Abstract
Mucocutaneous candidiasis (MC) is one of the first signs of human immunodeficiency virus (HIV) infection. Over 90% of patients with AIDS will eventually develop oropharyngeal candidiasis (OPC) at some time during their illness, and an additional 10% will develop esophageal candidiasis (EC). Although numerous antifungal agents are available, azoles, both topical (clotrimazole) and systemic (fluconazole, itraconazole), have replaced older topical antifungals (gentian violet and nystatin) in the management of MC in these patients. The systemic azoles, itraconazole and fluconazole, are generally safe and effective agents in HIV-infected patients with MC. A concern in these patients is the clinical relapse, which appears to be dependent on degree of immunosuppression and is more common following clotrimazole and ketoconazole than with fluconazole or itraconazole. Posaconazole is a new extended-spectrum triazole recently approved for the management of OPC. In vitro, posaconazole possesses potent activity against numerous Candida species, including strains that are resistant to fluconazole. Recent clinical trials demonstrate that posaconazole is as efficacious as fluconazole in producing a successful clinical response in HIV-infected patients with OPC/EC. In addition, posaconazole was safe and more effective in sustaining clinical success after treatment was discontinued. Posaconazole appears to be an effective alternative in the management of MC in this difficult- to-treat population.
Keywords: posaconazole, oropharyngeal and esophageal candidiasis, HIV-infected
Introduction
Symptomatic mucosal candidiasis (MC) arises in subjects colonized with Candida who are predisposed by illness, debility, or a local reduction in host resistance to an overgrowth of their own indigenous flora (Odds 1988; Vazquez and Sobel 2003). Colonization rates increase with severity of illness and duration of hospitalization (Johnston et al 1967).
Oral candidiasis has been described since Hippocrates, although Hippocrates used the term “aphthae” to describe this infection (Hippocrates and Adams 1939). Several clinical forms of oral candidiasis exist; thrush is the most commonly and widely recognized and is also called acute pseudomembranous candidiasis. Oropharyngeal candidiasis (OPC) may be the first manifestation of HIV infection and, approximately 80%–90% of patients with AIDS will develop oral candidiasis at some stage (Coker et al 1995; Silverman et al 1996). Although not as frequent as OPC, esophageal candidiasis (EC) is reported in approximately 10% of patients with AIDS, and unlike OPC, is capable of producing incapacitating illness, wasting syndrome, and malnutrition (Dupont et al 1994; Moore and Chaisson 1996). In addition, MC also occurs in individuals with underlying hematological malignancy, following solid organ transplantation, in those with congenital cell-mediated immune dysfunction, and following prolonged antimicrobial therapy (Jensen et al 1964; Johnston et al 1967; Scott and Jenkins 1982).
Even in the era of highly active antiretroviral therapy (HAART), HIV-infected individuals continue to suffer from recurrent OPC/EC (Vazquez and Sobel 2003; Pappas et al 2004). With the advent of HAART fewer HIV-infected patients are developing OPC/EC. In contrast, rate of OPC and EC has not been altered in developing countries where HAART is not readily available. Antiretroviral therapy has not altered the relative frequency of AIDS-defining illnesses, and OPC/EC remains among the most common. Mucocutaneous candidiasis is usually seen in those patients with CD4+ counts less that 100/mm3 (Imam et al 1990; Moore and Chaisson 1996; Vazquez and Sobel 2003). In a population of individuals with median CD4+ counts of 100–110/mm3, the incidence of esophageal candidiasis is approximately 4 per 100 person-years of observation (Moore and Chaisson 1996).
In the non-HIV infected individual, C. albicans accounts for approximately 70%–80% of oral isolates, while C. glabrata and C. tropicalis account for approximately 5%–8% each, and the other non-albicans Candida species are recovered only rarely (Vazquez and Sobel 2003). C. albicans is the species most often implicated in OPC/EC, consistently accounting for 90% or more of baseline isolates (Moore and Chaisson 1996; Wilcox et al 1997; Pappas et al 2004). There has been a significant increase in the frequency of non-albicans Candida species isolation in the HIV-infected individual (Barchiesi et al 1993; van’t Wout 1996). In the 1980s, non-albicans Candida species accounted for 3%–4 % of oral isolates recovered from HIV-infected patients, while in the 1990s, 17% of isolates recovered from HIV patients were non-albicans Candida species (Barchiesi et al 1993; van’t Wout 1996).
Therapy
Prompt therapy with an antifungal agent is indicated (Vazquez and Sobel 2003; Pappas et al 2004). Unfortunately, almost all patients with AIDS and successfully treated MC will eventually develop a recurrence in the absence of immune reconstitution (Reef and Meyer 1995). Therefore, in addition to antifungal therapy, antiretroviral therapy should be instituted as soon as possible.
Although safe and efficacious therapies are available, among the presently available armamentarium, all agents have some limitations. Topical agents may be used for OPC, but are ineffective for EC. Numerous antifungal agents are available for the treatment of OPC (Table 1) and EC (Table 2). However, several factors must be considered when choosing antifungal agents for patients with HIV or AIDS. One important factor is efficacy. In HIV-positive patients, antifungals are less efficacious than in patients with cancer, and time to antifungal response is also more prolonged (Darouiche 1998). In addition, the relapse rate is higher in patients with HIV than in other patient populations (Darouiche 1998; Vazquez 1999). Therefore, certain predisposed HIV-positive patients experience recurrent episodes of OPC and subsequently receive numerous courses of antifungals during their lifetime. As AIDS progresses, they frequently experience shorter intervals between episodes of OPC and esophageal candidiasis and thus more antifungal exposure, which may lead to antifungal resistance and severe morbidity (Vazquez and Sobel 1997).
Table 1.
Antifungals for the treatment of oropharyngeal candidiasis
| Antifungal agent | Form | Strength | Use |
|---|---|---|---|
| Topical | |||
| Nystatin | Pastille | 200,000 units | Dissolve 1-2 pastilles qid |
| Nystatin | Suspension | 100,000 units | 5 mL swish and swallow qid |
| Clotrimazole | Oral troche | 10 mg | Dissolve 1 troche 5 times/day |
| Amphotericin B | Suspension | 1 mg/mL | 1 mL swish and swallow qid |
| Amphotericin B | Lozenge | 100 mg | qid |
| Amphotericin B | Tablet | 10 mg | qid |
| Systemic | |||
| Ketoconazole | Tablet | 200 mg | 1-2 tablets qd-bid |
| Fluconazole | Tablet | 100 mg | 1 tablet qd |
| Fluconazole | Solution | 10 mg/mL | 10 ml qd |
| Itraconazole | Capsule | 100 mg | 200 mg qd |
| Itraconazole | Solution | 10 mg/mL | 10-20 ml qd-bid |
| Posaconazole | Suspension | 100 mg/2.5 mL | 100 mg qd |
Derived from data of Vazquez and Sobel (2003)
Notes: qid, four times daily; tid, three times daily; bid, twice daily; qd, once daily
Table 2.
Antifungals for the treatment of esophageal candidiasis
| Antifungal Agent | Form | Strength | Use |
|---|---|---|---|
| Ketoconazole | Tablet | 200 mg | 1–2 tablets qd-bid |
| Fluconazole | Tablet | 100 mg | 1 tablet qd |
| Fluconazole | Solution | 10 mg/ml | 10ml qd |
| Itraconazole | Capsule | 100 mg | 200 mg qd |
| Itraconazole | Solution | 10 mg/ml | 10–20 mL qd-bid |
| Voriconazole | tablet | 200 mg | 1 tablet bid |
Derived from data of Vazquez and Sobel (2003)
Notes: bid, twice daily; qd, once daily
Another possibly more important factor to consider when managing recurrent fungal infections in HIV-positive patients is the long-term consequences of antifungal therapy on mycoflora. It is important to note that, as with many infections in this patient population, antifungal treatment merely reduces the signs and symptoms of infection, and thus produces a transient clinical response by lowering the quantity of organisms in the affected area. It is difficult to eradicate yeast from the body of a patient infected with HIV (Vazquez and Sobel 1997; Vazquez and Sobel 2003). Subsequently, this leads to numerous courses of antifungals, development of antifungal resistance, and frequently, antifungal cross-resistance (Maenza et al 1997). This is reflected by the clinical ineffectiveness of antifungals to which a patient has not previously been exposed. Thus we are becoming increasingly aware that choosing the appropriate agent, even in the early stages of disease, is extremely important because of the future repercussions of this selection in the advanced stages of disease.
Presently available therapy which includes topical agents such as nystatin, amphotericin B, and clotrimazole are all somewhat effective, but tolerance and compliance are frequently problematic (Kozinin et al 1957; Quintiliani et al 1994; Vazquez 1999). In addition, topical agents are ineffective in EC, thus mandating systemic antifungal therapy (Vazquez 1999).
Nystatin is the time-honored treatment for oral thrush in otherwise healthy adults and infants. Its limitations include bitter taste, gastrointestinal (GI) side-effects, and a 4 times a day regimen, all of which eventually lead to reduced adherence and lower efficacy (Pons et al 1997; Vazquez 1999). More importantly, is its lack of efficacy in severely immunocompromised patients, such as those with HIV/AIDS (Quintiliani et al 1994; Pons et al 1997). In a published study comparing the efficacy of nystatin and oral fluconazole in HIV-positive patients, the clinical cure rate of nystatin was 52%, compared with 87% for fluconazole (Pons et al 1997). The mycological cure rate was also significantly lower for nystatin (6% vs 60%). In addition, the relapse rates 28 days after the end of therapy were 44% and 18%, respectively.
Amphotericin B oral suspension is also an alternative antifungal agent (Kozinin et al 1957; Vazquez 1999). In addition to the suspension, amphotericin B is also available as a lozenge and tablet. Like nystatin, it is not absorbed from the GI tract and must to be given 4 times daily; however, it does not have an unpleasant taste. Unfortunately, comparative studies evaluating amphotericin B oral solution and other antifungals are limited.
Azole antifungals have essentially replaced the topical polyene agents for the treatment of OPC in AIDS (Como and Dismukes 1994). Clotrimazole 10 mg troches administered 5 times/day were successful in treating mild-to-moderate OPC during the early stages of HIV disease and during the initial episodes of oral candidiasis in patients with neoplastic diseases (Schectman et al 1984). In a study comparing oral fluconazole and clotrimazole troches for oral candidiasis in persons with HIV or AIDS, efficacy was essentially the same, 98% and 94%, respectively (Pons et al 1993). At the end of antifungal therapy, fluconazole was more effective than clotrimazole in eradicating detectable yeast from the oral flora (65% vs 48%, respectively). In addition, patients receiving fluconazole were also more likely to remain asymptomatic through the second week of follow-up (82%) when compared with those receiving clotrimazole (50%).
Although topical therapy is frequently effective and relatively inexpensive, recurrent episodes of OPC in more advanced disease often require systemic azoles such as ketoconazole, fluconazole, itraconazole, and now posaconazole. Ketoconazole was the first available oral systemic imidazole antifungal agent and is highly effective even in debilitated patients (Como and Dismukes 1994). Clinical cure rates in excess of 75% have been achieved with daily ketoconazole administered for 10–14 days (Hughes et al 1993). In several comparative trials in patients with AIDS, ketoconazole was not as efficacious as fluconazole (70%–80% vs 94%–100%), and the mycological cure rates were also lower (DeWit et al 1989; Como and Dismukes 2003). Use of ketoconazole is limited by fears of hepatotoxicity and drug-drug interactions, and concerns about the reliability of gastric absorption and subsequent blood and tissue levels (Como and Dismukes 1994; Vazquez 1999). The drug’s absorption is markedly reduced under hypochlorhydric states. Thus, systemic absorption is a concern in patients with AIDS-related hypochlorhydria, and in those receiving H2-receptor antagonists (cimetidine, ranitidine,), sucralfate, antacids, didanosine, and proton pump inhibitors (omeprazole, lansoprazole) (Piscitelli et al 1996). In addition, since ketoconazole is a potent inhibitor of the cytochrome (CYP) P450 3A4 enzyme system, numerous reports describe interactions with the non-sedating H1-receptor antagonists (terfenadine, astemizole) and cisapride resulting in significant prolongation of the QT interval and occasional deaths due to cardiac dysrhythmias (Honig et al 1993; Meyer and Rodvold 1996). Thus, concomitant administration of ketoconazole with drugs metabolized via the same pathway (cyclosporine, digoxin, HIV-protease inhibitors, and several sedatives such as triazolam and midazolam) may produce increased levels of the second drug (Meyer and Rodvold 1996).
The older triazoles, fluconazole and itraconazole, have demonstrated excellent efficacy and safety profiles for many years, and have become the most frequently prescribed antifungals, especially for patients with HIV or AIDS (Hay 1990; Meunier et al 1990; Murray et al 1997). The clinical efficacy of fluconazole 50–100 mg/day was evaluated in several open-label and placebo-controlled trials and in double-blind comparative studies versus clotrimazole or ketoconazole in patients with either hematologic or solid organ malignancy or HIV infection (Hay 1990; Koletar et al 1990; Meunier et al 1990). Although most studies utilized a 100 mg daily dose, clinical efficacy has been achieved with a dose of 50 mg/day (Hay 1990). Clinical response was achieved in 80% of patients with severe underlying disease with the low dose of fluconazole. However, complete mycological cure is more difficult to attain. A striking feature of fluconazole is the rapidity of response, usually within 10 days with fluconazole 50 mg/day and within 5 days with 100–200 mg/day, even in the most severe forms of thrush associated with AIDS (Hay 1990; Darouiche 1998). In addition, overall clinical response rates indicate that failure is rare, and in most published studies, 80% or more of patients were clinically cured, with another 10%–15% experiencing considerable improvement (Vazquez 1999).
Itraconazole has a broad spectrum of activity, and like other azoles, it inhibits the synthesis of fungal ergosterol. Since the capsule formulation has variable absorption, a cyclodextrin solution formulation has been developed and is generally the formulation utilized in OPC/EC (Barone et al 1998). In a pharmacokinetic study, the solution demonstrated a 30% increase in itraconazole absorption. In addition, the solution has a much greater bioavailability in fasting patients compared with post-prandial administration (Hostetler et al 1992; Van de Velde et al 1996). A prospective, randomized trial in HIV-positive and AIDS patients with OPC, compared itraconazole oral solution 200 mg/day and fluconazole 100/mg day for 14 days (Graybill et al 1998). Clinical response rates were 97% for itraconazole and 87% for fluconazole, with few adverse events in both groups. However, approximately 50% of the patients in both groups experienced relapses at the 1-month follow-up evaluation.
Overall, itraconazole and fluconazole, have demonstrated an improved safety profile compared with other antimycotic agents; nevertheless, they must be used with caution. Itraconazole has similar drug interactions as ketoconazole due to the inhibition of the same CYP3A4 enzyme system (Hostetler et al 1992; Meyer and Rodvold 1996). Fluconazole is associated with fewer drug-drug interactions because it has less affinity for the enzyme (Kowalsky and Dixon 1991; Meyer and Rodvold 1996). The pharmacological interactions with fluconazole include phenytoin, rifampin, rifabutin, cyclosporin A, and possibly some of the protease inhibitors (Kowalsky and Dixon 1991; Tucker et al 1992; Meyer and Rodvold 1996). In certain situations, fluconazole may offer an advantage over ketoconazole or itraconazole because of the lower potential to produce drug-drug interactions.
The optimal antifungal agent for OPC is not known, but evaluation of the most recent literature seems to suggest that until now fluconazole and itraconazole appear to be the most appropriate agents in patients with HIV infection or AIDS.
Since topical agents are ineffective in the management of EC, relatively few oral drugs for systemic infection are available (Vazquez and Sobel 2003; Pappas et al 2004). The current guidelines of the Infectious Diseases Society of America recommend the use of systemic antifungal therapy (Pappas et al 2004). Currently available therapy includes oral and parenteral azoles (ketoconazole, fluconazole, itraconazole, and voriconazole) or parenteral polyenes (amphotericin B). More recently, the echinocandins (caspofungin [Cancidas®, Merck & Co., Inc.]; micafungin [Mycamine®, Astellas Pharma US, Inc.]; and anidulafungin [Eraxis®, Pfizer Inc.]) have all been approved for the treatment of EC.
Amphotericin B, the agent of choice for many years is no longer acceptable as first line therapy in most situations due to unacceptable nephrotoxicity and infusion-related reactions.
Voriconazole (Vfend®, Pfizer Inc.) is a newer triazole that has been shown to be 10- to 500-fold more potent in vitro than fluconazole against a wide spectrum of fungi, including fluconazole resistant Candida species (Como and Dismukes 2003; Pfizer 2005). Voriconazole 200 mg bid was approved for the treatment of EC in November 2004. In a randomized, double-dummy, double-blind, multicenter trial voriconazole 200 mg bid was compared with fluconazole 200 mg daily in esophageal candidiasis (Ally et al 2001). Overall success rates were comparable 98.2% for voriconazole compared with 95% for fluconazole. The overall safety and tolerability of both agents was similar.
The echinocandins are a relatively new class of antifungal, with a completely different mechanisms of action (Groll and Walsh 2003). All three are broad-spectrum and demonstrate excellent in vitro activity against most Candida species, including those species that are fluconazole-resistant (Groll and Walsh 2003). All three echinocandins have been approved for the treatment of EC. Thus far, 5 different clinical trials evaluating echinocandins in EC have been completed. The clinical studies compare the echinocandins to either fluconazole or amphotericin B (Groll and Walsh 2003). Overall, all three echinocandins demonstrated non-inferiority to the comparator in each of the five clinical trials. In addition, the overall safety profile was excellent for the three echinocandins. The two major concerns with the echinocandins in the management of EC are that there are no oral formulations thus mandating the use of parenteral therapy for a minimum of 2–3 weeks, or a switch to an oral azole, and the relapse rates of EC using the echinocandins appears to be slightly higher than the comparators (fluconazole or amphotericin B). Nevertheless, clinical relapse is not uncommon, particularly in patients with persistence of underlying immunodeficiency (eg, AIDS, chronic mucocutaneous candidiasis). Relapse appears to depend on duration of therapy and degree of immunosuppression, and may occur sooner following clotrimazole and ketoconazole therapy than after itraconazole or fluconazole therapy (DeWit et al 1989; Vazquez and Sobel 1999).
The clinical impact of antifungal resistance in patient with AIDS has been demonstrated in patients who fail standard antifungal therapy for OPC (Vazquez and Sobel 1997). After the onset of fluconazole-resistant thrush, patients had a median survival of 184 days. Moreover, after the onset of clinical resistance to amphotericin B, the patients had an astonishing 83-day median survival rate. Although mucosal candidiasis does not produce death directly, clinical failure is probably a co-morbidity factor in the rapid demise of these patients. Clinical failure is also a marker of severe immunosuppression and a nonfunctional immune system.
It is still not clear whether the total dose of antifungals, the duration of therapy, type of antifungal, or pattern of drug administration (continuous or episodic) are the most important determinants in the development of antifungal-refractory fungal disease (Maenza et al 1996). More than likely it is multifactorial, involving a combination of advanced immunosuppression, high fungal burdens, and prolonged exposure to antifungals (McCarthy et al 1991).
In addition to microbial resistance, reasons for recurrence of OPC or refractory disease include patient non-compliance, the degree of immunosuppression, drug interactions, and altered drug bioavailability (Maenza et al 1996). These limitations underscore the need for new agents that may provide advantages such as safer delivery, fewer drug-drug interactions, and an improved antifungal spectrum.
Posanconazole (Noxafil®, Schering-Plough) is a potent, oral extended-spectrum triazole antifungal recently approved by the FDA (Herbrecht 2004) (Figure 1). It is approved for the treatment of OPC, including OPC refractory to itraconazole and/or fluconazole and for the prophylaxis of infections due to Candida and Aspergillus spp. in patients who are at high risk for such infections, such as those undergoing hematopoietic stem cell transplant (HSCT) with graft-versus host disease or with prolonged neutropenia due to a hematologic malignancy or its treatment (Schering Corp 2006).
Figure 1.
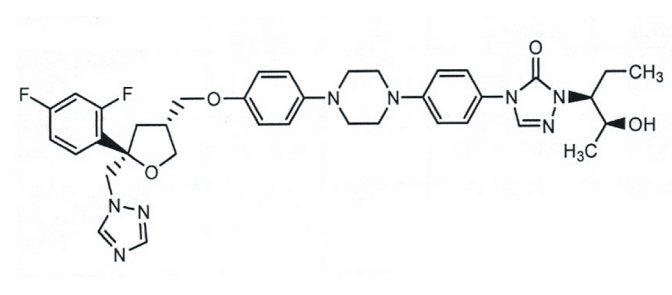
Structure of posaconazole.
Posaconazole, like other azole antifungals, inhibits lanosterol 14-alpha demethylase (CYP51), an enzyme that catalyzes the final step in the synthesis of ergosterol, an important component of the fungal cell membrane (Munayyer et al 2004). Mutations near the heme cofactor of CYP51 appear to reduce the binding affinity of compact azoles such as fluconazole and voriconazole and may lead to azole resistance in C. albicans (Li et al 2004). However, results of a study using 3-dimensional binding models suggest that the long side chain of posaconazole may result in tighter binding affinity and appears to stabilize binding. It appears that mutations in the heme site have far less impact on the susceptibility of the organisms to posaconazole, compared with fluconazole or voriconazole. Thus a greater number of mutations may be required to generate resistance to posaconazole than to fluconazole or voriconazole (Chau et al 2004; Li et al 2004; Xiao et al 2004). In addition, posaconazole is a substrate of the major facilitator pumps encoded by CDR1 and CDR2 in C. albicans, but is not a substrate of the major facilitator pumps encoded by MDR1 and FLU1 that efflux fluconazole (Heimark et al 2002). Posaconazole may be less susceptible than some azoles to the development of secondary azole resistance. In essence, although fluconazole and even voriconazole may demonstrate resistance to fluconazole, the majority of the time posaconazole will retain its in vitro susceptibility (Chau et al 2004; Li et al 2004; Xiao et al 2004).
In vitro activity
Posaconazole has demonstrated in vitro activity against Aspergillus, Fusarium and the Zygomycetes. Its activity in vitro against Candida spp. is similar to that of voriconazole, and includes itraconazole- and fluconazole-resistant strains of Candida, such as C. glabrata, and C. krusei (Sabatelli et al 2006). In vitro assays demonstrate posaconazole MIC90 values for C. albicans, C. parapsilosis,C. tropicalis, C.lusitaniae, and C. dubliniensis of 0.06–0.5 μg/mL, while MIC90 values for C. krusei and C. glabrata range from 0.5 to 4 μg/mL (Ostrosky-Zeichner et al 2003; Herbrecht 2004) (Table 3).
Table 3.
In vitro susceptibilities of Candida spp. to posaconazole, fluconazole, and itraconazole
| Posaconazole | Fluconazole | Itraconazole | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Organism | Range | 50% | 90% | Range | 50% | 90% | Range | 50% | 90% |
| C. albicans | ≤0.004-16 | 0.003 | 0.06 | 0.12– >64 | 0.25 | 0.5 | <0.004–16 | 0.003 | 0.12 |
| C. glabrata | 0.3– >4 | 0.5 | 2.0 | 0.25– >64 | 16 | >64 | 0.03– >4 | 1 | 8 |
| C. parapsilosis | 0.03–0.12 | 0.12 | 0.12 | 0.12–2.0 | 0.5 | 1 | 0.015–0.25 | 0.12 | 0.12 |
| C. tropicalis | 0.03– > 4 | 0.12 | 0.12 | 0.12– >64 | 0.5 | 2.0 | 0.015– >4 | 0.12 | 0.5 |
| C. krusei | 0.03–0.5 | 0.5 | 0.5 | 8– >64 | 32 | >64 | 0.12–2 | 0.5 | 0.5 |
| C. dublinieusis | 0.015–0.25 | 0.30 | 0.06 | 0.12– >64 | 0.12 | 0.5 | 0.015–0.5 | 0.06 | 0.25 |
| C. lusitaniae | 0.015–0.12 | 0.12 | 0.12 | 0.12–8 | 1 | 2 | 0.03–0.5 | 0.12 | 0.5 |
Pharmacokinetics (Table 4)
Table 4.
Pharmacokinetics of posaconazole
| Variable | Value |
|---|---|
| Volume of distribution (L) | 1774 |
| Protein binding (%) | >98 |
| Elimination | Via feces (77%) |
| Via urine (1%) | |
| Half-life (hours) | 35 (20–66) |
| Metabolism | Biotranformation via UDG pathway |
Derived from data of Herbrecht (2004).
Abbreviations: UDG, uridine diphosphate – glucoronosyltransferase
Absorption and distribution
Posaconazole is orally absorbed, with the greatest exposure achieved when it is administered as an oral suspension (Courtney et al 2003a). Following administration of rising single or multiple doses (tablet formulation) to healthy subjects, posaconazole exhibits dose-proportional pharmacokinetics up to 800 mg/day (Courtney et al 2003b). No increase in area under the plasma concentration-time curve (AUC) values is observed when the posaconazole dose is increased from 800 to 1200 mg/day. Following administration of the tablet or suspension formulations, posaconazole has an extensive volume of distribution (343–1341 L) and a long half-life (t½ approximately 25–35 h) (Courtney et al 2003a, b, c), with peak plasma concentrations attained at approximately 5–6 hours after dose. Steady state concentrations are attained at 7–10 days.
Posaconazole exposure is enhanced by co-administration with food. In a randomized, single-dose, open-label study conducted in 20 healthy male volunteers, administration of posaconazole with non-fat meal and a high-fat meal increased the AUC(0–72) 2.6- and 4-fold, respectively (p < 0.001 vs administration under fasting conditions) (Courtney et al 2004). Similarly, administration of posaconazole with a nutritional supplement (Boost® Plus; MeadJohnson® Nutritionals, Evansville, Indiana, USA) increased maximum plasma concentrations (Cmax) and AUC(0–72) 3.4- and 2.6-fold, respectively (Courtney et al 2003c).
When food intake is limited because of mucositis or other gastrointestinal dysfunction, dividing the daily dose enhances posaconazole’s bioavailability. In a study of healthy male volunteers (n = 18) given posaconazole 800 mg/day under fasted conditions, 200 mg qid and 400 mg bid dosing was associated with increases in Cmax and time to maximum plasma concentrations (tmax) compared with once-daily dosing (Ezzet et al 2006). Administration in split doses also improved estimated AUC, which doubled and tripled with twice-daily and qid dosing, respectively.
Metabolism/elimination
Posaconazole is primarily metabolized in the liver, where it undergoes glucuronidation and transformation into other biologically inactive metabolites (Krieter et al 2002). Approximately, 14% of an administered dose is excreted as multiple glucuronidated derivatives in the urine; an additional 77% is eliminated as parent compound in the feces. Minor amounts are excreted as parent compound in the urine.
Unlike itraconazole and voriconazole, posaconazole is not primarily metabolized by fungal cytochrome P450 enzymes (CYP450) (Wexler et al 2004). Thus, co-administering drugs that interact with the CYP450 enzyme system may alter itraconazole and voriconazole plasma concentrations, but is unlikely to alter posaconazole plasma concentrations. An evaluation of the effects of posaconazole on the various CYP450 enzymes demonstrated an inhibitory effect on CYP3A4 activity, but no influence on the activity of the other isoenzymes (CYP1A2, CYP2C8/9, CYP2D6 or CYP2E1) (Wexler et al 2004). In contrast to other azoles that are known to inhibit a variety of CYP450 drug-metabolizing isoenzymes (Albengres et al 1998; Vazquez 1999; Venkatakrishnan et al 2000), posaconazole is unique in that its effects on CYP450 enzyme activity are relatively limited. Therefore, posaconazole has the potential for fewer drug interactions compared with other azoles.
Special populations
Posaconazole pharmacokinetics are not significantly influenced by age, gender, or ethnicity (Courtney et al 2000a, d, e). Therefore, no dose adjustments are necessary to accommodate for differences in these patient factors. Furthermore, renal or hepatic impairment has no significant influence on the pharmacokinetics of posaconazole (Courtney et al 2000b; Courtney et al 2003f).
Clinical trials
A multicenter, randomized, evaluator-blinded study compared the efficacy of posaconazole 100 mg daily to fluconazole 100 mg daily for the treatment of OPC in patients infected with HIV (Vazquez et al 2006). The primary end point was defined as clinical success on day 14. Three-hundred fifty subjects were enrolled into the study, 178 received posaconazole and 172 received fluconazole. Clinical success occurred in 91.7% of patients treated with posaconazole and 92.5% of those treated with fluconazole, with a mycological success of 68% in both arms. On follow up day 42, mycological success remained greater in the posaconazole group (40.6% vs 26.4%; p = 0.038) and fewer patients in this group had experienced clinical relapses (31.5% vs 38.2%). Although it did not meet statistical superiority, it appears that posaconazole was somewhat more effective than fluconazole in preventing a clinical relapse 6 weeks after the conclusion of antifungal therapy. In general, adverse events were uncommon and were similar in both groups.
In a separate clinical trial, oral posaconazole was evaluated in the management of OPC/EC that was clinically refractory to either fluconazole or itraconazole (Skiest et al 2006). In this study, oral posaconazole was used in subjects with confirmed OPC or EC who failed to improve on conventional courses of either fluconazole at 100 mg daily or itraconazole 200 mg daily for a minimum of 10 days. Study subjects received either posaconazole 400 mg bid for 3 days, followed by 400 mg daily for 25 days or posaconazole 400 mg bid for 28 days. The primary end point was either cure or improvement after 28 days of therapy. In the modified intent-to-treat population (MITT), 75% (132/176) of treated subjects achieved a clinical response to posaconazole. Clinical response was similar in both dosing regimens (75.3% vs 74.7%). In addition, in the 43 patients who also had endoscopically proven EC, the clinical response rate was documented to be 74.4%.
Although in this study, patients were on study drug for a prolonged period of time (28 days), the overall incidence of adverse events associated with the study drug was low. The most commonly observed adverse events included diarrhea (11%), neutropenia (7%), flatulence (6%), and nausea (6%). Only 8 patients discontinued posaconazole because of treatment-related adverse events. The study concluded that posaconazole is a safe and effective treatment option for patients with HIV infection suffering from azole-refractory OPC/EC.
To further evaluate the safety and efficacy of long-term posaconazole in patients with azole-refractory OPC/EC, a non-comparative open-label study was performed (Vazquez et al 2007). Subjects who responded to the above mentioned trial, were eligible for a long term suppressive study. During the study period all patients received posaconazole 400 mg twice daily for up to 3 months. If patients were stable and clinically cured at three months, they were continued on therapy for up to 12 months. After the 12-month treatment course, 85.6% of subjects continued to remain symptom free. Posaconazole was well tolerated, with minimal adverse events. Overall, this study established that posaconazole at 400 mg twice daily demonstrated long-term safety, tolerability, and efficacy, thus offering a safe and long-term suppressive treatment option for HIV-infected subjects suffering from azole-refractory mucosal candidiasis.
Safety
Posaconazole has been relatively well tolerated in all clinical trials thus far. The most common adverse effects have been nausea and headache. Rash, dry skin, dizziness, paresthesias, and flushing have been described.
The most common adverse events reported in posaconazole clinical studies are of gastrointestinal in origin (eg, nausea, vomiting, dyspepsia, taste disturbance, diarrhea, and abdominal pain), as would be expected with a triazole (Herbrecht 2004; Skiest et al 2006; Vazquez et al 2006). Elevated liver enzyme levels are rarely reported, and most are mild to moderate in severity and are similar to those observed in placebo-treated subjects (Courtney et al 2003b; Skiest et al 2006). In healthy volunteers who received single or multiple posaconazole doses up to 1200 mg/day, no QT interval prolongation or other clinically relevant changes in electrocardiogram results have been observed (Courtney et al 2003b). Long-term administration of posaconazole does not appear to be associated with a different adverse event profile than short-term administration (Raad et al 2006; Skiest et al 2006; van Burik et al 2006; Vazquez et al 2007). Discontinuations because of adverse events were described in only two study reports. One report indicated that 22 of 98 patients with febrile neutropenia or refractory invasive fungal infections discontinued posaconazole therapy prematurely because of adverse events; however, most of these events were not related to posaconazole therapy (Ullmann et al 2006). The other report described one premature discontinuation because of nausea, vomiting and diarrhea, which were attributed to infection with Cryptosporidium and acid-fast bacteria, not posaconazole therapy (Pitisuttithum et al 2003).
Based on this limited number of subjects with severe underlying diseases, it appears that the adverse event profile is similar to that of fluconazole, with the most common events gastrointestinal in origin and with low incidence of hepatic or renal toxicity or rash. Additionally, visual adverse events such as those seen with voriconazole have not been reported (Pfizer 2003).
Drug interactions
Posaconazole is only an inhibitor of CYP3A4, thus it may potentate the effect and toxicity of drugs metabolized by this enzyme, including phenytoin, midazolam, rifabutin, cyclosporine, and tacrolimus; if given with posaconazole, cyclosporine doses should be reduced by one-quarter and tacrolimus doses by two-thirds, and serum levels of each should be monitored. Concurrent use of posaconazole with ergot alkaloids, pimozide, cisapride, halofantrine, astemizole, and quinidine is contraindicated (Wexler et al 2004).
Dosage
The recommended dose of posaconazole for OPC is a loading dose of 100 mg (2.5 mL) by mouth twice a day for the first day, followed by 100 mg daily for 13 days. For refractory OPC, the recommended dosage is 400 mg (10 mL) twice daily based on the severity of illness. Most patients receive 21–28 days of antifungal therapy. Posaconazole should be administered along with a full meal or with a liquid nutritional supplement. According to the manufacturer, if a full meal or supplement cannot be taken, alternative antifungal agents should be considered.
Conclusions
Numerous advances in antifungal therapy have been made in the last decade. The impressive results and minimal toxicity of azole compounds continue to make them attractive in the management of fungal infections in patients with AIDS. However, difficulties in managing these infections should remind us that we cannot rely on antifungals alone. We must continue to find ways to improve the body’s dysfunctional immune system. In addition, we must continue to develop more effective antifungal agents with different mechanisms of action and different modes of administration.
Clinical trials demonstrate that posaconazole is as effective as fluconazole in producing a successful outcome in HIV-infected patients with OPC. In addition, posaconazole was more effective than fluconazole in sustaining clinical success after completing antifungal therapy. Furthermore, in a separate long-term clinical trial, posaconazole also demonstrated to be effective in HIV-infected patients suffering from azole-refractory OPC/EC. In the several clinical trials conducted thus far, posaconazole has been established as an extremely safe and very tolerable antifungal agent, similar to either fluconazole or itraconazole.
Overall, posaconazole’s extended spectrum of activity, tolerability, long-term efficacy, safety profile and ease of use verify that it is an important addition to the antifungal armamentarium used to manage OPC and EC in any population. Posaconazole has also proven to be especially effective in the difficult to treat HIV-infected population suffering from azole refractory MC.
References
- Albengres E, Le Louet H, Tillement JP. Systemic antifungal agents: drug interactions of clinical significance. Drug Saf. 1998;18:83–97. doi: 10.2165/00002018-199818020-00001. [DOI] [PubMed] [Google Scholar]
- Ally R, Schurmann D, Kreisel W, et al. A randomized double-blind, double-dummy, multicenter trial of voriconazole and fluconazole in the treatment of esophageal candidiasis in immunocompromised patients. Clin Infect Dis. 2001;33:1447–54. doi: 10.1086/322653. [DOI] [PubMed] [Google Scholar]
- Barchiesi F, Morbiducci V, Ancarani F, et al. Emergence of oropharyngeal candidiasis caused by non-albicans species of Candida in HIV-infected patients. Eur J Epidemiol. 1993;9:455–56. doi: 10.1007/BF00157408. [DOI] [PubMed] [Google Scholar]
- Barone JA, Moskovitz BL, Guarnieri J, et al. Enhanced bioavailability of itraconazole in hydroxypropyl-β-cyclodextrin solution compared with capsules in healthy volunteers. Antimicrob Agents Chemother. 1998;42:1862–65. doi: 10.1128/aac.42.7.1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau AS, Mendrick CA, Sabatelli FJ, et al. Application of real-time quantitive PCR to molecular analysis of Candida albicans strains exhibiting reduced susceptibility to azoles. Antimicrob Agents Chemother. 2004;48:2124–31. doi: 10.1128/AAC.48.6.2124-2131.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker RJ, Fisher M, Tomlinson DR. Management of mycoses associated with HIV disease. Int J STD AIDS. 1995;6:408–12. doi: 10.1177/095646249500600605. [DOI] [PubMed] [Google Scholar]
- Como JA, Dismukes WE. Oral azole drugs as systemic antifungal therapy. N Eng J Med. 1994;330:263–72. doi: 10.1056/NEJM199401273300407. [DOI] [PubMed] [Google Scholar]
- Como J, Dismukes WE. Azole antifungal drugs. In: Dismukes WE, Pappas PG, Sobel JD, editors. Clinical Mycology. 1. New York, NY: Oxford University Press; 2003. pp. 64–87. [Google Scholar]
- Courtney R, Laughlin M, Gontz H, et al. Single-dose pharmacokinetics of posaconazole in subjects with various degrees of chronic liver disease. Annual Meeting of American Association of Pharmaceutical Scientists; October 29-November 2; Indianapolis, IN. 2000b. [Google Scholar]
- Courtney R, Martinho M, Lim J, et al. Evaluation of the effect of age, weights, race, and gender on posaconazole plasma concentrations in HIV-infected patients. 3rd European Congress of Clinical Microbiology and Infectious Diseases; May 10–13; Glasgow, Scotland: 2000a. [Google Scholar]
- Courtney R, Pai S, Laughlin M, et al. Pharmacokinetics, safety, and tolerability of oral posaconazole administered in single and multiple doses in healthy adults. Antimicrob Agents Chemother. 2003b;47:2788–95. doi: 10.1128/AAC.47.9.2788-2795.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney R, Sansone A, Calzetta A, et al. The effect of a nutritional supplement (Boost Plus) on the oral bioavailability of posaconazole. 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy; September 14–17; Chicago, IL. 2003c. [Google Scholar]
- Courtney R, Sansone A, Kantesaria B, et al. Effect of ethnicity on the pharmacokinetics of posaconazole in healthy volunteers. 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy; September 14–17, 2003; Chicago, IL. 2003d. [Google Scholar]
- Courtney R, Sansone A, Radwanski E, et al. Relative oral bioavailability of three formulations of posaconazole in healthy volunteers: basis for clinical development of the suspension. 13th European Congress of Clinical Microbiology and Infectious Diseases; May 10–13; Glasgow, Scotland. 2003a. [Google Scholar]
- Courtney R, Sansone A, Statkevich P, et al. Effect of age and gender on the pharmacokinetics of posaconazole in healthy volunteers. 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy; September 14–17; Chicago, IL. 2003e. [Google Scholar]
- Courtney R, Sansone A, Statkavich P, et al. Pharmacokinetics of posaconazole in subjects with varying degrees of renal insufficiency. 13th European Congress of Clinical Microbiology and Infectious Diseases; May 10–13; Glasgow, Scotland. 2003f. [Google Scholar]
- Courtney R, Wexler D, Radwanski E, et al. Effect of food on the relative bioavailability of two oral formulations of posaconazole in healthy adults. Br J Clin Pharmacol. 2004;57:218–22. doi: 10.1046/j.1365-2125.2003.01977.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darouiche RO. Oropharyngeal and esophageal candidiasis in immunocompromised patients: treatment issues. Clin Infect Dis. 1998;26:259–74. doi: 10.1086/516315. [DOI] [PubMed] [Google Scholar]
- DeWit S, Weerts D, Goossens H, et al. Comparison of fluconazole and ketoconazole for oropharyngeal candidiasis in AIDS. Lancet. 1989;1:746–8. doi: 10.1016/s0140-6736(89)92572-5. [DOI] [PubMed] [Google Scholar]
- Dupont B, Denning DW, Marriot D, et al. Mycosis in AIDS. J Med Vet Mycology. 1994;32(Suppl):65–77. doi: 10.1080/02681219480000731. [DOI] [PubMed] [Google Scholar]
- Ezzet F, Wexler D, Courtney R, et al. The oral bioavailability of posaconazole in fasted healthy subjects: basis for clinical dosage recommendations. Clin Pharmacokinet. 2007 doi: 10.2165/00003088-200544020-00006. In press. [DOI] [PubMed] [Google Scholar]
- Graybill JR, Vazquez J, Darouiche RO, et al. Itraconazole oral solution: a novel and effective treatment for oropharyngeal candidiasis in HIV/AIDS patients. Am J Med. 1998;104:33–9. doi: 10.1016/s0002-9343(97)00307-0. [DOI] [PubMed] [Google Scholar]
- Groll AH, Walsh TG. Cell wall synthesis inhibitors: echinocandins and nikkomycins. In: Dismukes WE, Pappas PG, Sobel JD, editors. Clinical Mycology. 1. New York, NY: Oxford University Press; 2003. pp. 88–103. [Google Scholar]
- Hay RJ. Overview of studies of fluconazole in oropharyngeal candidiasis. Rev Infect Dis. 1990;12(Suppl 3):S334–7. doi: 10.1093/clinids/12.supplement_3.s334. [DOI] [PubMed] [Google Scholar]
- Heimark L, Shipkova P, Greene J, et al. Mechanism of azole antifungal activity as determined by liquid chromatographic/mass spectrometric monitoring of ergosterol biosynthesis. J Mass Specgrom. 2002;37:265–9. doi: 10.1002/jms.280. [DOI] [PubMed] [Google Scholar]
- Herbrecht R. Posaconazole: a potent extended spectrum triazole antifungal for the treatment of serious fungal infections. Int J Clin Pract. 2004;58:612–24. doi: 10.1111/j.1368-5031.2004.00167.x. [DOI] [PubMed] [Google Scholar]
- Hippocrates CA, Adams F. Epidemics, Book 3. Baltimore: Williams and Wilkins; 1939. [Google Scholar]
- Honig PK, Wortham DC, Zamani K, et al. Terfenadine-ketoconazole interaction. Pharmacokinetic and electrocardiographic consequences. JAMA. 1993;269:1513–8. [PubMed] [Google Scholar]
- Hostetler JS, Hanson LH, Stevens DA. Effect of cyclodextrin on the pharmacology of antifungal oral azoles. Antimicrob Agents Chemother. 1992;36:477–80. doi: 10.1128/aac.36.2.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes WT, Bartley DL, Patterson GG, et al. Ketoconazole and candidiasis: a controlled study. J Infect Dis. 1983;147:1060–3. doi: 10.1093/infdis/147.6.1060. [DOI] [PubMed] [Google Scholar]
- Imam N, Carpenter CC, Mayer KH, Fisher A, Stein M, Danforth SB. Hierarchical pattern of mucosal candida infections in HIV-seropositive women. Am J Med. 1990;89:142–6. doi: 10.1016/0002-9343(90)90291-k. [DOI] [PubMed] [Google Scholar]
- Jensen KB, Stenderup A, Thomsen JB. Esophageal moniliasis in malignant neoplastic disease. Acta Med Scand. 1964;175:455–9. doi: 10.1111/j.0954-6820.1964.tb00593.x. [DOI] [PubMed] [Google Scholar]
- Johnston RD, Chick EW, Johnston NS, et al. Asymptomatic quantitative increase of Candida albicans in the oral cavity: predisposing conditions. South Med J. 1967;60:1244–7. doi: 10.1097/00007611-196711000-00023. [DOI] [PubMed] [Google Scholar]
- Koletar SL, Russell JA, Fass RJ, et al. Comparison of oral fluconazole and clotrimazole troches as treatment for oral candidiasis in patients infected with human immunodeficiency virus. Antimicrob Agents Chemother. 1990;34:2267–8. doi: 10.1128/aac.34.11.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalsky SF, Dixon DM. Fluconazole: a new antifungal agent. Clin Pharm. 1991;10:179–94. [PubMed] [Google Scholar]
- Kozinin PJ, Taschdjian CL, Dragutsky D, et al. Therapy of oral thrush: a comparative evaluation of gentian violet, mycostatin and amphotericin B. Monogr Ther. 1957;2:16–24. [Google Scholar]
- Krieter P, Flannery B, Musick T, et al. Pharmacokinetics and excretion of 14C posaconazole following oral administration in healthy male subjects. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; September 27–30; San Diego, CA. 2002. [Google Scholar]
- Li X, Brown, Chau AS, et al. Changes in susceptibility to posaconazole in clinical isolates of Candida albicans . J Antimicorb Chemother. 2004;53:74–80. doi: 10.1093/jac/dkh027. [DOI] [PubMed] [Google Scholar]
- McCarthy GM, Mackie ID, Koval J, et al. Factors associated with increased frequency of HIV-related oral candidiasis. J Oral Pathol Med. 1991;20:332–6. doi: 10.1111/j.1600-0714.1991.tb00940.x. [DOI] [PubMed] [Google Scholar]
- Maenza JR, Keruly JC, Moore RD, et al. Risk factors for fluconazole-resistant candidiasis in human immunodeficiency virus-infected patients. J Infect Dis. 1996;173:219–25. doi: 10.1093/infdis/173.1.219. [DOI] [PubMed] [Google Scholar]
- Meunier F, Aoun M, Gerard M. Therapy of oropharyngeal candidiasis in the immunocompromised host: a randomized double-blind study of fluconazole vs. ketoconazole. Rev Infect Dis. 1990;12(Suppl 3):S364–8. doi: 10.1093/clinids/12.supplement_3.s364. [DOI] [PubMed] [Google Scholar]
- Meyer JM, Rodvold KA. Drug biotransformation by the cytochrome P-450 enzyme system. Infect Med. 1996 Jun;:452–4. [Google Scholar]
- Moore RD, Chaisson RE. Natural history of opportunistic disease in an HIV-infected urban clinical cohort. Ann Intern Med. 1996;124:633–42. doi: 10.7326/0003-4819-124-7-199604010-00003. [DOI] [PubMed] [Google Scholar]
- Munayyer HK, Mann PA, Chau AS, et al. Posaconazole is a potent inhibitor of sterol 14 alpha demethylation in yeasts and molds. Antimicrob Agents Chemother. 2004;48:3690. doi: 10.1128/AAC.48.10.3690-3696.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray PA, Koletar SL, Mallegol I, et al. Itraconazole oral solution versus clotrimazole troches for the treatment of oropharyngeal candidiasis in immunocompromised patients. Clin Ther. 1997;19:471–80. doi: 10.1016/s0149-2918(97)80131-2. [DOI] [PubMed] [Google Scholar]
- Odds FC. A review and bibliography. London: Baillière Tindall; 1988. Candida and Candidosis. [Google Scholar]
- Ostrosky-Zeichner L, Rex JH, Pappas PG, et al. Antifungal susceptibility survey of 2,000 bloodstream Candida isolates in the United states. Antimicrob Agents Chemother. 2003;47:3149–54. doi: 10.1128/AAC.47.10.3149-3154.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas PG, Rex JH, Sobel JD, et al. Guidelines for treatment of candidiasis. Clin Infect Dis. 2004;38:161–89. doi: 10.1086/380796. [DOI] [PubMed] [Google Scholar]
- Pfizer, Inc. Package insert. NY, New York: 2003. [Google Scholar]
- Piscitelli SC, Flexner C, Minor JR, et al. Drug interactions in patients infected with human immunodeficiency virus. Clin Infect Dis. 1996;23:685–93. doi: 10.1093/clinids/23.4.685. [DOI] [PubMed] [Google Scholar]
- Pitisuttithum P, Gaona-Flores V, Negroni R, et al. Efficacy of posaconazole in treatment of central nervous system fungal infections: results of an open-label study. 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy; September 14–17; Chicago, IL. 2003. [Google Scholar]
- Pons V, Greenspan D, Debruin M, et al. Therapy for oropharyngeal candidiasis in HIV-infected patients: a randomized, prospective multicenter study of oral fluconazole versus clotrimazole troches. J Acquir Immune Defic Syndr. 1993;6:1311–6. [PubMed] [Google Scholar]
- Pons V, Greenspan D, Lozada-Nur F, et al. Oropharyngeal candidiasis in patients with AIDS: randomized comparison of fluconazole versus nystatin oral suspensions. Clin Infect Dis. 1997;24:1204–7. doi: 10.1086/513664. [DOI] [PubMed] [Google Scholar]
- Quintiliani R, Owens NJ, Quercia RA, et al. Treatment and prevention of oropharyngeal candidiasis. Am J Med. 1994;77(Suppl 4D):44–8. [PubMed] [Google Scholar]
- Raad II, Hachem RY, Herbrecht R, et al. Posaconazole as salvage treatment for invasive fusariosis in patients with underlying hematologic malignancy and other conditions. Clin Infect Dis. 2006;42:1398. doi: 10.1086/503425. [DOI] [PubMed] [Google Scholar]
- Reef SE, Mayer KH. Opportunistic candidal infections in patients infected with human immunodeficiency virus: prevention issues and priorities. Clin Infect Dis. 1995;21(Suppl 1):S99–102. doi: 10.1093/clinids/21.supplement_1.s99. [DOI] [PubMed] [Google Scholar]
- Sabatelli FJ, Patel R, Mann PA, et al. In vitro activities of posaconazole, fluconazole, itraconazole, voriconazole, and amphotericin B against a large collection of clinically important molds and yeasts. Approximately 18,000 strains of clinically significant yeasts and moulds. Antimicrob Agents Chemother. 2006;50:2009. doi: 10.1128/AAC.00163-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schering Corporation. Package insert. Kenilworth, NJ: 2006. [Google Scholar]
- Scott BB, Jenkins D. Gastro-oesophageal candidiasis. Gut. 1982;23:137–9. doi: 10.1136/gut.23.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shectman LB, Funaro L, Robin T, et al. Clotrimazole treatment of oral candidiasis in patients with neoplastic disease. Am J Med. 1984;76:91–4. doi: 10.1016/0002-9343(84)90755-1. [DOI] [PubMed] [Google Scholar]
- Silverman S, Jr, Gallo JW, McKnight ML, et al. Clinical characteristics and management responses in 85 HIV-infected patients with oral candidiasis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:402–7. doi: 10.1016/s1079-2104(96)80304-0. [DOI] [PubMed] [Google Scholar]
- Skiest DJ, Vazquez JA, Anstead GM, et al. Posaconazole for the treatment of azole-refractory oropharyngeal and esophageal candidiasis in subjects with HIV-infection. Clin Infect Dis. 2006 doi: 10.1086/511039. In press. [DOI] [PubMed] [Google Scholar]
- Tucker RM, Denning DW, Hanson LH, et al. Interactions of azoles with rifampin, phenytoin, and carbamazepine: in vitro and clinical observations. Clin Infect Dis. 1992;14:165–74. doi: 10.1093/clinids/14.1.165. [DOI] [PubMed] [Google Scholar]
- Ullmann AJ, Cornely OA, Burchard T, et al. Posaconazole vs fluconazole for prophylaxis of invasive fungal infections in allogenic hematopoietic stem cell transplant recipients with graft-versus-host disease. Poster presented at the 46th Interscience Conference on Antimicrob Agents Chemother.2005. [Google Scholar]
- van Burik JA, Hare RS, Solomon F, et al. Posaconazole is effective as salvage therapy in zygomycosis: a retrospective summary of 91 cases. Clin Infect Dis. 2006;42:e61. doi: 10.1086/500212. [DOI] [PubMed] [Google Scholar]
- Van de Velde VJS, Van Peer AP, Heykants JJP, et al. Effect of food on the pharmacokinetics of a new hydroxypropyl-β-cyclodextrin formulation of itraconazole. Pharmacotherapy. 1996;16:424–8. [PubMed] [Google Scholar]
- van’t Wout JW. Fluconazole treatment of candidal infections caused by non-albicans Candida species. Eur J Clin Microbiol Infect Dis. 1996;15:238–42. doi: 10.1007/BF01591361. [DOI] [PubMed] [Google Scholar]
- Vazquez JA, Sobel JD. Epidemiologic overview of resistance to oral antifungal agents in the immunocompromised host [abstract] Excerpta Medica. 1997:1–11. Abstract. [Google Scholar]
- Vazquez JA. Options for the management of mucosal candidiasis in patients with AIDS and HIV infection. Pharmacotherapy. 1999;19:76–87. doi: 10.1592/phco.19.1.76.30509. [DOI] [PubMed] [Google Scholar]
- Vazquez JA, Sobel JD. Candidiasis. In: Dismukes WE, Pappas PG, Sobel JD, editors. Clinical Mycology. 1. New York, NY: Oxford University Press; 2003. pp. 143–87. [Google Scholar]
- Vazquez JA, Skiest DJ, Nieto L, et al. A multicenter randomized trial evaluating posaconazole versus fluconazole for the treatment of oropharyngeal candidiasis in subjects with HIV/AIDS. Clin Infect Dis. 2006;42:1179–86. doi: 10.1086/501457. [DOI] [PubMed] [Google Scholar]
- Vazquez JA, Skiest DJ, Tissot-Dupont H, et al. Safety and efficacy of posaconazole in the long-term treatment of azole-refractory oropharyngeal and esophageal candidiasis in subjects with HIV infection. HIV Clin Trials. 2007 doi: 10.1310/hct0802-86. In press. [DOI] [PubMed] [Google Scholar]
- Venkatakrishnan K, Von Moltke LL, Greenblatt DJ. Effects of the antifungal agents on oxidative drug metabolism: clinical relevance. Clin Pharmacokinet. 2000;38:111–80. doi: 10.2165/00003088-200038020-00002. [DOI] [PubMed] [Google Scholar]
- Wexler D, Laughlin M, Courtney R, et al. Effect of posaconazole on cytochrome P450 enzymes: a randomized, open-label, two-way crossover study. Eur J Pharm Sci. 2004;21:645. doi: 10.1016/j.ejps.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Wilcox CM, Darouiche RO, Laine L, et al. A randomized, double-blind comparison of itraconazole oral solution and fluconazole tablets in the treatment of esophageal candidiasis. J Infect Dis. 1997;176:227–32. doi: 10.1086/514028. [DOI] [PubMed] [Google Scholar]
- Xiao L, Madison C, Chaui AS, et al. Three-dimensional models of wild-type and mutated forms of cytochrome P450 14 alpha-sterol demethylases from Aspergillus fumigatus and Candida albicans provide insights into posaconazole binding. Antimicrob Agents Chemother. 2004;48:568–74. doi: 10.1128/AAC.48.2.568-574.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]


