Abstract
To better understand the extent that empirically supported and promising substance abuse treatment approaches are implemented in community settings, treatment providers were surveyed regarding their perceptions and use of several psychosocial and pharmacological treatment interventions. Program directors (n=30) and staff members (n=331) from diverse community settings rated the effectiveness and extent of use of various treatment interventions, and provided information on program and workforce characteristics via self-administered questionnaires. On average, program directors and staff rated the psychosocial treatment interventions as effective, with the exception of vouchers/motivational incentives. About half of the treatment providers did not know the effectiveness of certain pharmacological treatments, including buprenorphine and naltrexone. Respondents from the majority of programs (55%–80%) reported using Motivational Enhancement Therapy, Community Reinforcement Approach, and Supportive Expressive Psychotherapy. The extent that programs used several of the treatment interventions was related to organizational training and information resources. The study findings provide important information regarding training and research dissemination efforts.
Keywords: Substance use disorders, Treatment workforce, Evidence-based treatment
1. Introduction
The adoption and implementation of empirically supported substance abuse treatment interventions in community settings continues to be an important topic of concern. Treatment providers are challenged to evaluate a wide array of interventions with varying levels of empirical support in order to select the best available technology to incorporate into clinical care. Programs are further tasked with determining whether the conditions and populations with which an innovation has been found to be effective are sufficiently comparable to justify use of the innovation in their setting (Brown, 2000).
Although many substance abuse and mental health interventions have been shown to be both clinically efficacious and cost-effective, they are often not widely adopted, and not sustained beyond the period of external funding (Roy-Byrne et al., 2003). Challenges of implementing evidence-based practices in community settings have been described (Miller, Zweben, & Johnson, 2005; Lamb, Greenlick & McCarty, 1998; Rawson, Marinelli-Casey, & Ling, 2002), and several studies have examined the relationship of organizational and workforce characteristics and the use of evidence-based practices (Fuller, Rieckmann, McCarty, Smith, & Levine, 2005; Knudsen, Roman, Ducharme, & Johnson, 2005). Further study of providers’ perspectives and experiences with a variety of treatment interventions are needed, particularly in relation to program and workforce characteristics. This knowledge will help to develop implementation strategies that take into account the intuitive appeal of various treatment approaches as well as training-related factors that facilitate the use of empirically supported treatment approaches. Treatment providers are key stakeholders and critical partners in the diffusion of new practices, and they exercise an important influence over the care that is provided (Sullivan et al., 2005). The present study examined treatment providers’ perspectives on the effectiveness of empirically supported and promising treatment interventions, and the extent these interventions are used in relation to programs’ training and information resources. By understanding how programs that use empirically supported interventions acquire treatment information, areas for improving staff training and research dissemination efforts can be identified.
1.1. Practitioner perspectives on treatment effectiveness
To better understand addiction treatment providers’ attitudes and beliefs about various treatment innovations, several studies have investigated the extent to which behavioral and pharmacological treatment approaches are viewed as effective in community-based programs. For example, Forman et al (2001) found that most treatment providers supported the increased use of research-based innovations and 12-step treatment approaches, however fewer providers endorsed the use of naltrexone and methadone. Another study found that treatment providers perceived 12-Step Facilitation and Motivational Interviewing as more effective than Contingency Management, Behavior Couples Therapy, and specific pharmacological treatments (McGovern, Fox, Xie, & Drake, 2004). Moreover, specific characteristics of the treatment workforce have been found to be associated with positive attitudes toward evidence-based practices. Aarons (2004) surveyed mental health program managers and clinicians regarding attitudes toward evidence-based practices, and found higher levels of staff education and tenure were associated with more positive attitudes toward manualized therapies and research based interventions.
It is important to understand treatment providers’ perspectives about the effectiveness of innovations, as studies have shown clinicians’ beliefs and expectations influence the extent that interventions are used. For example, nurses with higher outcome expectations toward a smoking cessation intervention spent more time counseling their patients about quitting than nurses with lower expectations (Borrelli et al., 2001). Similarly, Obert et al (2005) conducted a study in which a manualized treatment was introduced into a community treatment setting, and found that getting buy-in from personnel at all levels of the organization is critical before attempting to implement new substance abuse treatment practices.
1.2. Workforce characteristics related to use of treatment innovations
In addition to practitioner attitudes and beliefs, program and workforce characteristics have been found to affect the extent that innovative treatment techniques are implemented in community based programs. A study of substance abuse treatment in the Veterans Administration investigated attitudes and familiarity with evidence-based practices, and concluded that although treatment providers identified several treatments (e.g., smoking cessation treatment, naltrexone, and methadone dosing >60 mg/day) as having a strong evidence base, these treatments were not widely implemented (Willenbring et al., 2004). Program leaders commonly reported the lack of belief in their usefulness was a somewhat important barrier, while the lack of administrative support, time, and staff knowledge were more commonly perceived as significant obstacles to implementation.
A large-scale study of privately funded substance abuse treatment centers found that “environmental scanning” (i.e., seeking out treatment information from publications, participation in professional development, and other sources) was related to organizational use of a greater number of treatment innovations (Knudsen & Roman, 2004). In contrast, a study of community treatment providers found that although clinicians reported frequently using treatment innovations, including cognitive-behavioral therapy, 12-step approaches, and techniques consistent with a motivational interviewing approach, most reported having no or minimal formal workshop training, and infrequently using therapy manuals in clinical practice (Ball et al., 2002).
1.3. Empirically supported substance abuse treatment approaches
McGovern & Carroll (2003) described the “hierarchy of evidence” for various substance abuse treatment interventions including pharmacological (e.g., buprenorphine, disulfiram, methadone, naltrexone) and behavioral treatments (e.g., Contingency Management, Motivational Enhancement Therapy, Supportive-Expressive psychotherapy), categorizing these treatment approaches as “empirically validated” and “probably efficacious.” Miller & Wilbourne (2002) evaluated the efficacy and methodological quality of 361 controlled clinical trials for treatment of alcohol use disorders and found the treatment approaches with the strongest evidence for efficacy included brief interventions, Motivational Enhancement, Community Reinforcement Approach, and the medications naltrexone and acamprosate.
Chambless & Ollendick (2001) categorized the level of empirical evidence for psychological treatment practices for substance use disorders and other conditions (e.g., anxiety, depressive disorders). They found that studies were generally in agreement about the extent of evidence for treatment practices for some conditions, but there was less agreement for the treatment practices for chemical dependency. For example, the authors were unable to determine whether Community Reinforcement Approach and Motivational Interviewing met the criteria for category 1 (well-established/efficacious) or category 2 (probably efficacious) treatment approaches. These findings suggest there is some degree of uncertainty in determining which innovations are considered empirically validated.
Regarding pharmacotherapies, methadone, buprenorphine, disulfiram and naltrexone have undergone rigorous experimental designs and adherence protocols, and are considered Phase IV pharmacotherapeutic interventions by the United States Food and Drug Administration Center for Evaluation and Research (McGovern & Carroll, 2003). In addition, NIDA (1999) has identified agonist maintenance therapy as a specific research-based component of treatment for opiate dependent individuals. Studies have documented the effectiveness of disulfiram and naltrexone for the treatment of alcohol dependence (Miller & Wilbourne, 2002; Rosenthal, 2006; Anton et al., 2006), and methadone and buprenorphine for opiate dependence (McGovern & Carroll. 2003; Vocci, Acri, & Elkashef, 2005).
1.4. The present study
The present study, the Practice and Research Collaborative (PARC), examined treatment providers’ perspectives of the effectiveness of empirically supported treatment interventions, and the impact of training-related factors on the use of these interventions. Programs’ training resources and staff education were examined, as formal and ongoing training in substance abuse treatment has been identified as an important part of the transfer of evidence-based approaches into widespread practice (Simpson, 2002; Walters, Matson, Baer, & Ziedonis, 2005). Based on previous findings in which programs that engaged in environmental scanning used more treatment innovations (Knudsen & Roman, 2004), this study hypothesized that programs able to acquire treatment information from resources outside of their programs (e.g., journals, conferences, professional associations) would be more likely to use empirically supported treatment interventions to a greater extent. In addition, use of these interventions was hypothesized to be positively associated with staff education and programs’ training resources.
2. Methods
Program directors, counselors and clinical staff from diverse program settings in California were surveyed regarding the effectiveness and use of psychosocial treatment approaches that the National Institute on Drug Abuse (1999) has identified as scientifically based. These interventions include Motivational Enhancement Therapy, Supportive Expressive Psychotherapy, Community Reinforcement Approach, Matrix model, and Voucher-based reinforcement therapy. Treatment providers were also surveyed regarding several empirically supported pharmacological interventions, including methadone, buprenorphine, disulfiram and naltrexone. In addition, respondents provided information related to program and workforce characteristics.
2.1. Program Director and Workforce Survey Procedures and Sampling
A total of 32 program directors who oversee 43 treatment sites (28 outpatient, 10 residential, and 5 mixed modality) in 13 counties that participated in the California Treatment Outcome Project (CalTOP)a were asked to complete self-administered questionnaires. The CalTOP was a multi-site and multi-county prospective study conducted to develop, implement, and pilot test an automated outcome monitoring system for the statewide alcohol and other drug system of care. The programs cover a wide geographic area throughout northern, central and southern regions of California, and include both urban and rural settings in economically and demographically diverse communities. In the present study, program directors were contacted by telephone, provided with a description of the study, and asked to complete the Program Director surveys.
Program directors then provided a list of all program staff members who had direct contact with clients, and each staff member was asked to complete the Workforce survey. Program Director and Workforce surveys were mailed to directors and staff members at their programs. Study procedures were approved by the University of California, Los Angeles Institutional Review Board. The surveys were collected between January and September 2004.
Program Director Survey Participants
A total of 30 program directors (94%) who managed 41 treatment sites returned completed survey questionnaires; one director declined to participate, and one provided a list of program staff members but did not complete the Program Director survey. The questionnaire took approximately one hour to complete and respondents received $100 for their participation if their counties/programs allowed payment.
Among program directors (n=30), 50% reported their highest level of education was an associate degree or some college; 10% had a Bachelor’s degree, 27% had a Master’s degree, and 13% had a doctoral or other professional degree. On average, program directors had worked in the field of substance abuse treatment for 13.9 years (SD=6.8), and had been in their current positions for 6.6 years (SD=4.8); 53% were in their current position for less than five years, and 17% were in their current positions for one year or less. About two-thirds (63%) were women; 61 % were White (non-Latino), 7% African American (non-Latino), and 16% Latino. The average age of program directors was 47.9 (SD=8.0).
Workforce Survey Participants
A total of 366 staff members who had direct client contact (i.e., management staff, clinical supervisors, counselors, case managers, aides, medical staff, receptionists, interns, volunteers) were invited to complete the staff survey. Ninety percent of program staff (n=331) representing 31 programs (42 separate treatment sites) returned completed survey questionnaires; eight declined to participate and 27 did not respond to the questionnaire. The questionnaire took approximately 30 minutes to complete and respondents received $25 for their participation if their counties/programs allowed payment. Responses from staff members who reported their primary role as administrative support or clerical (e.g., office manager, receptionist, data entry worker; n=37) were excluded from the present analyses, as they may not have had knowledge of, or experience with the treatments identified in the survey. Thus, analyses of the Workforce survey included responses from a sample of 294 program staff members.
Among program staff (n=294), 85% reported that they provide counseling to clients and/or supervise counselors. Over three-fourths of program staff (78%) reported being counselors, case managers or in related positions (e.g., recovery specialist, behavioral health specialist); 9% were clinical supervisors or program managers; 6% were nurses; 1% were physicians; and 6% reported being in other positions (e.g., intern, counselor aide, house manager). Eight percent reported having a high school diploma or fewer years of education; 58% had an associate degree or completed some college; 19% had Bachelor’s degrees, 14% had Master’s degrees, and 2% had doctoral or other professional degrees. On average, program staff had worked in the field of substance abuse treatment for 7.8 years (SD=6.2), and had been in their current positions for 4.4 years (SD=4.7); 71% were in their current position for less than five years, and 23% were in their current positions for one year or less. Over two-thirds (70%) reported being in recovery; 60% were women; 60% were White (non-Latino), 13% were African American (non-Latino), 17% were Latino, and 10% reported being multiracial or other racial background. The average age of program staff was 48.0 (SD=9.5).
2.2. Survey measures
2.2.1. Treatment effectiveness and extent of use of interventions
Program Director and Workforce survey measures relevant to the present paper included survey items from the University of Georgia National Treatment Center Study (NTCS) pertaining to provider perspectives about the effectiveness and extent of use of psychosocial and pharmacological treatment approaches (Knudsen, Johnson, Roman, & Oser, 2003). Program Directors and staff members were asked to indicate the extent that they considered the following treatment interventions to be effective, based on their knowledge of, and personal experience with each approach: Motivational Enhancement Therapy (MET), Solution-Focused Therapyb (SFT), Community Reinforcement Approach (CRA), Supportive Expressive Psychotherapy (SEP), Matrix model, motivational incentives/vouchers, and medications including methadone, disulfiram, naltrexone and buprenorphine. Respondents were also asked to rate the extent to which each of these treatment interventions was used at their programs. Treatment effectiveness ratings ranged from 1 to 5, with 1 = not at all effective and 5 = very effective; ratings of the extent of use ranged from 1 = never used to 5 = always used when clinically indicated. Respondents were also given the option to select “don’t know” regarding the effectiveness and extent of use of each treatment.
2.2.2. Training resources
Training resources were assessed using a six-item training resources scale adapted from the Texas Christian University Organizational Readiness for Change (ORC) survey (Lehman, Greener, & Simpson, 2002). The scale assessed staff members’ perceptions of their programs’ support for counselor training and development, i.e., whether continuing education and attending professional conferences are priorities, and are funded by the program. Additionally, the scale assessed staff members’ satisfaction with the training opportunities available in the past year, and whether clinical staff members at the program are well trained. Responses to each question ranged from 1=strongly disagree to 5=strongly agree. Cronbach’s alpha was .72.
2.2.3. Information resources
The survey included items pertaining to the extent to which program staff acquire information about new treatment techniques from various resources (i.e., journals and professional publications; conferences, courses and seminars; membership in professional provider associations; conversations with members of other treatment organizations; conversations with county or state staff; and conversations with research entities). Each specific source of information was rated on a scale of 0–5 (0 indicated the information source was not used, and 5 indicated the information source was used to great extent). Knudsen & Roman (2004) summarized these information resources into a single measure of “environmental scanning.” Similarly, in the present analyses a summary variable was created in which each respondent’s scores on the six items were summed for an overall information resources score ranging from 0 to 30.
2.4. Data Analyses
We conducted descriptive statistics (means or percent) on ratings of treatment effectiveness by program directors and staff. Spearman correlation analyses were conducted to examine the bivariate association between programs’ use of empirically supported treatment interventions and training resources, staff education, and extent programs acquire treatment information from resources outside of their programs. Multiple regression analyses further assessed the extent of use of treatment interventions in relation to these factors simultaneously (programs’ training resources, staff education and information resources). The perceived effectiveness ratings of each intervention were also included in each model (e.g., the effectiveness ratings of MET were included in the model predicting the extent of use of MET). The parameter estimates reported are unstandardized beta coefficients. Unless otherwise indicated, the significance level (two-tailed) was set at p<.05.
3. Results
3.1. Perspectives on effectiveness of treatment interventions
On average, program directors and staff rated the psychosocial treatment interventions as somewhat effective (between 3.0 and 3.6 on a 5-point scale), with the exception of vouchers/motivational incentives (Table 1). The mean ratings of effectiveness of the pharmacotherapies were between 2.3 and 2.9 on the 5-point scale. Multivariate analyses of variance were conducted to examine whether staff and director ratings differed for the psychosocial treatment interventions overall and pharmacological interventions overall; no significant differences were observed for the psychosocial interventions (Wilks’ λ = .88, F(6, 90) = 2.11, p=.07) or for the pharmacological interventions (Wilks’ λ = .93, F(4, 120) = 2.36, p=.07). Many staff respondents and directors did not know the effectiveness of the Matrix model and several pharmacological treatments, including buprenorphine or naltrexone. Uncorrected chi-square tests indicated that the percentages of program staff who reported not knowing the effectiveness of the treatment interventions did not differed from the percentages reported by program directors.
Table 1.
Program director and staff mean ratings of treatment effectiveness (1=not at all, 5=very effective), and percent reporting don’t know effectiveness
| Mean rating (SD) | % Don't know | |||
|---|---|---|---|---|
| Director | Staff | Director | Staff | |
| Motivational Enhancement Therapy | 3.46 (0.86) | 3.54 (1.36) | 16.8 | 13.3 |
| Solution-Focused Therapy | 3.33 (1.03) | 3.55 (1.40) | 20.2 | 20.0 |
| Community Reinforcement Approach | 3.57 (0.90) | 3.43 (1.39) | 24.1 | 23.3 |
| Supportive Expressive Psychotherapy | 2.95 (0.89) | 3.44 (1.38) | 30.0 | 33.3 |
| Matrix Model | 3.58 (1.00) | 3.14 (1.42) | 42.6 | 60.0 |
| Vouchers (motivational incentives) | 2.65 (1.06) | 2.79 (1.12) | 32.4 | 43.3 |
| Methadone | 2.88 (1.14) | 2.92 (1.22) | 11.9 | 13.3 |
| Buprenorphine | 2.31 (1.08) | 2.86 (1.17) | 46.9 | 46.7 |
| Disulfiram | 2.39 (1.20) | 2.79 (1.09) | 22.4 | 23.3 |
| Naltrexone | 2.32 (1.06) | 2.60 (1.12) | 49.8 | 36.7 |
3.2. Program use of treatment interventions
The treatment interventions rated as effective (i.e., MET, SFT, CRA and SEP) were also most commonly used; between 53% and 80% of programs used these interventions (Figure 1). The Matrix model was among the higher rated treatments in terms of effectiveness, but was not commonly used, although most of the programs that used this approach used it frequently or always when clinically indicated (as compared to never or occasionally). Although the majority of programs used MET, SFT, CRA and SEP, half or more of the programs used these approaches rarely or occasionally. Most staff (76–92%) and program directors (90–100%) rated the extent of use of the treatment interventions rather than selecting the “don’t know” option (data not shown).
Figure 1.
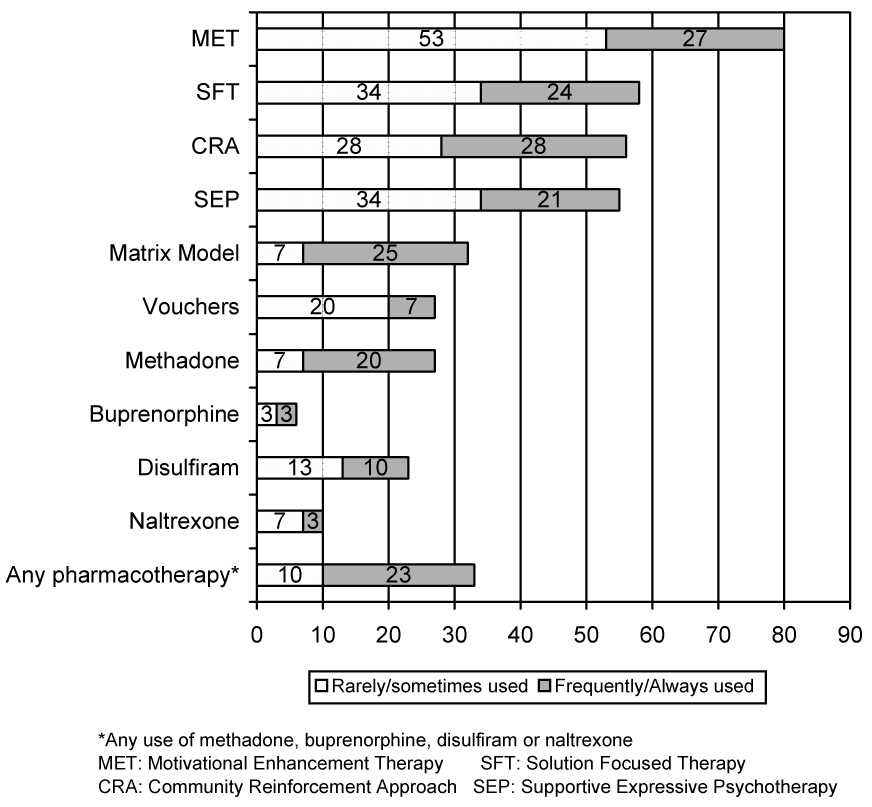
Percent of programs using specific treatment interventions rarely or occasionally and frequently or always
3.3. Staff training, education and information resources
Statistically significant positive correlations were observed between the extent of training resources and use of several treatment interventions, i.e., MET, CRA, Matrix model, buprenorphine and naltrexone. Fewer significant correlations were observed between staff education and extent of intervention use. Greater use of information resources was significantly related to the extent that MET, SEP, Matrix model, methadone, disulfiram and naltrexone were used (Table 2).
Table 2.
Correlations of staff-reported extent of use of treatment interventions with training resources, staff education and information resources
| Training Resources | Staff Education | Information Resources | ||||
|---|---|---|---|---|---|---|
| Treatment | r | p | r | p | r | p |
| Motivational Enhancement Therapy | .21 | <.001 | .11 | .093 | .20 | <.01 |
| Solution-Focused Therapy | .11 | .111 | .11 | .093 | .13 | .057 |
| Community Reinforcement Approach | .23 | <.001 | −.06 | .397 | .07 | .287 |
| Supportive Expressive Psychotherapy | .13 | .055 | .19 | <.01 | .19 | <.01 |
| Matrix Model | .19 | <.01 | .12 | .107 | .34 | <.001 |
| Vouchers | .09 | .201 | −.07 | .290 | .01 | .895 |
| Methadone | .03 | .661 | .11 | .103 | .34 | <.001 |
| Buprenorphine | .15 | <.05 | −.02 | .766 | .02 | .819 |
| Disulfiram | .13 | .056 | .18 | <.01 | .39 | <.001 |
| Naltrexone | .20 | <.01 | .00 | .952 | .21 | <.01 |
3.4. Multivariate analyses
Table 3 presents results of regression analyses examining the extent of use of psychosocial and pharmacological treatment interventions, in relation to perceived effectiveness of each intervention, and training resources, staff education, and information resources. Perceived effectiveness of each treatment significantly predicted greater use of the treatment. In general, more training resources predicted greater use of the psychosocial interventions, but not the use of the pharmacotherapies. Higher staff education was associated with greater use of SEP. Programs’ information resources were significantly related to the use of MET, Matrix model, methadone and disulfiram.
Table 3.
Staff report of extent of use of treatment interventions adjusted for perceived treatment effectiveness, training resources, staff education, and information resources
| MET | SFT | CRA | SEP | Matrix Model | Vouchers | Methadone | Buprenorphine | Disulfiram | Naltrexone | |
|---|---|---|---|---|---|---|---|---|---|---|
| Parameter Estimate (SE) | ||||||||||
| 0.52 | 0.55 | 0.62 | 0.56 | 0.60 | 0.51 | 0.57 | 0.54 | 0.56 | 0.51 | |
| Effectiveness Ratings | (0.08)** | (0.10)** | (0.09)** | (0.10)** | (0.08)** | (0.10)** | (0.09)** | (0.09)** | (0.08)** | (0.09)** |
| 0.03 | 0.01 | 0.05 | 0.03 | 0.03 | 0.03 | 0.00 | 0.01 | 0.00 | 0.01 | |
| Training Resources | (0.01)* | (0.01) | (0.01)** | (0.01) | (0.02)* | (0.01)* | (0.02) | (0.01) | (0.01) | (0.01) |
| 0.15 | −0.04 | −0.08 | 0.23 | 0.03 | −0.12 | 0.19 | 0.03 | 0.20 | 0.03 | |
| Staff Education | (0.18) | (0.19) | (0.18) | (0.21) | (0.16) | (0.22) | (0.23) | (0.22) | (0.22) | (0.15) |
| 0.04 | 0.04 | 0.03 | 0.04 | 0.08 | 0.00 | 0.07 | 0.01 | 0.08 | 0.01 | |
| Information Resources | (0.02)** | (0.02) | (0.02) | (0.02)* | (0.02)** | (0.02) | (0.02)** | (0.01) | (0.02)** | (0.01) |
| R-square | 0.24 | 0.18 | 0.30 | 0.24 | 0.27 | 0.26 | 0.24 | 0.17 | 0.22 | 0.18 |
MET: Motivational Enhancement Therapy; SFT: Solution Focused Therapy; CRA: Community Reinforcement Therapy; SEP: Supportive Expressive Psychotherapy
p<.01
p<.05
4. Discussion
This study examined treatment providers’ perspectives on specific substance abuse treatment interventions, the extent these interventions were used in community based programs, and whether training-related factors were associated with use of specific interventions. Similar to previous findings (Roy-Byrne et al., 2003; Willenbring, et al, 2004), most of the empirically supported psychosocial treatment approaches were perceived to be efficacious. However, these approaches were not routinely used in many community-based programs in California. Program directors’ effectiveness ratings did not differ significantly from staff ratings, nor did the percentages of directors and staff who reported they did not know the effectiveness of the interventions. The high rates of treatment providers who did not know the effectiveness of many of the interventions suggest personnel at all levels of the organization (e.g., directors, managers, counselors) may need to increase their exposure to empirically supported approaches, so that these approaches can be further integrated into community based programs. Increased efforts of researchers and policy makers toward wider dissemination of treatment information, presented in a way that is user friendly and tailored to the audience is an important initial step in the innovation diffusion process (Rogers, 1995).
A large proportion of both program directors and staff reported not knowing the effectiveness of several of the medications, and the mean effectiveness ratings were generally lower than the ratings for the psychosocial interventions. While four of the six psychosocial interventions were used in more than half of the programs, only one-third of the programs used any of the pharmacotherapies examined in this study. This finding follows the same trend found in Willenbring, et al (2004), in which 61% of program leaders reported a high level of current implementation of cognitive behavioral relapse prevention, but few (less than 10%) reported a high level of implementation of naltrexone or disulfiram for alcohol dependence.
Although there appear to be few research studies on the use of Solution-Focused Therapy (SFT) for treatment of substance abuse problems, SFT was considered by directors and staff as one of the more effective treatment approaches, and was used in more than half of the programs. SFT has been described in the NIDA’s Approaches to Drug Abuse Counseling (Miller, 2000) as a brief therapy approach developed over the past 20 years designed to help clients engage their own unique resources in solving the problems that bring them into treatment. SFT has been used with diverse patient populations in a variety of practice settings including office-based outpatient settings (Greenberg, Ganshorn, & Danilkewich, 2001; Hagen & Mitchell, 2001). The high ratings of effectiveness and use from both directors and staff suggest treatment providers may find the techniques and tools used in SFT fit particularly well with the complex needs of substance-abusing populations. Empirical support for these beliefs should be further examined in future studies.
As expected, the extent that interventions were perceived to be effective significantly predicted the extent they were used. In addition, training and information resources were significantly related to the use of treatment interventions. Programs in which staff perceived training as a high priority (e.g., training was ongoing and adequately funded), were more likely to use a range of empirically supported psychosocial treatment interventions. This finding supports Hoge and colleagues’ assertion that the tentative nature of what we know about substance abuse, mental illnesses, and the treatment of these disorders necessitates ongoing training, education and a “process” of lifelong learning. This process is essential if we are to shorten the well-documented 15–20 year delay between the demonstration of a treatment’s effectiveness and its widespread use (Hoge, Huey, & O'Connell, 2004). Funding and policies that support the provision of training resources may further promote the use of empirically supported treatment.
The extent that psychosocial and pharmacologic interventions were used was associated with treatment providers’ capacity to obtain treatment information from sources outside of their organizations, including journals, other treatment organizations, and county, state and research entities. This finding highlights the importance of disseminating information through multiple sources in order to achieve wider implementation, and supports Knudsen and Roman’s (2004) findings in which privately funded substance abuse treatment centers that engaged in “environmental scanning” used a greater number of treatment innovations.
Staff education level was not associated with the use of many of the treatment interventions examined in this study. While Knudsen and Roman (2004) found counselor education to be an important factor in the organizational use of substance abuse treatment innovations, relatively few of the treatment providers in the present study (35%) had completed a Bachelors degree. Thus, among primarily non-degreed treatment providers, education level may be a less important factor in the use of treatment innovations than programs’ training and information resources. Although the pursuit of advanced degrees among directors and staff would be expected to promote the use of treatment innovations, controlling for staff education in the multivariate analyses indicates that training and information resources remained important factors, apart from staff education.
Having adequate training and information resources are important aspects of transferring empirically supported interventions into community settings. However, other barriers to integrating effective interventions into widespread clinical use have been described, including the instability of the organizational, administrative and personnel infrastructures of treatment programs (McLellan & Meyers, 2004). Staff and management turnover, facility closures and restructuring and severe financial pressures, particularly for small, stand-alone treatment facilities, are substantial challenges to implementing and sustaining treatment innovations. In addition, the extent to which a proposed intervention fits with the organizational culture, goals, and capacities of program personnel will often determine whether the intervention is adopted and implemented. Given these issues and challenges, it is important to note that overall, many of the treatment providers viewed the interventions examined in this study as effective or somewhat effective. Although the interventions do not appear to be used extensively, most of the programs have at least some experience using empirically supported treatment approaches.
This study has several limitations. The programs in this study were selected based on their previous participation in the California Treatment Outcome Project (CalTOP), in which they were involved in collection of client satisfaction data and assessing treatment outcomes. These programs may have had more exposure to research, which may not reflect experiences of other community-based treatment providers. Many of these programs provided treatment to individuals dependent on methamphetamine, and although methamphetamine abuse has become a tremendous challenge for the entire nation (U.S. Department of Justice, 2007), this study’s findings may apply more closely to programs with treatment populations that include persons dependent on methamphetamine than programs without methamphetamine-dependent individuals. Because only 13 out of 58 counties were included in the study, the experience of other counties may not be fully represented. National studies indicate a greater proportion of treatment providers have advanced degrees and are employed as physicians, nurses and social workers (Mulvey, Hubbard, & Hayashi, 2003; McLellan, Carise, & Kleber, 2003) than the providers in the present sample. Consequently, California provider perspectives and use of empirically supported treatments may differ from national samples. Also, the measures of treatment intervention use were reported by treatment providers, and the fidelity of providers’ adherence to the principles of each treatment intervention was not assessed. Reliance on self report measures may have resulted in an over-estimation of the extent of intervention use. In addition, detailed descriptions of each treatment intervention were not provided in the survey. However, the data provide useful information regarding the extent an intervention is perceived as effective and used in relation to other interventions, and in relation to training and information resources available to programs.
Ensuring sufficient training resources (e.g., in-service training, continuing education and conferences) are provided in a format that is flexible which can be integrated into staff schedules may improve knowledge and implementation of research-based treatment techniques. Our study findings support Knudsen and Roman’s (2004) assertion that innovation adoption cannot solely be based on the existing knowledge resources within an organization, and program administrators should encourage their treatment workforce to seek and use external sources of treatment information. Treatment providers who are able to expand their knowledge and use of evidence-based treatment approaches may be better able to offer more choices and opportunities for treatment and recovery to their clients. Further study is needed on what type of information is useful and meaningful to treatment providers, how it should be “packaged,” and through what medium (e.g., journals, conferences, peers, etc.) it should be provided. In addition, research is needed to investigate how choices are made within organizations regarding adoption of innovations, program and workforce factors that facilitate and impede the adoption of innovations, and whether clients in programs that use a wider array of empirically supported treatment interventions experience better outcomes. Consideration of providers’ perspectives on treatment effectiveness, program resources, prior research experience, and current treatment context is essential to enhance the likelihood that empirically supported interventions are adopted and implemented.
Acknowledgments
The work on this manuscript was supported by grant DA014472 from the National Institute on Drug Abuse, Bethesda, MD. The authors thank the treatment providers who participated in the study, and Carter Bartee and Joy Yang for their assistance with data collection. Preliminary results were presented at the 67th Annual Meeting of the College on Problems of Drug Dependence, Orlando, FL. June, 2005.
Footnotes
Evans & Hser (2004) provide a detailed description of the treatment programs that participated in CalTOP and subsequently the PARC surveys.
In addition to psychosocial treatment approaches listed in the NTCS survey, the PARC surveys included Solution-Focused Therapy (SFT). During pilot testing of the PARC surveys, program director and staff respondents indicated that SFT was effective and commonly used for the treatment of substance abuse problems.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aarons GA. Mental health provider attitudes toward adoption of evidence-based practice: the Evidence-Based Practice Attitude Scale (EBPAS) Mental Health Services Research. 2004;6:61–74. doi: 10.1023/b:mhsr.0000024351.12294.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. Journal of the American Medical Association. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Ball S, Bachrach K, DeCarlo J, Farentinos C, Keen M, McSherry T, Polcin D, Snead N, Sockriter R, Wrigley P, Zammarelli L, Carroll K. Characteristics, beliefs, and practices of community clinicians trained to provide manual-guided therapy for substance abusers. Journal of Substance Abuse Treatment. 2002;23:309–318. doi: 10.1016/s0740-5472(02)00281-7. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Hecht JP, Papandonatos GD, Emmons KM, Tatewosian LR, Abrams DB. Smoking-cessation counseling in the home. Attitudes, beliefs, and behaviors of home healthcare nurses. American Journal of Preventive Medicine. 2001;21:272–277. doi: 10.1016/s0749-3797(01)00369-5. [DOI] [PubMed] [Google Scholar]
- Brown BS. From Research to Practice: The Bridge is Out and the Water’s Rising. Advances in Medical Sociology. 2000:345–365. [Google Scholar]
- California Department of Alcohol and Drug Programs. [accessed 2/8/07];Methamphetamine Awareness. 2007 http://www.adp.ca.gov/Meth/meth.shtml.
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Evans E, Hser YI. Pilot-testing a statewide outcome monitoring system: overview of the California Treatment Outcome Project (CALTOP) Journal of Psychoactive Drugs. 2004 Suppl 2:109–114. doi: 10.1080/02791072.2004.10400045. [DOI] [PubMed] [Google Scholar]
- Forman RF, Bovasso G, Woody G. Staff beliefs about addiction treatment. J Journal of Substance Abuse Treatment. 2001;21:1–9. doi: 10.1016/s0740-5472(01)00173-8. [DOI] [PubMed] [Google Scholar]
- Fuller BE, Rieckmann T, McCarty D, Smith KW, Levine H. Adoption of naltrexone to treat alcohol dependence. Journal of Substance Abuse Treatment. 2005;28:273–280. doi: 10.1016/j.jsat.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Greenberg G, Ganshorn K, Danilkewich A. Solution-focused therapy. Counseling model for busy family physicians. Canadian Family Physician. 2001;47:2289–2295. [PMC free article] [PubMed] [Google Scholar]
- Hagen BF, Mitchell DL. Might within the madness: solution-focused therapy and thought-disordered clients. Archives of Psychiatric Nursing. 2001;15:86–93. doi: 10.1053/apnu.2001.22408. [DOI] [PubMed] [Google Scholar]
- Hoge MA, Huey LY, O'Connell MJ. Best practices in behavioral health workforce education and training. Administration and Policy in Mental Health. 2004;32:91–106. doi: 10.1023/b:apih.0000042742.45076.66. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Johnson JA, Roman PM, Oser CB. Rural and urban similarities and differences in private substance abuse treatment centers. Journal of Psychoactive Drugs. 2003;35:511–518. doi: 10.1080/02791072.2003.10400499. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Roman PM. Modeling the use of innovations in private treatment organizations: the role of absorptive capacity. Journal of Substance Abuse Treatment. 2004;26:353–361. doi: 10.1016/s0740-5472(03)00158-2. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Roman PM, Ducharme LJ, Johnson JA. Organizational Predictors of Pharmacological Innovation Adoption: The Case of Disulfram. Journal of Drug Issues. 2005;35:559–574. [Google Scholar]
- Lamb S, Greenlick M, McCarty D. Bridging the Gap Between Practice and Research: Forging Partnerships with Community-Based Drug and Alcohol Treatment. Washington, DC: National Academy Press; 1998. [PubMed] [Google Scholar]
- Lehman WE, Greener JM, Simpson DD. Assessing organizational readiness for change. Journal of Substance Abuse Treatment. 2002;22:197–209. doi: 10.1016/s0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Carroll KM. Evidence-based practices for substance use disorders. Psychiatric Clinics of North America. 2003;26:991–1010. doi: 10.1016/s0193-953x(03)00073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Fox TS, Xie H, Drake RE. A survey of clinical practices and readiness to adopt evidence-based practices: Dissemination research in an addiction treatment system. Journal of Substance Abuse Treatment. 2004;26:305–312. doi: 10.1016/j.jsat.2004.03.003. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Carise D, Kleber HD. Can the national addiction treatment infrastructure support the public's demand for quality care? Journal of Substance Abuse Treatment. 2003;25:117–121. [PubMed] [Google Scholar]
- McLellan AT, Meyers K. Contemporary addiction treatment: a review of systems problems for adults and adolescents. Biological Psychiatry. 2004;56:764–770. doi: 10.1016/j.biopsych.2004.06.018. [DOI] [PubMed] [Google Scholar]
- Miller SD. Description of the Solution-Focused Brief Therapy Approach to Problem Drinking. In: Carroll KM, editor. Approaches to Drug Abuse Counseling. National Institute on Drug Abuse; 2000. [Google Scholar]
- Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben J, Johnson WR. Evidence-based treatment: why, what, where, when, and how? Journal of Substance Abuse Treatment. 2005;29:267–276. doi: 10.1016/j.jsat.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Mulvey KP, Hubbard S, Hayashi S. A national study of the substance abuse treatment workforce. Journal of Substance Abuse Treatment. 2003;24:51–57. doi: 10.1016/s0740-5472(02)00322-7. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. [accessed 2/14/07];Principles of Drug Addiction Treatment. 1999 http://www.drugabuse.gov/PODAT/PODATindex.html.
- Obert JL, Brown AH, Zweben J, Christian D, Delmhorst J, Minsky S, Morrisey P, Vandersloot D, Weiner A. When treatment meets research: clinical perspectives from the CSAT Methamphetamine Treatment Project. Journal of Substance Abuse Treatment. 2005;28:231–237. doi: 10.1016/j.jsat.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Rawson RA, Marinelli-Casey P, Ling W. Dancing with strangers: will U.S. substance abuse practice and research organizations build mutually productive relationships? Addictive Behaviors. 2002;27:941–949. doi: 10.1016/s0306-4603(02)00292-7. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 4th ed. New York: The Free Press; 1995. [Google Scholar]
- Rosenthal RN. Current and future drug therapies for alcohol dependence. Journal of Clinical Psychopharmacology. 2006;26 Suppl 1:S20–S29. [Google Scholar]
- Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB, Katon W, Sullivan G, Means-Christensen A, Bystritsky A. Moving treatment research from clinical trials to the real world. Psychiatric Services. 2003;54:327–332. doi: 10.1176/appi.ps.54.3.327. [DOI] [PubMed] [Google Scholar]
- Simpson DD. A conceptual framework for transferring research to practice. Journal of Substance Abuse Treatment. 2002;22:171–182. doi: 10.1016/s0740-5472(02)00231-3. [DOI] [PubMed] [Google Scholar]
- Sullivan G, Duan N, Mukherjee S, Kirchner J, Perry D, Henderson K. The role of services researchers in facilitating intervention research. Psychiatric Services. 2005;56:537–542. doi: 10.1176/appi.ps.56.5.537. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice. [accessed August 2007];2007 www.usdoj.gov/methawareness.
- Vocci FJ, Acri J, Elkashef A. Medication development for addictive disorders: the state of the science. American Journal of Psychiatry. 2005;162:1432–1440. doi: 10.1176/appi.ajp.162.8.1432. [DOI] [PubMed] [Google Scholar]
- Walters ST, Matson SA, Baer JS, Ziedonis DM. Effectiveness of workshop training for psychosocial addiction treatments: a systematic review. Journal of Substance Abuse Treatment. 2005;29:283–293. doi: 10.1016/j.jsat.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Willenbring ML, Kivlahan D, Kenny M, Grillo M, Hagedorn H, Postier A. Beliefs about evidence-based practices in addiction treatment: a survey of Veterans Administration program leaders. Journal of Substance Abuse Treatment. 2004;26:79–85. doi: 10.1016/S0740-5472(03)00161-2. [DOI] [PubMed] [Google Scholar]


