Abstract
Objective
To obtain information about newborn health outcomes among nine subgroups of the Asian population in the United States.
Design
Cross-sectional comparison of outcomes for births to Cambodian-, Chinese-, Filipino-, Indian-, Japanese-, Korean-, Laotian-, Thai-, and Vietnamese-origin mothers, and births to non-Hispanic white mothers. Regression models are used to compare neonatal mortality rates across groups, before and after controlling for a range of risk factors.
Setting
All California births between 1991 and 2001
Participants
2,304,301 newborns
Main Exposure
Racial and ethnic groups
Outcome Measure
Neonatal mortality (death within 28 days of birth)
Results
Unadjusted mortality rates in some Asian-American subgroups are significantly different from rates for non-Hispanic whites (non-Hispanic white rate=2.0 per 1,000 births; Chinese=1.2, Japanese=1.2, Korean=2.7; all p<0.05). For infants of Chinese mothers, observed risk factors explain the differences observed in unadjusted data. For Cambodian, Japanese, Korean, and Thai newborns, differences persist or even widen after risk factors are taken into account. After risk adjustment, infants of Cambodian, Japanese, and Korean mothers have significantly lower neonatal mortality rates than those born to non-Hispanic whites (adjusted OR=0.58 for Cambodian, 0.67 for Japanese, 0.69 for Korean, all p<0.05), and infants of Thai mothers have higher rates (adjusted OR 1.89, p<0.05).
Conclusions
There are significant variations in neonatal mortality between subgroups of the Asian-American population that are not entirely explained by differences in observable risk factors. Efforts to improve clinical care that treat Asian-Americans as a homogeneous group may miss important opportunities for improving infant health in specific sub-groups.
Introduction
Asian-Americans make up a large and growing portion of the U.S. population, but a firm understanding of patterns of care and outcomes among Asian-American newborns remains elusive.1 One important challenge is the potential for variations across the diverse national origin subgroups that make up the larger Asian-American population. In demography and related fields, it is increasingly common to encounter work that distinguishes a dozen or more subgroups that vary substantially in socioeconomic characteristics, cultural norms, and other attributes that could influence health care use and outcomes.2–4 In health care, relying on information about the Asian-American population as a whole when making policy or clinical judgments, or broadly applying information about just one or two subgroups, may miss important distinctions and lead to poorly targeted actions.
A number of existing studies provide useful information about birth outcomes for Asian-Americans.5–25 However, the existing literature provides only limited insight into subgroup variations within this population. Many studies analyzed data from the 1980s, and virtually all of them, particularly those incorporating risk adjustment and stronger analytic methods, have been forced by data constraints or other factors to focus either on the Asian-American population as a whole, or on just the larger subgroups (usually Chinese, Japanese, Filipinos, or Koreans). Differences in study methodology can also make it difficult to compare results across studies.
The primary objective of this paper is to provide a systematic comparison of neonatal mortality rates across many subgroups of the Asian-American population. We study a large dataset from California spanning 1991–2001, and examine nine national-origin subgroups: Cambodian, Chinese, Filipino, Indian, Japanese, Korean, Laotian, Thai, and Vietnamese populations, along with non-Hispanic white newborns. A second objective of this paper is to evaluate the contribution of observable risk factors to variations in neonatal mortality rates across Asian-American subgroups. Developing better information about risk factors could be very helpful in targeting new health improvement efforts for Asian-Americans, but the role of risk factors remains relatively poorly understood, particularly across the many population subgroups.
Data and Methods
Data
We used data from the California Office of Statewide Health Planning and Development (OSHPD), which links vital statistics records (birth and death certificates) with mother’s and infant’s hospital discharge data for more than 99% of in-hospital births in California. We limited our analysis to singleton live births between January 1, 1991 and December 31, 2001, with birth weights between 500g and 5500g and gestational ages of 44 weeks or less, for which a complete linkage of maternal hospitalization, infant hospitalization, and vital statistics data was achieved.
Following the convention of the Centers for Disease Control and Prevention, we classified each birth based on the race and ethnicity of the mother, as reported on the birth certificate. Race and ethnicity data from the birth certificate has been found to be of high quality for these groups.6 Among Asian-American newborns, we included those with any of the nine maternal national origins separately identified on the California birth certificate: Cambodian, Chinese, Filipino, Indian, Japanese, Korean, Laotian, Thai, and Vietnamese. This excluded Asian-American births with unspecified national origin or with other national origins that were not coded separately. We selected all infants born to non-Hispanic white mothers as our reference group. We removed a small number of newborns born with lethal anomalies (anencephaly, cervical spina bifida, autosomal dominant polycystic kidney disease, trisomy 13, and trisomy 18). Finally, we removed cases with missing data for any of the risk adjustment variables we use in the analysis. The final analytic sample contained complete information on a little more than 2.3 million births.
The study was approved by the institutional review board at Stanford University, the California Department of Health and Human Services’ committee for the protection of human subjects, and OSHPD.
Variables
Our main outcome measure was neonatal mortality, defined as death within 28 days of birth and coded using death certificate mortality information. Our main independent variable is race and ethnicity. The risk adjustment models also incorporated additional controls. From birth certificates, we developed measures of maternal age (20 or younger, 21–29, 30 years or older), maternal education (8 years or less, 9–11 years, 12 years or more), maternal nativity (U.S.-born, foreign-born), parity (0, 1–3, 4 or more previous births), time at which prenatal care began (1st or 2nd trimester, 3rd trimester), gender-specific newborn birth weight indicators (500–749g, 750–999g, 1000–1249g, 1250–1499g, 1500–1999g, 2000–2499g, 2500–3999g, 4000–5500g), and newborn gestational age (<28 weeks, 28–32 weeks, 33–35 weeks, 36–37 weeks, 38–42 weeks, 43–44 weeks). From data recorded on the birth certificates, we also created an indicator for the presence of any pregnancy risk factor and an indicator for the presence of any labor and delivery complication. From the hospital discharge data, we coded 49 groups of major anomalies using the diagnosis and procedure codes from the birth and immediate subsequent hospitalizations. These variables include anomalies of the gastrointestinal, genitourinary, central nervous, pulmonary, cardiac, skeletal, and skin systems, chromosomal abnormalities, and other miscellaneous conditions. We grouped these anomalies into four categories (high risk, moderately high risk, moderately low risk, and low risk) based on the relative risk of mortality associated with each. We also created an indicator variable for the presence of any of 11 other medical complications recorded in the delivery discharge record. Some of these are similar to complications recorded on the birth certificates, but including them in models appears to contribute additional explanatory power.26
Analytic Methods
After computing descriptive statistics and conducting bivariate comparisons, we employed individual-level multivariate logistic regression models to examine differences in neonatal mortality in births to Asian-origin and non-Hispanic white mothers, adjusting for various risk factors. We analyzed three model specifications. First, we estimated a model that included only dummy variables for race and ethnicity groups and a linear time trend. This model produces estimates of differences across the subgroups without adjusting for any characteristics of mothers or babies. We then estimated a model in which we included the full set of risk adjusters described above: gender-specific birthweight categories, gestational age, maternal age, maternal education, maternal place of birth, prenatal care start, the presence of pregnancy risk factors, the presence of complications of labor and delivery, and the presence of major anomalies and other complications recorded on hospital discharge records. Finally, since birthweight and gestational age appear to play central roles in newborn survival, we estimated an intermediate risk adjustment model in which we adjusted only for newborn sex, birthweight, and gestational age but did not include the other risk adjusters. Comparing results of the intermediate model to the full risk adjustment model provides information about the contribution of different risk adjusters to the results.
The coefficients on the race and ethnicity variables from each of these models provide information about differences across groups. In each model, non-Hispanic white was the omitted (reference) group, so each odds ratio reflects the difference between neonatal mortality rates in the given group to those for infants born to non-Hispanic white mothers. We computed robust standard errors for each coefficient and calculated Receiver-Operating Characteristic (ROC) curves to assess the goodness-of-fit of the logistic models.27 All analyses were performed using STATA statistical software (version 8.0, STATA Corp, College Station, Texas).
An appendix with further details on data definitions, analytic approaches, and alternate analyses is available from the authors.
Results
Of the 2,304,301 newborns in our data set, 483,246 (21%) were born to Asian-American mothers and the remaining 1,821,055 (79%) to non-Hispanic white mothers. Table 1 reports the number of births by subgroup. Three national origin subgroups – Chinese, Filipino, and Vietnamese – comprise over two-thirds of the Asian-American portion of the sample.
Table 1.
Maternal characteristics by group
| Cambodian | Chinese | Filipino | Indian | Japanese | Korean | Laotian | Thai | Vietmamese | All Asian Americans | Non-Hispanic White | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | |||||||||||
| 20 or younger | 12.5% * | 0.7% * | 5.3% * | 1.0% * | 1.3% * | 1.0% * | 19.0% * | 11.1% * | 3.5% * | 3.6% * | 6.9% |
| 21– 29 | 59.7% | 39.0% | 50.4% | 66.8% | 33.3% | 54.3% | 59.9% | 45.6% | 54.6% | 49.7% | 51.8% |
| 30 or older | 27.9% | 60.3% | 44.3% | 32.2% | 65.5% | 44.7% | 21.0% | 43.3% | 41.9% | 46.7% | 41.3% |
| Education | |||||||||||
| 8 years or less | 39.0% * | 6.0% * | 1.1% * | 2.0% * | 0.3% * | 0.5% * | 34.8% * | 6.9% * | 13.1% * | 6.5% * | 0.9% |
| 9–11 years | 16.5% | 5.9% | 5.2% | 5.3% | 1.3% | 1.5% | 17.8% | 10.4% | 11.6% | 6.6% | 8.9% |
| 12 years or more | 44.6% | 88.1% | 93.7% | 92.6% | 98.5% | 98.0% | 47.5% | 82.8% | 75.2% | 86.9% | 90.2% |
| Nativity | |||||||||||
| U.S. Born | 2.0% * | 10.4% * | 15.1% * | 5.2% * | 48.4% * | 3.3% * | 2.8% * | 4.9% * | 1.1% * | 10.9% * | 89.7% |
| Foreign Born | 98.0% | 89.7% | 84.9% | 94.8% | 51.6% | 96.8% | 97.2% | 95.1% | 99.0% | 89.1% | 10.3% |
| Prenatal Care | |||||||||||
| Start 1st/2nd Trimest. | 97.2% * | 98.5% * | 97.2% * | 98.2% | 99.0% * | 97.5% * | 96.7% * | 97.3% * | 98.1% | 97.9% * | 98.2% |
| Start 3rd Trimester | 2.9% | 1.5% | 2.8% | 1.8% | 1.1% | 2.5% | 3.3% | 2.7% | 1.9% | 2.1% | 1.8% |
| Birth Parity | |||||||||||
| no previous births | 32.6% * | 48.9% * | 43.8% * | 49.1% * | 49.1% * | 47.3% * | 32.6% * | 51.4% * | 45.0% * | 45.7% * | 42.1% |
| 1–3 previous births | 41.9% | 47.6% | 49.0% | 47.0% | 46.8% | 49.5% | 39.4% | 43.8% | 45.1% | 47.2% | 49.0% |
| >3 previous births | 25.6% | 3.4% | 7.3% | 3.9% | 4.0% | 3.2% | 28.0% | 4.8% | 9.9% | 7.1% | 8.9% |
| N | 17,677 | 116,795 | 138,389 | 47,006 | 29,762 | 39,641 | 12,978 | 5,722 | 75,276 | 483,246 | 1,821,055 |
denotes the distribution for the given Asian-American subgroup is significantly different than the distribution for Non-Hispanic Whites, p<0.01.
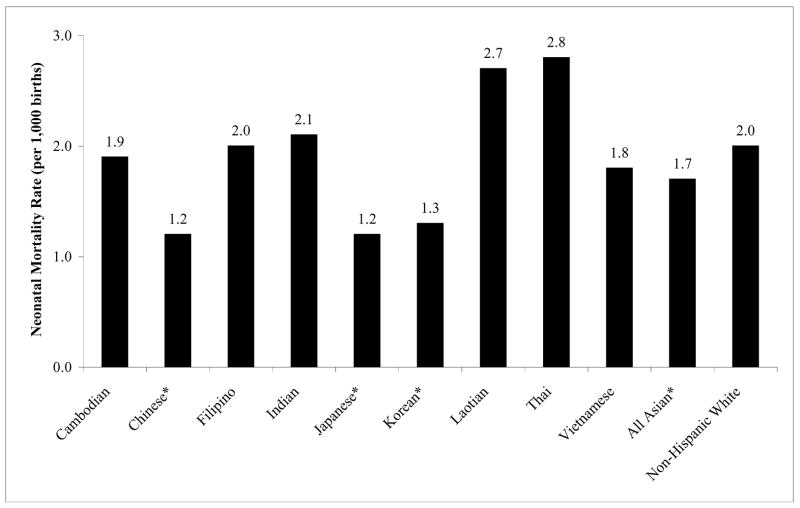
Unadjusted Neonatal Mortality
The unadjusted 28-day mortality rate across all infants is a little over 1.9 per 1000. There are large differences in unadjusted neonatal mortality rates across the subgroups in our sample (Figure 1). Infants born to women of Chinese, Japanese, and Korean national origin have significantly lower unadjusted neonatal mortality rates than infants born to non-Hispanic white women (all P<0.01). Infants born to women of Thai and Laotian national origin have the highest mortality rates. Neonatal mortality rates in these two groups are not significantly different from rates for infants born to non-Hispanic white women, though they are significantly different from rates for infants born to Chinese, Japanese, and Korean women. The neonatal mortality rates for infants born to Cambodian, Filipino, Indian, and Vietnamese women are not statistically different from non-Hispanic whites.
Figure 1.
Unadjusted neonatal mortality rates for Asian-American subgroups and non-Hispanic whites. * denotes groups for whom the unadjusted mortality rate is significantly different from the rate for non-Hispanic whites at the .01 level.
Demographic Characteristics and Risk Factors
Some of the differences in unadjusted neonatal mortality rates shown in Figure 1 may be related to differences in underlying population characteristics. Table 1 summarizes information about maternal characteristics for non-Hispanic whites and the Asian-American subgroups and reports statistical significance from chi-squared tests of the hypothesis that values for each Asian-American subgroup are the same as for non-Hispanic whites.
There is considerable variation in mother’s age across Asian-American subgroups. Mothers of Chinese and Japanese national origin are much more likely to be over 30 years old than non-Hispanic white mothers. Mothers of Cambodian, Laotian, and Thai national origin are much more likely than non-Hispanic white mothers to be under 20 years old. Mothers of Cambodian, Laotian, and Vietnamese national origin have the lowest educational attainment, and mothers of Filipino, Indian, Japanese, and Korean national origin the highest. Cambodian and Laotian mothers also have the highest rate of starting prenatal care in the 3rd trimester and the highest parity.
Table 2 summarizes key characteristics of newborns in our samples. Mean birthweight in each of the Asian-American subgroups is lower than the mean for non-Hispanic whites. Birthweights are highest in births to Chinese and Korean mothers, and lowest for births to Cambodian, Indian, and Laotian mothers. On the other hand, rates of very low birthweight are lower for births to Chinese, Japanese, Korean, and Vietnamese mothers than for births to non-Hispanic whites.
Table 2.
Sex, birthweight, and gestational age by group
| Cambodian | Chinese | Filipino | Indian | Japanese | Korean | Laotian | Thai | Vietnamese | All Asian American | Non-Hispanic White | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Infant Sex | |||||||||||
| Male | 51.1% | 52.1% ** | 52.0% ** | 52.0% * | 51.4% | 51.8% | 51.5% | 51.5% | 51.6% | 51.8% ** | 51.4% |
| Female | 48.9% | 48.0% | 48.0% | 48.0% | 48.7% | 48.2% | 48.5% | 48.5% | 48.4% | 48.2% | 48.6% |
| Birthweight (g) | 3162 ** | 3303 ** | 3241 ** | 3191 ** | 3256 ** | 3348 ** | 3157 ** | 3255 ** | 3215 ** | 3252 ** | 3460 |
| % VLBW[a] | 0.8% ** | 0.4% ** | 0.9% ** | 0.8% ** | 0.5% ** | 0.5% ** | 0.8% ** | 0.7% ** | 0.5% ** | 0.6% ** | 0.6% |
| % LBW[a] | 7.2% ** | 4.1% ** | 6.7% ** | 7.4% ** | 5.1% ** | 3.6% ** | 7.3% ** | 6.0% ** | 5.0% ** | 5.5% ** | 3.9% |
| Gestational Age | |||||||||||
| <28 weeks | 0.6% ** | 0.2% ** | 0.4% ** | 0.4% ** | 0.3% ** | 0.3% ** | 0.6% ** | 0.4% ** | 0.3% ** | 0.3% ** | 0.4% |
| 28–32 weeks | 1.4% | 0.4% | 1.0% | 0.7% | 0.5% | 0.5% | 1.5% | 1.1% | 0.7% | 0.8% | 0.7% |
| 33–35 weeks | 4.9% | 1.6% | 3.1% | 2.3% | 1.6% | 1.5% | 5.0% | 3.3% | 2.5% | 2.5% | 2.0% |
| 36–37 weeks | 9.3% | 4.9% | 7.4% | 5.9% | 5.1% | 4.4% | 8.9% | 8.0% | 6.4% | 6.2% | 5.4% |
| 38–42 weeks | 78.6% | 88.5% | 83.4% | 86.7% | 87.7% | 87.8% | 78.2% | 81.4% | 85.1% | 85.5% | 85.3% |
| 43–44 weeks | 5.2% | 4.4% | 4.7% | 4.1% | 4.7% | 5.5% | 6.0% | 5.8% | 5.0% | 4.7% | 6.3% |
denotes the Asian-American subgroup is significantly different from Non-Hispanic Whites, p<0.05;
denotes p<0.01.
VLBW is very low birthweight (<1,500g); LBW is low birthweight (<2,500g)
Comparing all Asian-American births to non-Hispanic whites, differences in gestational age are small. The rates of term births are similar, but infants born to Asian-American women are less likely to have gestational ages of more than 42 weeks, and correspondingly generally more likely to have gestational ages under 38 weeks. There are noticeable differences across subgroups, with the lowest rates of premature birth for Chinese, Japanese, and Korean national origin women, and the highest rates for Cambodian, Laotian, and Thai women.
Women in all of the Asian-American subgroups have fewer pregnancy risk factors reported on birth certificates than non-Hispanic white women, as well as fewer reported complications coded on the discharge abstracts (Table 3). Women in five of the nine subgroups have fewer complications of labor and delivery reported on birth certificates than non-Hispanic whites. Infants born to women of Chinese, Japanese, Korean, and Filipino national origin also have lower reported prevalence of major anomalies.
Table 3.
Infant risk factors by group
| Cambodian | Chinese | Filipino | Indian | Japanese | Korean | Laotian | Thai | Vietnamese | All Asian American | Non-Hispanic White | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pregnancy Risk Factors[a] | 4.3% ** | 6.7% ** | 9.5% ** | 9.3% ** | 8.0% ** | 4.5% ** | 6.4% ** | 8.4% ** | 5.5% ** | 7.4% ** | 13.0% |
| Complications of Labor or Delivery[b] | 15.4% ** | 17.0% | 18.4% ** | 17.6% | 15.9% ** | 14.0% ** | 17.0% | 18.4% * | 19.3% ** | 17.5% ** | 17.2% |
| Anomalies[c] | |||||||||||
| High Risk | 0.11% | 0.05% ** | 0.08% ** | 0.13% | 0.10% | 0.08% | 0.12% | 0.02% * | 0.09% * | 0.08% ** | 0.11% |
| Moderately High Risk | 0.27% | 0.17% ** | 0.24% | 0.20% | 0.19% | 0.20% | 0.18% | 0.16% | 0.22% | 0.21% ** | 0.24% |
| Moderately Low Risk | 0.35% | 0.34% | 0.45% ** | 0.43% | 0.30% * | 0.29% ** | 0.45% | 0.42% | 0.38% | 0.38% | 0.38% |
| Low Risk | 0.29% | 0.43% ** | 0.41% ** | 0.41% | 0.27% ** | 0.35% | 0.29% | 0.49% | 0.36% | 0.39% * | 0.37% |
| Other Complications[d] | 8.1% ** | 8.5% ** | 10.4% ** | 10.3% ** | 7.6% ** | 8.5% ** | 7.9% ** | 9.8% ** | 7.5% ** | 9.0% ** | 11.4% |
denotes the Asian-American subgroup is significantly different from Non-Hispanic Whites, p<0.05;
denotes p<0.01.
Base on birth certificate data. Includes pregnancy-related hypertension, eclampsia, chronic hypertension, renal disease, anemia, cardiac disease, lung disease, diabetes, Rh sensitization, hemoglobinathy, uterine bleeding, hydraamnios/oligohydramnios, incompetent cervix, herpes, tobacco consumption, previous infant larger than 4000g, and previous pre-term infant
Based on birth certificate data. Includes seizures, cephalopelvic disproportion, breech delivery, precipitous labor, premature placenta rupture, abruption placenta, placenta previa, other excessive bleeding, febrile fetus, moderate to heavy meconium, cord prolapse, fetal distress, and anesthetic complications
anomaly groups are derived from 49 major anomalies identified based on diagnosis and procedure codes from the hospital discharge abstracts. Additional detail available in the appendix.
Based on hospital discharge data. Includes oligohydramnios, placenta hemorrhage, prolapsed cord, premature ruptured membrane, fetal distress, small for gestational age, large for gestational age, hydrops fetalis no isoimmunization, maternal complications, hemolytic disorder, and other high risk maternal conditions
Adjusted Neonatal Mortality
To investigate the importance of risk factors, we estimated a series of regression models that progressively incorporated controls for risk factors (Table 4). These models include indicators for each subgroup and control for time trends. Model 1 includes no risk adjusters. Model 2 adjusts only for gender-specific birthweight distributions and gestational age. Model 3 includes the full set of risk adjusters.
Table 4.
Results from regression analyses
| Model 1: No Risk Adjustment
|
Model 2: Adjust for Sex, Birthweight, and Gestation
|
Model 3: Full Risk Adjustment
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Cambodian | 0.975 | (0.695 – 1.367) | 0.714 | (0.497 – 1.026) | 0.577 | (0.361 – 0.924) |
| Chinese | 0.642 | (0.543 – 0.758) | 0.748 | (0.628 – 0.891) | 0.932 | (0.752 – 1.156) |
| Filipino | 1.018 | (0.900 – 1.151) | 0.759 | (0.663 – 0.870) | 0.835 | (0.696 – 1.003) |
| Indian | 1.115 | (0.913 – 1.363) | 0.865 | (0.698 – 1.073) | 0.940 | (0.720 – 1.226) |
| Japanese | 0.620 | (0.446 – 0.861) | 0.619 | (0.442 – 0.867) | 0.668 | (0.449 – 0.995) |
| Korean | 0.663 | (0.503 – 0.874) | 0.663 | (0.492 – 0.893) | 0.694 | (0.486 – 0.991) |
| Laotian | 1.357 | (0.972 – 1.894) | 1.143 | (0.788 – 1.659) | 0.949 | (0.603 – 1.495) |
| Thai | 1.439 | (0.880 – 2.353) | 1.319 | (0.778 – 2.235) | 1.887 | (1.095 – 3.251) |
| Vietnamese | 0.943 | (0.795 – 1.119) | 0.949 | (0.793 – 1.136) | 1.006 | (0.798 – 1.269) |
Note: Omitted race/ethnicity category is non-Hispanic white. Models also contain additional covariates as described in the text. See the Appendix for full regression results.
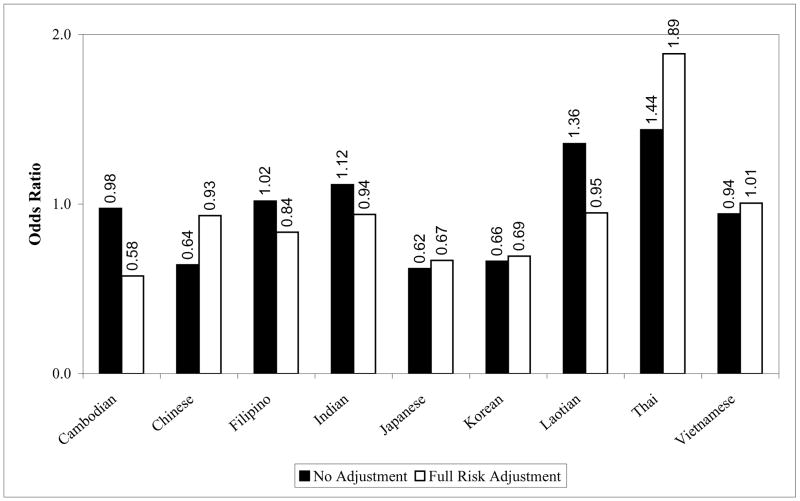
Without any risk adjustment, consistent with the results presented in Figure 1, infants born to women of Chinese, Japanese, and Korean national origin experience significantly lower risks for neonatal mortality compared to infants born to non-Hispanic whites (model 1). Given the relatively rare occurrence of neonatal death, it is reasonable to interpret the odds-ratios as relative risks,28 so we infer that infants born to mothers in these groups have neonatal mortality that is more than 30 percent lower non-Hispanic whites.
Adjusting for the full set of risk factors affects several of the odds ratios (model 3). Infants born to Japanese and Korean mothers continue to have better outcomes than those born to non-Hispanic whites after these adjustments, but outcomes for infants born to Chinese mothers are no longer statistically significantly better. Mortality rates for infants born to Cambodian mothers, who were no different from infants born to non-Hispanic white women before adjustment, are about 40 percent lower once we account for risk factors. Outcomes for infants born to Filipino mothers come very close to being significantly better than those for infants born to non-Hispanic white mothers. Mortality rates for infants born to Thai mothers are about 90 percent higher than for infants born to non-Hispanic white mothers on a risk-adjusted basis. Figure 2 depicts the changes in odds ratios that result from risk adjustment.
Figure 2.
Odds ratios for neonatal mortality for Asian-American subgroups relative to non-Hispanic whites, with no and full risk adjustment
Table 4 also presents results from an intermediate risk adjustment model (model 2), which adjusts only for the sex-specific birthweight distribution and gestational age. In many cases, odds ratios from this model fall in between the unadjusted odds ratio and the fully adjusted odds ratio, indicating that birthweight and gestational age contribute some of the changes in the odds ratios observed, but that other risk adjusters play important roles as well.
Calculated around the non-Hispanic white neonatal mortality rate of 2.0 deaths per 1,000 births, the odds ratios we observe for infants born to mothers of Cambodian, Japanese, and Korean national origin in our fully adjusted model would translate into reductions of 0.9, 0.7, and 0.6 in mortality rates per 1000 births, respectively. On the other hand, the odds ratio for infants born to mothers of Thai national origin would imply a mortality rate per 1,000 births that is higher by 1.8.
We have made all comparisons up to this point between the Asian-American subgroups and non-Hispanic whites. It may also be instructive to examine comparisons between the Asian-American subgroups themselves. Using our fully adjusted model, we find that outcomes for infants born to Thai mothers are statistically significantly worse than outcomes for infants born to mothers in each of the other Asian-American subgroups (P<.05 compared with infants born to Laotian mothers, P<.01 otherwise), but there are no other statistically significant differences when the various Asian-American subgroups are compared to other subgroups.
Discussion
In this large study of California births, we found noticeable variations in neonatal mortality across several Asian-American subgroups. In particular, after adjusting for a range of factors, we found significantly lower neonatal mortality rates for infants born to mothers of Cambodian, Japanese, and Korean national origin compared to infants born to non-Hispanic white mothers, and significantly higher rates for infants born to mothers of Thai national origin.
We also found that patterns of mortality rates are somewhat different in analyses that do and do not adjust for risk factors, suggesting that variations in risk factors plays an important role in variations in mortality rates for some of the groups. There are three general patterns in the results. First, in two subgroups, controlling for maternal and infant characteristics and risk factors results in more favorable comparisons with non-Hispanic whites. This is seen most strongly in births to Cambodian women, for whom outcomes are similar to non-Hispanic whites before risk factors are considered, but outcomes on a risk adjusted basis are much better than for non-Hispanic whites. A similar pattern is observed for births to Filipino mothers, though they end up just short of statistically significantly different from non-Hispanic whites in the fully risk adjusted model. For births in these subgroups, levels of the maternal and infant characteristics and risk factors that we measure appear to be disadvantageous relative to non-Hispanic whites, so that taking these factors into account improves the comparison with non-Hispanic whites.
Second, in two subgroups, controlling for maternal and infant characteristics and risk factors results in less favorable comparisons with non-Hispanic whites. For births to Chinese mothers, outcomes are statistically significantly better than for non-Hispanic whites before adjusting for risk factors, but when risk factors are taken into account there is no significant difference. This pattern is also observed for births to Thai women, where outcomes are somewhat worse than outcomes for births to non-Hispanic white mothers on an unadjusted basis (though not statistically significantly so) but outcomes on a risk-adjusted basis are significantly worse. This pattern of change suggests newborn and maternal characteristics that give an advantage relative to non-Hispanic whites. Once these advantages are controlled for, outcomes compare less favorably with non-Hispanic whites.
The third pattern is no change after adjusting for risk factors. For births to Japanese and Korean mothers, outcomes are better than for non-Hispanic whites before risk adjustment, and they remain better after risk adjustment, with relatively little change in the mortality odds ratios when risk adjustment is used. Among infants born to Indian, Vietnamese, and Laotian mothers, mortality rates are not significantly different from non-Hispanic whites before risk adjustment and they remain insignificantly different after risk adjustment. This pattern implies risk factors that are functionally similar in these subgroups and non-Hispanic whites.
The fact that some groups end up better off or worse off than non-Hispanic whites after risk adjustment is used can also provide useful information about the net effect of risk factors. Outcomes for births to Cambodian, Japanese, and Korean women are better than non-Hispanic whites on a risk adjusted basis. One implication of this is that there are other factors that contribute to better outcomes that both differ from non-Hispanic whites and are not among the set of variables that we measure. Outcomes for births to Thai mothers are worse, with the implication that they suffer from other factors that are unobserved, different from non-Hispanic whites, and contribute to worse outcomes.
We believe these results underscore the importance of expanding discussion of health care and outcomes for Asian-American newborns to include greater consideration of the diverse set of national origin subgroups. Efforts to improve clinical care that treat Asian-Americans as a homogeneous group may miss important opportunities for improving infant health in specific subgroups. In some of these subgroups, for example births to Cambodian and Filipino mother, a promising area for improvements might be to focus on reducing the incidence of risk factors. For births to Thai women, understanding the factors that drive worse outcomes on a risk adjusted basis would be important. In other subgroups, the risk factors that we can observe appear to already be generally comparable to other groups, and further investigation may be required to identify areas for potential action. Benefits could perhaps be obtained by studying of the causes of better outcomes for births to Japanese and Korean women.
This study used data on births in California. California has a large Asian-American population, and thus provides a valuable setting for study – public use data from the Census Bureau report that Asian-Americans make up nearly 13% of the state’s residents and about one third of the Asian-Americans in the U.S. reside in California. While undoubtedly not completely representative of Asian-Americans residing elsewhere, Asian-Americans in California as a group are statistically similar in many respects to other Asian-Americans according to 2004 data from the U.S. Census Bureau. Asian-Americans in California have a poverty rate very similar to that of Asian-Americans elsewhere (12%), though the percentage in households with incomes over $100,000 is slightly higher in California than elsewhere (26% vs. 22%). Education rates are similar, with 47% of California Asian-Americans holding a bachelors or graduate degree, compared with 49% of non-California Asian-Americans. 34% of California Asian-Americans were born in the U.S., as opposed to 32% of non-California Asian-Americans.
This study relied on administrative data which do not capture all aspects of care or health status. Further study with more detailed data sets that could capture other risk factors may contribute further valuable insights. Further explorations will also be needed to consider other potentially important interactions, such as the extent to which place of birth is related to the results we find for race and ethnicity. Most of the Asian-American mothers in our sample were born outside of the U.S., and so patterns may change as the U.S.-born Asian-American population grows.
The data used here include cases where birth certificates can be matched to discharge data records. This excludes out-of-hospital births, along with a small number of unlinkable inhospital births. Some of the Asian-American subgroups we study may have higher rates of out-of-hospital births than others, and some evidence suggests that out of hospital births have higher mortality rates than in-hospital births.29 Our results would not capture these patterns. The results also apply to cases where complete data could be obtained on the risk adjustment variables of interest. This affects a small number of cases, but patterns of missing data may vary by race and ethnicity, and cases with missing data in these fields do have disproportionately high mortality rates.
Significant advances in understanding of birth patterns in this group nationwide will likely require additional, more detailed, data. Many current data sources do not provide sufficient information about Asian-American subgroups. Currently, only Chinese, Filipino, and Japanese national origin are separately identified on the standard U.S. birth certificate. Further work with nationally representative datasets would clearly be valuable if the data to support such analysis were to become available.
Acknowledgments
We acknowledge support from the National Institute of Child Health and Human Development, 5R01HD44003. The authors had full access to all the data used in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Ghosh C. Healthy People 2010 and Asian Americans/Pacific Islanders: defining a baseline of information. American Journal of Public Health. 2003;93(12):2093–2098. doi: 10.2105/ajph.93.12.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Diverse Face of Asians and Pacific Islanders in California. Los Angeles, CA: Asian Pacific American Legal Center; 2005. [Google Scholar]
- 3.We the People: Asians in the United States. U.S. Census Bureau; 2004. CENSR-17. [Google Scholar]
- 4.Barnes JS, Bennett CE. The Asian Population: 2000. Washington DC: U.S. Census Bureau; Feb, 2002. [Google Scholar]
- 5.Alexander GR, Mor JM, Kogan MD, Leland NL, Kieffer E. Pregnancy outcomes of US-born and foreign-born Japanese Americans. American Journal of Public Health. 1996;86(6):820–824. doi: 10.2105/ajph.86.6.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baumeister L, Marchi K, Pearl M, Williams R, Braveman P. The validity of information on “race” and “Hispanic ethnicity” in California birth certificate data. Health Serv Res. 2000;35(4):869–883. [PMC free article] [PubMed] [Google Scholar]
- 7.Fuentes-Afflick E, Hessol NA. Impact of Asian ethnicity and national origin on infant birth weight. American Journal of Epidemiology. 1997;145(2):148–155. doi: 10.1093/oxfordjournals.aje.a009085. [DOI] [PubMed] [Google Scholar]
- 8.Fuentes-Afflick E, Hessol NA, Perez-Stable EJ. Maternal birthplace, ethnicity, and low birth weight in California. Archives of Pediatric and Adolescent Medicine. 1998;152(11):1105–1112. doi: 10.1001/archpedi.152.11.1105. [DOI] [PubMed] [Google Scholar]
- 9.Gann P, Nghiem L, Warner S. Pregnancy characteristics and outcomes of Cambodian refugees. American Journal of Public Health. 1989;79(9):1251–1257. doi: 10.2105/ajph.79.9.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gould JB, Madan A, Qin C, Chavez G. Perinatal outcomes in two dissimilar immigrant populations in the United States: a dual epidemiologic paradox. Pediatrics. 2003;111(6–1):676–682. doi: 10.1542/peds.111.6.e676. [DOI] [PubMed] [Google Scholar]
- 11.Kleinman JC. Infant mortality among racial/ethnic minority groups, 1983–1984. Mortality and Morbidity Weekly Report, CDC Surveillance Summary. 1990;39(3):31–39. [PubMed] [Google Scholar]
- 12.Madan A, Holland S, Humbert JE, Benitz WE. Racial differences in birth weight of term infants in a northern California population. Journal of Perinatology. 2002;22(3):230–235. doi: 10.1038/sj.jp.7210703. [DOI] [PubMed] [Google Scholar]
- 13.Matthews TJ, Menacker F, MacDorman MF. Infant mortality statistics from the 2001 period linked birth/infant death data set. National Vital Statistics Reports. 2003;52(2):1–27. [PubMed] [Google Scholar]
- 14.Mor JM, Alexander GR, Kieffer EC, Baruffi G. Birth outcomes of Korean women in Hawaii. Public Health Report. 1993;108(4):500–505. [PMC free article] [PubMed] [Google Scholar]
- 15.Mor JM, Alexander GR, Kogan MD, Kieffer EC, Ichiho HM. Similarities and disparities in maternal risk and birth outcomes of white and Japanese-American mothers. Pediatric Perinatal Epidemiology. 1995;9(1):59–73. doi: 10.1111/j.1365-3016.1995.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 16.Morrow HW, Chavez GF, Giannoni PP, Shah RS. Infant mortality and related risk factors among Asian Americans. American Journal of Public Health. 1994;84(9):1497–1500. doi: 10.2105/ajph.84.9.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel D, Patel U, Piotrowski ZH, Nelson M. Maternal and paternal risk factors and birth outcomes among Asian and Pacific Islanders in Illinois. Asian American and Pacific Islander Journal of Health. 1995;3(1):42–51. [PubMed] [Google Scholar]
- 18.Singh GK, Yu SM. Pregnancy Outcomes among Asian Americans. Asian American and Pacific Islander Journal of Health. 1993;1(1):63–78. [PubMed] [Google Scholar]
- 19.Singh GK, Yu SM. Birthweight differentials among Asian Americans. American Journal of Public Health. 1994;84(9):1444–1449. doi: 10.2105/ajph.84.9.1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh GK, Yu SM. Adverse Pregnancy Outcomes: Differences between US- and foreign-born women in major US racial and ethnic groups. American Journal of Public Health. 1996;86(6):837–843. doi: 10.2105/ajph.86.6.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang X, Strobino DM, Guyer B. Differences in cause-specific infant mortality among Chinese, Japanese and white Americans. American Journal of Epidemiology. 1992;135(12):1382–1393. doi: 10.1093/oxfordjournals.aje.a116249. [DOI] [PubMed] [Google Scholar]
- 22.Weeks JR, Rumbaut RG. Infant mortality among ethnic immigrant groups. Social Science & Medicine. 1991;33(3):327–334. doi: 10.1016/0277-9536(91)90367-l. [DOI] [PubMed] [Google Scholar]
- 23.Le LT, Kiely JL, Schoendork KC. Birthweight outcomes among Asian American and Pacific Islander subgroups in the United States. International Journal of Epidemiology. 1996;25(5):973–979. doi: 10.1093/ije/25.5.973. [DOI] [PubMed] [Google Scholar]
- 24.Shiono PH, Klebanoff MA, Graubard BI, Berendes HW, Rhoads GG. Birth weight among women of different ethnic groups. Journal of the American Medical Association. 1986;255(1):48–52. [PubMed] [Google Scholar]
- 25.Yu SM, Alexander GR, Schwalber R, Kogan MD. Prenatal care use among selected Asian American groups. American Journal of Public Health. 2001;91(11):1865–1868. doi: 10.2105/ajph.91.11.1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phibbs C, Bronstein J, Buxton E, Phibbs R. The Effects of Patient Volume and Level of Care on Neonatal Mortality. Journal of the American Medical Association. 1996;276:1054–1059. [PubMed] [Google Scholar]
- 27.Hosmer D, Lemeshow S. Applied Logistic Regression. New York, NY: Wiley; 1989. [Google Scholar]
- 28.Zhang J, Yu KF. What’s the Relative Risk?: A Method of Correcting the Odds Ratio in Cohort Studies of Common Outcomes. Journal of the American Medical Association. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 29.Pang JW, Heffelfinger JD, Huang GJ, Benedetti TJ, Weiss NS. Outcomes of planned home births in Washington State: 1989–1996. Obstetrics & Gynecology. 2002;100:253–259. doi: 10.1016/s0029-7844(02)02074-4. [DOI] [PubMed] [Google Scholar]