Abstract
Unprotected sexual intercourse remains a primary mode of HIV transmission in the United States. We found that receipt of services to reduce HIV transmission-risk behaviors was low among 3787 HIV-infected individuals and that men who have sex with men were especially unlikely to receive these services even though they were more likely to report unprotected sexual intercourse with seronegative and unknown serostatus casual partners. Greater efforts should be made to ensure that prevention counseling is delivered to all HIV-infected persons, especially men who have sex with men.
A recent critique of HIV prevention in the United States has argued for an increased focus on infected individuals who are most likely to engage in transmission-risk behaviors.1 Behavioral assessments to identify people at highest risk for infection are already a component of prevention guidelines2 and interventions for HIV-infected individuals.3–5 However, the actual delivery of prevention counseling may be hindered by factors unrelated to these assessments.6–8
In an evaluation of 16 publicly funded clinics, we found that providers were less likely to administer prevention counseling in settings serving primarily HIV-infected men who have sex with men (MSM).8 This observation is striking because it is critical to focus on MSM for prevention efforts. In 2005, 42% of newly diagnosed AIDS cases were attributable to male-to-male sexual contact,9 and recent studies of MSM have documented high levels of risk behaviors,10–17 sexually transmitted infections,10,11,18–22 and HIV.16,23
Our previous work did not allow us to examine whether delivery of prevention counseling was affected by differences in patients’ risk behaviors.8 In that study, we assessed only the types of services received during clinical appointments and did not capture detailed information on HIV transmission risks. To remedy this limitation, we examined data from the baseline assessment of the Healthy Living Project, a cognitive–behavioral intervention trial that has reduced transmission risks among HIV-infected people.4 We investigated whether the observed disparity in MSM’s receipt of services to help reduce HIV transmission-risk behaviors was replicated in a new sample and whether the prevalence of risk behaviors accounted for this difference.
METHODS
The Healthy Living Project baseline interview was completed by 3787 HIV-infected individuals in New York, New York; Milwaukee, Wisconsin; San Francisco, California; and Los Angeles, California. Participants were aged at least 18 years old, free of severe neuropsychological impairment, not involved in other HIV-related behavioral intervention studies, and willing to provide written informed consent and medical documentation of HIV infection. The trial examined the efficacy of an individual, 15-session intervention addressing stress and coping skills, avoidance of sexual and drug-related transmission risks, and active participation in health care decision making.24,25 Complete methodological24 and intervention25 descriptions are published elsewhere. A majority of participants were African American (n = 1841; 49%), Hispanic (n = 729; 19%), or White (n = 979; 26%). Their median age was 41 years (range 19–92). Most were male (n = 2773; 73%), not college educated (n = 2031; 54%), unemployed (n = 2659; 70%), on antiretroviral therapy (n = 2849; 75%), and had a CD4 count above 199 (n = 2802; 74%). Individuals were categorized as MSM (n = 1910; 50%) if they (1) were male and (2) either reported having had sexual contact with other men within the previous 3 months or, among sexually abstinent men, identified themselves as being gay or bisexual.
The baseline interview included a partner-by-partner assessment of sexual behavior in the previous 3 months.24 We defined HIV transmission-risk behavior as unprotected anal or vaginal intercourse with seronegative or unknown serostatus partners. The interview also assessed medical and social services received in the 3 months before trial participation and included a question about prevention services, which were described as “programs that work with persons who are HIV-positive to help reduce the spread of HIV.” We used generalized estimating equations, controlled for clustering by city, to examine the associations among prevention services, MSM status, and risk behaviors.
RESULTS
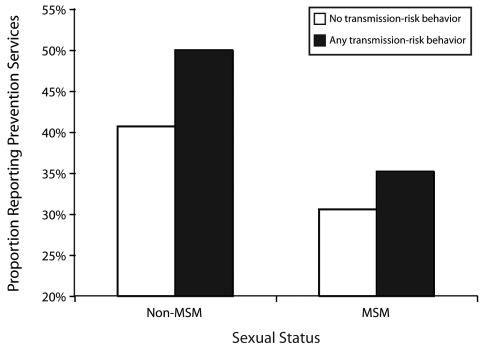
Approximately one third of participants (36%; n = 1356) had received prevention services in the 3 months before the interview. However, MSM were significantly less likely than were other participants to report receipt of these services (odds ratio [OR] = 0.64; 95% confidence interval [CI] = 0.54, 0.77) even though they were significantly more likely to report HIV transmission-risk behaviors with casual sexual partners (OR = 2.04; 95% CI = 1.46, 2.85). Nearly one third of MSM (31%; n=589) had received prevention programming, compared with 41% of non-MSM (n = 767). By contrast, 6% of MSM (n = 105) reported transmission-risk behaviors with casual sexual partners, compared with only 3% of non-MSM (n = 52).
As shown in Figure 1 ▶, when stratified by MSM status, fewer MSM than non-MSM received prevention services even though there was a positive association between risk behavior with casual sexual partners and prevention services (OR = 1.23; 95% CI = 1.11, 1.38 vs OR = 1.46; 95% CI = 1.15, 1.85). There was no correlation between prevention and risk behavior with steady sexual partners. In multivariable modeling, prevention services remained associated with non-MSM status as well as with race/ethnicity other than White, lack of antiretroviral therapy, and engaging in risk behaviors with casual sexual partners (Table 1 ▶).
FIGURE 1—
Receipt of prevention services among men, by sexual status and transmission-risk behavior with casual sexual partners: The Healthy Living Project, New York, NY; Milwaukee, WI; San Francisco, CA; and Los Angeles, CA, 1998–2006. Note. MSM = men who have sex with men.
TABLE 1—
Multivariate Associations With Receipt of HIV Prevention Services in the Previous 3 Months: The Healthy Living Project, New York, New York; Milwaukee, Wisconsin; San Francisco, California; and Los Angeles, California; 1998–2006
| Explanatory Variable | No.a | Adjusted OR (95% CI)b |
| Sexual Status | ||
| Non-MSM (Ref) | 1525 | 1.00 |
| MSM | 1608 | 0.69 (0.58, 0.82) |
| Race/Ethnicity | ||
| White (Ref) | 834 | 1.00 |
| African American | 1478 | 1.93 (1.38, 2.68) |
| Hispanic | 616 | 1.52 (1.16, 1.98) |
| Other | 205 | 1.52 (1.18, 1.94) |
| Gender | ||
| Female (Ref) | 801 | 1.00 |
| Male | 2286 | 1.08 (0.95, 1.22) |
| Transgender | 46 | 1.10 (0.89, 1.35) |
| Age (continuous variable) | 3313 | 1.00 (0.98, 1.02) |
| Education | ||
| High school or less (Ref) | 1646 | 1.00 |
| Some college or more | 1487 | 0.92 (0.79, 1.08) |
| Employment status | ||
| Not employed (Ref) | 2204 | 1.00 |
| Employed | 929 | 0.85 (0.67, 1.08) |
| CD4 cell count | ||
| < 200 (Ref) | 676 | 1.00 |
| ≥ 200 | 2457 | 0.91 (0.77, 1.09) |
| Currently on antiretroviral therapy | ||
| No (Ref) | 506 | 1.00 |
| Yes | 2627 | 0.81 (0.74, 0.89) |
| HIV transmission-risk behavior with steady sexual partners | ||
| No (Ref) | 2962 | 1.00 |
| Yes | 171 | 0.78 (0.51, 1.18) |
| HIV transmission-risk behavior with casual sexual partners | ||
| No (Ref) | 3008 | 1.00 |
| Yes | 125 | 1.30 (1.00, 1.68) |
a The number of participants does not sum to 3787 because of missing data.
b Standard errors were adjusted for clustering by city.
DISCUSSION
To maximize effectiveness, HIV prevention interventions must reach infected individuals who are particularly likely to engage in transmission-risk behaviors.1 Our research with HIV-infected people in 4 cities found that only a third had recently received prevention services and that MSM, who account for the largest group of new AIDS cases in the United States,9 were especially likely to have gone without such services even though they were more likely to report risk behaviors. In addition, prevention was lower among Whites and people receiving antiretroviral therapy.
These observations highlight substantial missed opportunities. Interventions are effective at reducing risk behaviors among people living with HIV.26 Increasing the delivery of prevention counseling may significantly reduce the epidemic’s spread. Greater efforts are needed to ensure that prevention counseling is delivered to all HIV-infected persons, especially MSM.
Acknowledgments
The Healthy Living Project was funded by cooperative agreements between the National Institute of Mental Health (NIMH) and Columbia University (U10MH057636); the Medical College of Wisconsin (U10MH057631); the University of California, Los Angeles (U10MH057615); and the University of California, San Francisco (U10MH057616).
The following were members of the NIMH Healthy Living Project Team. Research Steering Committee (site principal investigators and NIMH staff collaborators): Margaret A. Chesney, PhD, Anke A. Ehrhardt, PhD, Jeffrey A. Kelly, PhD, Willo Pequegnat, PhD, and Mary Jane Rotheram-Borus, PhD. Collaborating scientists, co-principal investigators, and investigators: Abdelmonem A. Afifi, PhD, Eric G. Benotsch, PhD, Michael J. Brondino, PhD, Sheryl L. Catz, PhD, William G. Cumberland, PhD, Don C. DesJarlais, PhD, Naihua Duan, PhD, Theresa M. Exner, PhD, Cheryl Gore-Felton, PhD, A. Elizabeth Hirky, PhD, Robert M. Kertzner, MD, Sheri B. Kirshenbaum, PhD, Lauren E. Kittel, PsyD, Robert Klitzman, MD, Martha Lee, PhD, Bruce Levin, PhD, Marguerita Lightfoot, PhD, Steven D. Pinkerton, PhD, Fen Rhodes, PhD, Juwon Song, PhD, Susan Tross, PhD, Lance S. Weinhardt, PhD, Robert Weiss, PhD, Hannah Wolfe, PhD, and Rachel Wolfe, PhD. Data Management and Analytic Support: Philip Batterham, MA, W. Scott Comulada, MS, Tyson Rogers, MA, and Yu Zhao, MS. Site project coordinators: Jackie Correale, MPH, Kristin Hackl, MSW, Daniel Hong, MA, Karen Huchting, BA, Joanne D. Mickalian, MA, and Margaret Peterson, MSW. NIMH: Christopher M. Gordon, PhD, Dianne Rausch, PhD, and Ellen Stover, PhD.
Human Participant Protection The study was reviewed and approved by the institutional review boards at Columbia University; the Medical College of Wisconsin; the University of California, Los Angeles; and the University of California, San Francisco.
Peer Reviewed
Contributors W.T. Steward originated the topic and led the writing. E. D. Charlebois, R. B. Goldstein, and F.L. Wong wrote statistical code necessary for the analyses. M. O. Johnson, R. H. Remien, and S. F. Morin made substantial contributions to the writing and had primary responsibilities for the study design and data collection at their sites.
References
- 1.Holtgrave DR, McGuire JF, Milan J Jr. The magnitude of key HIV prevention challenges in the United States: implications for a new national HIV prevention plan. Am J Public Health. 2007;97:1163–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV: recommendations of CDC, the Health Resources and Services Administration, the National Institutes of Health, and the HIV Medicine Association of the Infectious Disease Society of America. MMWR Morb Mortal Wkly Rep. 2003;52(RR-12): 1–24. [PubMed] [Google Scholar]
- 3.Fisher JD, Fisher WA, Cornman DH, Amico RK, Bryan A, Friedland GH. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. J Acquir Immune Defic Syndr. 2006;41:44–52. [DOI] [PubMed] [Google Scholar]
- 4.Healthy Living Project Team. Effects of a behavioral intervention to reduce risk of transmission among people living with HIV: the Healthy Living Project randomized controlled study. J Acquir Immune Defic Syndr. 2007;44:213–221. [DOI] [PubMed] [Google Scholar]
- 5.Malitz FE, Eldred L. Evolution of the special projects of national significance prevention with HIV-Infected Persons Seen in Primary Care Settings Initiative. AIDS Behav. 2007;11(suppl 5):S1–S5. [DOI] [PubMed] [Google Scholar]
- 6.Morin SF, Koester KA, Steward WT, et al. Missed opportunities: prevention with HIV-infected patients in clinical care settings. J Acquir Immune Defic Syndr. 2004; 36:960–966. [DOI] [PubMed] [Google Scholar]
- 7.Myers JJ, Steward WT, Charlebois E, Koester KA, Maiorana A, Morin SF. Written clinic procedures enhance delivery of HIV “Prevention With Positives” counseling in primary health care settings. J Acquir Immune Defic Syndr. 2004;37(suppl 2):S95–S100. [DOI] [PubMed] [Google Scholar]
- 8.Steward WT, Koester KA, Myers JJ, Morin SF. Provider fatalism reduces the likelihood of HIV prevention counseling in primary care settings. AIDS Behav. 2006;10:3–12. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. HIV/ AIDS Surveillance Report, 2005. Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention; 2007.
- 10.Centers for Disease Control and Prevention. Increases in unsafe sex and rectal gonorrhea among men who have sex with men—San Francisco, California, 1994–1997. MMWR Morb Mortal Wkly Rep. 1999; 48:45–48. [PubMed] [Google Scholar]
- 11.Chen SY, Gibson S, Katz MH, et al. Continuing increases in sexual risk behavior and sexually transmitted diseases among men who have sex with men: San Francisco, Calif, 1999–2001. Am J Public Health. 2002;92:1387–1388. [PMC free article] [PubMed] [Google Scholar]
- 12.Chen SY, Gibson S, Weide D, McFarland W. Unprotected anal intercourse between potentially HIV-serodiscordant men who have sex with men, San Francisco. J Acquir Immune Defic Syndr. 2003;33:166–170. [DOI] [PubMed] [Google Scholar]
- 13.Dodds JP, Nardone A, Mercey DE, Johnson AM. Increase in high risk sexual behaviour among homosexual men, London 1996–8: cross sectional, questionnaire study. BMJ. 2000;320:1510–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ekstrand ML, Stall RD, Paul JP, Osmond DH, Coates TJ. Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS. 1999;13:1525–1533. [DOI] [PubMed] [Google Scholar]
- 15.Elford J, Bolding G, Sherr L. High-risk sexual behaviour increases among London gay men between 1998 and 2001: what is the role of HIV optimism? AIDS. 2002;16:1537–1544. [DOI] [PubMed] [Google Scholar]
- 16.Katz MH, Schwarcz SK, Kellogg TA, et al. Impact of highly active antiretroviral treatment on HIV seroincidence among men who have sex with men: San Francisco. Am J Public Health. 2002;92:388–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van de Ven P, Prestage G, Crawford J, Grulich A, Kippax S. Sexual risk behaviour increases and is associated with HIV optimism among HIV-negative and HIV-positive gay men in Sydney over the 4 year period to February 2000. AIDS. 2000;14:2951–2953. [DOI] [PubMed] [Google Scholar]
- 18.Dupin N, Jdid R, N’Guyen YT, Gorin I, Franck N, Escande JP. Syphilis and gonorrhoea in Paris: the return. AIDS. 2001;15:814–815. [DOI] [PubMed] [Google Scholar]
- 19.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyber-space. JAMA. 2000;284:447–449. [DOI] [PubMed] [Google Scholar]
- 20.Stolte IG, Dukers NH, de Wit JB, Fennema JS, Coutinho RA. Increase in sexually transmitted infections among homosexual men in Amsterdam in relation to HAART. Sex Transm Infect. 2001;77:184–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heffelfinger JD, Swint EB, Berman SM, Weinstock HS. Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health. 2007;97:1076–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Truong HM, Kellogg T, Klausner JD, et al. Increases in sexually transmitted infections and sexual risk behaviour without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: a suggestion of HIV serosorting? Sex Transm Infect. 2006;82:461–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwarcz S, Scheer S, McFarland W, et al. Prevalence of HIV infection and predictors of high-transmission sexual risk behaviors among men who have sex with men. Am J Public Health. 2007;97:1067–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson MO, Catz SL, Remien RH, et al. Theory-guided, empirically supported avenues for intervention on HIV medication nonadherence: findings from the Healthy Living Project. AIDS Patient Care STDS. 2003; 17:645–656. [DOI] [PubMed] [Google Scholar]
- 25.Gore-Felton C, Rotheram-Borus MJ, Weinhardt LS, et al. The Healthy Living Project: an individually tailored, multidimensional intervention for HIV-infected persons. AIDS Educ Prev. 2005;17(1 suppl A):21–39. [DOI] [PubMed] [Google Scholar]
- 26.Herbst JH, Beeker C, Mathew A, et al. The effectiveness of individual-, group-, and community-level HIV behavioral risk-reduction interventions for adult men who have sex with men: a systematic review. Am J Prev Med. 2007;32(suppl 4):S38–S67. [DOI] [PubMed] [Google Scholar]