 604 | 2,819 ± 1097 | 0.001 |
| Operative time (min) | 179 ± 56.9 | 242 ± 58 | 0.001 |
| Hospital stay (day) | 18.4 ± 8.3 | 23.3 ± 11.2 | 0.1 |
| No. of decompressions | 2.6 ± 0.9 | 2.8 ± 1.0 | 0.5 |
The mean age was 64.4 (range 48–79) in the short fusion group and 66.9 (range 59–84) in the long fusion group with no statistical difference (P = 0.23). The numbers of medical co-morbidities were similar in both the groups. Medical co-morbidities included hypertension in 21 patients, DM in 11 patients, heart disease in 5 patients, liver disease in 4 patients, and pulmonary disease in 4 patients. The mean estimated blood loss was 1,671 ml in the short fusion group and 2,819 ml in the long fusion group with a statistically significant difference (P = 0.001). The mean operative time was 179 min in the short fusion group and 242 min in the long fusion group (P = 0.001).
Radiological parameters between two groups (Table 2)
Table 2.
Radiographic parameters between short fusion and long fusion
| Short fusion (n = 28) | Long fusion (n = 22) | P-value | |
|---|---|---|---|
| Cobb angle (°) | |||
| Preop | 16.3 ± 4.7 | 21.7 ± 6.0 | 0.001 |
| Final | 10.1 ± 5.4 | 6.1 ± 5.5 | 0.01 |
| Change | 6.3 ± 3.4 | 15.7 ± 6.8 | 0.001 |
| Lumbar lordosis (°) | |||
| Preop | 32.7 ± 10.9 | 25.7 ± 14.7 | 0.07 |
| Final | 31.6 ± 12.3 | 22.1 ± 10.4 | 0.05 |
| Change | 0.5 ± 3.6 | 8.7 ± 10.6 | 0.27 |
| Coronal C7 plumb (mm) | |||
| Preop | 7.3 ± 4.1 | 22.7 ± 0 11.4 | 0.03 |
| Final | 3.5 ± 1.4 | 12.8 ± 7.2 | 0.07 |
| Change | 3.7 ± 2.3 | 10.3 ± 7.3 | 0.04 |
| Sagittal C7 plumb (mm) | |||
| Preop | 40.2 ± 36.5 | 61.0 ± 30.7 | 0.03 |
| Final | 36.1 ± 0 41.2 | 66.2 ± 31.1 | 0.06 |
| Change | 4.1 ± 0 22.2 | −6.2 ± 29.0 | 0.06 |
| Lateral listhesis (mm) | |||
| Preop | 3.8 ± 1.6 | 5.2 ± 1.4 | 0.01 |
| Final | 2.0 ± 0.9 | 2.1 ± 1.0 | 0.58 |
| Change | 1.8 ± 1.2 | 3.1 ± 1.2 | 0.02 |
Before surgery, the average Cobb angle was 16.3° (range 11–28°) in the short fusion group and 21.7° (range 12–33°) in the long fusion group with statistical difference. At the last visit, the average Cobb angle was 10.1° in the short fusion group, and 6.1° in the long fusion group. The correction of the Cobb angle averaged 39% in the short fusion group and 72% in the long fusion group. The Cobb angle improved significantly in the long fusion group, more than in the short fusion group with a statistical difference (P = 0.001).
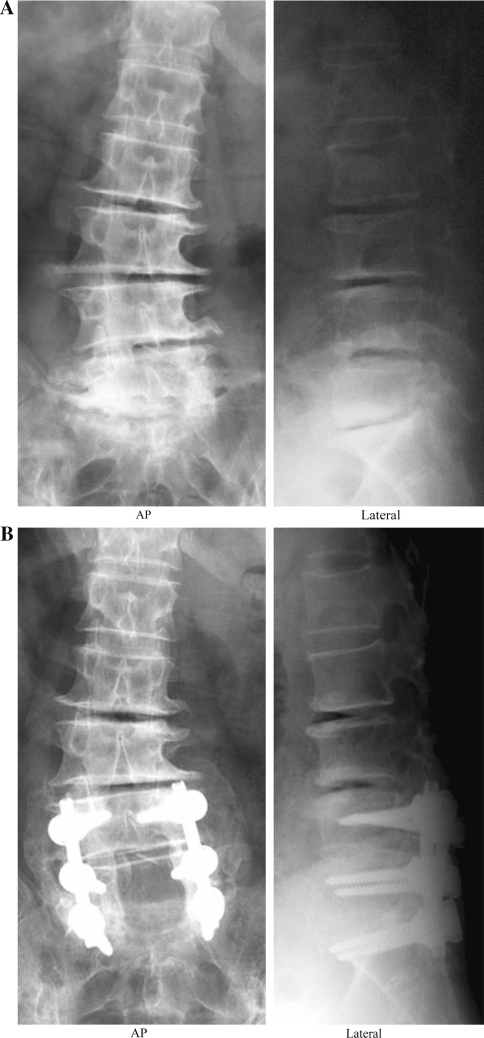
Lumbar lordosis was 32.7° before surgery and 31.6° at the last visit in the short fusion group (Fig. 1). In the long fusion group, it was 25.7° preoperatively, and 22.1° at the last visit. There was no statistical difference in the change of lumbar lordosis between the two groups (P = 0.27). We also evaluated lumbar lordosis in ten patients who received concomitant posterior lumbar interbody fusion. It was 32.1° before surgery and changed to 32.9° after surgery. Posterior interbody fusion had a positive effect in restoring lumbar lordosis.
Fig. 1.
a Preoperative coronal and sagittal lumbar radiographs showing degenerative lumbar scoliosis. The Cobb angle was 17° and lumbar lordosis was 9°. b Coronal and sagittal lumbar radiographs 3 years after surgery. With limited short fusion and posterior instrumentation, both parameters were not changed
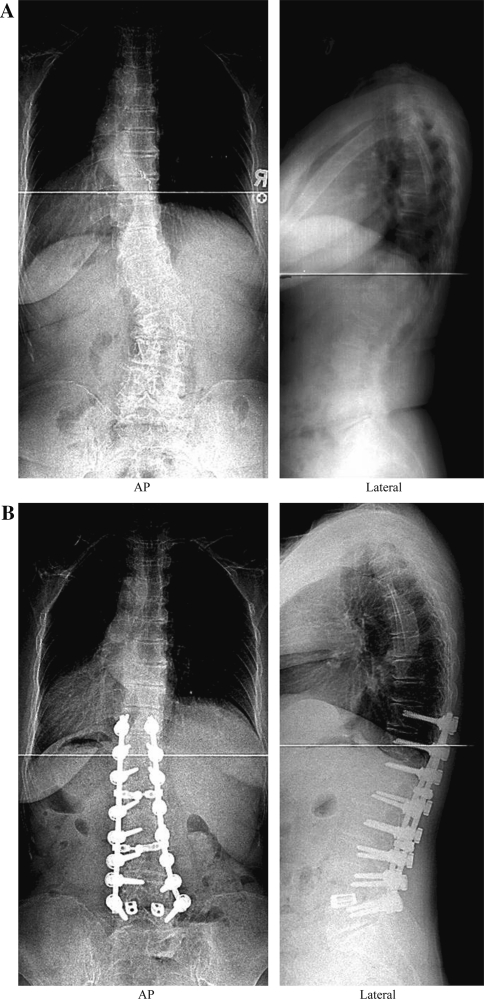
Coronal imbalance was 7.3 mm preoperatively and 3.5 mm at the last visit in the short fusion group. It was 22.7 mm before surgery and corrected to 12.8 mm at the last visit in the long fusion group (Fig. 2). As a result, the correction of coronal imbalance was better in the long fusion group than in the short fusion group with statistical significance (P = 0.04).
Fig. 2.
a Standing long cassette coronal and sagittal radiographs before surgery. The Cobb angle was 35° and lumbar lordosis was 54°. b Standing long cassette coronal and sagittal radiographs 2 years after long fusion and instrumentation with additional posterior interbody fusion at L4-5. The Cobb angle improved from 35 to 2°, and lumbar lordosis changed from 54 to 43°
In contrast, there was no difference in the correction of sagittal imbalance in both groups (P = 0.26). We selected long fusion for patients with severe sagittal imbalance. Before surgery, the average C7 plumb was 40.2 mm in the short fusion group and 61 mm in the long fusion group. The average C7 plumb after surgery was 66.2 mm in the long fusion group. Even with long fusion, however, sagittal imbalance did not improve. We already found that interbody fusion can improve the restoration of lumbar lordosis. Regarding sagittal imbalance, posterior lumbar interbody fusion proved to be ineffective. In ten patients who received interbody fusion, the average sagittal C7 plumb did not improve significantly, improving only from 56.3 ± 30.2 preoperatively to 54.2 ± 38.3 mm postoperatively. Interestingly, patients who had pseudarthrosis and/or adjacent segment disease demonstrated a significantly positive sagittal imbalance. The average sagittal C7 plumb at the last visit was 78.3 ± 41.8 mm in the patients who had late complications, whereas it was 47.2 ± 40.6 mm in the patients who did not have late complications.
Regarding rotational subluxation of the apical vertebra, the preoperative lateral listhesis was 3.8 mm in the short fusion group and 5.2 mm in the long fusion group. After surgery, it was corrected to 2.0 mm in the short fusion group and 2.1 mm in the long fusion group. So the correction of lateral listhesis was much better in the long fusion group (P = 0.02).
Complications (Table 3)
Table 3.
Complications
| Short fusion (n = 28) | Long fusion (n = 22) | |
|---|---|---|
| Total | 15 | 18 |
| Early complications | 5 | 9 |
| Pulmonary embolism | 0 | 1 |
| Ileus | 2 | 1 |
| Urinary tract infection | 1 | 0 |
| Transient delirium | 0 | 2 |
| Epidural hematoma | 0 | 1 |
| Superficial infection | 1 | 1 |
| Respiratory distress syndrome | 0 | 2 |
| Transient neurologic deficit | 1 | 0 |
| Breakdown L5-S1 disk | 0 | 1 |
| Late complications | 10 | 9 |
| Pseudarthrosis | 0 | 1 |
| Loosening of screws | 0 | 3 |
| Adjacent segment ds-proximal | 10 | 2 |
| Adjacent segment ds-distal | 0 | 3 |
Complications were divided into early perioperative (earlier than 3 months after surgery) complications and late complications. There were a total of 15 complications in 28 patients in the short fusion group, and 18 complications in 22 patients in the long fusion group.
Long fusion had more of a tendency to increase the early complication rate than did short fusion. In the long fusion group, there was pulmonary embolism in one patient, epidural hematoma in one patient—which was immediately removed—and respiratory distress syndrome in two patients. The short fusion group included ileus in two patients, urinary tract infection in one patient, and transient neurologic deficit in one patient.
Late complications included adjacent segment disease, pseudarthrosis, and loosening of screws. With reference to adjacent segment disease, only patients exhibiting symptomatic adjacent segment disease were included. The patients with radiographic abnormalities without symptoms were excluded in this study. Symptomatic adjacent segment disease was defined as the recurrence of back pain and/or leg pain after surgery, lasting for more than 6 weeks despite medication. These symptoms were identified by compatible findings on radiographic examinations.
Adjacent segment disease developed in ten patients in the short fusion group and in five patients in the long fusion group. In the short fusion group, all cases of the adjacent segment disease occurred proximally, including spinal stenosis (n = 4), compression fracture (n = 3), junctional kyphosis (n = 2), and lateral translation (n = 1). In the long fusion group, there were adjacent segment diseases proximally in two patients and distally in three patients, including compression fracture (n = 2), spinal stenosis (n = 2), and a herniated intervertebral disc (n = 1). Regarding the proximal fusion level, adjacent segment disease developed proximally in four of seven patients when the fusion stopped at L1. When the fusion extended up to T10, adjacent segment disease occurred in 1 of 12 patients.
Loosening of screws developed in three patients in the long fusion group. Pseudarthrosis was identified at L5-S1 in one patient with long fusion, whereas no pseudarthrosis was noted in the short fusion group. These four patients had posterior instrumentation alone with no anterior column support at L5-S1.
Reoperation was performed in seven patients. In the long fusion group, four patients received reoperation for distal adjacent segment disease in two patients, pseudarthrosis in one patient, and loosening of screws in one patient. In the short fusion group, three patients had a reoperation for proximal adjacent segment disease.
Clinical outcomes (Table 4)
Table 4.
Oswestry disability index
| Short fusion (n = 28) | Long fusion (n = 22) | P-value | |
|---|---|---|---|
| Preop | 65.3 ± 20.4 | 71.0 ± 12.4 | 0.12 |
| Final | 48.6 ± 27.6 | 47.8 ± 17.1 | 0.08 |
| Change | 17.8 ± 12.5 | 24.3 ± 11.3 | 0.14 |
The improvement of the Oswestry disability index was similar in both the groups (P = 0.137). The mean Oswestry disability index improved from 65.3 preoperatively to 48.6 at the last visit in the short fusion group, and in the long fusion group from 71.0 preoperatively to 47.8 at the last visit. There was a significant difference (P = 0.03) in the Oswestry disability index between the patients with late complications and those patients who did not have any late complications. The improvement of the Oswestry disability index was 11.8 in patients with late complications, whereas 19.8 in patients without complications
Discussion
Several surgical options have been used for degenerative lumbar scoliosis, including decompression alone, decompression and limited fusion within the deformity, and decompression and long instrumentation. The procedure of decompression alone is usually not recommended because it can lead to further collapse and instability, especially at the apex of the degenerative curve [1, 11, 14]. Decompression and short fusion within the deformity is performed in instances when a lesser Cobb angle or minimal lateral listhesis of the vertebral body is present. Tribus [13] recommended that the fusion could be limited to the levels decompressed in the patients with no coronal or sagittal imbalance. Long fusion and the correction of deformity are appropriate for patients with a greater Cobb angle in addition to coronal and sagittal imbalance.
It has been considered that the restoration of overall balance of the spine in the coronal and sagittal planes was more important than the correction of scoliosis [11]. Nevertheless, the restoration of lumbar lordosis and sagittal imbalance was not enough with posterior fusion and instrumentation [8, 15]. Daffner and Vaccaro [5] noted that the restoration of sagittal contouring might be difficult to perform in the aged spine when approached only posteriorly. Anterior column support using a structural graft or cage is known to improve lumbar lordosis.
In this study, long fusion and instrumentation proved successful to correct scoliotic curvature and coronal imbalance. We obtained a 39% correction of the Cobb angle with short fusion and a 72% correction with long fusion. But even with long fusion, the correction of lumbar lordosis and sagittal imbalance was insufficient. Posterior lumbar interbody fusion was also found to be ineffective on the restoration of sagittal imbalance. So, in patients with severe sagittal imbalance, there should be preoperative consideration for alternative surgical techniques such as corrective osteotomy.
Determining the extent of the fusion is the most important aspect of this surgery. The following principles were applied [12]: (1) The instrumentation should not end at the level of junctional kyphosis or spondylolisthesis. (2) The level of severe rotatory subluxation should be included in the fusion. (3) To balance the spine, the most horizontal vertebra should be chosen for upper instrumented vertebra.
When the fusion and fixation is confined to limited areas in the deformity, degeneration can be accelerated in the remaining curve and result in adjacent segment disease. If the fusion stops at the level of rotatory subluxation, the subluxation itself would be aggravated after surgery. To prevent adjacent segment problem, it is not recommended to stop a fusion within the deformity. When stopping the fusion at the thoracolumbar junction, adjacent segment disease also develops commonly above the fusion. Instead of stopping at the thoracolumbar junction, extending fusion to T10 or above is more effective at reducing adjacent segment disease. In this study, all cases of adjacent segment disease developed proximally in the short fusion group. In the long fusion, there were two cases of proximal adjacent segment disease and three cases of distal adjacent segment disease.
Another important consideration when deciding fusion level is whether or not to include the lumbosacral junction. In the patient with preexisting pathology at L5-S1, most surgeons decide to fuse to the sacrum. If there is a minimal degeneration at L5-S1, it is controversial whether to fuse or not. Stopping fusion at L5 can lead to subsequent degeneration at L5-S1. If fusion extends to the sacrum, the procedure would be bigger and the rate of pseudarthrosis would increase at the lumbosacral junction [3]. In the present study, subsequent degeneration at L5-S1 was frequent in the long fusion construct. There was adjacent segment disease in three patients at L5-S1. On the contrary, there was no adjacent segment disease at L5-S1 in the short fusion group.
The improvement of Oswestry disability index at the time of study showed no difference in both the groups. Claudication was the most common indication of the surgery. In all patients containing the short and long fusion group, decompression surgery for claudication was performed. It is presumed that patients would be satisfied to the surgery in part once the claudication was eliminated.
The limitations of this study were the relatively short duration of follow-up and differences in scoliotic curve magnitude and sagittal imbalance between two groups. After a minimum of 2 years it was impossible to draw definite conclusions about which method is the better technique. In terms of adjacent segment disease, the degenerated segments may get symptomatic in the future and cause deterioration in the clinical outcome.
Conclusions
Posterior fusion and instrumentation have been used for degenerative lumbar scoliosis. Long segment fusion proved better in correcting scoliotic curvature and coronal imbalance than did short fusion. Long fusion was also of greater advantage to improve rotational subluxation of apical vertebra. Even with long fusion, however, the correction of lumbar lordosis and sagittal imbalance was ineffective. The interbody fusion had a positive effect on improving lumbar lordosis, but was ineffective at restoring sagittal imbalance. Restoration of sagittal imbalance was difficult to perform by posterior instrumentation alone. In these patients with sagittal imbalance, alternative surgical techniques such as corrective osteotomy should be considered preoperatively.
There were substantial complications in both short and long fusion groups. Long fusion induced excessive intraoperative blood loss, which was closely related to the development of perioperative complication. Short fusion had the tendency to develop adjacent segment disease proximally. So, for patients with severe Cobb angle and rotatory subluxation, long fusion should be selected to minimize adjacent segment disease. Long fusion construct may increase the risk of the loosening of screws and pseudarthrosis. Thus, attention to augmentation for fixation should be a consideration to avoid complications related to instrumentation while performing long fusion.
References
- 1.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 2.Bradford DS, Tay DK, Hu SS. Adult scoliosis: operative management, complications, and outcomes. Spine. 1999;24:2617–2629. doi: 10.1097/00007632-199912150-00009. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, Edwards CC, Lenke LG. The pros and cons to saving the L5-S1 motion segment in a long scoliosis fusion construct. Spine. 2003;28:S234–S242. doi: 10.1097/01.BRS.0000092462.45111.27. [DOI] [PubMed] [Google Scholar]
- 4.Carreon LY, Puno RM, Dimar JR, et al. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Daffner SD, Vaccaro A. Adult degenerative lumbar scoliosis. Am J Orthop. 2003;2:77–82. [PubMed] [Google Scholar]
- 6.Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine. 1994;19:1619–1627. doi: 10.1097/00007632-199407001-00011. [DOI] [PubMed] [Google Scholar]
- 7.Gupta MC. Degenerative scoliosis options for surgical management. Orthop Clin N Am. 2003;34:269–279. doi: 10.1016/S0030-5898(03)00029-4. [DOI] [PubMed] [Google Scholar]
- 8.Marchesi DG, Aebi M. Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine. 1992;17:S304–S309. doi: 10.1097/00007632-199208001-00016. [DOI] [PubMed] [Google Scholar]
- 9.Pritchett JW, Bortel DT. Degenerative symptomatic lumbar scoliosis. Spine. 1993;18:700–703. doi: 10.1097/00007632-199305000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Schwab FJ, Smith VA, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27:387–392. doi: 10.1097/00007632-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 11.Simmons ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop. 2001;384:45–53. doi: 10.1097/00003086-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Simmons ED, Simmons EH. Spinal stenosis with scoliosis. Spine. 1992;17:S117–S120. doi: 10.1097/00007632-199201000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11:174–183. doi: 10.5435/00124635-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Vaccaro AR, Ball ST. Indications for instrumentation in degenerative lumbar spinal disorders. Orthopedics. 2000;23:260–271. doi: 10.3928/0147-7447-20000301-21. [DOI] [PubMed] [Google Scholar]
- 15.Zurbriggen C, Markwalder TM, Wyss S. Long-term results in patients treated with posterior instrumentation and fusion for degenerative scoliosis of the lumbar spine. Acta Neurochir (Wien) 1999;141:21–26. doi: 10.1007/s007010050261. [DOI] [PubMed] [Google Scholar]