Abstract
The ventromedial prefrontal cortex (vmPFC) and insular cortex are implicated in distributed neural circuitry that supports emotional decision-making. Previous studies of patients with vmPFC lesions have focused primarily on decision-making under uncertainty, when outcome probabilities are ambiguous (e.g. the Iowa Gambling Task). It remains unclear whether vmPFC is also necessary for decision-making under risk, when outcome probabilities are explicit. It is not known whether the effect of insular damage is analogous to the effect of vmPFC damage, or whether these regions contribute differentially to choice behaviour. Four groups of participants were compared on the Cambridge Gamble Task, a well-characterized measure of risky decision-making where outcome probabilities are presented explicitly, thus minimizing additional learning and working memory demands. Patients with focal, stable lesions to the vmPFC (n = 20) and the insular cortex (n = 13) were compared against healthy subjects (n = 41) and a group of lesion controls (n = 12) with damage predominantly affecting the dorsal and lateral frontal cortex. The vmPFC and insular cortex patients showed selective and distinctive disruptions of betting behaviour. VmPFC damage was associated with increased betting regardless of the odds of winning, consistent with a role of vmPFC in biasing healthy individuals towards conservative options under risk. In contrast, patients with insular cortex lesions failed to adjust their bets by the odds of winning, consistent with a role of the insular cortex in signalling the probability of aversive outcomes. The insular group attained a lower point score on the task and experienced more ‘bankruptcies’. There were no group differences in probability judgement. These data confirm the necessary role of the vmPFC and insular regions in decision-making under risk. Poor decision-making in clinical populations can arise via multiple routes, with functionally dissociable effects of vmPFC and insular cortex damage.
Keywords: risk, uncertainty, orbitofrontal cortex, neuropsychology, emotion
Introduction
Emotional decision-making requires the integration of information about the expected valences, magnitudes and probabilities of available response options. Disruption of these processes may give rise to risk-prone behaviour where choice is driven by positive outcomes that are available, despite possible adverse consequences. These behavioural changes are a common consequence of brain injury, and are also thought to characterize a number of neuropsychiatric disorders including substance use disorders and problem gambling (Paulus, 2007). Considerable insights can be gained into the underlying neural circuitry that supports decision-making from studies of patients with focal brain lesions, as well as functional imaging studies in healthy volunteers. These convergent methods have implicated a distributed circuit including the ventral and medial sectors of the prefrontal cortex, the insular cortex, as well as the striatum, amygdala and parietal cortex (see Clark and Manes, 2004; Ernst and Paulus, 2005; Krain et al., 2006 for review). However, the specific contributions of these regions to successful decision-making remain unclear. In addition, a number of intriguing recent findings from functional imaging remain unsubstantiated by lesion data. Lesion designs (or other interventional techniques like transcranial magnetic stimulation) are a crucial methodology in order to demonstrate the necessary involvement of a brain region in a particular process (Rorden and Karnath, 2004).
The ventromedial prefrontal cortex (vmPFC) has been widely recognized to play a critical role in successful decision-making, fuelled in part by well-studied single cases like Phineas Gage and EVR (Eslinger and Damasio, 1985; Damasio, 1994; Dimitrov et al., 1999; Cato et al., 2004). This area encompasses the medial part of the orbitofrontal cortex (Brodmann areas 10, 11, 12) as well as the more ventral sectors of the medial prefrontal cortex and anterior cingulate cortex (Brodmann areas 24, 25, 32). Patients with vmPFC damage commonly display a syndrome that includes poor judgement, socially inappropriate behaviour and impulsivity (Damasio, 1994; Berlin et al., 2004). These patients exhibit maladaptive choice on a laboratory test known as the Iowa Gambling Task (Bechara et al., 1994), where subjects are required to learn the profile of wins and losses associated with four card decks. Two decks (the ‘risky’ decks) yield high immediate wins, but with dramatic occasional losses that result in gradual debt over time. The other two (‘safe’) decks deliver smaller wins but with minor losses, such that there is an overall profit. Whilst healthy controls rapidly learn to select from the safe decks, patients with vmPFC damage fail to learn an advantageous strategy and maintain preference for the risky decks (Bechara et al., 1994, 2000). Their behaviour is driven by the short-term benefits associated with the risky decks, without regard for the longer-term negative consequences; a profile labelled ‘myopia for the future’ (Bechara et al., 1994, 2000).
The insular cortex may also play an important role in emotional decision-making, via its extensive reciprocal connectivity with the vmPFC (Augustine, 1996; Ongur and Price, 2000), as well as the amygdala and ventral striatum (Reynolds and Zahm, 2005). The Somatic Marker Hypothesis proposed that during decision-making, bodily states that were previously associated with choice options were retrieved by the vmPFC, and that the somatic and visceral representations themselves are held in the insular and somatosensory cortices (Damasio, 1994; Bechara and Damasio, 2005). Consistent with this theory, functional magnetic resonance imaging (fMRI) studies in healthy volunteers have reported activation of the anterior insular cortex immediately prior to risk-averse decisions (Kuhnen and Knutson, 2005), and correlating with the uncertainty of monetary reward (Critchley et al., 2001), overall risk preference (Paulus et al., 2003) and reward variance (Preuschoff et al., 2006). Such findings are broadly consistent with a wider role of the anterior insular cortex in signalling the expectancy of aversive outcomes (O’Doherty et al., 2003; Paulus and Stein, 2006), for example, in the anticipation of painful stimuli (Ploghaus et al., 1999) or unpleasant visual stimuli (Simmons et al., 2004). There is a paucity of lesion data to substantiate these findings from functional imaging, in order to demonstrate the necessary role of the insular cortex in decision-making. One study reported impaired ‘emotional intelligence’ and impaired performance on the Iowa Gambling Task in three patients with right insular cortex damage, who were included as a part of a ‘target’ group of patients with damage to brain areas involved in emotional processing (Bar-On et al., 2003). The primary aim of the present study was to further characterize impairments in decision-making in a larger group of cases with damage to the insular cortex.
Recent work has also highlighted a fundamental distinction that has been made between decision-making under risk versus decision-making under ambiguity. In decision-making under risk, the outcomes are uncertain but the outcome probabilities are known (Camerer and Weber, 1992). In ambiguous decisions, the outcomes are uncertain and the outcome probabilities are unknown or estimated. As players begin the Iowa Gambling Task, the contingencies of the four decks are unspecified, and as the task progresses, the trial by trial outcomes enable the outcome probabilities to be estimated. Imaging studies of the Iowa Gambling Task indicate recruitment of vmPFC during decision-making under ambiguity (Fukui et al., 2005; Northoff et al., 2006; Windmann et al., 2006). However, two recent functional imaging studies that compared decision-making under risk and ambiguity, reported activation in the lateral aspects of the frontal cortex during decision-making under ambiguity, contrasting with activation of posterior parietal cortex (Huettel et al., 2006) and striatum (Hsu et al., 2005) during decisions under risk. From these findings, we might expect frontal lesion patients to be unimpaired in decision-making with known probabilities. This is incongruent with the clinical phenomenology of vmPFC lesions, and in addition, other functional imaging studies indicated vmPFC recruitment during risky decision-making when outcome probabilities were known (Rogers et al., 1999b, 2004; Ernst et al., 2004), supported by meta-analysis (Krain et al., 2006). Studies have also reported changes in risk-taking on a task with known outcome probabilities following prefrontal cortical electrical stimulation in healthy volunteers (Knoch et al., 2006; Fecteau et al., 2007). Thus, the second aim of the present study was to examine the effects of vmPFC lesions on decision-making under risk, using a test with known outcome probabilities.
In the Cambridge Gamble Task, the subject is presented with an array of 10 red and blue boxes and the subject is instructed that the computer has hidden a token under one of the boxes. After guessing whether the token is hidden in a red or blue box, the subject is asked to wager a proportion of their points on that decision. Potential wagers are offered in an ascending or descending sequence that enables the separation of impulsive response tendencies from genuine risk preference (risk-preferent subjects must wait to place high wagers in the ascend condition) (Miller, 1992). Outcome probabilities of winning and losing are provided explicitly by the ratio of red to blue boxes, and thus the task assesses decision-making under risk rather than ambiguity. A further advantage of this design is that demands for stimulus-reinforcement learning, reversal learning (Fellows and Farah, 2005) and working memory (Hinson et al., 2002) are minimized. Increases in betting behaviour on the task have been shown previously in patients with frontal-variant frontotemporal dementia (Rahman et al., 1999), subarachnoid haemorrhage of the anterior communicating artery (Mavaddat et al., 2000) and patients with large frontal lesions that included the orbitofrontal cortex (Manes et al., 2002). These groups share pathology in the vmPFC; however, in none of these studies was the vmPFC selectively affected. The study by Manes et al. (2002) included five patients with focal orbitofrontal lesions who did not differ from healthy controls on either the Cambridge Gamble Task or the Iowa Gambling Task, but it may be notable that 4/5 cases in this group had left-sided unilateral damage (Tranel et al., 2002; Clark et al., 2003). Focal lesions of the dorsolateral or dorsomedial PFC impaired Iowa Gambling Task performance but did not significantly affect performance on the Cambridge Gamble Task (Manes et al., 2002). The present study sought to explore the differential effects of focal damage to the vmPFC and the insular cortex, on risky decision-making on the Cambridge Gamble Task. We hypothesized that patients with vmPFC and insular cortex lesions would both display increases in betting behaviour in comparison with healthy volunteers and a lesion control group with damage predominantly affecting the dorsolateral and ventrolateral PFC.
Methods
Subjects
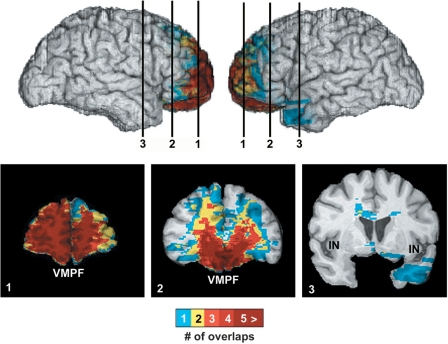
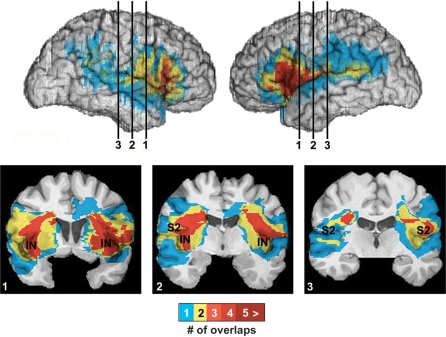
Neurological patients with focal lesions to the vmPFC (n = 20), the insular cortex (n = 13) and lesion controls (n = 12) were administered the Cambridge Gamble Task. Lesion patients were recruited from the Patient Registry in the Department of Neurology at the University of Iowa. All patients had focal, stable, adult-onset lesions sustained at least 1 year prior to testing, and had previously undergone extensive screening and evaluation with background measures of neuropsychological function, reported previously in Bechara et al. (1998), Tranel et al. (2005) and Bar-On et al. (2003). Exclusion criteria were a history of mental retardation, learning disability or psychiatric illness including substance abuse. Patients were selected for eligibility on the basis of neuroanatomical status obtained from MRI or computed tomography (CT) scanning (see Neuroanatomical analysis section subsequently). In the vmPFC group, the criterion for inclusion was damage in the unilateral or bilateral portions of the mesial orbital/ventromedial sector of the prefrontal cortex and/or the frontal pole (Fig. 1). Lesion aetiology in the vmPFC group was haemorrhage due to ruptured aneurysm of the anterior communicating artery or tumour resections, and the group including a mixture of bilateral (n = 10), right unilateral (n = 6) and left unilateral (n = 4) lesions. In the insular cortex lesion group, the lesion involved damage to any part of the insular cortex (anterior and/or posterior) and/or the adjacent secondary somatosensory cortex (SII) (Fig. 2). In the insular lesion group, lesion aetiology was haemorrhage in all cases, and all lesions were unilateral (left n = 6, right n = 7).
Fig. 1.
Lesion overlap in the vmPFC lesion group, in views of the right and left lateral surfaces, and coronal sections at three points moving from anterior (1) to posterior (3) within the frontal lobes. The colour bar indicates the number of overlapping cases at each voxel. There is maximal lesion overlap across the group in the ventral and medial aspect of the prefrontal cortex, comprising Brodmann areas 10, 11, 13, 14, 25 and 32. There was no damage to the insular cortex (IN).
Fig. 2.
Lesion overlap in the insular cortex lesion group, in views of the right and left lateral surfaces, and coronal slices at three points moving anterior (1) to posterior (3) within the insular–somatosensory region. The colour bar indicates the number of overlapping cases at each voxel. Whilst all cases had unilateral lesions, the area of damage in the right- and left-sided cases was highly symmetrical. There is maximal lesion overlap across the group in the anterior insular cortex and somatosensory SII region, extending posteriorly into the inferior parietal cortex in some subjects.
The lesion control group involved unilateral damage to any part of the dorsolateral and/or ventrolateral sector (including lateral orbital) of the prefrontal cortex, but spared damage to any part of the insular cortex, SII cortex, mesial orbital/ventromedial prefrontal cortex and frontal pole (Supplementary Fig. 1). The most important criterion for the lesion control group was that the lesion did not include any insular cortex or mesial orbital/ventromedial prefrontal cortex damage. The lesion controls had unilateral damage that was mostly due to strokes and a few tumour resections. The three lesion groups were compared with 41 healthy comparison subjects who were recruited through community advertising. Demographic characteristics of the four groups are displayed in Table 1.
Table 1.
Demographic characteristics of the four groups [mean (SD)]
| Controls | vmPFC | Insular | Lesion controls | |
|---|---|---|---|---|
| N | 41 | 20 | 13 | 12 |
| Age | 50.7 (10.9) | 54.2 (14.3) | 57.3 (11.0) | 59.2 (14.3) |
| Gender | 21M : 20F | 11M : 9F | 7M : 6F | 6M : 6F |
| Education | 14.4 (2.9) | 13.2 (1.9) | 13.5 (2.8) | 15.7 (5.1) |
| Years post-lesion | – | 9.9 (9.3) | 15.8 (13.1) | 11.6 (12.9) |
All subjects were tested in quiet laboratory conditions with task responses recorded via a touch-sensitive monitor. The study was approved by the human subjects committee at the University of Iowa. Before enrolment in the study, written informed consent was acquired in accordance with the Declaration of Helsinki.
Neuroanatomical analysis
Lesion location was generally confirmed using MRI, with a 1.5 T General Electric scanner with a spin gradient sequence, in 1.5 mm contiguous T1-weighted coronal slices. MRI scanning was not possible in some vmPFC patients due to clipped aneurysms, and a CT scan was acquired instead using either a Picker 1200 or Toshiba Express SX scanner, with tilt angle optimized per subject to avoid clip-related artefact (zoom 2.4, field of view 51 cm, fovea 212.5 mm, slice thickness 2–4 mm). Lesions of individual patients were transferred manually onto a normal reference brain using the MAP-3 technique (Damasio and Frank, 1992; Damasio, 1995; Frank et al., 1997). In brief, the method entails the following: (i) a normal 3D brain that is sliced in such a way that the slices match the slices of the MR/CT scan of the subject with the brain lesion; a match between the slices of the two brains is thus created; (ii) the contour of the lesion is transposed onto the slices of the normal brain, taking into consideration the relation of the lesion and the identified pertinent anatomical landmarks; (iii) for each lesion the set of contours constitutes an ‘object’ that can be co-rendered with the normal brain. The ‘objects’ corresponding to the different lesions in the group can intersect in space, and thus yield a maximal overlap relative to both surface and depth extension of damage. The number of subjects contributing to the overlap is known in each case.
Cambridge Gamble Task
The task was performed on a desktop PC with responses recorded via a touch-sensitive screen. Subjects completed four practice trials of the task, followed by eight blocks of nine trials, where at the start of each block, their total points was re-set to 100 points. The screen display is shown in Fig. 3. On each trial, the participant was presented with an array of 10 boxes, each coloured red or blue. The ratio of red:blue boxes varied from 1 : 9 to 9 : 1, in a pseudo-random order. The participant was instructed that the computer had hidden a token in one of the boxes, and they must guess where the token was hidden. First, they must choose whether they think the token is hidden under a red box or a blue box, by selecting one of the two coloured panels (‘RED’ or ‘BLUE’) at the foot of the screen. Judgement data were analysed in terms of the proportion of choices to the colour in the majority, and the deliberation time to make this decision was recorded. Second, the subject must gamble some points on their Red/Blue decision. Possible bets were displayed on the right-hand side of the screen in a sequence, and the subject could touch this box at any point to place their bet. Subjects completed four task blocks with bets presented in an ascending sequence, and four blocks with bets presented in a descending sequence. Available bets were offered as a proportion of their points on that trial (ascend condition: 5, 25, 50, 75 and 95%; descend condition: 95, 75, 50, 25 and 5%), presented in 5 s increments. If no bet was chosen, the final bet in the sequence was selected automatically. Comparison of the ascend and descend conditions enables an assessment of impulsive or delay-averse response tendencies. Impulsive/delay-averse subjects will place low bets in the Ascend condition, coupled with high bets in the Descend condition, whereas risk-preferent subjects will have to delay their response to place high bets in the Ascend condition. After the bet was selected, the hidden box was revealed. If the subject had chosen correctly, the bet was added to their current total, enabling higher wagers to be placed on the subsequent trial. Following incorrect choices, the bet was subtracted from the current total. Betting data were analysed in terms of the percentage of points staked, on trials where the participant selected the colour in the majority. Subjects were instructed to ‘Try to win as many points as you can’, and that the block would be terminated if their total points dropped as low as 1 point (a ‘bankruptcy’).
Fig. 3.
Schematic showing the screen display for the Cambridge Gamble Task.
Behavioural analysis
Behavioural data on the Cambridge Gamble Task were analysed using mixed-model analysis of variance (ANOVA) models with group (healthy controls, vmPFC lesion, insular cortex lesion and lesion control group) as a between-subjects fixed factor, and condition (Ascend, Descend) and ratio (9 : 1, 8 : 2, 7 : 3, 6 : 4) as within-subjects factors, using two sets of dependent variables: (i) mean percentage of points bet (‘betting behaviour’), and mean deliberation time to make colour choice (‘response latency’) (these variables conformed to assumptions of normality and were therefore appropriate for parametric statistics). The Greenhouse–Geisser correction was applied where sphericity was violated. Choice behaviour, in terms of the proportion of choices to the box colour in the majority, was highly negatively skewed, with many subjects selecting the likely outcome on the large majority of trials. These data could not be successfully transformed to achieve normality, and were consequently analysed with non-parametric Kruskal–Wallis tests in each condition, collapsing across box ratio.
Trials with a 5 : 5 ratio of red-blue boxes were included in the task design to ensure that participants perceived the task as a random trial sequence, but these trials were excluded from statistical analysis. Analysis of betting behaviour was also limited to trials where the subject selected the colour in the majority, to maintain independence of betting behaviour and choice behaviour. Between-group effects in the ANOVA models were analysed as follows. A planned comparison between the healthy control and lesion control groups was used to detect any difference in performance. Providing there was no evidence of a difference between the two control groups (at the liberal threshold of α = 0.25), they were pooled together for subsequent analysis. In the resulting three-group model, significant between-group effects were investigated using pair-wise comparisons with Fisher's LSD procedure, which is the most powerful technique for post hoc tests involving three groups (Cardinal and Aitken, 2006). Effect sizes for the group comparisons were calculated using Cohen's d, i.e. the difference between the means divided by the pooled SD (Cohen, 1988). Figure 5B and Supplementary Fig. 2B display a risk adjustment score to indicate the extent to which betting behaviour was moderated by the ratio of boxes, calculated using the formula 2a + b − c − 2d where a is the 9 : 1 ratio and d is the 6 : 4 ratio.
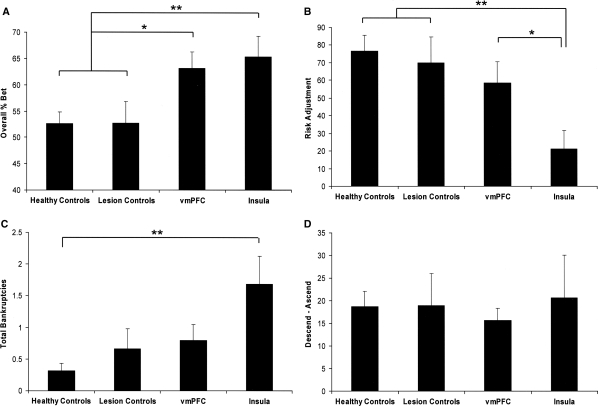
Fig. 5.
(A) Increased betting behaviour (collapsed across the ascending and descending conditions, and the ratio of boxes) in both the vmPFC and insular cortex lesion groups. Statistical differences against pooled control group: *P < 0.05 **P < 0.005. (B) Risk adjustment (calculated by the equation 2a + b − c − 2d, where a is the mean bet at the 9 : 1 ratio, b is the mean bet as the 8 : 2 ratio, etc.) collapsed across ascending and descending conditions, was selectively reduced in the insular cortex lesion group: these patients moderated their betting less as a function of the ratio of boxes than the other groups. **P < 0.005 against pooled control group. (C) The insular cortex lesion group experienced significantly more bankruptcies than healthy controls, where the total points dropped to 1 point within a block (Mann–Whitney non-parametric test **P < 0.005). (D) All groups placed higher bets in the descending condition (where the initial bets offered are high) than the ascending condition (where the initial bets offered are low), but the extent of this delay aversion did not differ between groups.
Results
Demographic characteristics of the four groups are displayed in Table 1. There were no significant differences between the groups in terms of age [F (3,82) = 1.98, P = 0.123], gender (χ2 = 0.116, df = 3, P = 0.990) or years of education [F (3,82) = 1.86, P = 0.145]. The three lesion groups did not differ significantly in the time since lesion onset [F (2,38) = 0.946, P = 0.397].
Betting behaviour
Lesions to the vmPFC and insular cortex produced selective and distinctive deficits on the Cambridge Gamble Task (Figs 4 and 5, and Table 2). A mixed-model ANOVA of betting behaviour (% points bet) contrasting the four groups, two conditions (ascend, descend) and four ratios (9 : 1, 8 : 2, 7 : 3, 6 : 4) as fixed factors revealed a significant main effect of group [F (3,82) = 4.45, P = 0.006]. There was a significant main effect of condition [F (1,82) = 48.0, P < 0.0001] due to higher betting in the Descend condition than the Ascend condition, but the condition interaction terms and 3-way interaction term were non-significant (all F < 1.13), indicating the betting group differences in betting were not due to motor impulsivity or delay-averse responding on the task (Fig. 5D). In addition, there was a significant main effect of ratio [F (3,246) = 66.4, P < 0.0001] and a significant ratio × group interaction effect [F (9,246) = 3.25, P = 0.012, Greenhouse–Geisser corrected ε = 0.488]. Overall, subjects placed higher bets at the more favourable ratios (i.e. 9 : 1 > 6 : 4), but from inspection (Fig. 4) this risk adjustment effect was attenuated specifically in the insular cortex lesion group. In a mixed model ANOVA, the appropriate error term for comparing two groups is that from a restricted model including only these groups (Cardinal and Aitken, 2006). An analysis contrasting betting in the vmPFC and healthy control groups (collapsing across condition) confirmed a significant main effect of group [F (1,59) = 7.37, P = 0.009] but the group × ratio interaction was not significant in this analysis [F (3,177) = 1.46, P = 0.257]. Thus, the vmPFC patients placed higher bets than healthy controls across all ratios, but adjusted their betting to a similar degree. In contrast, when the insular cortex and healthy control groups were compared, both the main effect of group [F (1,52) = 7.95, P = 0.007] and group × ratio interaction term were significant [F (3,156) = 9.13, P = 0.001 Greenhouse–Geisser corrected ε = 0.481]. Crucially, when vmPFC and insular cortex groups were compared directly, there was a significant group × ratio interaction effect [F (3,93) = 4.23, P = 0.032 Greenhouse–Geisser corrected ε = 0.485] but the main effect of group did not approach significance [F (1,31) = 0.210, P = 0.650]. Thus, whilst elevated betting was apparent in both the vmPFC and insular cortex lesion groups, the significant group × ratio interaction term in the omnibus ANOVA can be explained by reduced risk adjustment in the patients with insular cortex lesions but not vmPFC lesions.
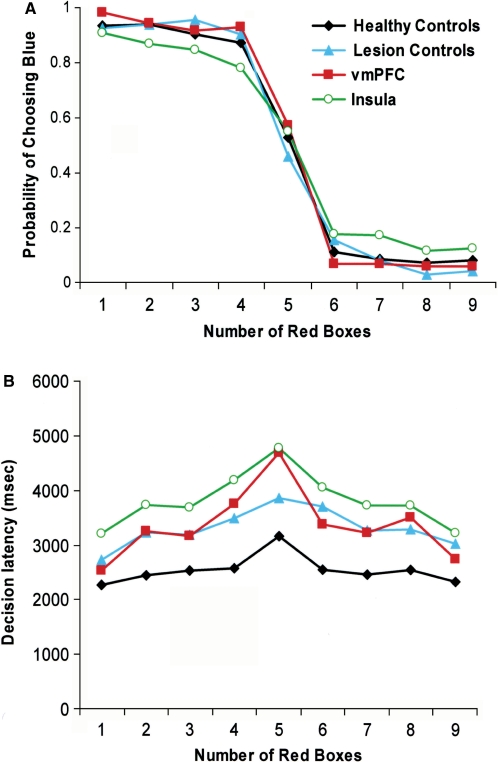
Fig. 4.
The effect of ratio on betting behaviour in the four groups of participants: healthy controls, vmPFC lesions, insular cortex lesions and the lesion control group.
Table 2.
Behavioural performance [mean (SD)] on the Cambridge Gamble Task, collapsed across all ratios of boxes
| Controls | vmPFC | Insular | Lesion controls | |
|---|---|---|---|---|
| Betting (% points available) | ||||
| Ascend | 43.3 (17.0) | 55.3 (15.5) | 55.1 (23.7) | 42.4 (18.9) |
| Descend | 62.0 (18.6) | 71.0 (14.7) | 75.8 (20.0) | 63.0 (19.1) |
| Judgement (proportion likely choice) | ||||
| Ascend | 0.90 (0.13) | 0.92 (0.13) | 0.84 (0.17) | 0.91 (0.12) |
| Descend | 0.92 (0.12) | 0.95 (0.07) | 0.85 (0.15) | 0.93 (0.11) |
| Deliberation time (ms) | ||||
| Ascend | 2367 (961) | 3306 (1276) | 3785 (1544) | 3238 (1486) |
| Descend | 2451 (1088) | 3049 (1614) | 3441 (1126) | 3237 (1547) |
| Total earnings | 3412 (1828) | 2913 (1535) | 1736 (1522) | 2947 (1560) |
The healthy control and lesion control groups did not differ significantly in their overall betting behaviour (t51 = 0.022, P = 0.983) or risk adjustment (t51 = 0.366, P = 0.716), thus these were combined to give a pooled control group for the purpose of between-groups analysis. Overall betting was elevated in both the vmPFC (P = 0.006, Cohen's d = 0.74) and insular cortex (P = 0.004, Cohen's d = 0.90) lesion groups compared with the pooled control group, with no difference between the vmPFC and insular cortex groups (P = 0.652, Cohen's d = 0.16). In contrast, the risk adjustment variable was significantly reduced in the insular cortex lesion group compared with both the pooled control group (P = 0.001, Cohen's d = 1.05) and the vmPFC lesion group (P = 0.046, Cohen's d = 0.79), and did not differ between the vmPFC and pooled control group (P = 0.229, Cohen's d = 0.31) (Fig. 5). The distributions of individual data-points for betting behaviour showed clear separation of the vmPFC and insular cortex cases from the healthy controls and lesion controls (Supplementary Fig. 2A). In contrast, the distributions of risk adjustment scores show clear separation of the insular cortex cases from each of the other three groups, with 12/13 cases scoring below the lower bound for the 95% confidence interval (CI) for the mean of the healthy control group (Supplementary Fig. 2B). An analysis of betting behaviour in relation to lesion laterality in the vmPFC and insular cortex groups did not reveal any significant effects (Supplementary Table 2).
Choice behaviour and overall performance
The four groups performed similarly in terms of choice behaviour, selecting the favourable odds on the vast majority of trials (85–94%, on average). This indicates basic processing and comprehension of the displayed trial-by-trial probabilities (Fig. 6). Whilst the insular cortex lesion group selected the colour in the majority least often (95% CI for ascend condition 0.73–0.94, descend condition 0.76–0.95), there were no significant differences between groups in either the ascend (Kruskal–Wallis χ2 = 2.86, P = 0.415) or descend (χ2 = 6.51, P = 0.089) condition. There was a significant effect of group on the response latency to make the colour decision [F (3,82) = 6.06, P = 0.001], where all three lesion groups took longer to deliberate compared with controls (vmPFC P = 0.008, insula P < 0.0001, lesion controls P = 0.021). The effect of ratio upon response latency was also significant [F (3,246) = 28.5, P < 0.0001] due to faster responding at more favourable odds, but there were no significant interactions with group status. It seems likely that this effect on deliberation may reflect non-specific psychomotor slowing after brain injury.
Fig. 6.
(A) Proportion of choices of the box colour ‘blue’ as a function of the number of red boxes in the array (1–9), in the vmPFC, insular cortex, lesion control and healthy control groups. When blue boxes were in the majority (i.e. number of red boxes was 1–4), subjects in all four groups reliably selected ‘blue’. When red boxes were in the majority (i.e. number of red boxes was 6–9), subjects in all four groups reliably selected ‘red’. Given this intact processing of basic trial-by-trial probabilities, the differences in betting behaviour in the vmPFC and insular cortex groups are assumed to reflect differences in risk processing. (B) Decision latencies (in milliseconds) to select ‘red’ or ‘blue’ as a function of the number of red boxes in the array (1–9).
Post hoc analyses examined the impact of the increases in betting behaviour upon overall task performance. One-way ANOVA of the total points earned on the task indicated a significant group difference [F (3,82) = 3.27, P = 0.025]. The healthy control and lesion control groups did not differ (t51 = 0.799, P = 0.428), and when the control groups were pooled together, earnings were reduced in the insular cortex lesion group compared with the pooled controls (P = 0.003), but not in the vmPFC group (P = 0.375) (Table 2). Performance can also be assessed by examining the number of blocks ending in ‘bankruptcy’ (Mavaddat et al., 2000). This occurs if the total score reaches ≤1 point during a block, whereupon the block is terminated. Non-parametric analysis of the total number of bankruptcies (maximum 8) indicated a significant difference between groups (Kruskal–Wallis χ2 = 13.1, df 3, P = 0.004), due to a significant pair-wise difference between the insular cortex group and healthy controls (U = 121.5, P < 0.0001) (Fig. 5C). The pair-wise comparison of the vmPFC group against healthy controls did not reach significance (U = 317, P = 0.064), although the average amount bet was significantly correlated with the number of bankruptcies in the vmPFC group (r20 = 0.524, P = 0.018).
Discussion
The present study is the first to characterize distinct effects of damage to the vmPFC and insular cortex on a neuropsychological measure of risky decision-making with known outcome probabilities. The three lesion groups all showed broadly intact processing of the basic trial-by-trial probabilities on the Cambridge Gamble Task, as evidenced by consistent choice of the box colour that was in the majority (Fig. 6), as well as indifferent choice and longer deliberation times in the equal odds (5 red : 5 blue) condition. Probability judgement did not differ significantly between the lesion groups and the healthy comparison group. However, deficits emerged on the measure of betting behaviour, when subjects were asked to wager some of their points on each colour decision. Elevated betting carries the possibility of achieving high gains on the task, but with the concomitant risk of dramatic loss. Patients with vmPFC lesions showed increased betting compared with healthy controls, and this effect was apparent regardless of the chances of winning. In fact, vmPFC patients adjusted their betting in accordance with the odds to the same degree as the healthy comparison group. The lesion control group, with damage predominantly affecting the dlPFC and/or vlPFC, showed comparable betting behaviour to healthy participants. This dissociation between the effects of vmPFC and dorsal PFC damage replicates our earlier observations with the Cambridge Gamble Task (Rahman et al., 1999; Mavaddat et al., 2000; Manes et al., 2002), although in these earlier studies the pathology was less focal. These data demonstrate a degree of neuroanatomical specificity for risk-taking within the PFC. The vmPFC group placed higher wagers across both the Ascend and the Descend task conditions, and as such, these deficits cannot be readily attributed to motor impulsivity or delay aversion (Miller, 1992; Cools et al., 2003). The increase in betting in the vmPFC group appears to represent a criterion shift in risk-taking behaviour across the task.
The increase in betting behaviour was not restricted to the vmPFC group. Patients with damage to the insular cortex also placed higher wagers in comparison with the healthy participants. However, the effects on betting behaviour were qualitatively distinct in the insular cortex and vmPFC lesion groups. Whilst the vmPFC patients adjusted their betting in relation to the probability of winning and losing to the same degree as healthy controls, the insular cortex lesion group were less sensitive to the odds of winning. This difference was revealed in a significant interaction between group and the ratio of boxes, in a model contrasting only the vmPFC and insular groups. The insular cortex group performed similarly to healthy participants when the odds were highly favourable (the 9 : 1 condition), when all subjects typically bet high. As the probability of losing increased, moving from the 9 : 1 ratio to the 6 : 4 ratio, healthy participants and the frontal patients reduced their wager accordingly. In contrast, the insular cortex lesion group maintained a high level of betting as the odds became less favourable, with increasing divergence from healthy participants.
These lesion data indicate a necessary role for the insular cortex in risk adjustment. A neuroanatomical dissociation between the overall amount bet and the degree of risk adjustment extends previous behavioural data using the Cambridge Gamble Task. In a factor analysis of data analysed in relation to ageing effects, the overall amount bet and the degree of risk adjustment loaded on distinct principal components (Deakin et al., 2004). Previous case–control studies in patients with chronic schizophrenia (Hutton et al., 2002) and bipolar disorder (Murphy et al., 2001) have shown attenuated risk adjustment in the context of no overall change in betting behaviour. Conversely, a recent pharmacological study in patients with frontotemporal dementia (where the earliest signs of pathology are in the vmPFC) showed a reduction of betting across all box ratios following treatment with the psychostimulant methylphenidate (Rahman et al., 2006).
Lesion overlap in the insular cortex group was greatest in the anterior portion, extending posteriorly into the secondary somatosensory cortex (SII) (Fig. 2). Functional imaging studies have reported signal change in the anterior insular cortex prior to risk-averse decisions (Kuhnen and Knutson, 2005), and correlating with risk avoidance (Paulus et al., 2003), reward variance (Preuschoff et al., 2006) and monetary uncertainty (Critchley et al., 2001). Further fMRI studies showed insular cortical responses during the anticipation of physical pain (Ploghaus et al., 1999) and unpleasant visual stimuli (Simmons et al., 2004), and in response to punishing feedback that preceded a reversal switch (O’Doherty et al., 2003). These data support a broader role for the insular cortex in signalling aversive consequences (Paulus and Stein, 2006), potentially via the representation of bodily sensations like unease or dread. On the Cambridge Gamble Task, we would expect these aversive anticipatory signals to increase as the odds become less favourable, causing the healthy subject to reduce his/her bet accordingly. Without access to these anticipatory signals of increasing risk, patients with insular damage appear to maintain high levels of wagering regardless of the likelihood of winning.
The detrimental effect of insular cortex damage on emotional decision-making is also predicted by the Somatic Marker hypothesis (Damasio, 1994; Bechara and Damasio, 2005), which posits a crucial role for the insular cortex in holding the representations of bodily states associated with different choice options. The present study did not directly assess the contribution of bodily signals to decision-making performance, but subsequent research may usefully employ psychophysiological recording to further explore the role of somatic feedback in guiding bet selection and risk adjustment on the Cambridge Gamble Task. Notably, two previous studies have included a small number of patients with right insular lesions in a group of ‘target patients’ with damage to brain areas involved in emotional processing. These studies indicated qualitatively similar impairments (on the Iowa Gambling Task and on an investment task) in patients with lesions to the insular cortex and vmPFC (Bar-On et al., 2003; Shiv et al., 2005). Using a more fine-grained behavioural assay, the present study indicates functionally dissociable effects of vmPFC and insular cortex damage on risky decision-making.
The distinction between decision-making under risk and decision-making under ambiguity may influence the neural circuitry recruited during behavioural choice. Two recent fMRI studies have compared brain activations during risky and ambiguous decisions (Hsu et al., 2005; Huettel et al., 2006). Somewhat surprisingly, PFC activation was predominantly associated with decisions made under ambiguity, which may seem incongruous with the current findings. In the study by Huettel et al. (2006), the lateral prefrontal cortex (Brodmann Area 8/9) was identified in the contrast of ambiguous minus risky decisions. Signal change in this region was correlated with ambiguity aversion, as well as with self-report ratings of impulsiveness. No significant voxels were identified in the ventral or medial aspects of the PFC. However, it seems likely that the vmPFC may have been recruited during both types of decisions, and the direct contrast of risk versus ambiguity may overlook such a response. In addition, susceptibility artefacts can limit the ability to detect signal change in the vmPFC using fMRI. Our data demonstrate that damage to the ventromedial region is sufficient to disrupt decision-making under risk, which is consistent with both the clinical phenomenology of vmPFC lesions, as well as earlier imaging studies that had detected vmPFC signal change during risk processing with known outcome probabilities (Rogers et al., 1999a, 2004; Ernst et al., 2004).
The increases in betting behaviour had a detrimental effect on overall task performance. The insular cortex lesion group experienced a greater number of bankruptcies and won fewer points overall, compared with the control group. These effects were also present to a lesser extent in the vmPFC group, where the number of bankruptcies was positively correlated with the average amount bet. A failure to appreciate potential loss is central to psychological definitions of risk taking (Slovic, 1987; Paulus et al., 2003; Lane et al., 2004; Weller et al., 2007). It represents a core clinical feature of the vmPFC lesion syndrome, which is also present in mania, substance abuse and problem gambling. It must be noted, however, that elevated betting on the Cambridge Gamble Task is additionally correlated with the outcome variance: as the wager increases, the difference between the win and loss outcomes increases proportionally. Outcome variance (irrespective of the potential for loss) is highlighted in economic models of risk (Lopes, 1987) and may also be represented in vmPFC and insular cortex circuitry (Sanfey et al., 2003; Preuschoff et al., 2006). For example, Sanfey et al. (2003) adapted the Iowa Gambling Task to compare preference for high variance and low-variance decks. Whilst healthy participants were variance averse, a subgroup of vmPFC lesion cases actually preferred the high-variance decks. In our data, the vmPFC and insular cortex lesion groups did not differ from controls in the SDs of point earnings on the task (Table 2). However, this analysis is limited by the fixed sequence of wins and losses on the task, which ensured that all subjects experienced a number of losses following choices of the more likely outcome. We explored further the effects of increased betting on outcome variance using a computerized simulation of the task that calculated trial outcomes probabilistically and in a fully randomized order (Supplementary Material and Supplementary Table S2). By imputing the mean bet at the four box ratios for each group of subjects, we assessed the mean and SD of total points won on the simulated task. Simulation of the vmPFC and insular cortex groups’ betting behaviour yielded moderately higher average total points, compared with simulated performance of healthy controls. Critically, the SD of the total points was increased dramatically in both the vmPFC and insular cortex simulations, to almost twice the SD for the healthy and lesion control simulations. Behavioural data in healthy participants indicate consistent preference for options that minimize outcome variance (Kahneman and Tversky, 1984; Sanfey et al., 2003). The vmPFC and insular cortex may operate in concert to implement these naturally occurring conservative biases, and lesions to this system appear to disengage these biases, resulting in risk-taking behaviour. The separation of neural substrates for loss aversion and variance aversion remains a target for future research.
Some limitations should be noted. First, the present study was focussed specifically on the evaluation of decision-making following vmPFC and insular cortex lesions, and further research is required to fully characterize the more general neuropsychological profile associated with insular cortex damage. Second, whilst this represents one of the largest studies of vmPFC damage in the literature, we had limited power to detect effects of lesion laterality and gender in order to examine some previous observations (Tranel et al., 2002, 2005) (Supplementary Material). Third, cases with entirely focal lesions to the vmPFC region are very rare, and in individual cases, lesions encroached into adjacent sectors of the PFC. Critically, this pathology in the lateral orbital region and dlPFC was also represented in the lesion control group, who performed at the level of healthy participants on the task. The insular cortex lesions not only extended into the secondary somatosensory cortex, but also, in some cases, into adjacent striatum and temporal cortex. Whilst it is conceivable that striatal pathology may have contributed to decision-making abnormalities, we previously reported no impairment on the Cambridge Gamble Task in unmedicated patients with Parkinson's disease (Cools et al., 2003) or in patients with Huntington's disease (Watkins et al., 2000). Previous findings of Iowa Gambling Task deficits in Parkinson's disease (Pagonabarraga et al., 2007) may be explained by the additional demands for stimulus-reinforcement learning in that task (Knowlton et al., 1996). In the present data set, the striatum was not consistently damaged in the insular cases with the greatest behavioural effects, and we consider it unlikely that striatal damage underlies the lack of risk adjustment in the insular group.
In conclusion, the present data demonstrate distinct impairments in risky decision-making in human cases with lesions to the vmPFC and insular cortex. On a task with minimal demands for learning or working memory, performance was intact in a lesion control group with mainly dlPFC and/or vlPFC damage. These data indicate a selective role for the ventromedial region, at least within the frontal cortex, in the regulation of decision-making with known outcome probabilities. These data also confirm the necessary role of the insular cortex in affective decision-making. The observation that insular cortex lesions increase risk-taking only at the more unfavourable odds is consistent with functional imaging studies indicating insular cortical involvement in the signalling of aversive outcomes. Interventions affecting vmPFC and insular cortex activation may have therapeutic potential in the treatment of neuropsychiatric conditions associated with abnormal decision-making.
Supplementary material
Supplementary material is available at Brain online.
Supplementary Material
Acknowledgements
The authors are grateful to Ms E Recknor for assistance with data collection and Dr R Cardinal for helpful discussion. The Cambridge Gamble Task is licensed to Cambridge Cognition plc. L.C., M.R.F.A., B.J.S. and T.W.R. are consultants for Cambridge Cognition plc. Program Project Grant from the National Institute of Neurological Disorders and Strokes (NINDS) (P01 NS019632, A.B. and H.D.); Economic and Social Research Council and Responsibility in Gambling Trust (RES-164-0010, L.C. and T.W.R.); Wellcome Trust Programme Grant (T.W.R., BJ Everitt, AC Roberts and B.J.S.); James S. McDonnell Foundation Collaborative Award (T.W.R., EA Phelps); Medical Research Council (UK) and Wellcome Trust consortium award to the Behavioural and Clinical Neuroscience Institute. Funding to pay the Open Access publication charges for this article was provided by the Wellcome Trust.
Glossary
Abbreviations:
- CT
computed tomography
- fMRI
functional magnetic resonance imaging
- SII
somatosensory cortex
- vmPFC
ventromedial prefrontal cortex
References
- Augustine JR. Circuitry and functional aspects of the insular lobe in primates including humans. Brain Res Brain Res Rev. 1996;22:229–44. doi: 10.1016/s0165-0173(96)00011-2. [DOI] [PubMed] [Google Scholar]
- Bar-On R, Tranel D, Denburg NL, Bechara A. Exploring the neurological substrate of emotional and social intelligence. Brain. 2003;126:1790–800. doi: 10.1093/brain/awg177. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio A. The somatic marker hypothesis: a neural theory of economic decision. Game Econ Behav. 2005;52:336–72. [Google Scholar]
- Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Tranel D, Anderson SW. Dissociation of working memory from decision making within the human prefrontal cortex. J Neurosci. 1998;18:428–37. doi: 10.1523/JNEUROSCI.18-01-00428.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechara A, Tranel D, Damasio H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000;123:2189–202. doi: 10.1093/brain/123.11.2189. [DOI] [PubMed] [Google Scholar]
- Berlin HA, Rolls ET, Kischka U. Impulsivity, time perception, emotion and reinforcement sensitivity in patients with orbitofrontal cortex lesions. Brain. 2004;127:1108–26. doi: 10.1093/brain/awh135. [DOI] [PubMed] [Google Scholar]
- Camerer C, Weber M. Recent developments in modelling preferences: uncertainty and ambiguity. J Risk Uncertainty. 1992;5:325–70. [Google Scholar]
- Cardinal RN, Aitken MRF. ANOVA for the behavioural sciences researcher. New Jersey, USA: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- Cato MA, Delis DC, Abildskov TJ, Bigler E. Assessing the elusive cognitive deficits associated with ventromedial prefrontal damage: a case of a modern-day Phineas Gage. J Int Neuropsych Soc. 2004;10:453–65. doi: 10.1017/S1355617704103123. [DOI] [PubMed] [Google Scholar]
- Clark L, Manes F. Social and emotional decision-making following frontal lobe injury. Neurocase. 2004;10:398–403. doi: 10.1080/13554790490882799. [DOI] [PubMed] [Google Scholar]
- Clark L, Manes F, Antoun N, Sahakian BJ, Robbins TW. The contributions of lesion laterality and lesion volume to decision-making impairment following frontal lobe damage. Neuropsychologia. 2003;41:1474–83. doi: 10.1016/s0028-3932(03)00081-2. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press; 1988. [Google Scholar]
- Cools R, Barker RA, Sahakian BJ, Robbins TW. L-Dopa medication remediates cognitive inflexibility, but increases impulsivity in patients with Parkinson's disease. Neuropsychologia. 2003;41:1431–41. doi: 10.1016/s0028-3932(03)00117-9. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Mathias CJ, Dolan RJ. Neural activity in the human brain relating to uncertainty and arousal during anticipation. Neuron. 2001;29:537–45. doi: 10.1016/s0896-6273(01)00225-2. [DOI] [PubMed] [Google Scholar]
- Damasio A. Descartes’ error: emotion, reason and the human brain. New York: G.P. Putnam; 1994. [Google Scholar]
- Damasio H. Human brain anatomy in computerized images. New York: Oxford University Press; 1995. [Google Scholar]
- Damasio H, Frank R. Three-dimensional in vivo mapping of brain lesions in humans. Arch Neurol. 1992;49:137–43. doi: 10.1001/archneur.1992.00530260037016. [DOI] [PubMed] [Google Scholar]
- Deakin J, Aitken M, Robbins T, Sahakian BJ. Risk taking during decision-making in normal volunteers changes with age. J Int Neuropsychol Soc. 2004;10:590–8. doi: 10.1017/S1355617704104104. [DOI] [PubMed] [Google Scholar]
- Dimitrov M, Phipps M, Zahn TP, Grafman J. A thoroughly modern Gage. Neurocase. 1999;5:345–54. [Google Scholar]
- Ernst M, Nelson EE, McClure EB, Monk CS, Munson S, Eshel N, et al. Choice selection and reward anticipation: an fMRI study. Neuropsychologia. 2004;42:1585–97. doi: 10.1016/j.neuropsychologia.2004.05.011. [DOI] [PubMed] [Google Scholar]
- Ernst M, Paulus MP. Neurobiology of decision making: a selective review from a neurocognitive and clinical perspective. Biol Psychiatry. 2005;58:597–604. doi: 10.1016/j.biopsych.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Eslinger PJ, Damasio AR. Severe disturbance of higher cognition after bilateral frontal lobe ablation: patient EVR. Neurology. 1985;35:1731–41. doi: 10.1212/wnl.35.12.1731. [DOI] [PubMed] [Google Scholar]
- Fecteau S, Knoch D, Fregni F, Sultani N, Boggio P, Pascual-Leone A. Diminishing risk-taking behavior by modulating activity in the prefrontal cortex: a direct current stimulation study. J Neurosci. 2007;27:12500–5. doi: 10.1523/JNEUROSCI.3283-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellows LK, Farah MJ. Different underlying impairments in decision-making following ventromedial and dorsolateral frontal lobe damage in humans. Cereb Cortex. 2005;15:58–63. doi: 10.1093/cercor/bhh108. [DOI] [PubMed] [Google Scholar]
- Frank RJ, Damasio H, Grabowski TJ. Brainvox: an interactive, multimodal visualization and analysis system for neuroanatomical imaging. Neuroimage. 1997;5:13–30. doi: 10.1006/nimg.1996.0250. [DOI] [PubMed] [Google Scholar]
- Fukui H, Murai T, Fukuyama H, Hayashi T, Hanakawa T. Functional activity related to risk anticipation during performance of the Iowa Gambling Task. Neuroimage. 2005;24:253–9. doi: 10.1016/j.neuroimage.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Hinson JM, Jameson TL, Whitney P. Somatic markers, working memory, and decision making. Cogn Affect Behav Neurosci. 2002;2:341–53. doi: 10.3758/cabn.2.4.341. [DOI] [PubMed] [Google Scholar]
- Hsu M, Bhatt M, Adolphs R, Tranel D, Camerer CF. Neural systems responding to degrees of uncertainty in human decision-making. Science. 2005;310:1680–3. doi: 10.1126/science.1115327. [DOI] [PubMed] [Google Scholar]
- Huettel SA, Stowe CJ, Gordon EM, Warner BT, Platt ML. Neural signatures of economic preferences for risk and ambiguity. Neuron. 2006;49:765–75. doi: 10.1016/j.neuron.2006.01.024. [DOI] [PubMed] [Google Scholar]
- Hutton SB, Murphy FC, Joyce EM, Rogers RD, Cuthbert I, Barnes TR, et al. Decision making deficits in patients with first-episode and chronic schizophrenia. Schizophr Res. 2002;55:249–57. doi: 10.1016/s0920-9964(01)00216-x. [DOI] [PubMed] [Google Scholar]
- Kahneman D, Tversky A. Choices, values and frames. Am Psychol. 1984;39:341–50. [Google Scholar]
- Knoch D, Gianotti LR, Pascual-Leone A, Treyer V, Regard M, Hohmann M, et al. Disruption of right prefrontal cortex by low-frequency repetitive transcranial magnetic stimulation induces risk-taking behavior. J Neurosci. 2006;26:6469–72. doi: 10.1523/JNEUROSCI.0804-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton BJ, Mangels JA, Squire LR. A neostriatal habit learning system in humans. Science. 1996;273:1399–402. doi: 10.1126/science.273.5280.1399. [DOI] [PubMed] [Google Scholar]
- Krain AL, Wilson AM, Arbuckle R, Castellanos FX, Milham MP. Distinct neural mechanisms of risk and ambiguity: a meta-analysis of decision-making. Neuroimage. 2006;32:477–84. doi: 10.1016/j.neuroimage.2006.02.047. [DOI] [PubMed] [Google Scholar]
- Kuhnen CM, Knutson B. The neural basis of financial risk taking. Neuron. 2005;47:763–70. doi: 10.1016/j.neuron.2005.08.008. [DOI] [PubMed] [Google Scholar]
- Lane SD, Cherek DR, Pietras CJ, Tcheremissine OV. Alcohol effects on human risk taking. Psychopharmacology. 2004;172:68–77. doi: 10.1007/s00213-003-1628-2. [DOI] [PubMed] [Google Scholar]
- Lopes LL. Between fear and hope: the psychology of risk. In: Berkowitz L, editor. Advances in experimental social psychology. New York, NY: Academic Press; 1987. pp. 255–95. [Google Scholar]
- Manes F, Sahakian B, Clark L, Rogers R, Antoun N, Aitken M, et al. Decision-making processes following damage to the prefrontal cortex. Brain. 2002;125:624–39. doi: 10.1093/brain/awf049. [DOI] [PubMed] [Google Scholar]
- Mavaddat N, Kirkpatrick PJ, Rogers RD, Sahakian BJ. Deficits in decision-making in patients with aneurysms of the anterior communicating artery. Brain. 2000;123:2109–17. doi: 10.1093/brain/123.10.2109. [DOI] [PubMed] [Google Scholar]
- Miller LA. Impulsivity, risk-taking, and the ability to synthesize fragmented information after frontal lobectomy. Neuropsychologia. 1992;30:69–79. doi: 10.1016/0028-3932(92)90015-e. [DOI] [PubMed] [Google Scholar]
- Murphy FC, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, Paykel ES, et al. Decision-making cognition in mania and depression. Psychol Med. 2001;31:679–93. doi: 10.1017/s0033291701003804. [DOI] [PubMed] [Google Scholar]
- Northoff G, Grimm S, Boeker H, Schmidt C, Bermpohl F, Heinzel A, et al. Affective judgment and beneficial decision making: ventromedial prefrontal activity correlates with performance in the Iowa Gambling Task. Hum Brain Mapp. 2006;27:572–87. doi: 10.1002/hbm.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Doherty J, Critchley H, Deichmann R, Dolan RJ. Dissociating valence of outcome from behavioral control in human orbital and ventral prefrontal cortices. J Neurosci. 2003;23:7931–9. doi: 10.1523/JNEUROSCI.23-21-07931.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ongur D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex. 2000;10:206–19. doi: 10.1093/cercor/10.3.206. [DOI] [PubMed] [Google Scholar]
- Pagonabarraga J, Garcia-Sanchez C, Llebaria G, Pascual-Sedano B, Gironell A, Kulisevsky J. Controlled study of decision-making and cognitive impairment in Parkinson's disease. Mov Disord. 2007;22:1430–5. doi: 10.1002/mds.21457. [DOI] [PubMed] [Google Scholar]
- Paulus MP. Decision-making dysfunctions in psychiatry–altered homeostatic processing? Science. 2007;318:602–6. doi: 10.1126/science.1142997. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Rogalsky C, Simmons A, Feinstein JS, Stein MB. Increased activation in the right insula during risk-taking decision making is related to harm avoidance and neuroticism. Neuroimage. 2003;19:1439–48. doi: 10.1016/s1053-8119(03)00251-9. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Stein MB. An insular view of anxiety. Biol Psychiatry. 2006;60:383–7. doi: 10.1016/j.biopsych.2006.03.042. [DOI] [PubMed] [Google Scholar]
- Ploghaus A, Tracey I, Gati JS, Clare S, Menon RS, Matthews PM, et al. Dissociating pain from its anticipation in the human brain. Science. 1999;284:1979–81. doi: 10.1126/science.284.5422.1979. [DOI] [PubMed] [Google Scholar]
- Preuschoff K, Bossaerts P, Quartz SR. Neural differentiation of expected reward and risk in human subcortical structures. Neuron. 2006;51:381–90. doi: 10.1016/j.neuron.2006.06.024. [DOI] [PubMed] [Google Scholar]
- Rahman S, Robbins TW, Hodges JR, Mehta MA, Nestor PJ, Clark L, et al. Methylphenidate (‘Ritalin’) can ameliorate abnormal risk-taking behavior in the frontal variant of frontotemporal dementia. Neuropsychopharmacology. 2006;31:651–8. doi: 10.1038/sj.npp.1300886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman S, Sahakian BJ, Hodges JR, Rogers RD, Robbins TW. Specific cognitive deficits in mild frontal variant frontotemporal dementia. Brain. 1999;122:1469–93. doi: 10.1093/brain/122.8.1469. [DOI] [PubMed] [Google Scholar]
- Reynolds SM, Zahm DS. Specificity in the projections of prefrontal and insular cortex to ventral striatopallidum and the extended amygdala. J Neurosci. 2005;25:11757–67. doi: 10.1523/JNEUROSCI.3432-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RD, Everitt BJ, Baldacchino A, Blackshaw AJ, Swainson R, Wynne K, et al. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: evidence for monoaminergic mechanisms. Neuropsychopharmacology. 1999a;20:322–39. doi: 10.1016/S0893-133X(98)00091-8. [DOI] [PubMed] [Google Scholar]
- Rogers RD, Owen AM, Middleton HC, Williams EJ, Pickard JD, Sahakian BJ, et al. Choosing between small, likely rewards and large, unlikely rewards activates inferior and orbital prefrontal cortex. J Neurosci. 1999b;19:9029–38. doi: 10.1523/JNEUROSCI.19-20-09029.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RD, Ramnani N, Mackay C, Wilson JL, Jezzard P, Carter CS, et al. Distinct portions of anterior cingulate cortex and medial prefrontal cortex are activated by reward processing in separable phases of decision-making cognition. Biol Psychiatry. 2004;55:594–602. doi: 10.1016/j.biopsych.2003.11.012. [DOI] [PubMed] [Google Scholar]
- Rorden C, Karnath HO. Using human brain lesions to infer function: a relic from a past era in the fMRI age? Nat Rev Neurosci. 2004;5:813–9. doi: 10.1038/nrn1521. [DOI] [PubMed] [Google Scholar]
- Sanfey AG, Hastie R, Colvin MK, Grafman J. Phineas gauged: decision-making and the human prefrontal cortex. Neuropsychologia. 2003;41:1218–29. doi: 10.1016/s0028-3932(03)00039-3. [DOI] [PubMed] [Google Scholar]
- Shiv B, Loewenstein G, Bechara A, Damasio H, Damasio AR. Investment behavior and the negative side of emotion. Psychol Sci. 2005;16:435–9. doi: 10.1111/j.0956-7976.2005.01553.x. [DOI] [PubMed] [Google Scholar]
- Simmons A, Matthews SC, Stein MB, Paulus MP. Anticipation of emotionally aversive visual stimuli activates right insula. Neuroreport. 2004;15:2261–5. doi: 10.1097/00001756-200410050-00024. [DOI] [PubMed] [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236:280–5. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Tranel D, Bechara A, Denburg NL. Asymmetric functional roles of right and left ventromedial prefrontal cortices in social conduct, decision-making, and emotional processing. Cortex. 2002;38:589–612. doi: 10.1016/s0010-9452(08)70024-8. [DOI] [PubMed] [Google Scholar]
- Tranel D, Damasio H, Denburg NL, Bechara A. Does gender play a role in functional asymmetry of ventromedial prefrontal cortex? Brain. 2005;128:2872–81. doi: 10.1093/brain/awh643. [DOI] [PubMed] [Google Scholar]
- Watkins LH, Rogers RD, Lawrence AD, Sahakian BJ, Rosser AE, Robbins TW. Impaired planning but intact decision making in early Huntington's disease: implications for specific fronto-striatal pathology. Neuropsychologia. 2000;38:1112–25. doi: 10.1016/s0028-3932(00)00028-2. [DOI] [PubMed] [Google Scholar]
- Weller JA, Levin IP, Shiv B, Bechara A. Neural correlates of adaptive decision making for risky gains and losses. Psychol Sci. 2007;18:958–64. doi: 10.1111/j.1467-9280.2007.02009.x. [DOI] [PubMed] [Google Scholar]
- Windmann S, Kirsch P, Mier D, Stark R, Walter B, Gunturkun O, et al. On framing effects in decision making: linking lateral versus medial orbitofrontal cortex activation to choice outcome processing. J Cogn Neurosci. 2006;18:1198–211. doi: 10.1162/jocn.2006.18.7.1198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.