Abstract
We examined the association between exposure to the California Tobacco Control Program and tobacco-related behaviors and perceptions among adults of Mexican descent. Three cross-sectional population-based surveys were conducted among adults in cities that represent full, partial, and no exposure to the program: San Diego, Calif, Tijuana, Mexico, and Guadalajara, Mexico, respectively.
After we controlled for socioeconomic differences, we found significantly different rates of smoking, exposure to environmental tobacco smoke, and smoking bans in the 3 cities. We also observed a parallel gradient of cross-city differences in theoretical mediators of tobacco control. This suggests a significant association among the California Tobacco Control Program, tobacco-control outcomes, and theoretical mediators of these outcomes.
Similar programs should be implemented in other regions; they have widespread effects on social norms and behaviors related to smoking and environmental tobacco smoke and can help achieve tobacco control across nations.
Tobacco use is one of the leading preventable causes of death in the United States1 and the world.2 In contrast with the improvements observed in high-income countries, smoking rates and related mortality are increasing in poor- and middle-income nations.3 International research on tobacco control and policies is crucial to expand the progress achieved in high-income countries to less-affluent regions of the world.4 This research can be strengthened with the use of comprehensive health behavior models.
The Behavioral Ecological Model (BEM)5 provides a strong foundation for the identification of determinants of health behaviors and has been applied to different health research areas.6–10 The BEM represents an extension of the operant learning principles11 and the theory of social learning,12 with emphasis on the role of reinforcement and modeling processes.5 This model posits that behaviors are determined by a hierarchy of determinants, including individual characteristics, the proximal social network, community-level factors, and the broader social and cultural context. Some factors are highly idiosyncratic (e.g., personal history of reinforcement), whereas others apply to large groups of individuals (e.g., policies, social norms, culture). Bidirectional influences operate between factors that belong to different levels of this hierarchy. Because of their consistent and generic influence,5 social norms and cultural factors are among the most powerful determinants of health behaviors. Laws, regulations, and public policies affect other levels of influence, leading, for instance, to changes in social norms, community sentiments, and individual attitudes and behaviors.
The California Tobacco Control Program’s (CTCP’s) comprehensive and policy-oriented tobacco-control efforts are consistent with the BEM. This program encompasses smokefree laws, tobacco taxation, restrictions in tobacco advertising and promotion, community involvement, media campaigns, and cessation services. Since its inception in 1988, this program has resulted in a shift in tobacco use and public attitudes toward tobacco and environmental tobacco smoke among California residents.13
The scope of the CTCP contrasts with the level of tobacco-control efforts of neighboring Mexico. Measures of economic nature, such as increasing tobacco taxes to reduce smoking, have only been partially used in Mexico.14 Moreover, advertising of tobacco in public venues is still permitted, sponsorship of events and use of promotional tobacco-related items is legal and widespread, and enforcement of bans on tobacco sales to minors is limited.15,16
Previous research in the United States has examined the association between state- and local-level tobacco-control policies and rates of tobacco use,17,18 exposure to environmental tobacco smoke,19 and smoking bans.20 We extend this work by examining the differences in tobacco use, exposure to environmental tobacco smoke, and related behaviors and perceptions among 3 populations of Mexican-descent adults who represented 3 different levels of exposure to tobacco-control policies: those who lived in a California city (i.e., San Diego, Calif), those who lived in a Mexican city located on the California–Mexico border (i.e., Tijuana, Baja California, Mexico), and those who lived in another Mexican city far away from California (i.e., Guadalajara, Jalisco, Mexico).
We hypothesized that, because of their exposure to the CTCP, adults of Mexican descent in San Diego would exhibit lower smoking rates, less exposure to environmental tobacco smoke, and a more negative perception of tobacco than their counterparts in Mexico. Moreover, because of exposure to California antitobacco media, social interactions with California residents, and exposure to smokefree public policies when traveling into California, we hypothesized that adults who lived in the Mexican border city of Ti-juana would experience some of the benefits of the CTCP. This would translate into lower rates of smoking, less exposure to environmental tobacco smoke, and more negative views on tobacco use among Tijuana residents compared with those in other Mexican cities located farther from California.
By testing this hypothesis, we sought to add to previous literature and further our understanding of how exposure to different tobacco-related policies was associated with differential tobacco use and environmental tobacco smoke. To our knowledge, this was the first study on this topic that involved an international comparison. The results may inform the widespread effects of comprehensive antitobacco programs, such as the CTCP, on social norms and behaviors related to smoking and environmental tobacco smoke and contribute to the expansion of this type of tobacco-control intervention to other regions of the world.
METHODS
Design and Study Sample
From 2003 to 2004, we conducted a cross-sectional survey in San Diego, Tijuana, and Guadalajara. These cities were purposefully selected to represent different levels of exposure to the CTCP, thus allowing us to explore the association between exposure to the CTCP and smoking, exposure to environmental tobacco smoke, smoking bans, history of tobacco-related diseases, and related perceptions.
Selection of study sites.
San Diego and Ti-juana are adjacent cities located at opposite sides of the California–Mexico border. San Diego (population 1 305 736) is located in California and fully exposed to the CTCP. Ti-juana (population 1 210 820) is located on the Mexican side of the California–Mexico border. Tijuana’s proximity to California makes it unique compared with other large Mexican border towns. Tijuana and San Diego share one of the busiest international borders in the world21 and nearly all border crossers (96%) are residents of either of the 2 cities.22 Through shared media, travel to California, and frequent interaction with California residents, Tijuana residents are partially exposed to the influence of the CTCP.
By contrast, Guadalajara (population 1 646 319) is located in western central Mexico, more than 1400 miles from the Mexico–California border. Residents of Guadalajara, although exposed to virtually the same tobacco-related policies as Tijuana residents, have no exposure to California media or residents from whom tobacco-control practices and attitudes might be acquired. The 3 cities are located in states that represent a continuum in the migration phenomenon between Mexico and the United States. Guadalajara represents a sending community,23 Tijuana an intermediate and often definite destination,24 and San Diego the receiving community for many individuals who migrate from Mexico to the United States.25–28
Sampling and recruitment procedures.
In San Diego, a telephone survey was conducted with a population-based sample of Mexican-descent adults. In 1999, the amount of Latino households with telephones in California exceeded 94%.29 We obtained residential telephone numbers from a vendor and selected them through stratified random sampling procedures, with as many strata as number of zip codes in San Diego. Trained interviewers called selected phone numbers and determined the eligibility of the household residents. Residents were eligible if they were 18 years or older, spoke English or Spanish, and self-identified as of Mexican descent. The eligible resident with the most recent birthday was selected to complete the interview. Up to 6 calls per phone number were made to make an initial contact with each targeted household, followed by up to 10 subsequent attempts to complete the interview with eligible target individuals. Nonresponses were replaced by newly randomly selected phone numbers. Interviews were administered by trained interviewers in English or Spanish, according to the participant’s preference.
Given the lower percentage of households with telephones in Tijuana and Guadalajara (57%–64%),30 a door-to-door household survey was conducted. A multistage, probability sampling design was used, with census tracts, city blocks, and households as sampling units. In each city, 80 census tracts, a block within each tract, and 5 households within each block were randomly selected. The resident adult with the most recent birthday was selected to participate in the survey. Up to 4 visits were made to each selected household to contact targeted respondents, followed by up to 10 subsequent visits to complete the survey with contacted respondents. Nonresponses were replaced by newly selected households by following a systematic replacement algorithm. Most interviews (90%) were conducted face to face, with 10% being conducted by telephone for cross-methods comparison purposes.
Response rates were 41%, 59%, and 64% in San Diego, Tijuana, and Guadalajara, respectively. Cooperation rates, defined as the number of completed interviews divided by the number of eligible individuals who were contacted, were 58%, 65%, and 69% in San Diego, Tijuana, and Guadalajara, respectively.
Sample characteristics.
Targeted numbers of participants were 1100 San Diego Mexican-descent adults and 400 adult residents in each Mexican city. Number sizes were set to provide prevalence estimates on smoking, environmental tobacco smoke exposure, and bans with reasonable precision levels for the 3 cities (i.e., 95% confidence intervals of ±3 and ±5 for the San Diego and Mexican samples, respectively). Final samples included 1103 Mexican-descent Americans who lived in San Diego, 398 Mexicans who lived in Ti-juana, and 400 Mexicans who lived in Guadalajara. Table 1 ▶ shows the sociodemographic characteristics of the 3 study samples. The profile of the 3 samples was similar to that of the reference populations, according to the 2000 census data from the United States31 and Mexico.30
TABLE 1—
Sample and Population Sociodemographic Characteristics of Mexican Descendents (N=1901): San Diego, Calif; Tijuana, Mexico; and Guadalajara, Mexico, 2003–2004
| San Diego | Tijuana | Guadalajara | ||||
| Sample | Populationa | Sample | Populationb | Sample | Populationb | |
| Total, No. | 1103 | 398 | 400 | |||
| Male gender, % | 47.9 | 48.6 | 46.9 | 49.8 | 49.9 | 46.2 |
| Mean age, y (SD) | 40.9 (15.6) | 37.0 (14.9) | 38.4 (15.0) | 35.7 (14.4) | 38.1 (16.5) | 39.1 (16.7) |
| High school or higher level of education, % | 45.4 | 41.6 | 35.2 | 36.3 | 56.7 | 40.1 |
| Married or cohabitating, % | 62.8 | 56.3 | 61.4 | 66.1 | 51.6 | 58.9 |
| Employment status, % | ||||||
| Employed full or part time | 53.8 | 57.1 | 56.5 | 62.8 | 51.5 | 59.2 |
| Student | 10.3 | 11.0 | 3.8 | 2.4 | 14.8 | 3.6 |
| Other | 36.0 | 33.0 | 39.7 | 34.9 | 33.8 | 27.1 |
| Foreign born, % | 76.2 | 62.4 | 2.8 | 1.6 | 1.5 | 0.5 |
Measures
Smoking and exposure to environmental tobacco smoke.
Most measures on smoking, environmental tobacco smoke exposure, and smoking bans were adapted from the California Tobacco Survey32 and the National Health Interview Survey.33 Measures were then translated to Spanish by bilingual, bicultural researchers and pilot tested for equivalence. For the Mexican surveys, we worked with researchers from Tijuana and Guadalajara to modify the Spanish version of the San Diego questionnaire and adapt it to the local dialect of these cities.
Respondents were classified as “current smokers” if they reported ever having smoked 100 cigarettes and at the time of the survey smoked some days or every day. To measure exposure to environmental tobacco smoke, 3 dichotomous variables were generated to represent daily exposure in the home, the work-place, and anywhere based on reported indoor exposure to other people’s cigarettes on a typical day. With regard to smoking bans, respondents who reported that smoking was completely banned (vs partially banned or allowed) inside their homes and workplaces were classified as having a smokefree policy in the home and workplace, respectively.
History of tobacco-related disease.
Respondents with a reported history of 1 or more tobacco-related diseases were classified as having a lifetime history of tobacco-related disease. Tobacco-related diseases included heart disease, lung cancer, other cancers, emphysema, bronchitis, pneumonia, asthma, shortness of breath, chronic obstructive pulmonary disease, other respiratory problems, high blood pressure, or otitis media.
Theoretical mediators of tobacco control.
The survey included measures on perceptions of mediators of the tobacco-control effects of the CTCP, based on the BEM. Ordinal scales were collapsed into dichotomous variables, with 1 representing the desirable category from a tobacco-control perspective (i.e., greatest antitobacco attitude or perception) and 0 representing any of the remaining categories.
Reported social criticism toward smoking was measured with 5 items that asked participants to rate the likelihood (very likely vs not likely at all or somewhat likely) of being criticized for smoking inside different venues (Table 2 ▶). To assess social norms, 3 survey items asked whether spouses or partners (yes vs no), and family members and friends (most vs some or none) tolerated smoking from others. Perceptions of immediate access to cigarettes were assessed on the basis of reported time it takes to get from the respondent’s home to the nearest tobacco-selling point (more than 1 minute vs 1 minute or less). To assess prevention and cessation programs, respondents were asked whether they had ever participated in a tobacco-prevention program and whether they were aware of free cessation programs in their communities.
TABLE 2—
Standardized Prevalence Rates and 95% Confidence Intervals (CIs) of Theoretical Mediators of Smoking, Exposure to Environmental Tobacco Smoke, and Smoking Bans, Among Mexican Descendents (N = 1901), by City: San Diego, Calif; Tijuana, Mexico; and Guadalajara, Mexico, 2003–2004
| San Diego, % (95% CI) | Tijuana, % (95% CI) | Guadalajara, % (95% CI) | |
| Social criticism for smoking inside public places very likely | |||
| Workplace | 72.4 (69.8, 75.1) | 52.5 (47.6, 57.5) | 47.8 (42.8, 52.8) |
| Restaurants | 70.2 (67.5, 73.0) | 47.0 (42.0, 51.9) | 32.0 (27.3, 36.7) |
| Public transportation | 84.7 (82.6, 86.9) | 68.9 (64.3, 73.5) | 65.9 (61.2, 70.7) |
| Schools | 87.8 (85.8, 89.7) | 70.9 (66.3, 75.4) | 64.6 (59.8, 69.4) |
| Health centers and hospitals | 92.5 (91.0, 94.1) | 87.3 (84.0, 90.6) | 93.4 (90.9, 95.9) |
| Intolerance toward smoking from normative group | |||
| Spouse | 65.4 (61.9, 68.9) | 57.0 (51.0, 63.1) | 41.7 (35.6, 47.9) |
| Most family members | 34.3 (31.4, 37.2) | 22.7 (18.6, 26.9) | 18.7 (14.8, 22.6) |
| Most friends | 21.2 (18.7, 23.7) | 13.2 (9.84, 16.6) | 5.38 (3.11, 7.65) |
| Perceived access to nearest tobacco selling point > 1 minute away from home | 89.2 (87.3, 91.0) | 79.2 (75.1, 83.2) | 66.4 (61.7, 71.1) |
| Participation in tobacco prevention and awareness of free, local cessation programs | |||
| Education | 13.7 (11.6, 15.7) | 6.79 (4.29, 9.29) | 5.91 (3.56, 8.26) |
| Cessation | 76.4 (73.9, 79.0) | 59.3 (54.4, 64.2) | 58.0 (53.1, 62.9) |
| Reported density of smoke-free public places | |||
| All workplaces | 19.9 (17.5, 22.3) | 9.69 (6.71, 12.7) | 8.00 (5.29, 10.7) |
| All restaurants | 34.3 (31.5, 37.2) | 9.25 (6.34, 12.2) | 6.52 (4.04, 9.01) |
| All public transportation | 68.3 (65.4, 71.1) | 43.5 (38.5, 48.6) | 48.4 (43.3, 53.4) |
| All schools | 75.2 (72.6, 77.8) | 67.4 (62.7, 72.1) | 48.4 (43.3, 53.4) |
| All health centers and hospitals | 80.1 (77.7, 82.5) | 77.6 (73.4, 81.7) | 77.1 (72.9, 81.2) |
| Reported legislation banning smoking inside public places | |||
| Workplaces | 35.9 (32.9, 38.8) | 22.2 (18.0, 26.4) | 19.3 (15.4, 23.3) |
| Restaurants | 46.8 (43.7, 49.8) | 21.9 (17.8, 26.1) | 14.2 (10.7, 17.7) |
| Public transportation | 90.8 (89.1, 92.6) | 78.4 (74.2, 82.5) | 84.9 (81.3, 88.5) |
| Schools | 87.5 (85.5, 89.5) | 82.7 (78.9, 86.5) | 76.5 (72.2, 80.7) |
| Health centers and hospitals | 86.5 (84.4, 88.6) | 87.2 (83.8, 90.5) | 87.4 (84.1, 90.7) |
| High support for smoke-free legislation for public places | |||
| Workplaces | 88.7 (86.8, 90.6) | 85.5 (82.0, 89.0) | 79.2 (75.1, 83.2) |
| Restaurants | 90.1 (88.3, 91.9) | 79.3 (75.2, 83.3) | 65.9 (61.2, 70.6) |
| Public transportation | 93.0 (91.5, 94.5) | 90.6 (87.7, 93.5) | 88.5 (85.3, 91.7) |
| Schools | 95.2 (94.0, 96.5) | 93.7 (91.2, 96.1) | 88.4 (85.2, 91.6) |
| Health centers and hospitals | 95.8 (94.6, 97.0) | 95.6 (93.6, 97.6) | 95.6 (93.5, 97.6) |
| Average SOMERSTOL composite score | 69.1 (68.3, 69.9) | 58.2 (56.8, 59.6) | 53.7 (52.3, 55.0) |
Note. SOMERSTOL = Scale of Theoretical Mediators of Tobacco Control.
With regard to perceived smokefree legislation and public policies, 5 survey items asked participants what the laws were on smoking in 5 different public places (Table 2 ▶). Data were subsequently recoded (smoking is completely banned vs smoking is allowed in certain areas or everywhere). Respondents were also surveyed with regard to the proportion of different public places that were smokefree in their city of residence (all vs not all are smokefree). To assess attitudes about smoke-free legislation, participants also were classified according to their degree of support (a lot vs some or no support at all) for laws that banned smoking in various public places.
Scale of theoretical mediators of tobacco control.
A composite scale, called SOMERSTOL, was created using the theoretical mediators of tobacco control described previously and listed in Table 2 ▶. The score on this scale was computed on the basis of the percentage of these mediators for which a participant’s response was coded as 1 (mean=63.9; SD=15.3; range = 16–96.2; Cronbach’s α = 0.76). Higher scores indicated greater levels of reported antitobacco social norms, regulations, and services in the community of residence. The construct validity of the scale was supported by both theoretical and empirical considerations. From a theoretical perspective, the scale items were designed to represent the different spheres of influence proposed by the BEM. Empirically, total scores on SOMERSTOL were significantly associated with smoking status (t = −3.13; df = 1830; P = .002), exposure to environmental tobacco smoke (t = −11.90; df = 1825; P < .001), and smoking bans in the home (t=13.23; df=1830; P<.001) and the workplace (t=7.93; df=7.69; P = .001). On average, participants who were nonsmokers, reported no exposure to environmental tobacco smoke, lived in a smoke-free home, or worked in a smoke-free work-place scored significantly higher in this scale.
Additional items were included to assess other health-related practices that were not expected to be related to exposure to the CTCP. These measures were used as contrast measures to rule out that cross-city differences in tobacco-related variables were caused not so much by the effects of the CTCP but attributable to the effect of other confounding variables that resulted in healthier habits among San Diego residents compared with those in the 2 Mexican cities, and in healthier habits among Tijuana residents compared with Guadalajara residents. Our contrast measures included physical activity (i.e., amount of time spent exercising during the past 7 days in minutes), alcohol use (i.e., number of alcohol drinks during the past 7 days), and sedentary behavior (i.e., average number of minutes spent watching television per day).
Statistical Analysis
To strengthen the comparability of the data, we standardized the 3 samples to match the age and gender characteristics of the Mexican-descent population in San Diego, with data from the US Census 2000.31 We estimated prevalence rates and 95% confidence intervals (CIs) for all study variables. Logistic and linear regression models were estimated to test for significant cross-city differences in each tobacco-related variable, with study site as the predictor and San Diego as the reference category. Odds ratios (ORs), multiple linear regression coefficients, and 95% CIs estimated for Tijuana and Guadalajara with these models were used to test for significant differences in tobacco-related variables between each Mexican city and San Diego. Tests for significant differences between Tijuana and Guadalajara were based on the overlap between the 95% CIs of the ORs and multiple linear regression coefficients estimated for each city. Nonoverlapping CIs indicated significant differences between the 2 Mexican cities with a P value lower than .05. All regression models included gender, age, marital status, employment status, education, and country of birth as covariates. These analyses were replicated for the non–tobacco-related health behaviors (e.g., exercise, alcohol use, and sedentary behavior). All analyses were conducted with SPSS version 14.0 (SPSS Inc, Chicago, Ill).
RESULTS
Figures 1 ▶–4 ▶ ▶ ▶ show weighted prevalence estimates and 95% CIs of current smoking, daily exposure to environmental tobacco smoke, smoking bans, and history of tobacco-related diseases by study site. In general, these estimates varied significantly across city in the hypothesized direction. For instance, the prevalence of exposure to environmental tobacco smoke was 32.6% (95% CI = 29.8%, 35.4%) in San Diego, 52.5% (95% CI=47.5%, 57.5%) in Tijuana, and 64.6% (95% CI = 59.8%, 69.4%) in Guadalajara. With regard to smoking bans in the home, the prevalence varied from 90.7% (95% CI = 89.0%, 92.4%) in San Diego, to 66.2% (95% CI = 61.5%, 70.9%) in Tijuana, and 39% (95% CI = 34.2%, 43.8%) in Guadalajara.
FIGURE 1—
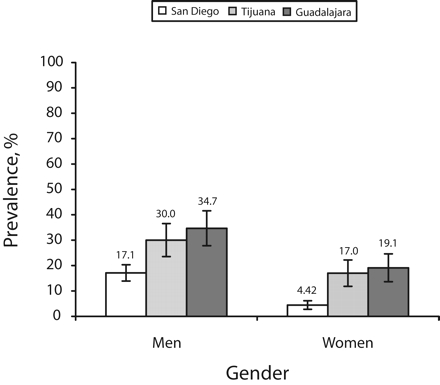
Standardized prevalence rates of current smoking among adults of Mexican descent (N = 1901), by gender and city: San Diego, Calif; Tijuana, Mexico; and Guadalajara, Mexico, 2003–2004.
Note. Cross-city comparisons represent significant differences (P < .05) based on results of logistic regression models with standardized data, after we controlled for age, gender, education level, marital status, and country of birth. For males and females, San Diego < Tijuana and San Diego < Guadalajara.
FIGURE 2—
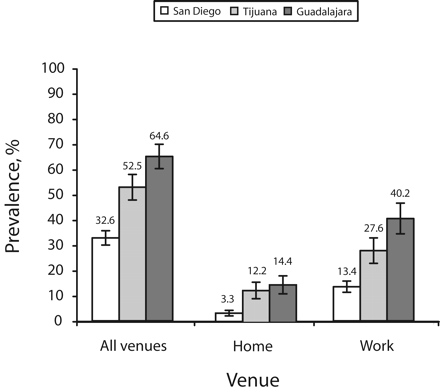
Standardized prevalence rates of daily exposure to environmental tobacco smoke among adults of Mexican descent (N = 1901), by venue and city: San Diego, Calif; Tijuana, Mexico; and Guadalajara, Mexico, 2003–2004.
Note. Cross-city comparisons represent significant differences (P < .05) based on results of logistic regression models with standardized data, after we controlled for age, gender, education level, marital status, and country of birth. For all venues, San Diego < Tijuana, San Diego < Guadalajara, and Tijuana < Guadalajara. For the home and workplace, San Diego < Tijuana and San Diego < Guadalajara.
FIGURE 3—

Standardized prevalence rates of smoking bans among adults of Mexican descent (N = 1901), by venue and city: San Diego, Calif; Tijuana, Mexico; and Guadalajara, Mexico, 2003–2004.
Note. Cross-city comparisons represent significant differences (P < .05) based on results of logistic regression models with standardized data, after we controlled for age, gender, education level, marital status, and country of birth. For the home and workplace, San Diego > Tijuana, San Diego > Guadalajara, and Tijuana > Guadalajara.
FIGURE 4—

Standardized prevalence rates of history of tobacco-related diseases among adults of Mexican descent (N = 1901), by city: San Diego, Calif; Tijuana, Mexico; and Guadalajara, Mexico, 2003–2004.
Note. Cross-city comparisons represent significant differences (P < .05) based on results of logistic regression models with standardized data, after we controlled for age, gender, education level, marital status, and country of birth. Comparison, San Diego < Tijuana, San Diego < Guadalajara, and Tijuana < Guadalajara.
Results from multivariate analyses indicated that the odds of being a current smoker were significantly greater for Tijuana (OR = 2.64; 95% CI = 1.86, 3.75) and Guadalajara (OR = 3.49; 95% CI = 2.49, 4.88) residents compared with Mexican-descent residents of San Diego. For this variable, no significant differences were found between the 2 Mexican cities (P > .05). Tijuana (OR = 2.15; 95% CI = 1.65, 2.80) and Guadalajara (OR = 4.0; 95% CI = 3.05, 5.24) residents were more likely to be exposed to environmental tobacco smoke than were Mexican-descent residents of San Diego. Moreover, Guadalajara residents were almost 2 times more likely to be exposed to environmental tobacco smoke than their counterparts in Tijuana (P < .05).
Significant cross-city differences in the hypothesized direction were observed for smoking bans in the home and the workplace among the 3 cities. Home smoking bans were less prevalent in Tijuana (OR=0.15; 95% CI=0.11, 0.22) and in Guadalajara (OR = 0.06; 95% CI = 0.04, 0.08) than in San Diego. Moreover, the OR for Tijuana residents was about 2.5 times greater (P < .05) than that estimated for their Guadalajara counterparts. The same gradient was found for the prevalence of smoking bans in the workplace among respondents employed full or part time. Tijuana and Guadalajara residents were less likely to work in a smokefree environment (Tijuana vs San Diego: OR = 0.64; 95% CI = 0.45, 0.90; Guadalajara versus San Diego: OR = 0.22; 95% CI = 0.15, 0.32). In addition, Guadalajara residents’ OR for the risk of not working in a smokefree environment was almost 3 times greater compared with that of the Ti-juana residents (P < .05).
A parallel pattern was observed for the likelihood of a lifetime history of tobacco-related diseases. On average, and compared with Mexican-descent residents of San Diego, Tijuana residents were 1.7 times more likely (95% CI = 1.31, 2.19) and Guadalajara residents were 3.07 times more likely (95% CI = 2.36, 4.01) to report a lifetime history of tobacco-related disease. The OR for Guadalajara was about 1.8 times greater than that estimated for Tijuana (P < .05).
Table 2 ▶ presents the estimated prevalence rates and 95% CIs for theoretical mediators of tobacco control, as well as average SOMER-STOL scores. In general, these estimates were highest for San Diego, next highest for Tijuana, and lowest for Guadalajara. For instance, the perception of very likely social criticism for smoking inside restaurants was endorsed by 70.2% of San Diego respondents, 47.0% of Tijuana respondents, and 32.0% of Guadalajara respondents. High support for smoke-free legislation that applies to restaurants was endorsed by 90.1%, 79.3%, and 65.9% of respondents in San Diego, Tijuana, and Guadalajara, respectively. Average SOMERSTOL scores were highest for Mexican-descent San Diego residents (69.1), followed by Tijuana residents (58.2) and Guadalajara residents (53.7).
Table 3 ▶ shows the results of logistic models estimated for each theoretical mediator of tobacco control, adjusted for all socioeconomic variables included in the analyses. In general, ORs estimated for the association between study site and the probability of each theoretical tobacco-control mediator differed in a pattern similar to that for tobacco-control outcomes.
TABLE 3—
Adjusted Odds Ratios (ORs) and 95% Confidence Intervals (CIs) for Cross-City Differences Based on Logistic Regression Models for Each Theoretical Mediator of Tobacco Control Among Mexicans in Tijuana and Guadalajara, Mexico, and Americans of Mexican Descent in San Diego, Calif (N = 1901): 2003–2004.
| Tijuana | Guadalajara | |
| Social criticism for smoking inside public places very likely, OR (95% CI) | ||
| Workplace | 0.43 (0.33, 0.56) | 0.37 (0.28, 0.47) |
| Restaurants | 0.37 (0.28, 0.48) | 0.21 (0.16, 0.27) |
| Public transportation | 0.36 (0.27, 0.48) | 0.34 (0.25, 0.46) |
| Schools | 0.31 (0.22, 0.42) | 0.28 (0.21, 0.39) |
| Health centers and hospitals | 0.63 (0.42, 0.95) | 1.09 (0.67, 1.78) |
| Intolerance toward smoking from normative group, OR (95% CI) | ||
| Spouse | 0.56 (0.41, 0.77) | 0.31 (0.23, 0.43) |
| Most family members | 0.54 (0.40, 0.72) | 0.42 (0.31, 0.57) |
| Most friends | 0.50 (0.35, 0.71) | 0.20 (0.12, 0.32) |
| Perceived access to nearest tobacco selling point > 1 minute away from home | 0.48 (0.34, 0.67) | 0.26 (0.19, 0.35) |
| Participation in tobacco prevention and awareness of free, local cessation programs, OR (95% CI) | ||
| Education | 0.57 (0.36, 0.92) | 0.31 (0.19, 0.52) |
| Cessation | 0.34 (0.26, 0.45) | 0.37 (0.28, 0.49) |
| Reported density of smoke-free public places, OR (95% CI) | ||
| All workplaces | 0.50 (0.33, 0.74) | 0.38 (0.25, 0.58) |
| All restaurants | 0.26 (0.18, 0.39) | 0.17 (0.11, 0.26) |
| All public transportation | 0.36 (0.27, 0.47) | 0.44 (0.34, 0.57) |
| All schools | 0.58 (0.43, 0.77) | 0.30 (0.23, 0.39) |
| All health centers and hospitals | 0.80 (0.59, 1.09) | 0.79 (0.58, 1.06) |
| Reported legislation banning smoking inside public places, OR (95% CI) | ||
| Workplaces | 0.56 (0.41, 0.75) | 0.48 (0.35, 0.65) |
| Restaurants | 0.32 (0.24, 0.44) | 0.21 (0.15, 0.29) |
| Public transportation | 0.30 (0.20, 0.43) | 0.49 (0.33, 0.73) |
| Schools | 0.41 (0.28, 0.60) | 0.36 (0.25, 0.51) |
| Health centers and hospitals | 0.82 (0.56, 1.21) | 0.79 (0.54, 1.15) |
| High support for smoke-free legislation for public places, OR (95% CI) | ||
| Workplaces | 0.68 (0.46, 0.99) | 0.43 (0.30, 0.61) |
| Restaurants | 0.36 (0.25, 0.52) | 0.20 (0.14, 0.28) |
| Public transportation | 0.79 (0.50, 1.25) | 0.55 (0.36, 0.85) |
| Schools | 0.62 (0.35, 1.09) | 0.37 (0.23, 0.60) |
| Health centers and hospitals | 1.13 (0.61, 2.11) | 0.90 (0.49, 1.66) |
| SOMERSTOL composite score,a b (95% CI) | −11.3 (−13.0,−9.7) | −15.3 (−16.9, −13.7) |
Note. SOMERSTOL = Scale of Theoretical Mediators of Tobacco Control. San Diego, Calif, was the reference category. All regression models included gender, age, level of education, marital status, employment status, and country of birth as covariates and were based on standardized data.
aAdjusted unstandardized regression coefficients (b) and 95% CIs were based on a linear regression model of total scores in the SOMERSTOL scale.
Cross-city differences in tobacco-control outcomes were paralleled by differences in the likelihood of perceptions of social criticism, reported normative rejection of smoking, participation in tobacco cessation or education programs, access to tobacco selling points, beliefs regarding smokefree legislation, and density of smokefree public places. For instance, compared with San Diego, Tijuana (OR = 0.37; 95% CI = 0.28, 0.48) and Guadalajara respondents (OR = 0.21; 95% CI = 0.16, 0.27) were significantly less likely to report that they would be criticized for smoking in restaurants, with the OR for Tijuana respondents being about 1.76 times greater than that estimated for Guadalajara residents (P<.05). Similarly, Tijuana (OR=0.50; 95% CI = 0.35, 0.71) and Guadalajara residents (OR = 0.20; 95% CI = 0.12, 0.32) were also less likely than were San Diego residents to perceive their friends as intolerant toward smoking. Furthermore, Tijuana respondents’ OR was about 2.5 times greater than that estimated for Guadalajara respondents (P < .05).
Overall, results from multivariate analyses indicated that, compared with San Diego residents of Mexican descent, Tijuana residents were significantly less likely to perceive theoretical mediators of tobacco control (e.g., perceived criticism for smoking, support for smokefree legislation, and so on) for 21 of 26 theoretical mediators examined (81%). In the case of Guadalajara residents versus Mexican-descent San Diego residents, the former were significantly less likely to report these perceptions for 23 of the 26 theoretical mediators (88%). As for comparisons between the 2 Mexican cities, differences reached statistical significance only for 3 theoretical mediators: reported criticism for smoking in restaurants, perceived negative reactions from friends, and perceived density of smokefree schools (Table 3 ▶). However, the direction of the variations of the ORs estimated for the 2 cities was consistent with our hypothesis. In 22 of the 26 theoretical mediators examined (85%), ORs for Tijuana residents were higher than those for Guadalajara residents, which indicated a tendency for the residents of the border town to be more likely to perceive these theoretical mediators. The likelihood of obtaining this consistent pattern of results (i.e., 22 of 26) by chance is less than 1 in 1000 (P value based on binomial test and Z approximation < .001).
With regard to differences in SOMERSTOL scores, results from a linear regression model indicated that not only were average scores for Tijuana (b = −11.3; 95% CI = −13.0, −9.7) and Guadalajara (b = −15.3; 95% CI = −16.9, −13.7) significantly different from those estimated for San Diego but also were statistically different between the 2 Mexican cities (P < .05; Table 3 ▶).
Our contrast analyses indicated that cross-city differences in exercise, alcohol use, and sedentary behavior did not resemble those found for tobacco-related outcomes and theoretical mediators. Results from multivariate analyses indicated that the 3 cities did not significantly differ in the amount of time their residents spent exercising (Tijuana vs San Diego: b = −33.6; 95% CI = −113.8, 46.7; Guadalajara vs San Diego: b = −26.2; 95% CI = −105.6, 53.2). Residents of Tijuana (b = 1.56; 95% CI = 0.58, 2.54) and Guadalajara (b = 1.3; 95% CI = 0.33, 2.27) consumed a higher number of alcoholic drinks during the previous 7 days than did San Diego residents. However, no differences were found between the 2 Mexican cities (P > .05). With regard to sedentary behavior, Tijuana residents reported a higher number of daily minutes spent watching television compared with San Diego residents (b = 21.1; 95% CI = 7.58, 34.6), but no significant differences were found between San Diego and Guadalajara residents (P > .05).
DISCUSSION
We examined tobacco-related behaviors and perceptions on Mexican-descent adults residing in 3 cities representing differential levels of exposure to the CTCP. The consistent finding of gradual cross-city differences in smoking, exposure to environmental tobacco smoke, and smoking bans suggested a dose–effect relationship between exposure to this program and these tobacco-related behaviors. This interpretation is strengthened by the differences observed in tobacco-related diseases and theoretical mediators of tobacco control.
According to the BEM,34 the composite of policies, media campaigns, economic measures, and provision of tobacco cessation and education services that a program like the CTCP entails leads to changes in social sentiments and public views on tobacco use and exposure to environmental tobacco smoke. In turn, these cultural changes create differences in actual and perceived opportunities to smoke, differential rates of exposure to people who model smoking behavior in a variety of social contexts, and varying social and economic costs associated with smoking behaviors. In all, the configuration of these social, cultural, legal, and structural factors results in different benefits or cost ratios associated with smoking in different communities and, consequently, in differential rates of smoking, exposure to environmental tobacco smoke, and, ultimately, tobacco-related morbidity that parallel these ratios.
The comprehensive and long-standing CTCP seems to have altered tobacco-related views and practices not only among California residents, but also among Mexican residents in Tijuana. This is suggested by the pattern of differences in tobacco use, exposure to environmental tobacco smoke, policies, and theoretical correlates between the border city of Tijuana and the more distant Guadalajara. Tijuana participants consistently reported tobacco-related behaviors and perceptions that were positioned approximately midway between responses from San Diego and Guadalajara participants. At the time the survey was conducted, no real differences in tobacco-related legislation existed between Tijuana and Guadalajara. In both cities, as in Mexico as a whole, existing laws about tobacco banned smoking in government buildings and health centers, prohibited sales of tobacco to minors, and restricted direct advertising of tobacco products in certain media (i.e., radio) and during specific time periods (i.e., television ads only allowed in the evening). Our findings suggested that the CTCP, through media, traveling, and social interaction, has permeated the Tijuana culture and produced increments in the degree of tobacco control in this Mexican city compared with other Mexican cities outside California’s radius of influence, such as Guadalajara.
The influence of the CTCP on Tijuana residents is supported by the lack of similar cross-city differences in other health-related behaviors, such as exercise, alcohol, and time spent in sedentary behaviors. If our findings with regard to tobacco-related outcomes and theoretical mediators were explained by other unaccounted graded variables, one would expect to see a similar pattern of cross-city differences in other health-related behaviors. Our contrast analyses did not show evidence of this gradient for exercise, alcohol use, and sedentary behavior. Moreover, we did find significant differences in tobacco-related behaviors and diseases, which suggests that cross-city differences were specifically related to variables that were modifiable through exposure the CTCP.
Comparisons of smoking and exposure to environmental tobacco smoke in Tijuana versus other border towns far away from California, such as Ciudad Juarez (Chihuahua, Mexico) and Nuevo Laredo (Tamaulipas, Mexico) strengthen the validity of our inferences. Both Ciudad Juarez (population 1 512 354) and Nuevo Laredo (population 348 387) border Texas, whose smokefree legislation and spending on tobacco control contrast with that of California. In 2006, Texas still lacked provisions that banned or restricted smoking in public places and spent 6.79% of the Centers for Disease Control and Prevention–recommended minimum for tobacco control. In the same year, California already had smokefree provisions in place and spent 48.27% of the Centers for Disease Control and Prevention–recommended minimum on tobacco prevention control.35–37
On a range of tobacco-related behaviors, attitudes, and cultural factors examined by the Global Youth Tobacco Surveys38,39 and other Mexican surveys,40 estimates for youths in Tijuana were generally better than those for youths in Ciudad Juarez and Nuevo Laredo (i.e., 11.5% of Tijuana youths reported having smoked in the past 30 days compared with 22.6% in Ciudad Juarez and 16.5% in Nuevo Laredo). By contrast, consumption by youths of other drugs is highest in Tijuana compared with Ciudad Juarez and Guadalajara.41 These findings suggest that the differences between Tijuana and Guadalajara do not stem merely from the border location of Tijuana or other sociodemographic differences between the populations of these 2 cities, but rather from Tijuana’s proximity to California and exposure to the CTCP. Programs of similar comprehensiveness and duration may generalize across national borders and translate into substantial reductions of smoking, exposure to environmental tobacco smoke, and related morbidity at the population level.
Mexico has recently signed and ratified the World Health Organization’s Framework Convention on Tobacco Control. This international treaty on tobacco control sets standards for banning tobacco advertising and promotion and provides guidance for nations to establish tobacco-related regulations, taxation, smokefree public places, and education and cessation programs. Mexican public health officials can look at Tijuana as a case study that shows that Mexican nationals are responsive to and supportive of tobacco-control measures, even when these are experienced only indirectly through interactions with California-based residents and media. On the basis of this experience, Mexico officials could abstract lessons to design structural interventions to expand tobacco control in Mexico and reduce the level of morbidity and mortality associated with tobacco use and exposure to environmental tobacco smoke.
Limitations
In this study, we used a cross-sectional design and a surrogate measure of exposure to the CTCP (i.e., city of residence vs exposure to specific activities of the CTCP). Residents in the 3 selected cities may have presented differences in unmeasured confounding variables. Our results were consistent with previous US research that evidenced an association between state- and community-level tobacco control measures and tobacco use,17,18 environmental tobacco smoke exposure,19 and smoking bans.20 Our findings were also supported by evidence on the progressive reduction in smoking, environmental tobacco smoke exposure, and tobacco-related mortality observed in California since the introduction of the CTCP.13,42–44 The lack of data for Tijuana and Guadalajara from the period prior to the CTCP precludes us from establishing causal temporal order in the observed associations. Cross-sectional designs, surrogate measures, and systematic selection of study sites are often the only available methods for research on tobacco policies. Cumulative evidence from such natural experiments builds the basis for advancing tobacco-control efforts.
Cooperation rates across the 3 cities were moderate and comparable to those attained by statewide tobacco surveys.13 The sociodemographic profile of the 3 study samples closely resembled that of the target populations in San Diego, Tijuana, and Guadalajara. The greater percentage of foreign-born individuals among the San Diego sample compared with the target population increased the comparability to Tijuana and Guadalajara, making the case for the influence of exposure to the CTCP even stronger.
The use of 2 different data collection methods (i.e., phone survey in San Diego vs door-to-door household surveys in Mexico) raises the possibility of a measurement artifact. This artifact would not explain the pattern of differences observed between the 2 Mexican cities. We observed no significant differences in prevalence estimates of smoking, exposure to environmental tobacco smoke, and smoking bans between respondents interviewed by phone and face-to-face in Mexico (data not shown). Thus, it is unlikely that our findings would have varied substantially had we used the same data-collection methods across the 3 study sites.
Measures were based solely on self-report. Self-reported measures on smoking, exposure to environmental tobacco smoke, home policies, and health conditions have demonstrated satisfactory validity levels.45–48 Variations in social stigma associated with smoking in the 3 cities might have led to different levels of accuracy of self-reports on smoking and exposure to environmental tobacco smoke across these cities. According to the BEM,5 changes in social norms and attitudes about health-related behaviors trigger behavioral changes at the population level. In California, changes in attitudes about smoking have been paralleled by reductions in smoking, environmental tobacco smoke exposure, and per capita cigarette sales over the past 2 decades.13,49 These theoretical and empirical considerations suggest that our findings reflected cross-city differences in consumption and exposure rather than just variations on the accuracy of self-reports. Future tobacco research that includes both self-report and biological measures on smoking and exposure to environmental tobacco smoke is warranted to corroborate these results.
Conclusions
Our results suggest a significant association between exposure to the CTCP and the prevalence of tobacco-related behaviors and perceptions. The prevalence of home bans, tobacco use, environmental tobacco smoke exposure, tobacco-related diseases, and theoretical mediators of these outcomes paralleled the different levels of exposure to the California culture generated by the CTCP. These results indicated that comprehensive tobacco-control programs such as the CTCP have widespread effects and should be adopted in other regions to reduce smoking, exposure to environmental tobacco smoke, and tobacco-related morbidity throughout the population.
Acknowledgments
This study was supported in part by funds from the Tobacco-Related Disease Research Program of the University of California (grant 11RT-0148).
The authors would like to thank the 3 anonymous reviewers for their comments and suggestions on this article.
Human Participation Protection This study was approved by San Diego State University’s institutional review board.
Peer Reviewed
Contributors A. P. Martínez-Donate and M. F. Hovell originated and supervised the study. C. R. Hofstetter and G. J. González-Pérez assisted with sampling and survey methodology. A. P. Martínez-Donate led and reviewed data analysis. A. Kotay and M. A. Adams assisted with data analysis. All authors reviewed and edited previous versions of the article.
References
- 1.Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States, 1995–1999. MMWR Morb Mortal Wkly Rep. 2002; 51:300–303. [PubMed] [Google Scholar]
- 2.World Health Organization. Tobacco Free Initiative Web page. Why is tobacco a public health priority? Available at: http://www.who.int/tobacco/health_priority/en/index.html. Accessed June 29, 2006.
- 3.Peto R, Lopez AD. Future worldwide health effects of current smoking patterns. In: Koop CE, Pearson CE, Schwartz MR, eds. Critical Issues in Global Health. San Francisco, Calif: Jossey-Bass; 2001:154–161.
- 4.Warner KE. The role of research in international tobacco control. Am J Public Health. 2005;95: 976–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hovell MF, Wahlgren DR, Gehrman CA. The behavioral ecological model: integrating public health and behavioral science. In: DiClemente RJ, ed. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. San Francisco, Calif: Jossey-Bass; 2002:347–385.
- 6.Martinez-Donate AP, Hovell MF, Zellner J, Sipan CL, Blumberg EJ, Carrizosa C. Evaluation of two school-based HIV prevention interventions in the border city of Tijuana, Mexico. J Sex Res. 2004;41:267–278. [DOI] [PubMed] [Google Scholar]
- 7.Sallis JF, Hovell MF. Determinants of exercise behavior. Exerc Sport Sci Rev. 1990;18:307–330. [PubMed] [Google Scholar]
- 8.Hovell MF, Wahlgren DR, Russos S. Preventive medicine and cultural contingencies: the great natural experiment. In: Lamal PA, ed. Cultural Contingencies: Behavior Analytic Perspectives on Cultural Practices. Westport, Conn: Praeger Publications; 1997:1–29.
- 9.Lavelle JM, Hovell MF, West MP, Wahlgren DR. Promoting law enforcement for child protection: a community analysis. J Appl Behav Anal. 1992;25: 885–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wahlgren DR, Hovell MF, Slymen DJ, Conway TL, Hofstetter CR, Jones JA. Predictors of tobacco use initiation in adolescents: a two-year prospective study and theoretical discussion. Tob Control. 1997;6: 95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skinner BF. Science and Human Behavior. New York, NY: Macmillan; 1953.
- 12.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
- 13.Gilpin EA, White MM, White VM, et al. Tobacco Control Successes in California: A Focus on Young People, Results From the California Tobacco Surveys, 1990–2002. La Jolla, Calif: University of California, San Diego; 2004.
- 14.Meneses-Gonzalez F, Marquez-Serrano M, Sepulveda-Amor J, Hernandez-Avila M. The tobacco industry in Mexico [in Spanish]. Salud Publica Mex. 2002; 44(suppl 1):S161–S169. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Illegal sales of cigarettes to minors—Mexico City, Mexico, 1997. MMWR Morb Mortal Wkly Rep. 1997;46: 440–444. [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Illegal sales of cigarettes to minors—Ciudad Juarez, Mexico; El Paso, Texas; and Las Cruces, New Mexico, 1999. MMWR Morb Mortal Wkly Rep. 1999;48: 394–398. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. State-specific prevalence of current cigarette smoking among adults, and policies and attitudes about secondhand smoke—United States, 2000. MMWR Morb Mortal Wkly Rep. 2001;50:1101–1106. [PubMed] [Google Scholar]
- 18.American Lung Association. Tobacco control summary reports. State laws restricting smoking in public places and workplaces. Available at: http://slati.lungusa.org/appendixa.asp. Accessed July 5, 2006.
- 19.Albers AB, Siegel M, Cheng DM, Rigotti NA, Biener L. Effects of restaurant and bar smoking regulations on exposure to environmental tobacco smoke among Massachusetts adults. Am J Public Health. 2004; 94:1959–1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levy DT, Romano E, Mumford EA. Recent trends in home and work smoking bans. Tob Control. 2004; 13:258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Department of Transportation, Bureau of Transportation Statistics. Special tabulation, June 2005. Table 1–45: U.S.-Mexican border land-passenger gateways: entering the United States. Available at: http://www.bts.gov/publications/national_transportation_statistics/excel/table_01_45.xls. Accessed July 5, 2006.
- 22.Meissner D. Forum Fronterizo: Solving Our Border-Crossing Problem in an Era of Terrorism. University of California Television; 2001. Available at: http://web-cast.ucsd.edu:8080/ramgen/UCSD_TV/6167For-FroBorCro.rm. Accessed July 5, 2006.
- 23.Instituto Nacional de Geografía y Estadística [National Institute of Statistics, Geography, and Informatics]. Migrant population to the United States of America by federative entity and gender, 2000 [in Spanish]. Available at: http://www.inegi.gob.mx/est/contenidos/espanol/rutinas/ept.asp?t=mpob67&c=3244. Accessed June 29, 2006.
- 24.Instituto Nacional de Geografía y Estadística [National Institute of Statistics, Geography, and Informatics]. Immigration, emigration, and net migration by federative entity, 1995–2000 [in Spanish]. Available at: http://www.inegi.gob.mx/est/contenidos/espanol/rutinas/ept.asp?t=mpob62&c=3239. Accessed June 29, 2006.
- 25.Roberts BR, Frank R, Lozano-Ascencio F. Transnational migrant communities and Mexican migration to the US. Ethn Racial Stud. 1999;22:238–266. [Google Scholar]
- 26.Bauer T, Epstein G, Gang IN. Herd Effects or Migration Networks? The Location Choice of Mexican Immigrants in the U.S. Bonn, Germany: Institute for the Study of Labor; 2002. Discussion paper 551.
- 27.Bean FD, Corona R, Tuirán R, Woodrow-Lafield KA. Quantification of Migration. Estimating Unauthorized Mexican Migration to the United States. Migration Between Mexico and United States, Binational Study. Austin, Tex: Mexican Ministry of Foreign Affairs and US Commission on Immigration Reform. 1998;1:1–90.
- 28.Jones RC. Undocumented migration from Mexico: some geographical questions. Ann Assoc Am Geogr. 1982;72:77. [Google Scholar]
- 29.Community Partnership Agreement: Community Technology Foundation. Current telephone penetration levels. Comparison of 1994, 1995, 1996, 1997, 1998, and 1999 telephone penetration rate estimates for Pacific Bell using current population survey data. Available at: http://www.partnership.pacbell.net/text/phone_levels.html. Accessed November 16, 2001.
- 30.Instituto Nacional de Estadistica, Geografía e Informática [National Institute of Statistics, Geography, and Informatics]. Municipal system of databases [in Spanish]. Availaible at: http://www.inegi.gob.mx/inegi/default.aspx. Accessed October 15, 2007.
- 31.US Bureau of the Census. American Fact Finder, 2000. Available at: http://factfinder.census.gov/home/saff/main.html?_lang=en. Accessed April 28, 2005.
- 32.California Department of Health Services, Tobacco Control Section. California Tobacco Survey: 2002 [computer file]. La Jolla, Calif: Cancer Prevention and Control Unit, University of California, San Diego; 2004.
- 33.National Center for Health Statistics. National Health Interview Survey. Questionnaires, datasets, and related documentation 1997–2006. Available at: http://www.cdc.gov/nchs/about/major/nhis/quest_data_related_1997_forward.htm. Accessed March 21, 2007.
- 34.Hovell M, Roussos S, Hill L, Johnson NW, Squier C, Gyenes M. Engineering clinical leadership and success in tobacco control: recommendations for policy and practice in Hungary and Central Europe. Eur J Dent Educ. 2004;8(suppl 4):51–60. [DOI] [PubMed] [Google Scholar]
- 35.American Lung Association. State of tobacco control: 2006. Available at: http://lungaction.org/reports/tobacco-control06.html. Accessed February 13, 2007.
- 36.Campaign for Tobacco-Free Kids. Special reports. State tobacco settlement. Texas, 2006. Available at: http://www.tobaccofreekids.org/reports/settlements/toll.php?StateID=TX. Accessed February 13, 2007.
- 37.Campaign for Tobacco-Free Kids. Special reports. State tobacco settlement. California, 2006. Available at: http://www.tobaccofreekids.org/reports/settlements/state.php?StateID=CA. Accessed February 13, 2007.
- 38.Centers for Disease Control and Prevention. Global youth tobacco survey fact sheet, Mexico-Ti-juana. Available at: http://www.cdc.gov/tobacco/global/GYTS/factsheets/2003/Mexico_tijuana_fact-sheet.htm. Accessed July 5, 2006.
- 39.Centers for Disease Control and Prevention. Global youth tobacco survey fact sheet, Mexico-Juarez. Available at: http://www.cdc.gov/tobacco/global/gyts/factsheets/2003/Mexico_Juarez_factsheet.htm. Accessed July 5, 2006.
- 40.Secretaria de Salud, Instituto Nacional de Salud Publica [Secretariat of Health, National Institute of Public Health]. Survey on tobacco use among youth. Mexico 2003 [in Spanish]. Available at: http://www.insp.mx/tabaco/libro/inicio.html. Accessed February 13, 2007.
- 41.Medina-Mora ME, Cravioto P, Villatoro J, Fleiz C, Galvan-Castillo F, Tapia-Conyer R. Drug use among adolescents: results from the National Survey on Addictions, 1998 [in Spanish]. Salud Publica Mex. 2003; 45(suppl 1):S16–S25. [PubMed] [Google Scholar]
- 42.Norman GJ, Ribisl KM, Howard-Pitney B, Howard KA, Unger JB. The relationship between home smoking bans and exposure to state tobacco control efforts and smoking behaviors. Am J Health Promot. 2000;15: 81–88. [DOI] [PubMed] [Google Scholar]
- 43.Fichtenberg CM, Glantz SA. Association of the California Tobacco Control Program with declines in cigarette consumption and mortality from heart disease. N Engl J Med. 2000;343:1772–1777. [DOI] [PubMed] [Google Scholar]
- 44.Barnoya J, Glantz S. Association of the California tobacco control program with declines in lung cancer incidence. Cancer Causes Control. 2004;15:689–695. [DOI] [PubMed] [Google Scholar]
- 45.Hovell MF, Zakarian JM, Wahlgren DR, Matt GE, Emmons KM. Reported measures of environmental tobacco smoke exposure: trials and tribulations. Tob Control. 2000;9(suppl 3):22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84:1086–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–218. [DOI] [PubMed] [Google Scholar]
- 48.Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS). Soz Praventivmed. 2001;46:S3–S42. [PubMed] [Google Scholar]
- 49.Orzechowski W, Walker RC. The Tax Burden on Tobacco: Historical Compilation. Vol 37. Arlington, Va: Orzechowski and Walker; 2003.


