Summary
Objective
To assess reasons for low uptake of immunization amongst orthodox Jewish families.
Design
Qualitative interviews with 25 orthodox Jewish mothers and 10 local health care workers.
Setting
The orthodox Jewish community in North East London.
Main outcome measures
Identification of views on immunization in the orthodox Jewish community.
Results
In a community assumed to be relatively insulated from direct media influence, word of mouth is nevertheless a potent source of rumours about vaccination dangers. The origins of these may lie in media scares that contribute to anxieties about MMR. At the same time, close community cohesion leads to a sense of relative safety in relation to tuberculosis, with consequent low rates of BCG uptake. Thus low uptake of different immunizations arises from enhanced feelings of both safety and danger. Low uptake was not found to be due to the practical difficulties associated with large families, or to perceived insensitive cultural practices of health care providers.
Conclusions
The views and practices of members of this community are not homogeneous and may change over time. It is important that assumptions concerning the role of religious beliefs do not act as an obstacle for providing clear messages concerning immunization, and community norms may be challenged by explicitly using its social networks to communicate more positive messages about immunization. The study provides a useful example of how social networks may reinforce or challenge misinformation about health and risk and the complex nature of decision making about children's health.
Introduction
Concern about the re-emergence of certain childhood infectious diseases has followed evidence about declining rates of immunization since publicity was given to claims associated with a (now discredited) 1998 study1 of the triple MMR vaccine and autism. During 2003/04, more than two thirds of Primary Care Trusts (PCTs) in England (221 of 294) reported less than 85% coverage for MMR.2 Local variations included 19 PCTs with coverage below 70%, 15 of which were located in London.
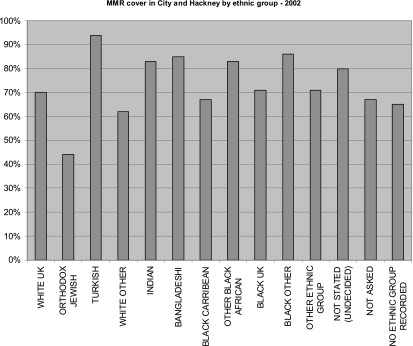
Lower rates of childhood immunization have been found amongst disadvantaged communities3–5 and within certain minority ethnic communities where uptake of preventive health programmes has traditionally been low.6,7 In the City and Hackney area of east London there are exceptionally low rates of immunization amongst the orthodox Jewish community (46% for both diphtheria and MMR), in spite of relatively high rates (80 and 90%) for other ethnic groups in the area and an overall rate of 70% of children aged two being immunized for MMR8 ( Figure 1).
Figure 1.
Population Database: Regional Interactive Child Health System (2002)
Quantitative studies conducted before the MMR media scare found that this community valued immunization but wanted better access to services.9 Perceptions of unsympathetic treatment by practice staff, logistical difficulties associated with large family size and fears of allergic reactions have also been identified as factors in explaining low immunization uptake.10 In relation to BCG immunization, also low in orthodox Jewish groups, explanations have pointed to the perceptions of community members that they are less vulnerable to tuberculosis because of a mutual aid ethos which historically has prevented families experiencing dire poverty, and are safe from infection by ‘outsiders’ because of the enclosed nature of the community.11 The influence of mass media (television, newspapers, magazines and the internet) on attitudes to immunization in this community is assumed to be weak because reluctance to integrate with other ethnic groups leads community members to resist exposure to such media.12 Communicating risk is complex and messages are not received or interpreted in a homogeneous way in the general population,13 yet very little is known about how such messages may be filtered and circulated within minority communities.
Our study investigates whether there are specific religious or ethnic reasons for low uptake of immunization amongst orthodox Jewish families in North East London and explores perceptions of barriers such as larger family size, the role of local health care services, and the significance of wider sources such as local and national media reporting.
Setting
The orthodox Jewish community in North East London is the largest such community in Europe. The 2001 Census14 indicated that 5.3% of Hackney residents are Jewish, although local estimates suggest that the actual figure may be double this, with approximately 20,000 members. The community is largely insular, providing many services for its members. Adhering strictly to Jewish law means that the cost of living for this group is higher than for others. Key factors include the cost of kosher food and the need, for religious reasons, to send children to private Jewish schools. There is also evidence of more domestic overcrowding in the orthodox Jewish population, as families tend to be larger and have more children under 16 in comparison with other groups.15
Good health is regarded extremely highly and it is considered to be a religious obligation to seek medical attention when ill.16 It is not uncommon for serious illnesses to be concealed, particularly hereditary, chronic or mental illness. There are many diverse voluntary groups within the community which provide health and social care services. While local statutory health services are used in times of illness, or where there is a need for hospitalization (particularly maternity), the use of complementary health care facilities and practitioners is growing in popularity. Some health promotion activities are not considered appropriate, such as inviting unmarried women to participate in cervical screening.17
Methods
The orthodox Jewish community is particularly difficult to reach as secular contact is regarded with suspicion. Records of two general practices known to serve a high proportion of the orthodox Jewish community were used to select children aged between 2–3 years. Mothers were contacted by letter and telephone, with researchers emphasizing that the study was independent of their GP and their religious community. A total of 14 women agreed to take part. We also used ‘snowballing’, where participants are asked to suggest others who may take part, and a further 11 women were recruited in this way. This is a common method for qualitative investigations of populations that are otherwise hard to reach or who have limited contact with health professionals and allows us to further examine the social processes which surround health decision making.18,19 There were no significant differences in characteristics between the two groups. Most respondents (20 of 25) were born and had lived in the area all their lives. The mean age of mothers was 29.7 years (range 21–44). Family size varied, with women having between one and nine children (mean 4.1). Most participants (21 of 25) had no additional educational qualifications beyond completing secondary school.
Preliminary background interviews were conducted with ten health care staff who had significant contact with the community through local GP practices and who were either responsible for implementing immunization programmes or may be expected to give advice on this to orthodox Jewish mothers. These included five outreach workers with specific links to the community (e.g. responsible for support in areas including nutrition, mental health, family support and baby clinic); one health visitor; one GP, one Practice Manager; one Practice Nurse; and one receptionist. Members of the research team also met with local Rabbis and discussed the study with GPs and health related community workers to secure approval from religious leaders and to develop a culturally appropriate research design. Ethical approval was awarded by the North East London and The City Research Ethics Sub Committee and the Ethics Committee for the London School of Hygiene and Tropical Medicine. Off Site Hazard and Risk Assessments were completed for the interviewers at the London School of Hygiene and Tropical Medicine.
Semi-structured interviews with orthodox Jewish mothers commenced in May 2003. These were conducted by two female interviewers, as most women were breastfeeding and unable to initiate this in mixed company. It was also important that interviewers were able to build rapport with the participants. For logistical reasons interviews took place in participants' homes – this was easier for the participants, who were commonly looking after more than one pre-school child at home – and a male interviewer could have been an intrusive presence. Interviews were scheduled in line with the religious calendar. Our interview protocol was designed to first collect demographic details, second to explore decisions concerning general health issues, and third to examine beliefs and behaviour concerning immunization ( Table 1). The interview sessions lasted between 25 and 90 minutes and were, with permission, audio-recorded and transcribed fully.
Table 1.
Interview protocol. The interview schedule included both closed and open ended questions in three distinct parts
| Demographics | This part focused on the background details:
|
|---|---|
| Decision making about health | This part focused on ways in which health decisions are routinely made:
|
| Attitudes and beliefs towards childhood immunization | This part addressed specific attitudes and beliefs concerning childhood immunization:
|
Transcripts were read and discussed by members of the team, who marked key passages according to analytical themes. Researchers used some of the principles of grounded theory, developing analytical constructs which were then applied in an iterative manner across the sample allowing us to confirm, reject or modify concepts during the study.20 Responses to key questions were thus cross-tabulated and commonalities and differences were highlighted across all participants and for each immunization (BCG, MMR and DTP [diphtheria, tetanus and pertussis/polio]). This was designed to reflect the complexity of decision making, since it was found that most participants did not statically occupy a ‘pro’ or ‘anti’ position on immunization, varying their views over time and in relation to each kind of immunization. Deviant cases were particularly sought out in order to explore the factors which influenced those participants who did not adhere to community norms. No new themes emerged after analysis of 25 transcripts, which suggests that theoretical saturation had been reached.21
Results
Only one participant had fully immunized all four of her children. The rest indicated that they perceived BCG to be unnecessary, or that they were undecided about the advisability of MMR or the whooping cough element of DTP, or that they would be less likely to immunize their younger children than they had been for the older ones. The difficulty of taking children along to clinics was not raised spontaneously by mothers. Mothers were also asked about their perceptions of local health care services. Negative perceptions were highlighted mainly in relation to restricted practice opening times or having to rearrange appointments because of a sick child. About half of the mothers (13 of 25) said they felt neutral about the local services or thought they were ‘fine’; one wanted to change her GP for personal reasons. Criticisms focused on lengthy waiting times (6 of 25) or complementary medicine being unavailable (4 of 25) rather than staff insensitivity. Just one respondent mentioned that staff could be more culturally aware
‘I just feel that maybe some health visitors should be taught more about Jewish people… make them more aware that we're not offish, we're just very busy.’ (participant 18)
Health professionals were sometimes praised for their sensitive and supportive role:
‘I have a good relationship with my health visitor who is a blessing. You know ‘cause I suffer from manic depression after childbirth so she keeps on visiting me. She's ever so nice, she's really helped me. She does more than her job. She spends a lot of time with me and I appreciate it.’ (participant 2)
Social networks and media influence
It was clear from comments made by both mothers and local health care staff that advice circulated through informal social networks. It appeared that the importance of this was related to the community's relative lack of exposure to mass media sources ( Table 2). Nevertheless, controversies originating in the mass media reached and circulated through these networks, creating anxieties about certain vaccines, thus suggesting only a partial insulation of the community from external influence. Some participants were clearly in more direct touch with the themes of current scares than others, suggested by the following contrasting comments:
‘There is always an anxiety… maybe through bad publicity. You hear little bits of information here and there and it plays on your mind… You know “why didn't Tony Blair give his last one the immunization?”’(participant 8)
‘This [child] hasn't had the MMR yet, the youngest, because of all the scares. The other two [children] had everything.’ (participant 18)
‘I'm hearing so many different things about [the MMR] that I just don't know… there's so much about autism and all these horrible things and measles, mumps and rubella aren't really deathly diseases. I'm kind of leaning towards not doing it.’ (participant 16)
‘Some people have told me that they have caught cancer, I don't know if that is true or not, they say from the immunization of MMR.’ (participant 12)
Table 2.
Informal networks
| Participant 1 | ‘We get more from the community. We just like sort of ask each other. We have friends and then we have these people that help people with health problems and we basically go to them and they more or less know what you should or shouldn't do and everything’ |
|---|---|
| Participant 3 | ‘It's the same as anything, you just ask family and friends’ |
| Participant 8 | ‘We are a close-knit community, even linked to all the orthodox Jewish communities internationally, if something bad happens to someone over in New York, we'll know it in an instant (…) Anything that would happen on that way, we would hear about it soon enough and it would definitely affect people's decisions I think. Things happen and you hear about it’ |
| Participant 16 | ‘The truth is, I'm hearing (about MMR side effects) mostly from friends. I don't really read much papers as I don't have time for any of that. And I don't have the internet, so… I ask friends what they've seen articles about or what they've heard about. I haven't done much research’ |
| Key informant 3, outreach worker | ‘People here don't read newspapers, secular newspapers, they certainly don't have TVs, for the most part they don't listen to the radio. So there's a lack of knowledge about the outside world. So a lot of community learning here is third hand, from someone else which can be great because it's instant but it can also be detrimental because it's like Chinese whispers. You only need one poor child to have been affected (adversely) because of immunization and that will spread around the community’ |
| Key informant 9, outreach worker | ‘It does go by family groupings and then out to friends. It's a very social community. People do interact very much. If lady X says that her child was fine when she was born and it wasn't until after she gave that injection that her child became unwell, that led to a retardation and a disability then everybody gets scared. Everybody thinks “Oh that's a dangerous one to give. I think I'll stay away from it now even though I gave my older ones it”.’ |
| Key informant 1, outreach worker | ‘It's like Chinese whispers, you know, it [a story] can start off as one thing maybe and then it can just blow out of all proportions. Each one adds their own little something! The messages from the professionals, the GPs and the health visitors, are all going out “yes you must, yes you must” but this one will ask her sister “Did you get..?”, “Oh no, I didn't do that”, “Oh well then I'm not going to”. They don't even know why!’ |
Safety
The separation of the community from outside influence led to feelings of safety about tuberculosis and therefore a lack of need for the BCG vaccination, a situation that local health care providers occasionally supported, although this was not done consistently. It was clear that non-uptake of BCG was a long-standing practice in the community, to the extent that it was accorded thestatus of a ‘Jewish belief’ ( Table 3).
Table 3.
Perceptions of BCG
| Participant 9 | ‘The Jewish community don't give it because we don't need the BCG. We don't have anything to do with other ethnic groups. We've only got to do literally with Jewish people. We don't bathe together. We don't have anything to do with them.’ |
|---|---|
| Participant 5 | ‘We (orthodox Jews) don't give it.’ |
| Participant 1 | ‘I don't really know why but I don't know… when I went to my doctor he told me nobody does it so I shouldn't do it basically. What's the reason? I'm not really sure.’ |
| Participant 13 | ‘My mother in law explained it to me and she showed me leaflets. I read about it and decided we're not going to do it, to go with the Jewish belief.’ |
| Participant 3 | ‘(My GP) said “It's very important because we are living with so many different cultures in such a small area”. So I did it but now I think it was a bit of a mistake…’ |
| Participant 16 | ‘I asked my friends and they were like “yeah well, they tell you to do it in Hackney because the area is maybe lower-class, or whatever and this is the sort of thing that may be circulated, but in our circle we don't have it…” The same way we don't have the issue of AIDS.’ |
Danger
MMR and the whooping cough vaccine carried very different connotations, largely involving anxiety about a wide variety of adverse effects, evidence for which came from knowledge of local children within the community believed to have suffered them ( Table 4). In a community concerned more generally with the maintenance of boundaries between itself and the outside world, injections of foreign substances associated with illness had powerful symbolic force:
‘In my head it's like this. I have a healthy child and an immunization is a disease. I am putting the disease in the child. Who knows how good this immunization is? You know all the stories about immunizations and there are bad batches.’ (participant 17)
‘(The belief is that) with immunization you have a healthy child and then you're injecting a foreign something that could change that child. That's what happens with the immunizations. With the other health issues, exercise and… nothing's going to happen to them if they do exercise, or go swimming or… you know what I mean?’ (Key informant 1, outreach worker)
Table 4.
Adverse effects of immunizations (MMR and pertussis)
| Participant 2 | ‘He's not well, maybe a bit Downs Syndrome, but I'm not sure. But he doesn't look well either and the father said that was after the whooping cough (immunization)’ |
|---|---|
| Participant 13 | ‘There's children who have gone into comas, children who have had fits and all sorts. I know a child who fits till now and is on medication’ |
| Participant 3 | ‘I've heard they can make reactions, like making kids go deaf (…) I'm not too clear about it’ |
| Participant 6 | ‘brain damage, I'm not sure’ |
| Participant 10 | ‘There was one case here, a child that contracted polio because he was given MMR, something wrong with the batch or some story and maybe his immune system was a bit low…that was what fuelled doubts.’ |
| Participant 17 | ‘There was a family (…) they had a perfectly normal child who received MMR at age 2 and he subsequently became blind, mentally retarded and deaf. And I think that's a pretty bad reaction! And some people even die.’ |
| Participant 9 | ‘My friend she has a little boy she did give the MMR and he's got inflammation on his brain. She doesn't know if it came from the MMR but she's almost sure it was from that because just the day afterwards it happened.’ |
In the face of such threats, religiously inspired fatalism played an important part in supporting a decision not to immunize:
‘When you don't know what to do, when there's a risk involved both ways, then there's no need to put yourself in the danger of doing one of them. By not doing it (we) trust that God will help you out of these things.’ (participant 13)
‘I feel that if God wants her to get it [an illness] she will get it.’ (participant 4)
Most participants (23 of 25), when asked what came to mind when they heard the term ‘MMR’, linked it with such fears. Two women, though, did not associate this with anxiety and in fact perceived MMR as a routine immunization which they – and, crucially, others in their social networks – gave to their children:
‘Nothing in particular (comes to mind). I knew I had to do it so I just did it.’ (participant 2)
‘Everybody gives it. I've never really worried about (it). I'm happy to give them. Why should (children) suffer basically? If there's something to prevent that? That's basically my decision why I did it… All my friends went and all my sisters (to the clinic for immunizations). It doesn't take long, it doesn't cost any money and why not?’ (participant 1)
These two cases are important because they exemplify that different social norms exist within the same community. Social networks may therefore act as a support or deterrent to immunization for some women.
Discussion
Statement of principal findings
Low rates of immunization in the orthodox Jewish community we studied were not perceived to be due to practical difficulties associated with large families, or to insensitive cultural practices of health care providers. In a community relatively insulated from direct media influence, word of mouth is nevertheless a potent source of rumours about vaccination dangers, whose origin may lie in media scares. Combined with religious fatalism and a more generalized concern about the potential for harm done to the community from outside influence, such rumours succeed in raising vaccination anxieties to high levels. At the same time, the factor of community cohesion (and perhaps religious security) may also explain the relative safety felt in relation to tuberculosis. Paradoxically, in this case feelings of safety led to low BCG immunization rates, as found by other investigators.22
The study identified that individuals in this community have a range of views on these matters. Changes in attitudes over time appear to have occurred, with many families having partially immunized their children, perhaps holding back with younger ones in the light of currently raised levels of anxiety. Additionally, the two cases where women not only immunized their children routinely but also believed that others in their immediate networks did so are of particular interest. Such variability suggests that efforts by local health care providers to influence members of the community, perhaps by feeding positive stories of the benefits of immunization into the informal system for circulating rumour, may be influential.
Strengths and weaknesses of the study
Our sampling from this difficult-to-reach population may be more likely to contain individuals open to contact with ‘outsiders’, something that may be associated with a greater willingness to immunize. In the light of this, the finding that anxieties about MMR were so common is all the more remarkable. The explanations provided by these interviewees for their own behaviour are likely to be helpful in understanding the views of others in the community who did not participate in the study. We were also unable to access those who do not receive Western medicine due to our recruitment from general practices. This is a problem which has been noted in other studies of ethnic minority groups and health beliefs,23 although recent studies have suggested that complementary medicine is not necessarily considered to be an alternative to immunization.24
Implications for clinicians and policy makers
Our findings suggest that it is important to monitor the views and practices of this community over time as these do not remain static. In turn, a better understanding of how and why they change will provide beneficial leads in identifying how health providers may make culturally sensitive interventions. It may be possible to challenge community norms by explicitly using its existing social networks to communicate more positive messages about immunization, though it is important to recognize that this group have information networks that span several countries, including the USA and Israel. During the period May to 18 July 2007 there were a total of 39 cases of measles in Hackney, most of these involving children from the orthodox Jewish community.24 Outbreaks of measles in orthodox Jewish communities in Jerusalem were most likely to involve unvaccinated children, prompting calls for special attention to specific sub-populations.25 Investigations of how different socially situated groups receive and process health information will yield benefits for minority communities and the wider population.
Footnotes
DECLARATIONS —
Competing interests None declared
Funding This study was funded by City and Hackney Teaching Primary Care Trust and held at the London School of Hygiene and Tropical Medicine
Ethical approval Granted by North East London & The City Research Ethics Sub Committee and the Ethics Committee for the London School of Hygiene and Tropical Medicine. In addition to this we completed off-site hazard and risk assessments for Lesley Henderson and Tamar Sutton who conducted the interviews
Guarantor LH
Contributorship LH participated in the design of the study, collected and analysed data and led in the writing of this paper. CM and NT participated in the design of the study, analysed data and participated in writing the paper
Acknowledgements
We would like to thank all of those who agreed to take part in the study. Thanks to Tamar Sutton who was involved in the initial study design and conducted some of the interviews and thanks to Clive Seale for comments on an earlier version of the paper
References
- 1.Wakefield A, Murch S, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998;351:637–41. doi: 10.1016/s0140-6736(97)11096-0. [DOI] [PubMed] [Google Scholar]
- 2.NHS Immunisation Statistics, England: 2003/04. http://www.dh.gov.uk/assetRoot/04/09/95/77/04099577.pdf
- 3.Marsh GN, Channing DM. Comparison in use of health services between a deprived and an endowed community. Arch Dis Child. 1987;62:392–6. doi: 10.1136/adc.62.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jarman B, Bosanquet N, Rice P, Dollimore N, Leese B. Uptake of immunisation in district health authorities in England. BMJ (Clin Res Ed) 1988;296:1775–8. doi: 10.1136/bmj.296.6639.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feder GS, Vaclavik T, Streetly A. Traveller Gypsies and childhood immunization: a study in east London. Br J Gen Pract. 1993;43:281–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Baker MR, Bandaranayake R, Schweiger MS. Differences in rate of uptake of immunisation among ethnic groups. BMJ (Clin Res Ed) 1984;288:1075–8. doi: 10.1136/bmj.288.6423.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhopal RS, Samim AK. Immunization uptake of Glasgow Asian children: paradoxical benefit of communication barriers? Community Med. 1988;10:215–20. doi: 10.1093/oxfordjournals.pubmed.a042409. [DOI] [PubMed] [Google Scholar]
- 8.City & Hackney Primary Care Trust. Regional Interactive Health System. 2002.
- 9.Cuninghame CJ, Charlton CP, Jenkins SM. Immunization uptake and parental perceptions in a strictly orthodox Jewish community in north-east London. J Public Health Med. 1994;16:314–7. [PubMed] [Google Scholar]
- 10.Loewenthal KM, Bradley C. Immunization uptake and doctor's perceptions of uptake in a minority group: implications for interventions. Psychol Health Med. 1996;1:223–30. [Google Scholar]
- 11.Abbott S. Health Visiting and the Orthodox Jewish Community, Report for City and Hackney Primary Care Trust. London: CHPCT; 2002. [Google Scholar]
- 12.Abbott S. Lay and professional views on health visiting in an orthodox Jewish community. Br J Community Nurs. 2004;9:80–5. doi: 10.12968/bjcn.2004.9.2.12424. [DOI] [PubMed] [Google Scholar]
- 13.Bellaby P. Communication and miscommunication of risk: understanding UK parents' attitudes to combined MMR vaccination. BMJ. 2003;327:725–8. doi: 10.1136/bmj.327.7417.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UK 2001 Census. www.statistics.gov.uk/census2001.
- 15.Spitzer J, Hennessy E, Neville L. High group A streptococcal carriage in the orthodox Jewish community of North Hackney. Br J Gen Pract. 2001;51:101–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Dosani S. Caring for Jewish Patients. BMJ. 2003;327:169. [Google Scholar]
- 17.Purdy S, Jones KP, Sherratt M, Fallon PV. Demographic characteristics and primary health care utilization patterns of strictly orthodox Jewish and non-Jewish patients. Fam Pract. 2000;17:233–5. doi: 10.1093/fampra/17.3.233. [DOI] [PubMed] [Google Scholar]
- 18.Arber S. Designing samples. In: Gilbert N, editor. Researching social life. London: Sage; 1993. pp. 68–92. [Google Scholar]
- 19.Lawton J, Naureen A, Hallowell N, Hanna L, Douglas M. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. BMJ. 2005;330:1247. doi: 10.1136/bmj.38460.642789.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green J. Grounded theory and constant comparative method. BMJ. 1998;316:1064–5. [PubMed] [Google Scholar]
- 21.Green J, Thorogood N. Qualitative Methods for Health Research. London: Sage; 2004. [Google Scholar]
- 22.Greenhalgh T, Helman C, Chowdhury M. Health Beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. BMJ. 1998;316:978–83. doi: 10.1136/bmj.316.7136.978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smailbegovic M, Laing G, Bedford H. Why do parents decide against immunization? The effect of health beliefs and health professionals. Child Care Health Dev. 2003;29:303–11. doi: 10.1046/j.1365-2214.2003.00347.x. [DOI] [PubMed] [Google Scholar]
- 24.City and Hackney Teaching Primary Care Trust. Update on Measles Outbreak in Hackney, City and Hackney Teaching Primary Care Trust, Press Information. London: CHPCT; 2007. Jul 18, [Google Scholar]
- 25.Stein- Zamir C, Zentner G, Abramson N, et al. Measles outbreaks affecting children in Jewish ultra-orthodox communities in Jerusalem. Epidemiol Infect. 2008;136:207–14. doi: 10.1017/S095026880700845X. [DOI] [PMC free article] [PubMed] [Google Scholar]