Abstract
Background
We studied the relationship between longer delays from symptom onset to hospital presentation and the use of any reperfusion therapy, door-to-balloon time, and door-to-drug time.
Methods
Cohort study of patients with ST-elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from January 1, 1995 to December 31, 2004. Delay in hospital presentation was categorized into 1 hour intervals as ≤1 hour, >1 to 2 hours, >2 to 3 hours, etc., and >11 to 12 hours. The study analyzed 3 groups: 440,398 patients for the association between delay and use of any reperfusion therapy; 67,207 patients for the association between delay and door-to-balloon time; 183,441 patients for the association between delay and door-to-drug time.
Results
In adjusted analyses, patients with longer delays between symptom onset and hospital presentation were less likely to receive any reperfusion therapy, had longer door-to-balloon times, and had longer door-to-needle times (all p<0.0001 for linear trend). For patients presenting ≤1 hour, >1 to 2 hours, and >2 to 3 hours, >9 to 10 hours, >10 to 11 hours, and >11 to 12 hours after symptom onset, the use of any reperfusion therapy were 77%, 77%, 73%, 53%, 50%, and 46% respectively; door-to-balloon times were 99, 101, 106, 123, 125, and 123 minutes respectively; door-to-drug times were 33, 34, 36, 46, 44, and 47 minutes respectively.
Conclusions
Longer delays from symptom onset to hospital presentation were associated with reduced likelihood of receiving primary reperfusion therapy, and even among those treated, late presenters had significantly longer door-to-balloon and door-to-drug times.
Keywords: myocardial infarction, reperfusion, angioplasty, fibrinolysis, quality
Introduction
Timely reperfusion therapy with fibrinolytic therapy or primary percutaneous coronary intervention reduces infarct size and adverse clinical consequences, including mortality, for patient with ST-elevation myocardial infarction.1–11 The guidelines state that patients with ST-elevation myocardial infarction who present within 12 hours from onset of symptoms should be treated with reperfusion therapy and target a door-to-balloon time <90 minutes and door-to-drug time <30 minutes.12 Recently, quality improvement initiatives have focused attention on where hospital delays occur and strategies to reduce door-to-balloon time.13–14
Rapid and appropriate treatment with reperfusion therapy, in accordance with the guidelines, requires a consistent approach to all eligible patients. In particular, patients who are eligible for reperfusion therapy but who present later after the onset of symptoms may not elicit the same response from the health care system. According to the guidelines, recommendations for reperfusion therapy are not different for patients with ST-elevation myocardial infarction presenting earlier versus later within the 12 hours interval after the onset of symptoms.12 However, whether patients presenting later in the interval are less likely to be treated with reperfusion therapy is not known. Moreover, among those who are treated, whether there is less urgency associated with their care, resulting in longer door-to-balloon and door-to-drug times has not been documented. If present, these gaps may contribute to worse outcomes in late presenting patients. Knowledge of these patterns would emphasize the importance of earlier presentation and focus attention on logistical and system issues that contribute to lower use of any reperfusion therapy and longer delays in treatment for patients presenting later after the onset of symptoms.
To address these issues, we undertook a study to evaluate the relationship between longer delays from symptom onset to hospital presentation and the use of any reperfusion therapy, door-to-balloon time, and door-to-drug time among patients with ST-elevation myocardial infarction between 1995 to 2004 from National Registry of Myocardial Infarction. This database is ideally positioned to address this question because it is comprised of contemporary, diverse, and national data.
Methods
Study Design and Sample
The study sample included patients enrolled in National Registry of Myocardial Infarction, a voluntary, prospective registry of patients with acute myocardial infarction, from January 1, 1995 to December 31, 2004. Participating hospitals, data collection methods, verification methods, and reliability have been previously described.15–16 Criteria for diagnosis of acute myocardial infarction used the International Classification of Diseases, 9th Revision, Clinical Modifications discharge diagnosis code of 410.X1 and was confirmed with one of the following criteria: (1) two-fold or greater elevation of cardiac biomarkers; (2) electrocardiogram evidence; and (3) echocardiographic, scintigraphic, or autopsy evidence. Participating hospitals, if required, obtained Institutional Review Board approval for data abstraction.
During our study period from 1995 to 2004, there were 1,926,108 admissions for acute myocardial infarction. The following patients were excluded sequentially: patients who did not have new or presumed new ST-segment elevation in 2 or more leads or left bundle branch block on the first electrocardiogram (n=1,161,187); patients who developed symptoms for acute myocardial infarction after hospital admission date and time (n=14,433); patients who had an unknown time of symptom onset (n=173,051); patients who had a first electrocardiogram time that was not the diagnostic electrocardiogram time for ST-elevation myocardial infarction (n=71,842); patients who had an unknown time of first electrocardiogram (n=23,268); and patients who had a delay from symptom onset to hospital arrival >12 hours (n=41,929). The remaining group of 440,398 patients with ST-elevation myocardial infarction who presented to the hospital within ≤12 hours from symptom onset comprised our study population for the analysis of the association between delay and use of any reperfusion therapy.
To analyze the relationship between delay in hospital presentation and timeliness of reperfusion therapy, the following patients were additionally excluded from the previous study population: patients who were transferred-in from another hospital (n=98,064) and patients who received reperfusion therapy >12 hours after hospital arrival (n=2,491). Then, patients who did not receive primary percutaneous coronary intervention (n=272,636) were excluded to create a study group of 67,207 patients to analyze the association between delay and door-to-balloon time. Similarly, patients who did not receive fibrinolytic therapy (n=156,402) were excluded to create a study group of 183,441 patients to analyze the association between delay and door-to-drug time.
Data Collection and Measures
Delay in hospital presentation was calculated from the documented date and time of symptom onset to the documented date and time of hospital arrival. Use of any reperfusion was defined as receiving either fibrinolytic therapy or primary percutaneous coronary intervention as a primary reperfusion strategy within ≤12 hours of hospital arrival. Door-to-balloon time was defined as time from hospital arrival to first balloon inflation and door-to-drug time was defined as time from hospital arrival to administration of fibrinolytic therapy. For the outcomes of door-to-balloon time and door-to-drug time, we log transformed the outcome measures and performed parametric analysis because their distributions were skewed. To improve the clinical interpretability of the results, we converted the logged values from the models back to their original units, i.e., minutes, using geometric means17–18 and simulation with 10,000 reiterations.19 The geometric mean gives less weight to outlying values and thus better reflects the median as compared with the arithmetic mean.
To evaluate the independent effect of delay in hospital presentation on use of any reperfusion, door-to-balloon time, door-to-drug time, and in-hospital mortality, we adjusted for the following patient and hospital variables. Patient variables included: sociodemographic (age; gender; race/ethnicity classified as white, Black, Hispanic, Asian, and other; and payer type categorized as commercial insurance, Medicare only, Medicare and any other insurance, Medicaid or self pay, and other); medical history (current smoker, diabetes, hypertension, hypercholesterolemia, family history of coronary artery disease, prior myocardial infarction, prior congestive heart failure, prior percutaneous coronary intervention, prior coronary artery bypass surgery, prior stroke, prior angina, absence of chest pain at presentation, congestive heart failure at time of presentation, cardiogenic shock at presentation, systolic blood pressure <90 mmHg at presentation, heart rate >100 beats per minute at presentation); time of day and day of week at presentation (weekdays were defined as Monday to Friday and included daytime from >8am– 4pm, evening from >4pm–12midnight, and night from >12 midnight-8am; weekends were defined as Saturday and Sunday and included daytime from >8am-4pm, evening from >4pm–12midnight, and night from >12 midnight–8am). Hospital variables included: U.S. census region (West, South, Midwest, Northeast), teaching hospitals defined as participation in an accredited residency or fellowship training program, and type of cardiac facilities (interventional, interventional without surgery on site, invasive but not interventional, and non-invasive). All these variables were selected based on their clinical and statistical significance from previous studies.11,20–21
Statistical Analyses
For the outcomes of door-to-balloon time and door-to-drug time as a function of delay in hospital presentation, multivariable generalized linear models were constructed for each outcome to estimate the associations between delay in hospital presentation adjusted for all patient and hospital characteristics. The time from symptom onset to hospital presentation was categorized into 1 hour intervals as ≤1 hour, >1 to 2 hours, >2 to 3 hours, etc., and >11 to 12 hours. By introducing 11 dummy variables representing these categories into the generalized linear models (with the first category as reference group), we estimated the unadjusted outcomes and adjusted outcomes in these categories. We constructed the test of overall differences and also linear trend in outcomes among these categories in the models.
For the outcome of use of any reperfusion, multivariable logistic regression models were constructed to estimate the associations between delay in hospital presentation adjusted for all patient and hospital characteristics. The multivariate models were repeated after excluding patients who were transferred in from another hospital and after excluding patients who had documented contraindications to fibrinolytic therapy or who were treated with emergent coronary artery bypass surgery. These results were not reported separately because the direction and magnitude of the effects were similar to the prior analyses and did not change the conclusions.
For the outcome of in-hospital mortality, multivariable logistic regression models were constructed in the group of patients who were treated with primary percutaneous coronary intervention and in the group who were treated fibrinolytic therapy as the primary reperfusion strategy, and the associations between delay in hospital presentation and in-hospital mortality were estimated and adjusted for all patient and hospital characteristics as well as door-to-balloon time or door-to-drug time respectively.
Statistical analyses were performed using SAS versions 9.1 (SAS, Inc, Cary, NC) and Stata version 8.0 (Stata Corp, College Station, TX).
Results
Study Population
Baseline characteristics of the 3 groups, namely for the use of any reperfusion therapy, those treated with primary percutaneous coronary intervention, and those treated with fibrinolytic therapy are shown in Table 1. Patient and hospital characteristics were generally similar for all 3 groups with a majority being younger (age <70 years), men, and white patients. Diabetic patients comprised 18% to 21% and those with prior myocardial infarction comprised 17% to 19%. Patients treated with primary percutaneous coronary intervention were more likely to be treated during weekday daytime hours 8am-4pm (41%) or have cardiogenic shock (3%) as compared with patients treated with fibrinolytic therapy during weekday daytime (29%) or have cardiogenic shock (1%).
Table 1.
Baseline Characteristics of Study Cohorts
| Cohort for Use of Any Reperfusion Therapy | Cohort Treated with Primary PCI | Cohort Treated with Fibrinolytic Therapy | ||||
|---|---|---|---|---|---|---|
| Description | # | % | # | % | # | % |
| N | 440398 | 100.00 | 67207 | 100.00 | 183441 | 100.00 |
| Demographics | ||||||
| Age | ||||||
| Age <60 | 182894 | 41.53 | 31719 | 47.20 | 84140 | 45.87 |
| Age 60 to 69 | 104765 | 23.79 | 16100 | 23.96 | 45809 | 24.97 |
| Age 70 to 79 | 96045 | 21.81 | 13118 | 19.52 | 37683 | 20.54 |
| Age ≥80 | 56694 | 12.87 | 6270 | 9.33 | 15809 | 8.62 |
| Female | ||||||
| No | 297095 | 67.46 | 47950 | 71.35 | 127956 | 69.75 |
| Yes | 143303 | 32.54 | 19257 | 28.65 | 55485 | 30.25 |
| Race | ||||||
| White | 380685 | 86.44 | 57060 | 84.90 | 159283 | 86.83 |
| Black | 21966 | 4.99 | 3626 | 5.40 | 9091 | 4.96 |
| Hispanic | 12424 | 2.82 | 2114 | 3.15 | 5591 | 3.05 |
| Asian | 6292 | 1.43 | 1273 | 1.89 | 2722 | 1.48 |
| Other/Unknown | 19031 | 4.32 | 3134 | 4.66 | 6754 | 3.68 |
| Health insurance | ||||||
| Commercial (HMO/PPO) only | 175229 | 39.79 | 30240 | 45.00 | 81202 | 44.27 |
| Medicare only | 126381 | 28.70 | 15013 | 22.34 | 48112 | 26.23 |
| Medicare with any other insurance | 57409 | 13.04 | 9024 | 13.43 | 18139 | 9.89 |
| Medicaid or Self | 47604 | 10.81 | 8043 | 11.97 | 21025 | 11.46 |
| Other/Unknown | 33775 | 7.67 | 4887 | 7.27 | 14963 | 8.16 |
| Medical history | ||||||
| Current smoker | ||||||
| No | 279099 | 63.37 | 40743 | 60.62 | 110986 | 60.50 |
| Yes | 161299 | 36.63 | 26464 | 39.38 | 72455 | 39.50 |
| Diabetes | ||||||
| No | 348944 | 79.23 | 55174 | 82.10 | 148966 | 81.21 |
| Yes | 91454 | 20.77 | 12033 | 17.90 | 34475 | 18.79 |
| Prior MI | ||||||
| No | 355765 | 80.78 | 55932 | 83.22 | 152256 | 83.00 |
| Yes | 84633 | 19.22 | 11275 | 16.78 | 31185 | 17.00 |
| Hypertension | ||||||
| No | 226786 | 51.50 | 35316 | 52.55 | 100187 | 54.62 |
| Yes | 213612 | 48.50 | 31891 | 47.45 | 83254 | 45.38 |
| Hypercholesterolemia | ||||||
| No | 299441 | 67.99 | 43165 | 64.23 | 126308 | 68.85 |
| Yes | 140957 | 32.01 | 24042 | 35.77 | 57133 | 31.15 |
| Family history of CAD | ||||||
| No | 303735 | 68.97 | 47098 | 70.08 | 122896 | 66.99 |
| Yes | 136663 | 31.03 | 20109 | 29.92 | 60545 | 33.01 |
| Prior CHF | ||||||
| No | 411373 | 93.41 | 65058 | 96.80 | 176629 | 96.29 |
| Yes | 29025 | 6.59 | 2149 | 3.20 | 6812 | 3.71 |
| Prior PCI | ||||||
| No | 396519 | 90.04 | 57705 | 85.86 | 167642 | 91.39 |
| Yes | 43879 | 9.96 | 9502 | 14.14 | 15799 | 8.61 |
| Prior CABG | ||||||
| No | 406665 | 92.34 | 63173 | 94.00 | 171814 | 93.66 |
| Yes | 33733 | 7.66 | 4034 | 6.00 | 11627 | 6.34 |
| Stroke | ||||||
| No | 415298 | 94.30 | 64009 | 95.24 | 177402 | 96.71 |
| Yes | 25100 | 5.70 | 3198 | 4.76 | 6039 | 3.29 |
| Angina | ||||||
| No | 394263 | 89.52 | 61096 | 90.91 | 166270 | 90.64 |
| Yes | 46135 | 10.48 | 6111 | 9.09 | 17171 | 9.36 |
| Presentation | ||||||
| Chest pain at presentation | ||||||
| Yes | 401564 | 91.18 | 63656 | 94.72 | 176246 | 96.08 |
| No | 38834 | 8.82 | 3551 | 5.28 | 7195 | 3.92 |
| Cardiogenic shock | ||||||
| No | 431855 | 98.06 | 65159 | 96.95 | 181505 | 98.94 |
| Yes | 8543 | 1.94 | 2048 | 3.05 | 1936 | 1.06 |
| Systolic Blood Pressure <90 mmHg | ||||||
| No | 418381 | 95.00 | 63427 | 94.38 | 174956 | 95.37 |
| Yes | 22017 | 5.00 | 3780 | 5.62 | 8485 | 4.63 |
| Pulse >100 beats per minute | ||||||
| No | 375139 | 85.18 | 59612 | 88.70 | 162563 | 88.62 |
| Yes | 65259 | 14.82 | 7595 | 11.30 | 20878 | 11.38 |
| Current CHF | ||||||
| No | 381018 | 86.52 | 61275 | 91.17 | 164674 | 89.77 |
| Yes | 59380 | 13.48 | 5932 | 8.83 | 18767 | 10.23 |
| Time of presentation | ||||||
| Weekday daytime | 141476 | 32.12 | 27566 | 41.02 | 53905 | 29.39 |
| Weekday evening | 86357 | 19.61 | 11168 | 16.62 | 36660 | 19.98 |
| Weekday night | 81585 | 18.53 | 11293 | 16.80 | 34972 | 19.06 |
| Weekend daytime | 59104 | 13.42 | 8647 | 12.87 | 25867 | 14.10 |
| Weekend evening | 37670 | 8.55 | 4597 | 6.84 | 16842 | 9.18 |
| Weekend night | 34206 | 7.77 | 3936 | 5.86 | 15195 | 8.28 |
| Year of presentation | ||||||
| 1995 | 56930 | 12.93 | 4531 | 6.74 | 29352 | 16.00 |
| 1996 | 59677 | 13.55 | 5967 | 8.88 | 29950 | 16.33 |
| 1997 | 56917 | 12.92 | 6614 | 9.84 | 27697 | 15.10 |
| 1998 | 54210 | 12.31 | 6847 | 10.19 | 22930 | 12.50 |
| 1999 | 58760 | 13.34 | 8133 | 12.10 | 23952 | 13.06 |
| 2000 | 44550 | 10.12 | 7194 | 10.70 | 17524 | 9.55 |
| 2001 | 40631 | 9.23 | 8004 | 11.91 | 14797 | 8.07 |
| 2002 | 27240 | 6.19 | 6414 | 9.54 | 8871 | 4.84 |
| 2003 | 23604 | 5.36 | 7163 | 10.66 | 5454 | 2.97 |
| 2004 | 17879 | 4.06 | 6340 | 9.43 | 2914 | 1.59 |
| Hospital characteristics | ||||||
| Cardiac facilities | ||||||
| Non-invasive | 65567 | 14.89 | 0 | 0.00 | 46643 | 25.43 |
| Invasive but non-interventional | 84848 | 19.27 | 32 | 0.04 | 60167 | 32.80 |
| Interventional | 268030 | 60.86 | 61991 | 92.24 | 66274 | 36.13 |
| Interventional without OHS | 21953 | 4.98 | 5184 | 7.71 | 10357 | 5.65 |
| Teaching Status | ||||||
| No | 250987 | 56.99 | 34759 | 51.72 | 121258 | 66.10 |
| Yes | 189411 | 43.01 | 32448 | 48.28 | 62183 | 33.90 |
| Census division | ||||||
| West | 106378 | 24.15 | 19905 | 29.62 | 42967 | 23.42 |
| South | 138032 | 31.34 | 19439 | 28.92 | 56683 | 30.90 |
| Mid-West | 132827 | 30.16 | 23063 | 34.32 | 48301 | 26.33 |
| Northeast | 63161 | 14.34 | 4800 | 7.14 | 35490 | 19.35 |
CHF =congestive heart failure; CABG =coronary artery bypass surgery; CAD =coronary artery disease; HMO =health maintenance organization; MI= myocardial infarction; OHS =onsite heart surgery; PCI =percutaneous coronary intervention; PPO = preferred provider organization;
Multivariable Analysis of Delay and Use of Any Reperfusion
In adjusted analyses, patients with longer times between symptom onset and hospital presentation were significantly less likely to receive any reperfusion therapy (Figure 1, p<0.0001 for linear trend). For early presenters with times from symptom onset to hospital presentation of ≤1 hour, >1 to 2 hours, and >2 to 3 hours, patients with ST-elevation myocardial infarction were treated with any reperfusion therapy in 77% (reference group), 77% (odds ratio 1.0, p=0.81), and 73% (odds ratio 0.88, p<0.0001) respectively. In late presenters with times >9 to 10 hours, >10 to 11 hours, and >11 to 12 hours, the use of any reperfusion therapy was 53% (odds ratio 0.36, p<0.0001), 50% (odds ratio 0.33, p<0.0001), and 46% (odds ratio 0.27, p<0.0001) respectively.
Figure 1.
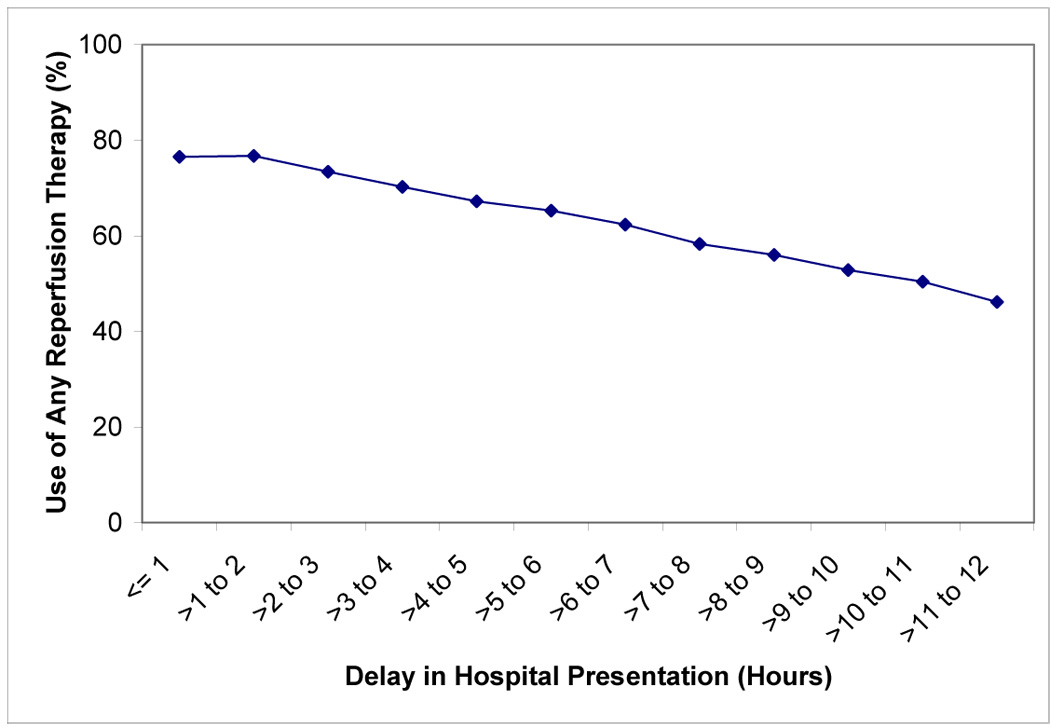
Delay in Hospital Presentation and Use of Any Reperfusion Therapy
Multivariable Analysis of Delay and Timeliness of Reperfusion Therapy
In adjusted analyses, among patients who were treated with primary percutaneous coronary intervention, those with longer time from symptom onset to hospital presentation had significantly longer door-to-balloon times (Figure 2, p<0.0001 for linear trend). For early presenters with times from symptom onset to hospital presentation of ≤1 hour, >1 to 2 hours, and >2 to 3 hours, patients were treated with door-to-balloon times of 99, 101, 106 minutes respectively. In late presenters with times of >9 to 10 hours, >10 to 11 hours, and >11 to 12 hours, door-to-balloon times were 123, 125, and 123 minutes respectively.
Figure 2.
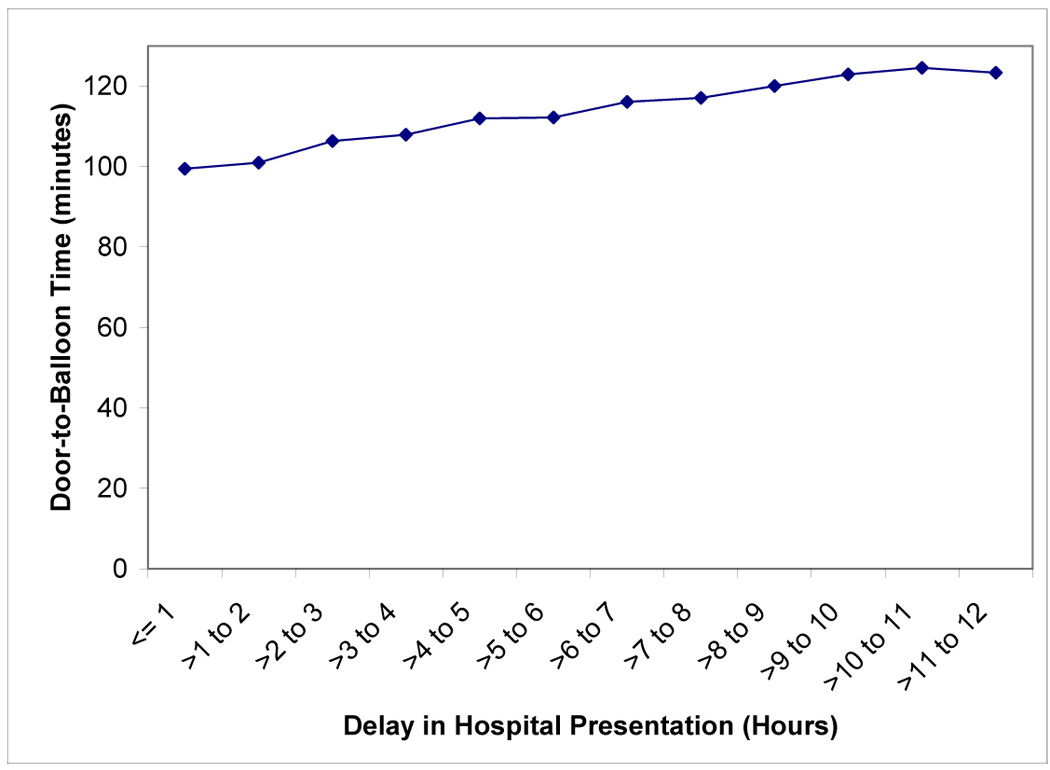
Delay in Hospital Presentation and Door-to-Balloon Time
Among patients who received fibrinolytic therapy, those with longer delay in hospital presentation also had significantly longer door-to-drug times (Figures 3, p<0.0001 for linear trend). For time intervals from symptom onset to hospital presentation of ≤1 hour, >1 to 2 hours, >2 to 3 hours, >9 to 10 hours, >10 to 11 hours, and >11 to 12 hours, patients were treated with door-to-drug times of 33, 34, 36, 46, 44, and 47 minutes respectively.
Figure 3.
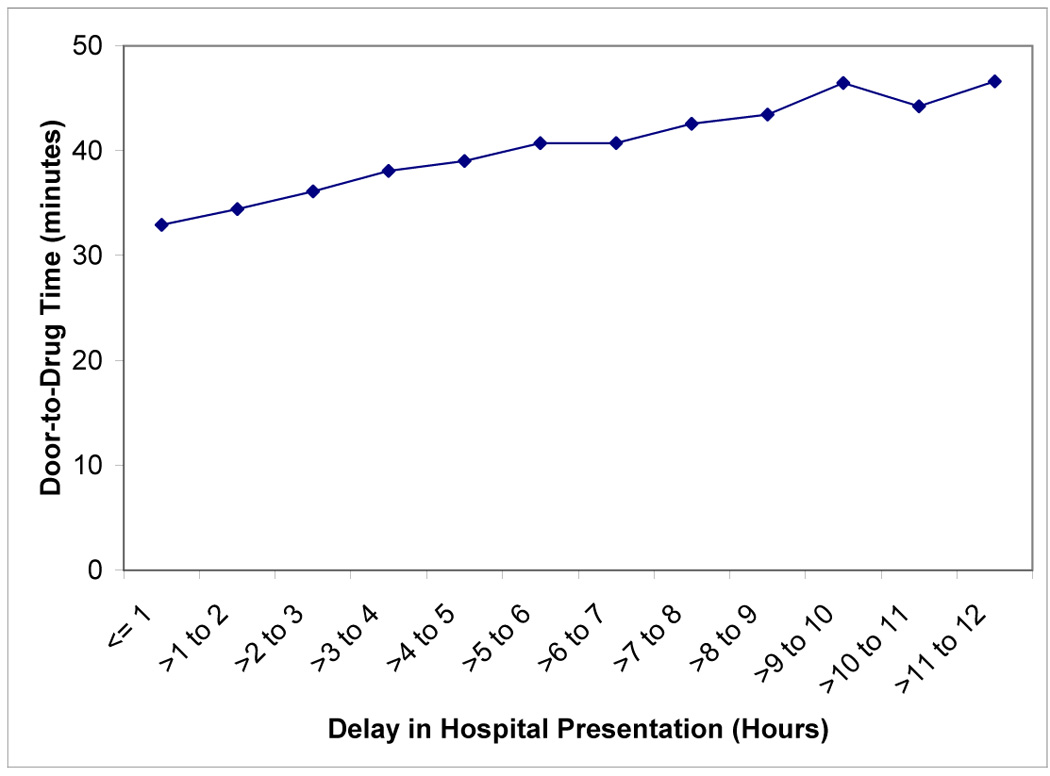
Delay in Hospital Presentation and Door-to-Drug Time
Multivariable Analysis of Delay and In-hospital Mortality
Among patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention, the time interval from symptom onset to hospital presentation was associated with increased in-hospital mortality even after adjusting for door-to-balloon time (Figure 4, p<0.0001 for linear trend). For early presenters with times from symptom onset to hospital presentation of ≤1 hour, >1 to 2 hours, and >2 to 3 hours, in-hospital mortality rates were 4.9% (reference group), 4.0% (odds ratio 0.82, p<0.0001), and 4.0% (odds ratio 0.76, p<0.0001) respectively. In comparison, late presenters with times >9 to 10 hours, >10 to 11 hours, and >11 to 12 hours had in-hospital mortality rates of 5.4% (odds ratio 0.91, p=0.62), 6.9% (odds ratio 1.2, p=0.34), and 6.6% (odds ratio 1.2, p=0.37) respectively.
Figure 4.
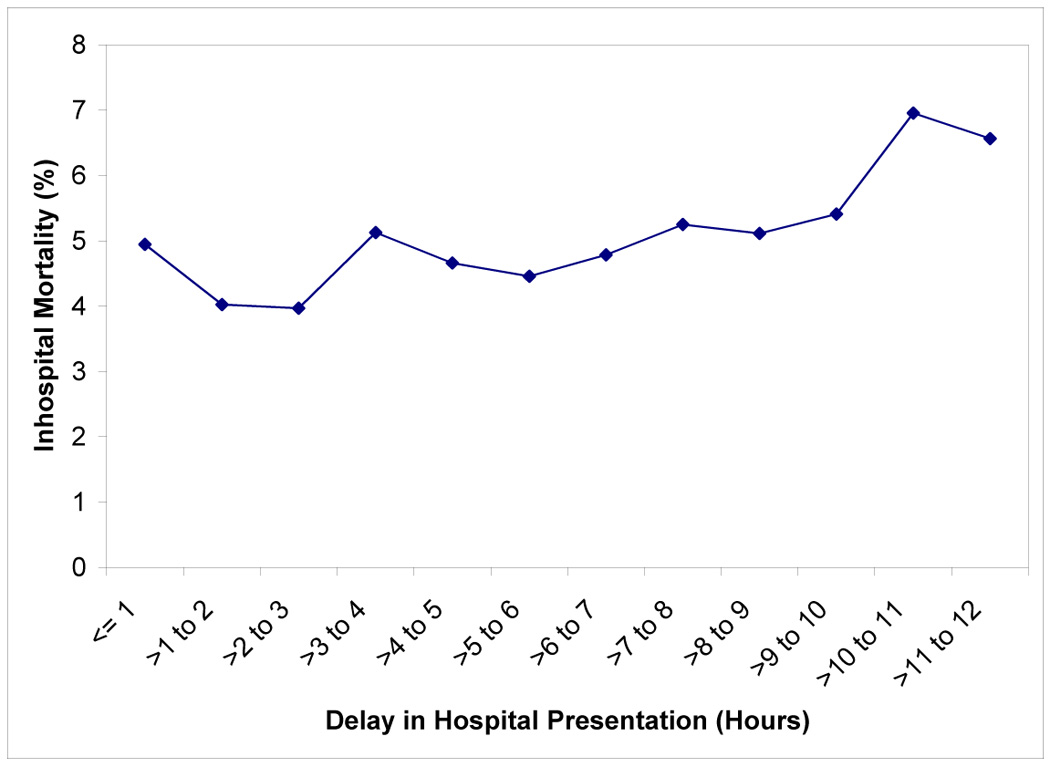
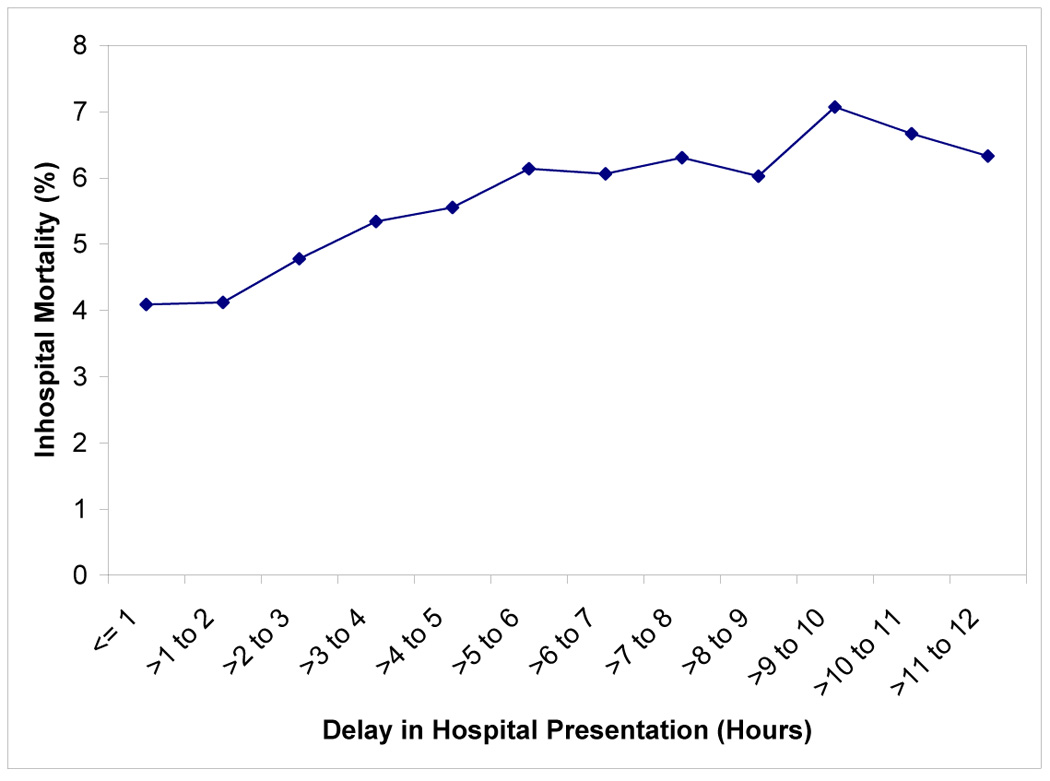
Figure 4A. Delay in Hospital Presentation and In-Hospital Mortality Among Patients Treated with Primary PCI
Figure 4B. Delay in Hospital Presentation and In-Hospital Mortality Among Patients Treated with Fibrinolytic Therapy
Among patients with ST-elevation myocardial infarction treated with fibrinolytic therapy, the time interval from symptom onset to hospital presentation was associated with increased in-hospital mortality even after adjusting for door-to-drug time (Figure 5, p<0.0001 for linear trend). For early presenters with times from symptom onset to hospital presentation of ≤1 hour, >1 to 2 hours, and >2 to 3 hours, in-hospital mortality rates were 4.1% (reference group), 4.1% (odds ratio 0.93, p=0.022), and 4.8% (odds ratio 0.98, p=0.52) respectively. In comparison, late presenters with times of >9 to 10 hours, >10 to 11 hours, and >11 to 12 hours had in-hospital mortality rates of 7.1% (odds ratio 1.5, p<0.0001), 6.7% (odds ratio 1.3, p=0.067), and 6.3% (odds ratio 1.2, p=0.17) respectively.
Discussion
In our study of patients with ST-elevation myocardial infarction spanning a 10 year period (1995–2004), we found that longer time intervals from symptom onset to hospital presentation were associated with reduced likelihood of receiving primary reperfusion therapy, and even among those treated, late presenters had significantly longer door-to-balloon and door-to-drug times. Although guidelines state that patients with ST-elevation myocardial infarction who present within 12 hours after onset of symptoms should be treated with rapid reperfusion therapy, we found longer times to hospital presentation may contribute to downstream hospital delays in administration of reperfusion therapy and consequently, delay may represent a novel risk factor associated with poorer quality of hospital care for ST-elevation myocardial infarction.
Our study is the largest contemporary report of the relationship between time from symptom onset to hospital presentation and subsequent treatment with and timeliness of reperfusion therapy and advances the existing research in several respects. Previous studies have shown that patients with longer door-to-balloon times6,11, longer door-to-drug times2, and longer total ischemic times between symptom onset and reperfusion therapy3,8 were associated with higher in-hospital mortality rates. However, our study is the first to demonstrate the independent effect of longer time intervals from symptom onset to hospital presentation among patients with ST-elevation myocardial infarction. We demonstrated that longer times to hospital presentation were associated with significantly lower use of any reperfusion therapy, longer door-to-balloon times, and longer door-to-drug times. The novel finding from our study is that longer times to hospital presentation is a risk factor for additional downstream hospital delays in treatment with and timeliness of any reperfusion therapy.
Furthermore, among patients treated with primary percutaneous coronary intervention or fibrinolytic therapy, longer times to hospital presentation were associated with increased in-hospital mortality rates, even after adjusting for other clinical factors and door-to-balloon time or door-to-drug time respectively. The high mortality rates observed among patients presenting within <2 hours of symptom onset may represent those who are at highest clinical risk such as those with cardiogenic shock. Despite the survival bias among late presenters (some late presenters who died out of hospital would not be included in this observational registry), there was still a linear trend for increased mortality rates among patients who presented late.
Possible explanations for the relationship between delay in hospital presentation and use of any reperfusion and timeliness of reperfusion therapy include: (a) patients who present early after onset of symptoms may elicit more urgency from providers to initiate reperfusion therapy; and (b) patients who present late may exhibit more atypical or no symptoms which subsequently lead to missed or late diagnosis as well as confusion or reluctance to administer reperfusion therapy. Among patients with ST-elevation myocardial infarction eligible to receive reperfusion, an optimal system of care should not exclude patients from reperfusion therapy or incur incremental delays in door-to-balloon or door-to-drug times simply because of longer times to hospital presentation.
Recently, there is great interest in strategies to reduce door-to-balloon time13 and to develop systems of care to transfer and increase number of patients who are eligible to receive primary percutaneous coronary intervention across large geographic regions.14 These innovative approaches have focused on coordinating and streamlining processes within a hospital and between hospital networks to reduce door-to-balloon time. In concert with these initiatives, reliable systems that deliver timely reperfusion to all eligible ST-elevation myocardial infarction patients should be developed regardless of the duration of delay in hospital presentation.22–23 With the knowledge that delay in hospital presentation negatively impacts use of any and timeliness in administering reperfusion therapy, attention should be focused on logistical and system issues for providers and patients. Providers should seek to eliminate hospital delays in reperfusion therapy for patients who present late after the onset of symptoms. Moreover, it will also be important to understand which patient groups are at greatest risk for longer delays24–27 as well as to evaluate novel interventions aimed at reducing delays in hospital presentation.
Acknowledgments
Funding: Research supported by grant R01 HL072575 of National Heart, Lung, and Blood Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: Collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet. 1994;343:311–322. [PubMed] [Google Scholar]
- 2.Newby LK, Rutsch WR, Califf RM, et al. Time from symptom onset to treatment and outcomes after thrombolytic therapy: GUSTO-1 investigators. J Am Coll Cardiol. 1996;27:1646–1655. doi: 10.1016/0735-1097(96)00053-8. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Mooradd M, Guriwitz JH, et al. Impact of time to treatment with tissue plasminogen activator on morbidity and mortality following acute myocardial infarction (NRMI 2) Am J Cardiol. 1998;82:259–264. doi: 10.1016/s0002-9149(98)00342-7. [DOI] [PubMed] [Google Scholar]
- 4.Zijlstra F, Patel A, Jones M, et al. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2–4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2002;23:550–557. doi: 10.1053/euhj.2001.2901. [DOI] [PubMed] [Google Scholar]
- 5.Gibson CM, Murphy SA, Kirtane AJ, et al. Association of duration of symptoms at presentation with angiographic and clinical outcomes after fibrinolytic therapy in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2004;44:980–987. doi: 10.1016/j.jacc.2004.05.059. [DOI] [PubMed] [Google Scholar]
- 6.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 7.De Luca G, Suryapranata H, Zijlstra F, et al. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42:991–997. doi: 10.1016/s0735-1097(03)00919-7. [DOI] [PubMed] [Google Scholar]
- 8.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 9.Brodie BR, Stone GW, Cox DA, et al. Impact of treatment delays on outcomes of primary percutaneous coronary intervention for acute myocardial infarction: Analysis from the CADILLAC trial. Am Heart J. 2006;151:1231–1238. doi: 10.1016/j.ahj.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Brodie BR, Webb J, Cox DA, et al. Impact of time to treatment on myocardial reperfusion and infarct size with primary percutaneous coronary intervention for acute myocardial infarction (from the EMERALD Trial) Am J Cardiol. 2007;99:1680–1686. doi: 10.1016/j.amjcard.2007.01.047. [DOI] [PubMed] [Google Scholar]
- 11.McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 12.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs AK, Antman EA, Ellrodt G, et al. Recommendation to develop strategies to increase the number of ST-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006;113:2152–2163. doi: 10.1161/CIRCULATIONAHA.106.174477. [DOI] [PubMed] [Google Scholar]
- 15.Rogers WJ, Canto JG, Lambrew CT, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the U.S. from 1990 through 1999: The National Registry of Myocardial Infarction 1, 2, and 3. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 16.Every NR, Frederick PD, Robinson M, et al. A comparison of the National Registry of Myocardial Infarction 2 with the Cooperative Cardiovascular Project. J Am Coll Cardiol. 1999;33:1886–1894. doi: 10.1016/s0735-1097(99)00113-8. [DOI] [PubMed] [Google Scholar]
- 17.Bland JM, Altman DG. The use of transformation when comparing two means. BMJ. 1996;312:1153. doi: 10.1136/bmj.312.7039.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bland JM, Altman DG. Transformations, means, and confidence intervals. BMJ. 1996;312:1079. doi: 10.1136/bmj.312.7038.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.King G, Tomz M, Wittenberg J. Making the most of statistical analyses: improving interpretation and presentation. Am J Pol Sci. 1998;44:341–355. [Google Scholar]
- 20.Nallamothu BK, Bates ER, Herrin J, et al. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction 3/4 analysis. Circulation. 2005;111:761–767. doi: 10.1161/01.CIR.0000155258.44268.F8. [DOI] [PubMed] [Google Scholar]
- 21.Magid DK, Wang Y, Herrin J, et al. Relationship Between Time of Day, Day of Week, Timeliness of Reperfusion, and In-Hospital Mortality for Patients With Acute ST-Segment Elevation Myocardial Infarction. JAMA. 2005;294:803–812. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 22.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 23.Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease. JAMA. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg RJ, Gurwitz JH, Gore JM. Duration of and temporal trends (1994–1997) in prehospital delay in patients with acute myocardial infarction: The Second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: The Worchester Heart Attack Study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 26.McGinn AP, Rosamond WD, Goff DC, et al. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: Experience in 4 U.S. communities from 1987–2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 27.Luepker RV. Delay in acute myocardial infarction: Why don’t they come to the hospital more quickly and what we can do to reduce delay. Am Heart J. 2005;150:368–370. doi: 10.1016/j.ahj.2005.05.012. [DOI] [PubMed] [Google Scholar]


