Abstract
A challenge for subunit vaccines whose goal is to elicit CD8+ cytotoxic T lymphocytes (CTLs) is to deliver the antigen to the cytosol of the living cell, where it can be processed for presentation by major histocompatibility complex (MHC) class I molecules. Several bacterial toxins have evolved to efficiently deliver catalytic protein moieties to the cytosol of eukaryotic cells. Anthrax lethal toxin consists of two distinct proteins that combine to form the active toxin. Protective antigen (PA) binds to cells and is instrumental in delivering lethal factor (LF) to the cell cytosol. To test whether the lethal factor protein could be exploited for delivery of exogenous proteins to the MHC class I processing pathway, we constructed a genetic fusion between the amino-terminal 254 aa of LF and the gp120 portion of the HIV-1 envelope protein. Cells treated with this fusion protein (LF254-gp120) in the presence of PA effectively processed gp120 and presented an epitope recognized by HIV-1 gp120 V3-specific CTL. In contrast, when cells were treated with the LF254-gp120 fusion protein and a mutant PA protein defective for translocation, the cells were not able to present the epitope and were not lysed by the specific CTL. The entry into the cytosol and dependence on the classical cytosolic MHC class I pathway were confirmed by showing that antigen presentation by PA + LF254-gp120 was blocked by the proteasome inhibitor lactacystin. These data demonstrate the ability of the LF amino-terminal fragment to deliver antigens to the MHC class I pathway and provide the basis for the development of novel T cell vaccines.
Whereas serum Igs are believed to be sufficient for protection conferred by most current vaccines (1), CD8+ cytotoxic T cells (CTLs) are believed to be important in clearing viral infections (1–8). A more vigorous CTL response against a viral infection thus should be beneficial (9–13). Thus, vaccines eliciting specific CTLs should be valuable, especially in the case of viruses that produce chronic infections, such as HIV. Although live viruses elicit CTL immunity, soluble whole proteins, such as subunit vaccines, with or without adjuvants, generally do not (14–17). Because whole exogenous proteins are usually internalized via the endosomal system, they are processed for presentation by class II major histocompatibility complex (MHC) molecules, generally not class I. In contrast, presentation by class I MHC molecules typically occurs only for proteins proteolytically processed in the cytoplasm of the cell. Cytosolic proteins are digested into short peptides by proteasomes, and the resulting peptides are transported by transporters of antigenic peptides into the endoplasmic reticulum, where they bind to nascent class I MHC molecules, which carry them out to the cell surface for display to CD8+ T cells (17). Therefore, CD8+ CTLs, which uniquely recognize peptide epitopes presented by class I MHC molecules, provide surveillance against abnormal proteins synthesized in the cell, such as viral proteins or tumor antigens. The challenge in designing a nonliving vaccine for induction of CD8+ CTLs thus is to introduce the vaccine protein into the cytosol of cells for processing and presentation by their class I molecules.
Several CTL vaccine strategies have been employed with varying effectiveness, including live attenuated bacterial and viral strains, immunostimulatory complexes (ISCOMs) and liposome delivery systems for soluble antigens, and DNA-based vaccines. Unfortunately, each of these systems contains its own unique set of problems and is not always suitable for all individuals (18–21). Particularly, in the case of HIV-1 and its macaque close cousin simian immunodeficiency virus (SIV), live attenuated virus has been shown to protect adult monkeys from a subsequent challenge with virulent virus (22), but the safety of an attenuated strain, especially in newborns, has been questioned (23).
A number of bacterial toxins contain catalytic domains that share the ability to gain access to the host cell cytosol, where they can exert their effects. Although each toxin may differ in the mechanism or route by which it gains entry to the cytosol, the overall effect is that of a “molecular syringe” that is able to inject the toxic protein into the cell. Several bacterial toxins, including diphtheria toxin (DT), Pseudomonas exotoxin A (PE), pertussis toxin, and the pertussis adenylate cyclase, have been used in attempts to deliver peptide epitopes to the cell cytosol as internal or amino-terminal fusions (24–27). These systems are restricted in their use as potential vaccines, because their capacity to deliver larger protein antigens is limited and many individuals have already been immunized against the carrier toxin.
Although peptides are able to stimulate a cellular immune response, whole protein antigens may be better suited for use in an effective vaccine for two reasons. First, the epitope that is essential for protection in one genetic background may prove to be irrelevant in a different genetic background. Therefore, it is beneficial for a broadly applied T cell vaccine to use the full-length protein from which the various relevant epitopes are derived. Second, peptides recognized by CTLs are processed from the whole protein by specialized degradative machinery, including the proteasome complex. In certain instances, the processing of the relevant peptide epitopes is dependent on the flanking amino acid sequences (28). However, flanking residues are not always important for proper processing (29). Because it currently is not possible to accurately predict which epitopes are dependent on their context for proper processing, it is important to deliver the entire antigen to the cell cytosol for optimal processing and presentation.
Bacillus anthracis secretes two toxins into the extracellular medium during growth (30, 31). The two toxins consist of three distinct proteins that combine in a pairwise fashion (32, 33). Protective antigen (PA) combines with lethal factor (LF) or edema factor (EF). PA combined with LF constitutes lethal toxin, whereas PA combined with EF makes edema toxin (34, 35). In a simple model of intoxication, PA (83 kDa) binds to a protein receptor on the surface of cells. PA is then cleaved by a cellular protease (furin) and the amino-terminal 20-kDa fragment is released, leaving a 63-kDa fragment, PA63, bound to the cell (36–38). PA63 is able to bind either LF or EF. The toxin is then endocytosed and transported into the cell. Conversion of PA to PA63 allows formation of an oligomeric form of PA, which, after exposure to low pH in late endosomes, forms channels in cell membranes (39, 40). It is believed that these channels facilitate the delivery of LF or EF from the endosome to the cytosol of the cell (41, 42). We have previously described the internalization of fusion proteins containing anthrax toxin lethal factor and the catalytic domains of other bacterial toxins (43–45). These active fusions were used to define the amino-terminal 254 aa of LF as those necessary for uptake of the fusions (46). In this work, we have taken advantage of the efficient delivery of LF fusion proteins to the cytosol to intracellularly inoculate living cells with whole protein antigens. This system will provide the basis for new potent CTL vaccines.
MATERIALS AND METHODS
Reagents and General Procedures.
Restriction endonucleases and DNA modifying enzymes were purchased from Life Technologies, Boehringer Mannheim, or New England Biolabs. Oligonucleotides were synthesized on a PCR mate (Applied Biosystems) and purified on oligonucleotide purification cartridges (Applied Biosystems). The PCR was performed with a GeneAmp kit according to the manufacturer’s directions (Perkin–Elmer/Cetus). Bacterial media preparation, restriction digests, ligation, and phosphatase treatment of DNA were performed by standard protocols (47). Peptide P18IIIB was made by an automated peptide synthesizer (Applied Biosystems) and purified by HPLC liquid chromatography before use (48). Lactacystin was synthesized in the lab of E. J. Corey (Harvard University, Cambridge, MA) and was a generous gift of Jonathan Yewdell and Jack Bennink (National Institute of Allergy and Infectious Diseases, Bethesda, MD).
Plasmid Construction.
The plasmid used for expressing the LF254-gp120 fusion protein in Escherichia coli was constructed by ligation of the pGEX-KG vector (Pharmacia) with PCR-amplified LF and gp120 gene sequences. The DNA encoding residues 1–254 of LF were amplified from plasmid pLF7 with primers that added unique XbaI and MluI sites on the 5′ and 3′ ends, respectively (49). The primers were 5′-TCT AGA TCT AGA AGC GGG CGG TCA TGG TGA TGT AGG-3′ (primer 1) and 5′-GAT CTT TAA GTT CAC GCG TGG ATA GAT TTA TTT CTT G-3′ (primer 2). The gene for gp120 was amplified from plasmid HXB2-env with primers that added unique restriction sites for MluI on the 5′ end and XhoI on the 3′ end of the amplified gene (43). The sequences were 5′-CCG CGT ACG CGT ATG AGA GTG AAG GAG AAA TAT CAG-3′ (primer 3) and 5′-TTC GAG CTC GAG TTA TCT TTT TTC TCT CTG CAC CAC-3′ (primer 4). Primer 4 introduced a stop sequence (TAA) after the gp120 coding sequence. The amplified DNA products and the pGEX-KG plasmid DNA were digested with the appropriate restriction enzymes. Vector DNA was dephosphorylated with bacterial alkaline phosphatase for 30 min. All three DNA fragments were purified from low-melting-point agarose after electrophoresis by extraction with phenol-chloroform, mixed, and ligated overnight at 16°C with T4 DNA ligase. The ligated DNA was used to transform chemically competent E. coli (DH5α, high efficiency, Life Technologies). Transformed E. coli were selected on ampicillin containing solid media (50 μg/ml) and screened by restriction analysis of extracted plasmid. Clones that had the expected restriction pattern were confirmed by DNA sequencing.
Expression and Purification of the LF254-gp120 Fusion Protein.
The use of plasmid pGEX-KG allowed for the expression of the three-part fusion protein (GST-LF254-gp120) after induction by isopropyl-1-thio-β-d-galactopyranoside (IPTG) and rapid purification by adsorption to glutathione-Sepharose 4B. The expression and purification of GST-LF fusion proteins was described previously (44). E. coli strain SG12036 was transformed with the pGEX-KG-LF254-gp120 fusion vector and grown in rich media (superbroth, 100 μg/ml of ampicillin) with shaking at 225 rpm at 37°C. When the cell density at A600 reached 0.6–0.8, IPTG was added to a final concentration of 1 mM. After further incubation for 2 hr, the bacterial cells were pelleted by centrifugation and then resuspended in 100 mM phosphate buffer (pH 7.4), 150 mM NaCl, 1% Triton X-100, 5 mM EDTA, 5 μg/ml leupeptin, 10 μg/ml aprotinin, and 10 μg/ml 4-(2-aminoethyl)-benzenesulfonylfluoride. The bacterial cells were disrupted by sonication, and the clarified extracts were applied to a glutathione-Sepharose 4B column previously equilibrated with buffer (100 mM phosphate, pH 7.4/150 mM NaCl/1% Triton X-100). The column was washed extensively, and the bound fusion protein was eluted with 10 mM glutathione in 50 mM Tris, pH 8.0/0.5 mM EDTA. The eluted protein was concentrated by ultrafiltration with a Centriprep-30 device (Amicon) and analyzed for purity by electrophoresis on nondenaturing and SDS polyacrylamide gels (Phast gels, Pharmacia). Protein concentrations were determined by the micro BCA method with BSA as a standard (Pierce).
Protective Antigen Proteins.
Protective antigen was expressed in B. anthracis from the expression vector pYS5 and purified by established procedures (50, 51). Mutant PA molecules PA CFD and PA–D were constructed by site-directed mutagenesis and have been previously described (52).
Cell Lines.
P815, a DBA/2-derived (H-2d) mastocytoma (ATCC TIB-64) used as target cells in the CTL assay, was maintained in RPMI 1640 medium supplemented with 10% FCS. The HIV gp120-specific CTL lines 9.23.3 and α15–12, which recognize the V3 epitope RGPGRAFVTI, have been previously described (13, 48, 53). HIV gp120-specific CTL lines were derived from BALB/c spleens taken from mice previously immunized with a recombinant vaccinia virus expressing the gp160 protein and restimulated weekly. 9.23.3 CTLs were stimulated with 10 μM P18IIIB peptide pulsed on 5 × 106 irradiated splenocytes [3,000 rads (1 rad = 0.01 Gy)] with 5 × 105 CTLs per well, in a 24-well plate containing 2 ml of a 1:1 mixture of RPMI 1640 medium and Eagle–Hanks’ amino acid medium (EHAA) supplemented with l-glutamine, sodium pyruvate, nonessential amino acids, penicillin, streptomycin, 5 × 10−5 M 2-mercaptoethanol, 10% fetal calf serum, and 10% T-stim (Collaborative Biomedical Products). Stimulation of the α15–12 CTL line used the same media mixture; however, these CTLs were restimulated with mitomycin C-treated α15–12 cells at 5 × 105 CTLs, 5 × 105 15–12 cells, and 5 × 106 irradiated (3,000 rads) BALB/c splenocytes per well. 15–12 cells were isolated from transfected BALB/c 3T3 cells, which express the gp160 protein from the IIIB strain of HIV-1 (48).
Cytotoxic Lymphocyte Assay.
51Cr release assays were performed as previously described (54). When appropriate, target cells were treated with PA (100 ng/ml) and/or LF254-gp120 fusion protein (1.0 ng/ml when used with α15–12 CTL or 50 ng/ml when used with 9.23.3 CTL) for 12 hr in serum-free media. After treatment, the target cells (5 × 105 cells) were labeled with 200 μCi (1 Ci = 37 GBq) of Na251CrO4 in 100 μl of RPMI 1640 for 2 hr at 37°C. In some cases, target cells were pulsed with peptide (1.0–10.0 μM) during labeling. Following labeling, targets were washed three times and added at 3,000 cells per well along with the appropriate number of effector cells in 96-well round-bottom plates. Supernatants were harvested after 6 hr and counted in an Isomedic gamma counter (ICN). The mean of triplicate samples was calculated and the percent 51Cr release was determined using the following formula. Percent 51Cr release = 100 × [(experimental 51Cr release − control 51Cr release)/(maximum 51Cr release − control 51Cr release)], where experimental 51Cr release represents counts from target cells mixed with effector cells, control 51Cr release represents target cells mixed with medium alone (spontaneous release), and maximum 51Cr release represents counts from target cells exposed to 2.5% Triton X-100.
RESULTS
Plasmid Construction.
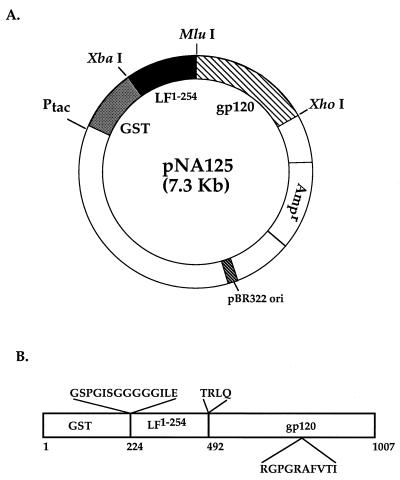
The LF sequences required for binding to PA and translocation to the cell cytosol were genetically fused to the gp120 portion of the envelope gene from HIV-1 strain HXB2. This fusion was constructed in the pGEX-KG vector, resulting in a three-way protein fusion of the 26-kDa glutathione S-transferase domain with LF residues 1–254 and residues 1–511 of the gp160 protein. The inclusion of the Gly5-containing linker from pGEX-KG and the alteration of a base following the XbaI site before the 5′ end of the LF1–254 gene fragment resulted in a modified 14-residue spacer (GSPGISGGGGGILE) between the GST domain and LF1–254 (Fig. 1). The addition of the unique MluI and PstI sites to the 5′ end of the coding sequences for the gp120 portion of the envelope gene added four additional residues, TRLQ, between LF1–254 and gp120 (Fig. 1). The addition of residues at the amino- and carboxyl-terminal ends of LF1–254 do not appear to affect the function of the protein with respect to PA binding and protein translocation (42, 44). The resulting fusion protein has a calculated molecular mass of 114,852 Da and a calculated pI of 7.00.
Figure 1.
Plasmid construct and fusion protein. (A) Plasmid NA125 construct for expression of LF254-gp120 fusion protein in E. coli. GST, 26-kDa glutathione S-transferase domain from the parent vector pGEX-KG; LF1–254, coding sequences for residues 1–254 of mature LF; gp120, coding sequences for residues 1–511 of HXB2-env gene. (B) Expressed GST-LF254-gp120 protein. The carboxyl-terminal residue of the linker from pGEX-KG was changed from D to E, and four residues, TRLQ, were added between the LF254 and gp120 portions of the construct due to DNA manipulations. The V3 epitope, RGPGRAFVTI, recognized by CTL begins at residue 807 of the fusion protein.
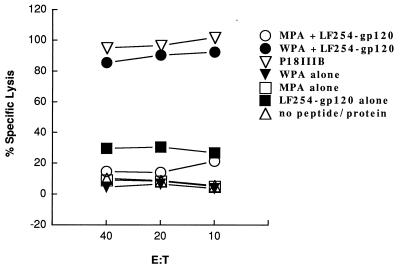
Specific Cytolysis of Target Cells Sensitized with LF254-gp120 Fusion Proteins by HIV gp120-Specific CTL.
The mouse mastocytoma cell line P815 was incubated with PA or PA mutants and/or LF254-gp120 fusion protein for 12 hr in serum-free conditions. The cells were then washed and labeled with 51Cr for use as target cells. The labeled P815 target cells were mixed at different ratios with the effector CTL cell line 9.23.3, which recognizes the peptide epitope, RGPGRAFVTI, from the V3 loop of gp120 (13, 48, 53). Killing of the target cell population was determined by measuring release of 51Cr into the media (Fig. 2). Target cells treated with wild-type PA and LF254-gp120 fusion protein were efficiently recognized and lysed by the 9.23.3 CTL line. To ensure maximal lysis, effector-to-target ratios starting at 40:1 were used. Lysis was still on a plateau at an effector-to-target ratio of 10. The recognition and lysis was dependent on the presence of functional PA, demonstrating that processing of the fusion protein relies on internalization via the PA receptor. Treatment with a translocation-defective mutant PA protein (52) or without the addition of PA resulted in minimal lysis of the target cells, placing a limit on the amount of LF254-gp120 that is proteolytically degraded extracellularly and thus able to sensitize target cells without active transport into the cytosol. This implies that the LF254-gp120 fusion protein needs to gain access to the cell cytosol for processing and presentation. Treatment with PA alone, mutant PA alone, or the LF254-gp120 fusion alone did not sensitize the target cells for lysis. Target cells pulsed with P18IIIB peptide served as a positive control and resulted in cell lysis when effector cells were added. To compare the relative potency of the LF254-gp120 with that of the optimal decapeptide P18-I10 for sensitizing target cells for recognition by these CTL (53, 55, 56), titration experiments were performed. The P18-I10 decapeptide sensitized targets for lysis in the range of 10−10 to 10−11 M, based on specific lysis >10% as a threshold for positivity, whereas the LF254-gp120 sensitized targets with as little as 4 × 10−14 M protein (data not shown). Therefore, the fusion construct was at least 2.5 logs more potent on a molar basis than the optimal binding peptide.
Figure 2.
Recognition of cells treated with gp120 anthrax toxin fusions by gp120-specific cytotoxic lymphocytes. The mouse mastocytoma cell line P815 was incubated with wild-type protective antigen (WPA) or mutant PACFD (MPA) and/or LF254-gp120 fusion proteins (50 ng/ml). P815 cells pulsed with 1.0 μM P18IIIB peptide served as a control. After 12 hr, the cells were washed and the treated P815 cells were labeled with 51Cr. Labeled P815 cells were then mixed at different ratios with the CTL cell line 9.23.3, which recognizes the peptide sequence RGPGRAFVTI from gp120. Killing of the target cell population was determined by measuring release of 51Cr into the medium (% lysis). Background lysis was determined with untreated, 51Cr labeled, P815 cells. These data are the replicate of three experiments.
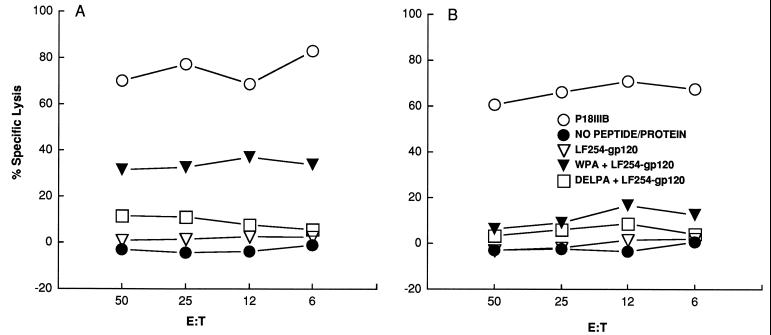
Lactacystin Prevents Lysis of PA/LF254-gp120-Treated Target Cells.
To demonstrate the requirement for LF254-gp120 processing by the classical MHC class I pathway, we examined the ability of the specific proteasome inhibitor, lactacystin, to inhibit presentation of the V3 epitope on the cell surface. Incubation of P815 cells with 10 μM lactacystin for 45 min prior to the addition of PA and LF254-gp120 significantly decreased lysis of the target cells by the α15–12 CTL line (Fig. 3). Lactacystin inhibition of peptide presentation shows that the processing of the peptide epitope from the fusion protein depends on the function of the proteasome complex. This indicates that the protein fusion was delivered to the cytosol of the cell, where it interacts with the proteasome complex and precludes the role of any alternate processing pathways for presentation by the anthrax toxin LF254-gp120 fusion protein.
Figure 3.
Inhibition of fusion protein processing by lactacystin. P815 cells were treated with 1 ng/ml of the GST-LF254-gp120 fusion protein alone and with PA (WPA) or mutant PA–D (DELPA) in the presence (B) or absence (A) of 10 μM lactacystin. 51Cr-labeled target cells were mixed with α15–12 CTLs, and specific lysis was measured. Target cells were treated with the P18IIIB peptide as a positive control for cell lysis. These data are the representative of three experiments.
DISCUSSION
The primary goal of this study was to determine the ability of an anthrax lethal factor fusion to deliver antigenic proteins to the cell cytosol for processing and presentation with class I molecules on the cell surface. We demonstrated the ability of the LF254-gp120 fusion, in conjunction with PA, to sensitize target cells (Fig. 2). The requirement for functional PA shows that the LF254-gp120 fusion needs to gain access to the intracellular environment to be processed. Other toxins that have been used as fusions with peptide epitopes have also resulted in presentation of the epitope on the surface of antigen presenting cells in the proper context. Examples include DT, PE, pertussis toxin, and the Bordetella pertussis adenylate cyclase (24–27, 57). However, the processing and presentation of peptide epitopes from each of these fusion proteins do not appear to occur through the classical MHC class I processing pathway but instead via various alternate pathways.
DT was used as a delivery system with peptide epitopes from influenza virus fused to the amino-terminal end of the toxin (24). Although it was demonstrated that the peptide-toxin fusion gained access to the inside of the cell, processing and presentation of the antigens was not demonstrated. Subsequently, it was reported that DT was able to translocate additional protein domains into the cell cytosol (57, 58). Genetic fusions of an inactive DT protein with an active DT catalytic domain were translocated into the cytosol, where they were toxic. However, fusions with other protein domains had reduced abilities to deliver proteins or were unable to bind to the DT receptor and were not translocated. The entire genetic fusion appeared to be very stable in the cytosol, with no indication of any processing 6 hr after translocation, which may imply that the translocated DT or DT fusions are not accessible to the degradative machinery in the cell.
A truncated PE has also been genetically fused to influenza A peptide epitopes (25). The ability of PE-peptide antigen fusions to deliver the antigenic peptide to the MHC class I molecules on the surface of target cells was examined. Specific lysis by CTLs recognizing the influenza A epitopes within the fusion protein was detected. However, it was determined that the PE fusions trafficked through the cell differently from native PE. In fact, blocking translocation after adding the PE fusions to cells had no effect on processing and presentation of the antigenic peptide (59). The authors proposed that a certain amount of proteolysis occurs in the endosome and that there exist, in the endosome, MHC class I molecules able to bind the processed peptide; thus, recycling of these complexes to the cell surface can mark the cell for recognition and lysis by CTLs. These PE fusions may enter a noncytosolic pathway for presenting exogenous antigens to the MHC class I molecules (60, 61).
Peptides from the lymphocytic choriomeningitis virus nucleoprotein were inserted into the S1 subunit of pertussis toxin and the pertussis adenylate cyclase (26, 27, 57, 62). These fusions specifically sensitized target cells to the appropriate CTLs. However, the dependence on the classical pathway for processing and presentation of the antigen to the MHC class I pathway was not established. The adenylate cyclase fusions were tested for their effectiveness in vivo and were able to generate CTLs. Production of CTLs was dependent on coinjection of the fusion protein with alum, which implies that the fusions are processed by an alternate exogenous pathway for MHC class I antigen.
In the case of LF254-gp120, we have demonstrated that delivery to the cytosol requires active PA and that presentation requires a functional proteasome complex. Use of lactacystin, a specific inhibitor for proteasomes, provides an unequivocal demonstration that these constructs enter the cytosolic degradative pathway involved in classical processing for class I MHC presentation (Fig. 3) (63). Thus, in this case a bacterial toxin fusion protein has been diefinitively shown to deliver a whole protein antigen to the classical cytosolic MHC class I pathway.
The anthrax lethal toxin system has several additional advantages over the other bacterial toxins for vaccine use. First, LF fusion proteins are nontoxic, because the entire catalytic domain has been deleted. Even the “detoxified” DT still retains 1/800 of the wild-type activity, which is enough to preclude its use in vitro or in vivo (24, 64). In contrast, the entire catalytic domain of LF, residues 255–776, has been deleted in LF254-gp120. Our prior studies have shown that only LF residues 1–254 are needed for efficient delivery of fused polypeptides (46). Second, LF fusions can be produced as soluble proteins in standard GST expression vectors. The binary nature of the toxin allows production of LF fusions without manipulation or alteration of the cell-binding properties of PA. LF residues 1–254 appear indifferent to addition of peptides or larger proteins at either the amino or carboxyl termini and still retain their ability to bind PA (44). These additions to LF do not appear to seriously affect the ability of PA to translocate protein into the cell cytosol. In contrast, expression and purification of the other toxin fusions require either use of special hosts capable of secretion of the modified holotoxins or refolding after purification from inclusion bodies. Third, LF fusions appear to be proficient at delivering proteins to the cell cytosol. LF-Pseudomonas exotoxin A fusions are 100 times more potent than wild-type PE, demonstrating that the delivery of the active domain is more efficient (43). The ability of our system to efficiently deliver antigen to the cytosol is reflected in the comparatively small amount of protein needed to achieve recognition by CTL. Both the pertussis cyclase delivery system and the pertussis toxin delivery system require 50 times more antigen on a molar basis to achieve similar recognition of target cells by CTL (26, 27). Finally, LF254 appears capable of delivering protein antigens that are large enough that hosts from varied genetic backgrounds can be expected to process the appropriate epitope from the antigen and properly present it.
Preliminary in vivo experiments show that a single subcutaneous injection of the LF254-gp120 fusion along with PA is able to elicit a vigorous CTL response in the spleens of vaccinated animals (data not shown). We are currently refining the immunization procedure and testing the PA dependence of the in vivo response to confirm a cytosolic processing mechanism, as well as investigating the ability of other LF254-antigen fusions, including LF254-gp41, LF254-reverse transcriptase, and LF254-NEF, to generate an immune response.
A recent study by Ballard et al. (65), performed concurrently with the present study, addresses the effectiveness of in vivo immunization with anthrax toxin fusion constructs, using a fusion of LF with a nine-residue peptide from the listeriolysin protein of Listeria monocyotogenes, and shows protective efficacy against infection. However, because this study used only a nonpeptide minimal fragment from the protein, which can bind directly to class I MHC molecules and does not require processing through the class I pathway, it did not address the question of whether the toxin fusion construct could introduce a whole foreign vaccine protein into the cytosolic class I MHC processing pathway and elicit appropriate degradation and presentation with a class I MHC molecule. Our present study demonstrates this critical mechanistic point and shows that whole protein antigens may be introduced in this fashion for potential use as vaccines. Whole protein antigens have the advantage that they are not limited to single epitopes that are presented by only one or a few MHC molecules and are also more susceptible to escape mutations. However, they have the disadvantage that they are usually harder to introduce into the class I MHC processing pathway without a live viral vector (17). Thus, the major advantage of anthrax toxin fusion proteins is the ability to introduce whole complex foreign proteins to this processing pathway. Thus, the Ballard et al. study (65) and ours complement each other in demonstrating the utility of the anthrax lethal toxin fusion system for the stimulation of a cellular immune response.
In conclusion, we have taken advantage of several unique properties of anthrax toxin to construct fusion proteins that transport large proteins into the cytosol of living cells, where they are processed through the classical pathway for loading onto MHC class I molecules and presentation to CD8 CTL. Anthrax toxin appears particularly well suited, of all the bacterial toxins, to development of safe and potent vaccines for induction of CTL immunity.
Acknowledgments
We thank Dr. E. J. Corey for synthesizing and Drs. Jonathan Yewdell and Jack Bennink for the generous gift of lactacystin.
ABBREVIATIONS
- LF
lethal factor
- PA
protective antigen
- CTL
cytotoxic T lymphocyte
- MHC
major histocompatibility complex
- PE
Pseudomonas exotoxin A
- GST
glutathione S-transferase
References
- 1.Robbins J B, Schneerson R, Szu S C. J Infect Dis. 1995;171:1387–1398. doi: 10.1093/infdis/171.6.1387. [DOI] [PubMed] [Google Scholar]
- 2.Taylor P M, Askonas B A. Immunology. 1986;58:417–420. [PMC free article] [PubMed] [Google Scholar]
- 3.Lin Y L, Askonas B A. J Exp Med. 1981;154:225–234. doi: 10.1084/jem.154.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lukacher A E, Braciale V L, Braciale T J. J Exp Med. 1984;160:814–826. doi: 10.1084/jem.160.3.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMichael A J, Gotch F M, Noble G R, Beare P A S. N Engl J Med. 1983;309:13–17. doi: 10.1056/NEJM198307073090103. [DOI] [PubMed] [Google Scholar]
- 6.Byrne J A, Oldstone M B. J Virol. 1984;51:682–686. doi: 10.1128/jvi.51.3.682-686.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klavinskis L S, Tishon A, Oldstone M B A. J Immunol. 1989;143:2013–2016. [PubMed] [Google Scholar]
- 8.Klavinskis L S, Whitton J L, Joly E, Oldstone M B A. Virology. 1990;178:393–400. doi: 10.1016/0042-6822(90)90336-p. [DOI] [PubMed] [Google Scholar]
- 9.Klavinskis L S, Tishon A, Oldstone M B. J Immunol. 1989;143:2013–2016. [PubMed] [Google Scholar]
- 10.Taylor P M, Askonas B A. Immunology. 1986;58:417–420. [PMC free article] [PubMed] [Google Scholar]
- 11.Sarin P S, Mora C A, Naylor P H, Markham R, Schwartz D, Kahn J, Heseltine P, Gazzard B, Youle M, Rios A, Goldstein A L. Cell Mol Biol. 1995;41:401–407. [PubMed] [Google Scholar]
- 12.van Kuyk R, Torbett B E, Gulizia R J, Leath S, Mosier D E, Koenig S. J Immunol. 1994;153:4826–4833. [PubMed] [Google Scholar]
- 13.Alexander-Miller M A, Leggatt G R, Berzofsky J A. Proc Natl Acad Sci USA. 1996;93:4102–4107. doi: 10.1073/pnas.93.9.4102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harding C V. In: Cellular Proteolytic Systems. Ciechanover A J, Schwartz A L, editors. New York: Wiley; 1994. pp. 163–180. [Google Scholar]
- 15.Carbone F R, Bevan M J. In: Fundamental Immunology. Paul W E, editor. New York: Raven; 1989. pp. 541–567. [Google Scholar]
- 16.Townsend A, Bodmer H. Annu Rev Immunol. 1989;7:601–624. doi: 10.1146/annurev.iy.07.040189.003125. [DOI] [PubMed] [Google Scholar]
- 17.Germain R N, Margulies D H. Annu Rev Immunol. 1993;11:403–450. doi: 10.1146/annurev.iy.11.040193.002155. [DOI] [PubMed] [Google Scholar]
- 18.Cease K B, Berzofsky J A. Annu Rev Immunol. 1994;12:923–989. doi: 10.1146/annurev.iy.12.040194.004423. [DOI] [PubMed] [Google Scholar]
- 19.Takahashi H, Takeshita T, Morein B, Putney S D, Germain R N, Berzofsky J A. Nature (London) 1990;344:873–875. doi: 10.1038/344873a0. [DOI] [PubMed] [Google Scholar]
- 20.Ulmer J B, Donnelly J J, Parker S E, Rhodes G H, Felgner P L, Dwarki V J, Gromkowski S H, Deck R R, DeWitt C M, Friedman A, Hawe L A, Leander K R, Martinez D, Perry H C, Shiver J W, Montgomery D L, Liu M A. Science. 1993;259:1745–1749. doi: 10.1126/science.8456302. [DOI] [PubMed] [Google Scholar]
- 21.White W I, Cassatt D R, Madsen J, Burke S J, Woods R M, Wassef N M, Alving C R, Koenig S. Vaccine. 1995;13:1111–1122. doi: 10.1016/0264-410x(94)00058-u. [DOI] [PubMed] [Google Scholar]
- 22.Daniel M D, Kirchhoff F, Czajak S C, Sehgal P K, Desrosiers R C. Science. 1992;258:1938–1941. doi: 10.1126/science.1470917. [DOI] [PubMed] [Google Scholar]
- 23.Baba T W, Trichel A M, An L, Liska V, Martin L N, Murphey-Corb M, Ruprecht R M. Science. 1996;272:1486–1489. doi: 10.1126/science.272.5267.1486. [DOI] [PubMed] [Google Scholar]
- 24.Stenmark H, Moskaug J O, Madshus I H, Sandvig K, Olsnes S. J Cell Biol. 1991;113:1025–1032. doi: 10.1083/jcb.113.5.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donnelly J J, Ulmer J B, Hawe L A, Friedman A, Shi X P, Leander K R, Shiver J W, Oliff A I, Martinez D, Montgomery D. Proc Natl Acad Sci USA. 1993;90:3530–3534. doi: 10.1073/pnas.90.8.3530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carbonetti N, Tishon A, Oldstone M, Rappuoli R. Abstr Annu Meet Am Soc Microbiol. 1995;95:295. [Google Scholar]
- 27.Sebo P, Fayolle C, d’Andria O, Ladant D, Leclerc C, Ullmann A. Infect Immunol. 1995;63:3851–3857. doi: 10.1128/iai.63.10.3851-3857.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Del Val M, Schlicht H-J, Ruppert T, Reddehase M J, Koszinowski U H. Cell. 1991;66:1145–1153. doi: 10.1016/0092-8674(91)90037-y. [DOI] [PubMed] [Google Scholar]
- 29.Hahn Y S, Braciale V, Braciale T J. J Exp Med. 1991;174:733–736. doi: 10.1084/jem.174.3.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith H, Keppie J. Nature (London) 1954;173:869–870. doi: 10.1038/173869a0. [DOI] [PubMed] [Google Scholar]
- 31.Smith H, Stanley J L. J Gen Microbiol. 1962;29:517–521. doi: 10.1099/00221287-29-3-517. [DOI] [PubMed] [Google Scholar]
- 32.Smith H, Stoner H B. Fed Proc. 1967;26:1554–1557. [PubMed] [Google Scholar]
- 33.Leppla S. In: Bacterial Toxins and Virulence Factors in Disease: Handbook of Natural Toxins, Vol 8. Moss J, Iglewski B, Vaughan M, Tu A, editors. New York: Dekker; 1995. pp. 543–572. [Google Scholar]
- 34.Friedlander A M. J Biol Chem. 1986;261:7123–7126. [PubMed] [Google Scholar]
- 35.Leppla S H. Proc Natl Acad Sci USA. 1982;79:3162–3166. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leppla S H, Klimpel K R, Arora N. In: Molecular Mechanisms of Bacterial Virulence. Kado C I, Crosa J H, editors. Dordrecht, The Netherlands: Kluwer; 1994. pp. 127–139. [Google Scholar]
- 37.Klimpel K R, Molloy S S, Thomas G, Leppla S H. Proc Natl Acad Sci USA. 1992;89:10277–10281. doi: 10.1073/pnas.89.21.10277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Novak J M, Stein M P, Little S F, Leppla S H, Friedlander A M. J Biol Chem. 1992;267:17186–17193. [PubMed] [Google Scholar]
- 39.Blaustein R O, Koehler T M, Collier R J, Finkelstein A. Proc Natl Acad Sci USA. 1989;86:2209–2213. doi: 10.1073/pnas.86.7.2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Milne J C, Collier R J. Mol Microbiol. 1993;10:647–653. doi: 10.1111/j.1365-2958.1993.tb00936.x. [DOI] [PubMed] [Google Scholar]
- 41.Milne J C, Furlong D, Hanna P C, Wall J S, Collier R J. J Biol Chem. 1994;269:20607–20612. [PubMed] [Google Scholar]
- 42.Milne J C, Blanke S R, Hanna P C, Collier R J. Mol Microbiol. 1995;15:661–666. doi: 10.1111/j.1365-2958.1995.tb02375.x. [DOI] [PubMed] [Google Scholar]
- 43.Arora N, Klimpel K R, Singh Y, Leppla S H. J Biol Chem. 1992;267:15542–15548. [PubMed] [Google Scholar]
- 44.Arora N, Leppla S H. Infect Immunol. 1994;62:4955–4961. doi: 10.1128/iai.62.11.4955-4961.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arora N, Williamson L C, Leppla S H, Halpern J L. J Biol Chem. 1994;269:26165–26171. [PubMed] [Google Scholar]
- 46.Arora N, Leppla S H. J Biol Chem. 1993;268:3334–3341. [PubMed] [Google Scholar]
- 47.Sambrook J, Fritsch E F, Maniatis T. Molecular Cloning: A Laboratory Manual. Cold Spring Harbor, NY: Cold Spring Harbor Lab. Press; 1989. [Google Scholar]
- 48.Takahashi H, Cohen J, Hosmalin A, Cease K B, Houghten R, Cornette J, DeLisi C, Moss B, Germain R N, Berzofsky J A. Proc Natl Acad Sci USA. 1988;85:3105–3109. doi: 10.1073/pnas.85.9.3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robertson D L, Leppla S H. Gene. 1986;44:71–78. doi: 10.1016/0378-1119(86)90044-2. [DOI] [PubMed] [Google Scholar]
- 50.Singh Y, Chaudhary V K, Leppla S H. J Biol Chem. 1989;264:19103–19107. [PubMed] [Google Scholar]
- 51.Leppla S H. In: Methods in Enzymology, Vol. 165. Harshman S, editor. Orlando, FL: Academic; 1988. pp. 103–116. [DOI] [PubMed] [Google Scholar]
- 52.Singh Y, Klimpel K R, Arora N, Sharma M, Leppla S H. J Biol Chem. 1994;269:29039–29046. [PubMed] [Google Scholar]
- 53.Shirai M, Pendleton C D, Berzofsky J A. J Immunol. 1992;148:1657–1667. [PubMed] [Google Scholar]
- 54.Alexander M A, Damico C A, Wieties K M, Hansen T H, Connolly J M. J Exp Med. 1991;173:849–858. doi: 10.1084/jem.173.4.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kozlowski S, Corr M, Takeshita T, Boyd L F, Pendleton C D, Germain R N, Berzofsky J A, Margulies D H. J Exp Med. 1992;175:1417–1422. doi: 10.1084/jem.175.6.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Takeshita T, Takahashi H, Kozlowski S, Ahlers J D, Pendleton C D, Moore R L, Nakagawa Y, Yokomuro K, Fox B S, Margulies D H, Berzofsky J A. J Immunol. 1995;154:1973–1986. [PubMed] [Google Scholar]
- 57.Madshus I H, Olsnes S, Stenmark H. Infect Immunol. 1992;60:3296–3302. doi: 10.1128/iai.60.8.3296-3302.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Madshus I H, Stenmark H, Sandvig K, Olsnes S. J Biol Chem. 1991;266:17446–17453. [PubMed] [Google Scholar]
- 59.Ulmer J B, Donnelly J J, Liu M A. Eur J Immunol. 1994;24:1590–1596. doi: 10.1002/eji.1830240721. [DOI] [PubMed] [Google Scholar]
- 60.Kovacsovics-Bankowski M, Rock K L. Science. 1995;267:243–246. doi: 10.1126/science.7809629. [DOI] [PubMed] [Google Scholar]
- 61.Rock K L. Immunol Today. 1996;17:131–137. doi: 10.1016/0167-5699(96)80605-0. [DOI] [PubMed] [Google Scholar]
- 62.Fayolle C, Sebo P, Ladant D, Ullmann A, Leclerc C. J Immunol. 1996;156:4697–4706. [PubMed] [Google Scholar]
- 63.Fenteany G, Standaert R F, Lane W S, Choi S, Corey E J, Schreiber S L. Science. 1995;268:726–731. doi: 10.1126/science.7732382. [DOI] [PubMed] [Google Scholar]
- 64.Barbieri J T, Collier R J. Infect Immunol. 1987;55:1647–1651. doi: 10.1128/iai.55.7.1647-1651.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ballard J D, Collier R J, Starnbach M N. Proc Natl Acad Sci USA. 1996;93:12531–12534. doi: 10.1073/pnas.93.22.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]