Abstract
Several in vitro studies have demonstrated that genetic polymorphisms result in functionally significant changes in cytochrome p4501A1 (either CYP1A1 MspI or exon 7) but the few epidemiologic studies of these polymorphisms in oesophageal squamous-cell carcinoma have been inconclusive. These inconclusive results motivated us to further examine the relationship between CYP1A1 MspI and exon 7 polymorphisms and risk of oesophageal cancer. In total, 146 cases of oesophageal squamous-cell-carcinoma and 324 control cases (a total of 470 cases) were genotyped from records at three Taiwan hospitals. No significant association was noted for the CYP1A1 MspI polymorphism variable between carcinoma and control cases. In contrast, the frequency of Ile/Ile, Ile/Val, and Val/Val in exon 7 was 68 (46.6%), 62 (42.5%), and 16 (11.0%) in carcinoma cases and 179 (55.3%), 127 (39.2%), and 18 (5.6%) in control cases, respectively. After factoring out other potential contributing factors, patients with Val/Val showed a 2.48 (95% CT=1.15–5.34) greater risk of developing oesophageal cancer than those with Ile/Ile. A slightly (albeit not significantly) greater risk was identified in subjects with Ile/Val (OR=1.34; 95% CI=0.86–2.07). These findings suggest that an exon 7 polymorphism, not a MspI polymorphism, in CYP1A1 may be pivotal in the development of oesophageal cancer.
British Journal of Cancer (2002) 87, 529–532. doi:10.1038/sj.bjc.6600499 www.bjcancer.com
© 2002 Cancer Research UK
Keywords: oesophageal cancer, squamous-cell-carcinoma, cytochrome p4501A1, genetic polymorphism
The CYP1A1 gene code in the aryl hydrocarbon hydroxylase (AHH) enzyme is closely associated with the metabolism of polycyclic aromatic hydrocarbons (PAHs) carcinogens (Crofts et al, 1994). Previous studies have suggested that variant alleles of CYP1A1 MspI polymorphism are associated with malignancies, particularly lung cancer (Kawarjiri et al, 1990; Nakachi et al, 1991; Hayashi et al, 1992; Xu et al, 1996). As reported by Bartsch et al (2000), no association was identified between CYP1A1 MspI and exon 7 polymorphisms and oesophageal cancer risk in a series of studies done on populations of Caucasians and Japanese (Lucas et al, 1996; Hori et al, 1997; Morita et al, 1997; van Lieshout et al, 1999). However, Nimura et al (1997) studied 89 oesophageal carcinoma patients and 137 cancer-free control patients in an ethnically Chinese population and reported that heavy smokers with Val/Val genotypes of CYP1A1 exon 7 had a three-fold risk of developing oesophageal cancer as compared to those with Ile/Ile genotypes. A subsequent study by Roth et al (2000) did not find any significant effect of CYP1A1 exon 7 polymorphisms in 56 individuals with mild or moderate squamous dysplasia and 56 control individuals (a relatively small sample size) from Linxian, a region of high oesophageal cancer risk in China. Recently, Wang et al (2002) genotyped 127 oesophageal cancer cases and 101 controls and found that individuals with the CYP1A1 Val/Val genotype had a higher risk of developing oesophageal cancer than those with Ile/Ile (OR=2.48, 95%CI=1.12–5.54). In view of the apparently significant influence of ethnicity in previous studies, we have examined further the role of CYP1A1 MspI and exon 7 polymorphisms in oesophageal cancer risk in Taiwan.
MATERIALS AND METHODS
Selection of cases and controls
Over the four-year period of this study, we recruited 146 patients with pathologically-proven oesophageal squamous-cell-carcinoma undergoing treatment at three hospitals in Taiwan, including the National Taiwan University Hospital, the Kaohsiung Medical University Hospital, and the Kaohsiung Veterans General Hospital. Concurrently, the preventive medicine department at each hospital did their best to also recruit 1–4 malignancy-free subjects per recruited carcinoma patient as healthy controls (n=324). Healthy control subjects were selected based on being the same gender as the recruited carcinoma patient and being in the hospital during the same time and of roughly the same age (±3 years). Subjects in this study were interviewed by trained interviewers using a standardized questionnaire to collect demographic and substance use (cigarette, alcohol, and areca) information. This study was approved by National Taiwan University's IRB Hospital. Informed consent was obtained from all subjects.
CYP1A1 MspI polymorphism
The MspI polymorphism in the CYP1A1 3′ flanking region was determined using PCR and RFLP (Wu et al, 1998). The DNA sample was amplified with 2 primers: 5′-CAGTGAAGAGGTGTAGCCGC-3′ (upstream) and 5′-TAGGAGTCTTGTCTCATGCC-3′ (downstream) (Perkin Elmer, Taipei, Taiwan). Amplification was performed by initial denaturation at 94°C for 5 min, followed by 30 cycles at 94°C for 1 min, 61°C for 1 min, 72°C for 1 min, and a final extension at 72°C for 7 min.
The 10-μl amplification result was digested using 3 units MspI (New England Biolabs, Beverly, MA, USA). When an MspI restriction site was present, the fragment of 340 bp was digested into two lengths of 140- and 200-bp. Homozygous wild-type individuals lacked the 140- and 200-bp fragment, and heterozygous individuals had three bands; homozygous-rare allele individuals lacked the large parent band while showing the smaller bands.
CYP1A1 Ile/Val polymorphism
The BsrDI polymorphism in CYP1A1 exon 7 was determined using PCR and RFLP, according to the method used by Cascorbi et al (1996), albeit with slight modifications. The DNA sample was amplified with two primers: 5′-CTGTCTCCCTCTGGTTACAGGAAGC-3′ (upstream) and 5′-TTCCACCCGTTGCAGCAGGATAGCC-3′ (downstream) (Perkin Elmer, Taipei, Taiwan). Amplification was performed by initial denaturation at 95°C for 5 min, followed by 35 cycles at 95°C for 30 s, 73.5°C for 30 s, 72°C for 30 s, and a final extension at 72°C for 7 min. The final product was digested by BsrDI. When a BsrDI restriction site was present, the fragment of 204-bp was digested into two lengths of 65- and 139-bp. Individuals with Ile/Ile had the 65- and 139-bp fragment, heterozygous individuals had three bands; and individuals with Val/Val retained the larger parent bands (204-bp).
Laboratory QA/QC
We included one positive control and one negative control samples in each genotyping set (∼10 samples). The positive control sample was included to ensure complete digestion of the PCR product by restriction enzymes. The negative control was placed with the same reagents as those used with actual samples, with the exception of DNA templates.
Statistical analysis
The gene frequency and Hardy-Weinberg equilibrium tests were conducted, with results entered into multiple logistic regression models to determine, after adjustments had been made for other factors of influence, the level of association between CYP1A1 MspI and exon 7 polymorphisms and oesophageal cancer risk. Factors of influence (covariates) in the models included the variables of age (>65 years and ⩽65 years), gender, education level (⩾college, high school, and ⩽elementary school), and race (Fukienese, Mainlander, and ‘other’). The data were analysed using the SAS statistical package and all P-values were two-sided.
RESULTS
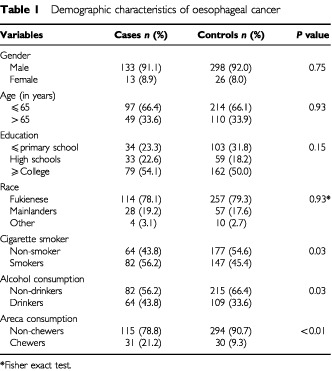
The mean age for carcinoma and control cases was 60.6 and 61.2 years, with an associated age range of 37 to 81 and 34 to 84 years, respectively. The habitual use of cigarettes (P=0.03), alcohol (P=0.03), and areca (P<0.01) provided the most significant predictors of oesophageal cancer risk (Table 1).
Table 1. Demographic characteristics of oesophageal cancer.
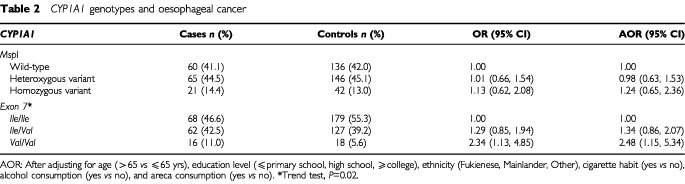
The frequency of MspI polymorphism in wild-type, heterozygous variant, and homozygous variant control cases was 136 (42.0%), 146 (45.1%), and 42 (13.0%), respectively. The gene frequency of the variant allele was 35.5%. The frequency of Ile/Ile, Ile/Val, and Val/Val in exon 7 among controls was 179 (55.3%), 127 (39.2%), and 18 (5.6%), respectively. The gene frequency of the variant allele (Val) was 25.2%. The distribution of the different genotypes in both MspI and exon 7 polymorphisms among the 324 control cases closely conformed to Hardy-Weinberg expected frequencies (χ2=0.04; d.f.=2; P=0.98 and χ2=0.28; d.f.=2; P=0.87, respectively).
The frequency of Ile/Ile, Ile/Val, and Val/Val in exon 7 was 68 (46.6%), 62 (42.5%), and 16 (11.0%) in carcinoma cases and 179 (55.3%), 127 (39.2%), and 18 (5.6%) in control cases, respectively. As lists of those genotypes with elevated oesophageal cancer risk were similar both after adjusting only for substance use and after adjusting for substance use along with age, gender, education, and race, we present here the results for the latter category. Compared to those with Ile/Ile, subjects carrying Val/Val had a 2.34-fold risk (95% CI=1.13–4.85) of developing oesophageal cancer. After adjusting for other potential confounding factors, the result remained similar (OR=2.48; 95% CI=1.15–5.34) (Table 2). The results show even a slightly greater risk after further adjusting for MspI polymorphism (OR=2.71; 95% CI=1.75–6.38). A slight, but not significant, risk elevation was found in subjects with Ile/Val both before and after adjusting for confounding factors (OR=1.29 and 1.34; 95% CI=0.85–1.94 and 0.86–2.07, respectively). In contrast, we found no significant polymorphic effect of CYP1A1 MspI on oesophageal cancer (Table 2).
Table 2. CYP1A1 genotypes and oesophageal cancer.
DISCUSSION
The results of this study found that those cases with the CYP1A1 Val/Val genotype had a 2.34 times higher risk (95% CI=1.13–4.85) of developing oesophageal cancer than those with the Ile/Ile genotype. In contrast, the CYP1A1 MspI genetic polymorphism was not found to be associated with elevated oesophageal cancer risk. Several studies on ethnic Japanese populations reported no association between CYP1A1 MspI and exon 7 polymorphisms and risk of oesophageal cancer (Hori et al, 1997; Morita et al, 1997; van Lieshout et al, 1999). However, their small case population (less than 100 oesophageal cancer cases were investigated) may not be sufficient to make a scientific determination regarding genotype significance. Although Roth et al (2000) found no significant effect of CYP1A1 exon 7 polymorphisms on either the 56 individuals with mild or moderate squamous dysplasia or the 56 control cases from a high oesophageal cancer risk region with an ethnic Chinese population, Nimura et al (1997) found subjects in China with heavy smoking habits had a three times higher frequency of the CYP1A1 Val/Val variant. Recently, Wang et al (2002) also found that individuals with the CYP1A1 Val/Val genotype had a higher risk of developing oesophageal cancer than those with the Ile/Ile (OR=2.48, 95% CI=1.12–5.54). Our findings approximate the Wang et al (2002) findings.
Human cancers, e.g., gastrointestinal cancers, were suggested to be the result of the activation of procarcinogens into carcinogens (Nakajima et al, 1996). Murray et al (1994) and Nakajima et al (1996) examined the expression of cytochrome P450s in human esophagi with squamous-cell carcinomas. Both studies found that the amount of cytochrome P450 1A1 expression in tumorous tissue to be significantly higher than that in non-tumorous tissues. These two findings suggest that the inducible CYP1A1 gene might contribute to oesophageal cancer development. In two in vitro studies, Kiyohara et al (1996) examined the relationship between AHH inducibility (3-methylcholanthrene (MC)-induced AHH activity/non-induced AHH activity) and the frequency of CYP1A1 MspI and exon 7 polymorphisms in peripheral lymphocytes in 84 healthy Japanese male subjects in vitro. They found the age-adjusted AHH inducibility (mean±standard error) of the wild-type, heterozygous, and homozygous variants of the CYP1A1 MspI gene to be 4.89±0.36, 4.82±0.29, and 13.61±1.44, respectively. Furthermore, the homozygous variants had significantly higher AHH inducibility than the combined wild-type and heterozygous variants. However, no association was found between AHH inducibility and CYP1A1 exon 7 polymorphisms. In contrast, Crofts et al (1994) measured gene expression levels and AHH enzymatic activity levels of MspI and exon 7 polymorphisms in mitogen-stimulated lymphocytes in 51 healthy subjects. They reported that subjects with the exon 7 polymorphism (variant alleles) (n=12) had a relative level of CYP1A1 mRNA inducibility (induced/basal) of 9.0±1.7, versus 5.9±0.6 in people with the wild-type alleles (n=39). However, variant genotypes at the MspI site had no effect on CYP1A1 gene induction. Our results in this epidemiologic study align more closely with those obtained by Crofts et al (1994).
Our previous study found the prevalence (number) of homozygous wild-types, heterozygous variants, and homozygous variants in CYP1A1 MspI polymorphisms to be 42.5% (34), 42.5% (34), and 15.0% (12), respectively, among 80 coke-oven workers (Wu et al, 1998). This distribution parallels the control population recruited for our present study, suggesting no potential selection bias was present.
In summary, this study found CYP1A1 exon 7 (but not MspI) polymorphism to be a factor in elevated oesophageal cancer risk. This association suggests that carcinogen biotransformation may be a contributing factor to the etiology of oesophageal squamous-cell-carcinoma among the population in Taiwan.
Acknowledgments
This research was supported by grants from the Taiwan National Science Council (NSC 90-2320-B-037-040 and NSC 90-2320-B-037-052), the Taiwan National Health Research Institute (NHRI-CN-IN-9007P), and the Faculty Research Innovation Fund of Kaohsiung Medical University (Drs TF Chen and OL Chen).
References
- BartschHNairURischARojasMWikmanHAlexandrovK2000Genetic polymorphism of CYP genes, alone or in combination, as a risk modifier of tobacco-related cancers Cancer Epidemiol Biomarkers Prev 9328 [PubMed] [Google Scholar]
- CascorbiIBrockmollerJRootsI1996A C4887A polymorphism in exon 7 of human CYP1A1: population frequency, mutation linkages, and impact on lung cancer susceptibility Cancer Res 5649654969 [PubMed] [Google Scholar]
- CroftsFTaioliETrachmanJCosmaGNCurrieDTonioloPGarteSJ1994Functional significance of different human CYP1A1 genotypes Carcinogenesis 1529612963 [DOI] [PubMed] [Google Scholar]
- HayashiSWatanabeJKawarjiriK1992High susceptibility to lung cancer analyzed in terms of combined genotype P4501A1 and Mu-class glutathione-S-transferase genes Jpn J Cancer Res 83866870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HoriHKawanoTEndoMYuasaY1997Genetic polymorphisms of tobacco- and alcohol-related metabolizing enzymes and human oesophageal squamous cell carcinoma susceptibility J Clin Gastroenterol 25568575 [DOI] [PubMed] [Google Scholar]
- KawarjiriKNakachiKImaiKYoshiiAShinodaNWatanabeJ1990Identification of genetically high risk individuals to lung cancer by DNA polymorphisms of the cytochrome P4501A1 gene FEBS Lett 263131133 [DOI] [PubMed] [Google Scholar]
- KiyoharaCHirohataTInutsukaS1996The relationship between aryl hydrocarbon hydroxylase and polymorphisms of the CYP1A1 gene Jpn J Cancer Res 871824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LucasDMenezCFlochFGourlaouenYSparfelOJoannetIBodenezPJezequelJGouerouHBerthouFBardouLGMenezJF1996Cytochromes P4502E1 and P4501A1 genotypes and susceptibility to cirrhosis or upper aerodigestive tract cancer in alcoholic caucasians Alcohol Clin Exp Res 2010331037 [DOI] [PubMed] [Google Scholar]
- MoritaSYanoMShiozakiHTsujinakaTEbisuiCMorimotoTKishibutiMFujitaJOgawaATaniguchiMInoueMTamuraSYamazakiKKikkawaNMizunoyaSMondenM1997CYP1A1, CYP2E1 and GSTM1 polymorphisms are not associated with susceptibility to squamous-cell carcinoma of the esophagus Int J Cancer 71192195 [DOI] [PubMed] [Google Scholar]
- MurrayGIShawDWeaverRJMcKayJAEwenSWMelvinWTBurkeMD1994Cytochrome P450 expression in oesophageal cancer Gut 35599603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NakachiKImaiKHayashiSWatanabeJKawarjiriK1991Genetic susceptibility to squamous cell carcinoma of the lung in relation to cigarette smoking dose Cancer Res 5151775180 [PubMed] [Google Scholar]
- NakajimaTWangRSNimuraYPinYMHeMVainioHMurayamaNAoyamaTIidaF1996Expression of cytochrome P450s and glutathione S-transferases in human esophagus with squamous-cell carcinomas Carcinogenesis 1714771481 [DOI] [PubMed] [Google Scholar]
- NimuraYYokoyamaSFujimoriMAokiTAdachiWNasuTHeMPingYMIidaF1997Genotyping of the CYP1A1 and GSTM1 genes in oesophageal carcinoma patients with special reference to smoking Cancer 80852857 [DOI] [PubMed] [Google Scholar]
- RothMJDawseySMWangGTangreaJAZhouBRatnasingheDWoodsonKGOliveroOAPoirierMCFryeBLTaylorPRWestonA2000Association between GSTM1*0 and squamous dysplasia of the esophagus in the high risk region of Linxian, China Cancer Lett 1567381 [DOI] [PubMed] [Google Scholar]
- van LieshoutEMRoelofsHMDekkerSMulderCJWobbesTJansenJBPetersWH1999Polymorphic expression of the glutathione S-transferase P1 gene and its susceptibility to Barrett's esophagus and oesophageal carcinoma Cancer Res 59586589 [PubMed] [Google Scholar]
- WangAHSunCSLiLSHuangJYChenQS2002Relationship of tobacco smoking CYP1A1 GSTM1 gene polymorphism and oesophageal cancer in Xi'an World J Gastroenterol 84953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WuMTHuangSLHoCKYehYFChristianiDC1998Cytochrome P450 1A1 MspI polymorphism and urinary 1-hydroxypyrene concentrations in coke-oven workers Cancer Epidemiol Biomarkers Prev 7823829 [PubMed] [Google Scholar]
- XuXKelseyKTWienckeJKWainJCChristianiDC1996Cytochrome P450 CYP1A1 MspI polymorphism and lung cancer susceptibility Cancer Epidemiol Biomark Prev 5687692 [PubMed] [Google Scholar]


