Abstract
Parathyroid hormone-related peptide is a regulatory protein implicated in the pathogenesis of bone metastases, particularly in breast carcinoma. Parathyroid hormone-related peptide is widely expressed in primary prostate cancers but there are few reports of its expression in prostatic metastases. The aim of this study was to examine the expression of parathyroid hormone-related peptide and its receptor in matched primary and in bone metastatic tissue from patients with untreated adenocarcinoma of the prostate. Eight-millimetre trephine iliac crest bone biopsies containing metastatic prostate cancer were obtained from 14 patients from whom matched primary tumour tissue was also available. Histological grading was performed by an independent pathologist. The cellular location of mRNA for parathyroid hormone-related peptide and parathyroid hormone-related peptide receptor was identified using in situ hybridization with 35S-labelled probe. Expression of parathyroid hormone-related peptide and its receptor was described as uniform, heterogenous or negative within the tumour cell population. Parathyroid hormone-related peptide expression was positive in 13 out of 14 primary tumours and in all 14 metastases. Receptor expression was evident in all 14 primaries and 12 out of 14 metastases. Co-expression of parathyroid hormone-related peptide and parathyroid hormone-related peptide receptor was common (13 primary tumours, 12 metastases). The co-expression of parathyroid hormone-related peptide and its receptor suggest that autocrine parathyroid hormone-related peptide mediated stimulation may be a mechanism of escape from normal growth regulatory pathways. The high frequency of parathyroid hormone-related peptide expression in metastases is consistent with a role in the pathogenesis of bone metastases.
British Journal of Cancer (2002) 86, 322–325. DOI: 10.1038/sj/bjc/6600115 www.bjcancer.com
© 2002 The Cancer Research Campaign
Keywords: prostate cancer, parathyroid hormone-related peptide, bone metastases
Despite increasing detection and treatment of early prostate cancer, this disease still accounts for 9000 deaths annually in England and Wales (Office for National Statistics, 1998). The development of bone metastases is undoubtedly a major cause of morbidity and mortality; patients presenting with osseous involvement have a mean survival of just 2.5 years (George, 1988).
The overwhelming majority of prostate cancer bone metastases are osteoblastic, characterized by increased rates of lamellar bone resorption and replacement with abnormal woven bone. Therefore, in common with osteolytic metastases, osteoclast activation is a key step in the pathogenesis of osteoblastic bone metastases (Clarke et al, 1991, 1993). Consequently osteo-active cytokines and growth factors produced by cancer cells may influence the tropism of certain tumours for metastasis to bone, and offer an advantage in the genesis of bony secondaries.
Parathyroid hormone related peptide (PTHrP) is a protein with N-terminal homology to PTH (Guise et al, 1997). It is able to bind to and activate the PTH receptor and is consequently a potent stimulant of osteoclasts and osteoblasts (Abou-Samra et al, 1992). Work in breast carcinoma has suggested that PTHrP may be an important factor in bone metastasis. Serum PTHrP levels are elevated in patients with bone metastases (Bundred et al, 1991) and that there is up regulation of PTHrP expression in the metastatic tissue (Powell et al, 1991). Additionally there are also found to be high levels of expression of the receptor for PTHrP in breast cancer bone metastases (Downey et al, 1996).
PTHrP is expressed in benign prostate, although its function is unclear (Cramer et al, 1996). In primary prostate cancer PTHrP staining intensity increases with tumour grade (Asadi et al, 1996), and in vitro cell line studies have suggested that it may be a significant autocrine growth factor (Iwamura et al, 1994a). Drawing on the work in breast cancer and the parallels between the two tumours, it has been suggested that PTHrP may be a potential factor in the pathogenesis of prostate cancer bone metastases (Guise, 1997).
It is hypothesized that expression of PTHrP and PTHrP receptor (PTHrPr) offer an advantage in the genesis of bone metastases in prostate cancer through paracrine and autocrine mechanisms. The aim of this study was to test this hypothesis by investigation of the co-expression of PTHrP and PTHrP receptor in matched pairs of untreated primary prostate cancer and their corresponding bone metastases.
MATERIALS AND METHODS
Having obtained informed consent, iliac crest bone biopsies were taken from men known or strongly suspected to have untreated metastatic prostate cancer from whom primary prostatic tissue was also available. Local Ethics Committee approval was granted for the study. All specimens were fixed in formalin and the bone biopsies decalcified in EDTA. All tissue was embedded in paraffin wax. On analysis of the bone specimens 14 were found to contain metastatic prostate cancer. All primary and metastatic tumours were graded according to the Gleason system (Gleason and Mellinger, 1974) by an independent pathologist.
The expression of PTHrP and PTHrPr were determined by in situ hybridization on 7 μm tissue sections. The cDNA probes were kind gifts to the Department of Osteoarticular Pathology from Dr MT Gillespie (St Vincent's Institute for Medical Research, Victoria, Australia) and Dr E Schipani (Massachusetts General Hospital, MA, USA) respectively.
Probe labelling
Radioactive labelling of the probe using 35S was achieved using the Amersham Megaprime™ DNA labelling system. The probe and primer were mixed, then the double stranded DNA probe denatured by immersion in a boiling bath. The labelling reaction was initiated by mixing the denatured DNA, reaction buffer, unlabelled deoxynucleotide triphosphate, 35S-deoxycytosine triphosphate, and Kenlow fragment of DNA polymerase. Following incubation at 37°C for 1 h, the reaction was stopped by the addition of 0.2 M EDTA pH 8.0. The labelled probe was then purified by centrifugation.
Prehybridization
Following dewaxing, tissue sections mounted on sialane coated slides were subjected to the following procedures. Tissue permeabilization was carried out by incubation with proteinase K for 1 h (5 μg ml−1 for prostate and 10 μg ml−1 for bone sections). Control sections were created by elimination of the hybridization signal by incubation for 2 h at 37°C with RNase A. Post-fixation was carried out in 0.4% paraformaldehyde at 4°C.
Hybridization
The hybridization buffer containing the 35S-labelled probe was applied to all tissue sections and then incubated overnight at 37°C.
Post-hybridization washes
A series of progressively higher stringency washes were performed, using 0.5×SSC/1 mM EDTA/10 mM Dithiolthreitol, then 0.5×SSC/1 mM EDTA, and then in 50% formamide : 50% 0.15 M NaCl/5 mM Tris pH 7.4/0.5 mM EDTA pH 8.0, (SSC – standard saline citrate solution: 7.5 mM NaCl/0.75 mM NaCitrate). Final washes were then performed in 0.5×SSC, initially at 55°C then at room temperature. Sections were dehydrated in industrial methylated spirit and air dried.
Detection
Binding of the radiolabelled probe was detected by autoradiography. After exposure at 4°C for 2–3 weeks to a layer of Ilford K5 emulsion, slides were developed using Ilford D-19 developer, and fixed with Ilford Hypam. Sections were counter stained with Mayer's haematoxylin, dehydrated and mounted with Xam.
Analysis
Precipitation of the silver granules produced by autoradiography was assessed using a Leitz Laborlux 12 microscope with the ×20 objective lens, with transmitted light and dark field condensers. The distribution of signal across the tumour cell was described as uniform, heterogeneous or negative.
RESULTS
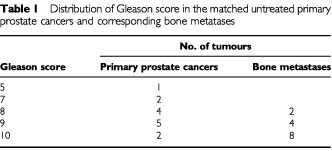
Only three of the primary tumours were moderately differentiated, the remainder being poorly differentiated (Gleason ⩾8). All metastases were poorly differentiated. The distribution of tumour grades are shown in Table 1.
Table 1. Distribution of Gleason score in the matched untreated primary prostate cancers and corresponding bone metatases.
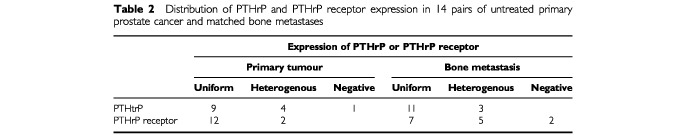
PTHrP expression was positive in 13 out of 14 primary tumours and in all 14 metastases. PTHrP expression was greater in the metastases than the primary tumours. Uniform staining was detected in 11 cases, three metastases exhibited heterogeneous staining, and in no case was PTHrP staining negative. Receptor expression was evident in all 14 primaries and 12 out of 14 metastases. The majority of primary tumours (85%) had uniform expression, while seven and five metastases had uniform (Figure 1) and heterogeneous staining respectively. In eight cases there was similar expression levels of PTHrP receptor in the paired tumours, while in six cases there was down regulation of receptor expression in the metastatic prostate cells. The patterns of PTHrP and PTHrP receptor expression in the specimens are summarized in Table 2.
Figure 1.
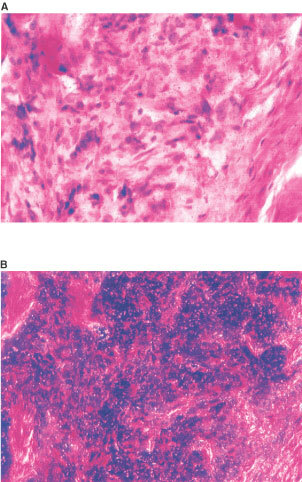
Section of prostatic bone metastasis having undergone in-situ hybridization with the probe for PTHrP receptor. Micrograph (A) standard light ground field, stained with H&E, and micrograph (B) is the same section but with dark ground field, and the silver grains show as the bright spots. The distribution of the bright spots over the metastatic cells indicate uniform signal for PTHrP receptor.
Table 2. Distribution of PTHrP and PTHrP receptor expression in 14 pairs of untreated primary prostate cancer and matched bone metastases.
DISCUSSION
Animal models of bone metastasis have demonstrated the importance of PTHrP in the metastatic cascade. The activation of osteoclasts by PTHrP in conjunction with interleukin 1 has been shown to be essential for bone metastasis development (Arguello et al, 1988). In mice inoculated with highly metastatic breast and lung cancer cell lines, treatment with an anti-PTHrP antibody, reduced both tumour burden and osteoclastic bone resorption (Guise et al, 1996; Iguchi et al, 1996).
PTHrP has been most extensively investigated in breast carcinoma, where 60% of primary tumours are found to have positive expression of PTHrP (Southby et al, 1990; Bundred et al, 1992). In metastases in soft tissues only 17% are positive for PTHrP in contrast to 92% of those in bone (Powell et al, 1991). These findings support the view that PTHrP has a role in the development and progression of bone metastases.
Although PTHrP is expressed in normal prostate (Cramer et al, 1996), benign prostatic epithelial cells do not show enhancement of growth in the presence of PTHrP in tissue culture (Peehl et al, 1997). PTHrP is secreted by all three commonly studied human malignant prostatic cell lines (PC3, DU-145, and LNCaP) and levels are highest in the bone metastasis derived PC3 line (Iwamura et al, 1994a). The same study demonstrated that culture with synthetic PTHrP led to increased proliferation of PC3 and DU-145 cells (Iwamura et al, 1994a), suggesting that PTHrP may be a significant autocrine factor in prostate tumour growth, particularly in bone metastases.
PTHrP expression in primary prostatic carcinoma is common (Iwamura et al, 1993; Lee et al, 1997). Lymph node metastases exhibit similar levels of PTHrP expression to those of poorly differentiated primary tumours (Asadi et al, 1996). In this study mRNA for PTHrP was detected in all 14 primary prostate tumours, although expression was heterogeneous in four cases. In the corresponding bone metastases, all 14 were positively staining, all but three being uniformly stained. Previous studies of 10 (Bryden et al, 2002) and 14 (Iddon et al, 2000) archival prostatic bone metastases by immunohistochemistry have demonstrated PTHrP expression in only 50% of samples. Differences in the technique of PTHrP detection are unlikely to account for this, as concordance between immunohistochemistry and in-situ hybridization for detection of PTHrP has been described (Iwamura et al, 1994b) suggesting that PTHrP expression is regulated at the gene level. This difference may be due to variation in PTHrP expression with tumour grade as described for primary prostate carcinoma (Iwamura et al, 1993). In our previous study 7 out of 10 specimens contained well or moderately differentiated tumour (Bryden et al, 2002), and lower levels of PTHrP expression might be anticipated than in the exclusively poorly differentiated group of prospectively collected metastases. In the series investigated by Iddon et al (2000), neither the differentiation of the metastases, nor their treatment status (untreated, hormone manipulated or escaped hormonal control) is described, and it is therefore difficult to comment given these variables. It must also be considered that the sample sizes are small and that the differences in levels of PTHrP expression might simply represent true variation.
Despite the proposed importance of PTHrP in the development of prostatic bone metastases, paradoxically, hypercalcaemia is found in less than 2% of patients. In contrast to this, hypercalcaemia is seen in up to 20% of breast cancer sufferers with bone metastases (Coleman and Reubens, 1987). Hypercalcaemia may be partially accounted for by the release of bone bound calcium from lytic deposits, and conversely in the sclerotic metastases of prostate cancer there is calcium ‘bone hunger’ for new bone formation, which may even lead to secondary hyperparathyroidism (Minisola et al, 1987). However the humoural contribution of PTHrP to calcium homeostasis derangement is well described in breast cancer, and the detection of PTHrP is strongly correlated with hypercalcaemia (Bundred et al, 1991). Few studies have investigated the serum levels of PTHrP in prostate cancer specifically but levels have been found to be similar to those in normocalcaemic patients without malignancy (Kao et al, 1990). This would be consistent with the variable secretion of PTHrP into the serum from tumours in which PTHrP can be detected (Dunne et al, 1993). Consequently the autocrine/paracrine effects of PTHrP are not universally coupled to the humoural effects.
Staining of the same specimens for the receptor for PTHrP was positive in all 14 primary prostate tumours and expression was heterogeneous in only two cases. In the bone metastases, 12 of 14 stained positively, but in six staining was heterogeneous. The role of the PTHrP receptor has not previously been described clearly in benign or malignant human prostate tissue. Immunohistochemistry has failed to demonstrate the PTHrP receptor in the canine model of benign prostate (Blomme et al, 1998), which would be consistent with the lack of growth factor response to PTHrP found in benign prostate by Peehl et al (1997).
The high levels of PTHrP receptor demonstrated in this study in primary (100%) and metastatic (85%) prostate cancer are similar to those described in breast carcinoma, where PTHrP receptor can be detected in 61–96% of tumours (Carron et al, 1997; Downey et al, 1997; Iezzoni et al, 1998) using in-situ hybridization or PCR. There are no comparable data for prostate cancers available. However for PTHrP to have an autocrine or paracrine effect, it is logical that the PTHrP receptor would need to be expressed within the tissue. PTHrP does not appear to act as a growth factor in benign tissue (Peehl et al, 1997), consequently it might be hypothesized that development of PTHrP receptor expression is a significant component of the malignant phenotype.
Overall, this study has shown a high level of expression of PTHrP and its receptor in bone metastases of prostate cancer and their corresponding primary tumours. This supports the previously described work in prostate and other tumour systems, proposing that PTHrP is a likely mediator predisposing to the formation of bone metastases. The co-expression of PTHrP and its receptor would suggest that PTHrP is able to act as an autocrine and/or paracrine growth factor in prostate cancer.
Further work to define and investigate the expression of the PTHrP receptor in benign and malignant prostatic tissue would be important to determine whether this is a feature exclusive to malignant prostatic cells and whether there is any temporal relationship to the presence of bone metastases.
Acknowledgments
This work was supported by the Prostate Research Campaign (UK)
References
- Abou-SamraAJuppnerHForceTFreemanMWKongXFSchipaniEUrenaPRichardsJBonventreJVPottsJrJT1992Expression cloning of a common receptor for parathyroid hormone and parathyroid hormone-related peptide from rat osteoblast-like cells: a single receptor stimulates intracellular accumulation of both cAMP and inositol trisphosphates and increases intracellular free calcium Proc Natl Acad Sci USA 8927322736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ArguelloFBaggsRBFrantzCN1988A murine model of experimental metastasis to bone and bone marrow Cancer Res 4868766881 [PubMed] [Google Scholar]
- AsadiFFarrajMSharifiRMalakoutiSAntarSKukrejaS1996Enhanced expression of parathyroid hormone-related protein in prostate cancer as compared with benign prostatic hyperplasia Hum Pathol 2713191323 [DOI] [PubMed] [Google Scholar]
- BlommeESugimotoYMcCauleyLKLinYCCapenCCRosolTJ1998Stromal and epithelial cells of the canine prostate express parathyroid hormone-related protein, but not the PTH/PTHrP receptor Prostate 36110120 [DOI] [PubMed] [Google Scholar]
- BrydenAAGIslamSFreemontAJShanksJHClarkeNWGeorgeNJR2002Parathyroid hormone-related peptide expression in prostatic bone metastases Prostate Cancer Prostatic Dis,in press [DOI] [PubMed]
- BundredNJRatcliffeWAWalkerRAColeySMorrisonJMRatcliffeJG1991Parathyroid hormone related protein and hypercalcaemia in breast cancer Br Med J 30315061509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BundredNJWalkerRARatcliffeWAWarwickJMorrisonJMRatcliffeJG1992Parathyroid hormone related protein and skeletal morbidity in breast cancer Eur J Cancer 28690692 [DOI] [PubMed] [Google Scholar]
- CarronJFraserWDGallagherJA1997PTHrP and the PTH/PTHrP receptor are co-expressed in human breast and colon tumours Br J Cancer 7610951098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ClarkeNWMcLureJGeorgeNJR1991Morphometric evidence for bone resorption and replacement in prostate cancer Br J Urol 687480 [DOI] [PubMed] [Google Scholar]
- ClarkeNWMcLureJGeorgeNJR1993Osteoblastic function and osteomalacia in metastatic prostate cancer Eur Urol 24286290 [DOI] [PubMed] [Google Scholar]
- ColemanRReubensRD1987The clinical course of bone metastases from breast cancer Br J Cancer 556166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CramerSPeehlDMEdgarMGWongSTDeftosLJFeldmanD1996Parathyroid hormone-related protein (PTHrP) is an epidermal growth factor-regulated secretory product of human prostatic epithelial cells Prostate 292029 [DOI] [PubMed] [Google Scholar]
- DowneySHoylandJABundredNJFreemontAJ1996Is overexpression of parathyroid hormone-related peptide receptor a predisposing factor in bone metastases from breast cancer? Br J Surg 83699 [Google Scholar]
- DowneySHoylandJFreemontAJKnoxFWallsJBundredNJ1997Expression of the receptor for parathyroid hormone-related protein in normal and malignant breast tissue J Pathol 183212217 [DOI] [PubMed] [Google Scholar]
- DunneFLeeSRatcliffeWAHutchessonACBundredNJHeathDA1993Parathyroid hormone-related protein (PTHrP) gene expression in solid tumours associated with normocalcaemia and hypercalcaemia J Pathol 171215221 [DOI] [PubMed] [Google Scholar]
- GeorgeNJR1988Natural history of localised prostate cancer managed by conservative therapy alone Lancet i494497 [DOI] [PubMed] [Google Scholar]
- GleasonDMellingerGT1974Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging J Urol 1115864 [DOI] [PubMed] [Google Scholar]
- GuiseTYinJJTaylorSDKumagaiYDallasMBoyceBFYonedaTMundyGR1996Evidence for a causal role of parathyroid hormone-related protein in the pathogenesis of human breast cancer-mediated osteolysis J Clin Invest 9815441549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GuiseT1997Parathyroid hormone-related protein and bone metastases Cancer 8015721580 [DOI] [PubMed] [Google Scholar]
- IddonJBundredNJHoylandJDowneySEBairdPSalterDMcMahonRFreemontAJ2000Expression of parathyroid hormone-related protein and its receptor in bone metastases from prostate cancer J Pathol 191170174 [DOI] [PubMed] [Google Scholar]
- IezzoniJBrunsMEFriersonHFScottMGPenceRADeftosLJBrunsDE1998Coexpression of parathyroid hormone-related protein and its receptor in breast carcinoma: a potential autocrine effector system Mod Pathol 11265270 [PubMed] [Google Scholar]
- IguchiHTanakaSOzawaYKashiwakumaTKimuraTHiragaTOzawaHKonoA1996An experimental model of bone metastasis by human lung cancer cells: the role of parathyroid hormone-related protein in bone metastasis Cancer Res 5640404043 [PubMed] [Google Scholar]
- IwamuraMdi Sant'AgneseWuGBenningCMCockettATKDeftosLJAbrahamssonP-A1993Immunohistochemical localization of parathyroid hormone-related protein in human prostate cancer Cancer Res 5317241726 [PubMed] [Google Scholar]
- IwamuraMAbrahamssonP-AFossKAWuGCockettATKDeftosLJ1994aParathyroid hormone related protein: a potential autocrine growth regulator in human prostate cancer cell lines Urology 43675679 [DOI] [PubMed] [Google Scholar]
- IwamuraMWuGAbrahamssonPAdi Sant'AgnesePACockettATDeftosLJ1994bParathyroid hormone-related protein is expressed by prostatic neuroendocrine cells Urology 43667674 [DOI] [PubMed] [Google Scholar]
- KaoPKleeGGTaylorRLHeathH1990Parathyroid hormone-related peptide in the plasma of patients with hypercalcaemia and malignant lesions Mayo Clin Proc 6513991407 [DOI] [PubMed] [Google Scholar]
- LeeCWojnoKJOesterlingJESingletonTMcCauleyLLehrJMontieJEPientaK1997Expression of parathyroid hormone-like protein in prostate cancer and prostatic intraepithelial neoplasia J Urol 157225 [Google Scholar]
- MinisolaSPerugiaGScardaAScarnecchiaLTuzzoloDRossiWMazzuoliG1987Biochemical picture accompanying sclerotic bone metastases of prostatic origin Br J Urol 60443446 [DOI] [PubMed] [Google Scholar]
- Office for National Statistics1998Estimates of newly diagnosed cancers, England and Wales 19931997InONS Monitor Population and Health.The Stationery Office: London [Google Scholar]
- PeehlDEdgarMGCramerSDDeftosLJ1997Parathyroid hormone-related protein is not an autocrine growth factor for normal prostatic epithelial cells Prostate 314752 [DOI] [PubMed] [Google Scholar]
- PowellGSouthbyJDanksJAStillwellRGHaymanJAHendersonMABennettRCMartinTJ1991Localization of parathyroid hormone-related protein in breast cancer metastases: increased incidence in bone compared with other sites Cancer Res 5130593061 [PubMed] [Google Scholar]
- SouthbyJKissinMWDanksJAHaymanJAMoseleyJMHendersonMABennettRCMartinTJ1990Immunohistochemical localization of parathyroid hormone-related protein in human breast cancer Cancer Res 5077107716 [PubMed] [Google Scholar]


